Vol. 26 - Num. 101
Original Papers
Adherence of prescribing practices in streptococcal pharyngitis and acute otitis media to treatment guidelines
Marcelo Vivas Morescoa, Beatriz Barbarin Sorozabalb, Silvia García de Garayo Díazc, José Tomás Ramos Amadord
aPediatra. CS de Salvatierra. Álava. España.
bPediatra. CS de San Adrián. Navarra. España.
cMatemática. OSI Álava de Osakidetza. Álava. España.
dServicio de Pediatría. Hospital Clínico San Carlos. Madrid. Instituto de Investigación Sanitaria Hospital Clínico San Carlos (IdISSC). Universidad Complutense. Madrid. España.
Correspondence: M Vivas. E-mail: marcevivas@gmail.com
Reference of this article: Vivas Moresco M, Barbarin Sorozabal B, García de Garayo Díaz S, Ramos Amador JT. Adherence of prescribing practices in streptococcal pharyngitis and acute otitis media to treatment guidelines . Rev Pediatr Aten Primaria. 2024;26:35-43. https://doi.org/10.60147/c4a39d2d
Published in Internet: 05-02-2024 - Visits: 3101
Abstract
Background and objective: to analyse the degree of adherence of primary care paediatricians to consensus treatment guidelines for acute pharyngotonsillitis and acute otitis media.
Material and methods: retrospective observational study with collection of data from the electronic health records of patients with suppurative AOM and streptococcal AP in
patients aged 0 to 14 years residing in Araba over an 18-month period.
Results: in the group of patients with suppurative AOM, 238 episodes were evaluated, with a proportion of appropriate prescribing of 56.7% and underdosing as the main reason of inappropriate prescribing. In the group of patients with streptococcal AP, 1721 episodes were evaluated, with a proportion of appropriate prescribing of 57%, and the main causes of inappropriate prescribing being prescription of excessive doses and short-duration regimens.
Conclusion: in both suppurative AOM and streptococcal AP, the frequency of appropriate prescribing was somewhat lower compared to other studies. Achieving appropriate treatment for these diseases in primary care settings is of vital importance due to their high incidence. Ensuring correct documentation in patient health records is another opportunity for improvement.
Keywords
● Acute otitis media ● Acute pharyngitis ● TreatmentINTRODUCTION
Acute otitis media (AOM) and acute pharyngitis/tonsillitis (APT) are two of the most commonly diagnosed and managed diseases in primary care (PC) paediatric practice. Therefore, it is of utmost importance that treatment guidelines for these diseases are correctly implemented, to ensure antibiotics are only prescribed when their use is indicated and adhering to the recommended dose and duration. In the study presented in this article we analysed the degree of adherence to treatment guidelines for APT and AOM by PC paediatricians, as it is widely believed that errors in antibiotic prescribing occur relatively frequently. To this end, we made a retrospective assessment of the appropriateness of treatment for streptococcal APT and suppurative AOM in paediatric services at the PC level in the province of Araba (Basque Country, Spain) over an 18-month period, using as reference the guidelines for the management of these diseases published by the Asociación Española de Pediatría (AEP, Spanish Association of Pediatrics).
MATERIAL AND METHODS
We designed a retrospective observational study of anonymised data collected from electronic health records, after obtaining consent, dividing patients in 2 groups: patients with a diagnosis of streptococcal AP and patients with a diagnosis of suppurative AOM. Cases were selected using the codes of the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10). The codes used for suppurative AOM were H66011 (suppurative AOM, right ear), H66012 (suppurative AOM, left ear), H66013 (bilateral suppurative AOM) and H66019 (suppurative AOM, unspecified ear), and the codes used for streptococcal APT were J020 (streptococcal pharyngitis) and J0300 (acute streptococcal tonsillitis). The age range in both groups was 0 to 14 years. The included patients resided in the province of Araba (Basque Country, Spain) and received a diagnosis for either of these diseases between September 1, 2021 and March 1, 2023 (18 month period).
In each group, we assessed the adherence to current treatment recommendations based on the consensus document for the diagnosis and treatment of APT published by the AEP in 20111 (and its update published in 20202) for APT and the consensus document on the aetiology, diagnosis and treatment of AOM published by the AEP in 2012.3
The variables analysed in both groups were: age at diagnosis (in the case of more than 1 episode occurring during the study period, we recorded the age at the time of the earliest diagnosis), sex, most recently recorded weight at time of prescribing, active ingredient of the antibiotic, daily dose, interval between doses, daily dose divided by most recently recorded patient weight, adherence of treatment to guidelines used as the standard of good clinical practice, performance (or lack thereof) of a rapid diagnostic test (RDT) for group A beta-haemolytic Streptococcus (GABHS) in cases of streptococcal APT, collection of exudate and microbial isolation.
To determine whether the age distribution was normal, we used the Kolmogorov-Smirnov test in both groups, and found that the distribution was not normal in either.
RESULTS
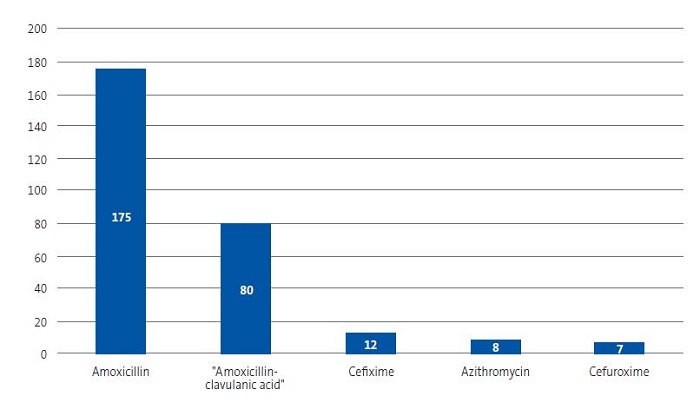
The number of episodes of suppurative AOM initially included in the study was 353, of which 115 had to be excluded from the analysis because of insufficient information. The median age was 4 years (interquartile range, 2-6), with a mild predominance of male patients (male to female ratio, 1.11). The most frequently prescribed oral antibiotic was amoxicillin (n = 175), followed by amoxicillin-clavulanic acid (n = 80) (Figure 1). The antibiotic treatment of 56.7% of the episodes adhered correctly to the treatment guidelines used as reference (135 of the total of 238 cases of suppurative AOM). Underdosing was the main reason that prescribing was inappropriate (82.5%). In 145 cases of suppurative AOM, culture of ear drainage was ordered, with positive isolation in 88.2% (n = 128), and the most frequently isolated pathogen was Haemophilus influenzae (n = 61; 47.6% of the total positive ear drainage cultures), followed by Staphylococcus aureus (n = 21; 16.4% of the total positive ear drainage cultures). Table 1 presents the main results of the analysis of the appropriateness of antibiotic treatment in suppurative AOM.
| Figure 1. Total number of antibiotic prescriptions in cases of suppurative acute otitis media (n = 238) |
|---|
 |

| Table 1. Summary of the results of studies on the appropriateness of antibiotic treatment in acute otitis media and streptococcal acute pharyngitis/tonsillitis in paediatric patients | ||
|---|---|---|
| Suppurative AOM | Streptococcal APT | |
| Total cases under study | 238 analysed episodes (115 excluded due to missing data) | 1721 analysed episodes (295 excluded due to missing data) |
| Total appropriate regimens prescribed | n = 135 | n = 981 |
| Total inappropriate regimens prescribed |
n = 103 82.5% underdosing 7.7% excessive dose 7.7% inappropriate antibiotic |
n = 740 23.1% excessive dose 23.3% too short course 11.2% too long course |
|
AOM: acute otitis media; APT: acute pharyngitis/tonsillitis. |
||

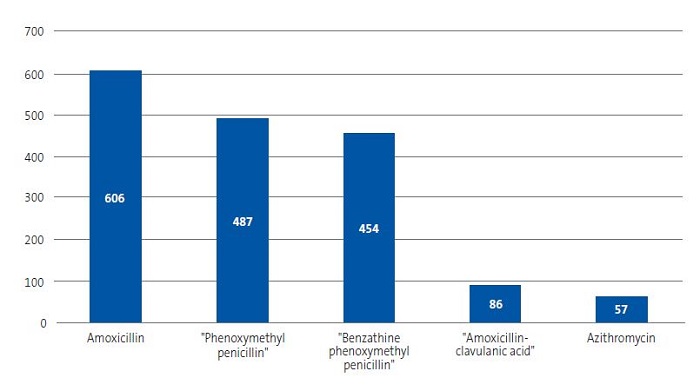
As regards cases of streptococcal APT, 1721 were included in the study analysis, with hardly a difference in frequency based on sex (male to female ratio, 1.08). The median age was 6 years (interquartile range, 5-9). The most frequently prescribed antibiotic was amoxicillin (n = 606; 35% of episodes), which was used at the recommended dose in 74.2% of the episodes. Phenoxymethylpenicillin (n = 487; 28.2%) and benzathine phenoxymethylpenicillin (n = 454; 26.3%) followed in frequency (Figure 2). Phenoxymethylpenicillin was prescribed at an appropriate dose in 99% of cases and benzathine phenoxymethylpenicillin in 81.4%. A RDT for detection of GABHS was performed in 1123 episodes, of which 729 (64.3%) turned out positive. Throat cultures were performed in 833 patients (surprisingly, only in 166 patients with a negative RDT), and the results were positive in 495 cases (59.4%). Of the total episodes of streptococcal APT, 981 (57%) were treated correctly, and the main reasons that prescribing was inappropriate was excessive dose of the active ingredient (23.1%) and shorter than recommended duration (23.3%). Table 1 presents the main results of the analysis of the appropriateness of antibiotic treatment in streptococcal APT.
| Figure 2. Total number of antibiotic prescriptions in cases of acute streptococcal pharyngitis/tonsillitis (n = 1721) |
|---|
 |

DISCUSSION
Acute pharyngitis/tonsillitis is a frequently diagnosed infectious disease in paediatric care, both in PC and hospital emergency settings. The aetiology in the paediatric population is usually viral, but the impact of streptococcal APT is particularly important on account of the potential short- and long-term complications if it is not treated correctly.4,5
When it comes to its management, the use of a clinical rule is recommended to determine whether performance of a RDT for GABHS. For instance, a score of 3 points in the McIsaac score offers a positive predictive value of 28-35% and a score of 4 points a positive predictive value of 51-53%.6,7 The consensus document on APT of the AEP from 2011 recommends performance of a RDT for GABHS if the McIsaac score is 2 points or greater in the absence of manifestations suggestive of viral infection. If there is a high suspicion and the RDT is negative or not available, performance of throat culture is recommended.1,8 The Asociación Española de Pediatría de Atención Primaria (AEPap, Spanish Association of Primary Care Paediatrics), on the other hand, recommends performance of a RDT if the patient has a score of 3 or 4 points in the Centor scale.9 As for treatment, penicillin V (potassium or benzathine phenoxymethylpenicillin) and amoxicillin continue to be the first-line antibiotics in 10-day courses, and benzathine phenoxymethylpenicillin can be given as a single daily dose or split in 2 daily doses without affecting the rate of GABHS at the end of treatment.2,10 In the case of poor adherence to oral treatment or vomiting, the best choice is penicillin G benzathine as a single intramuscular dose (which has been established as the first-line treatment in some countries to improve adherence).1,11
Studies on the appropriateness of antibiotic prescribing in APT have yielded contradictory results. An evaluation of antibiotic prescribing conducted at the PC level in the region of Aragon, Spain, in patients aged 0 a 14 years with a diagnosis of upper respiratory tract infection published in 2014, found that the group with the highest proportion managed with antibiotherapy corresponded to patients with APT (75%).12 In 2015, Piñeiro13 reviewed all the discharge reports and diagnostic tests conducted in children aged less than 14 years with a diagnosis of APT in a paediatric emergency department and concluded that the proportion treated with antibiotherapy was 46.3%. All patients who received antibiotherapy had undergone microbiological testing with correct antimicrobial selection, and the duration of treatment and dose interval were appropriate in more than 85% of prescriptions. Ochoa14 carried out a prospective multicentre study in 11 Spanish hospitals published in 2003, and found that the proportion of cases treated with the first-line antibiotic agent for streptococcal APT was low.
A study conducted in the United States analysed 184 032 outpatient visits conducted in 2010 and 2011 using data collected by the Centers for Disease Control and Prevention (CDC), finding that antibiotherapy was prescribed in 12.6% of the visits. Cases of APT were third in terms of antibiotherapy prescribing frequency and the proportion in which prescribing was appropriate was 65.9%.15 Another study assessed appropriateness of antibiotic prescribing in APT between 2014 and 2019 in 3 paediatric emergency departments in Italy and found a reduction in the unnecessary use of broad-spectrum antibiotics after implementation of certain measures.16 Table 2 presents the main findings of these studies of APT.
| Table 2. Summary of studies on the appropriateness of prescribing, results for cases of acute pharyngitis/tonsillitis | |||
|---|---|---|---|
| Study | Setting | Outcomes analysed to assess appropriateness | Results |
| Malo12 | Primary care | Antibiotic (active ingredient) | 63% of APT cases managed with first-line antibiotics |
| Percentage of APT cases managed with antibiotherapy | 75% of APT cases managed with antibiotics | ||
| Piñeiro13 | Hospital ED | Antibiotic (active ingredient) | Appropriate antibiotic selection in 100% |
| Dose | Appropriate antibiotic dose in 100% | ||
| Duration of antibiotherapy | Appropriate duration of treatment in 85.2% | ||
| Ochoa14 | Hospital ED | Percentage of APT cases managed with antibiotherapy | 81.5% of APT cases managed with antibiotherapy |
| Antibiotic (active ingredient) indicated for APT | Appropriate prescribing in 45.2% | ||
| Fleming - Dutra15 | Outpatient | Percentage managed with antibiotherapy | 56.2% of APT cases managed with antibiotherapy |
| Percentage of APT cases managed with antibiotherapy with a positive RDT for GABHS | Positive RDT for GABHS in 65.9% of APT cases managed with antibiotherapy | ||
| Barbieri16 | Hospital ED | Antibiotic (active ingredient) | Percentages varied between centres and semesters |
| Dose | Improvement in antibiotic prescribing after implementation of measures | ||
|
APT: acute pharyngitis/tonsillitis; ED: femergency department; GABHS: group A beta-haemolytic Streptococcus; RDT: rapid diagnostic test. |
|||

When we compared the findings of the aforementioned studies regarding the appropriateness of antibiotic prescribing in streptococcal APT compared to ours, we found frequencies that were slightly smaller in our study (keeping in mind the heterogeneity of the results of the previous studies). A key factor in the assessment of the appropriateness of antibiotic prescribing is the correct documentation of the patient’s weight before but not too far from the date of the prescription. Due to the COVID-19 pandemic, many of the check-ups scheduled in the routine healthy child programme, during which anthropometric measurements are taken, were delayed. In addition, the substantial workloads of PC paediatricians hinder the appropriate documentation of the weight used for the purpose of antibiotic prescribing. Taking this into consideration, the frequency of appropriate prescribing may actually be higher than estimated based on the available data. On the other hand, it is clear that errors in the duration of the antibiotic course can only be interpreted as poor adherence to current guidelines.
Otitis media (OM) is another infectious disease frequently encountered in PC paediatrics.17,18 It chiefly affects children under 5 years and its incidence is greater in developing countries.19 In terms of its aetiology, we ought to underscore the decrease in the frequency of Streptococcus pneumoniae as the leading causative agent due to the inclusion of the pneumococcal conjugate vaccine in the routine immunization schedule.20 The spectrum of otitis media includes 3 forms of disease: AOM, suppurative AOM and chronic suppurative AOM.21 The diagnosis is based on the development of characteristic signs and symptoms (earache, abnormal otoscopy findings and fever or malaise), classifying AOM cases as confirmed or possible based on whether all criteria are met or just some.22 The indication of antibiotherapy depends on the age and history of the patient and the severity of disease, and amoxicillin is currently the first-line treatment.23 The most recent guidelines of the AEP, published in 2023, expand the group of patients in whom watchful waiting with analgesia is indicated for initial management, followed by re-evaluation within a short time period.24
The findings of previous studies regarding the appropriateness of antibiotic prescribing in AOM in paediatric care have also been heterogeneous. Malo12 analysed antibiotic prescribing at the PC level in Aragon over a 1-year period in patients with a diagnosis of AOM and concluded that 72% of cases were treated with antibiotherapy and that appropriate prescribing was infrequent. Croche25 assessed the appropriateness of antibiotic prescribing in the emergency department of a regional hospital in 2013, concluding that 51.9% of prescriptions were inappropriate and that AOM was the disease in which the inappropriate prescribing was most frequent (47.6%). García-Moreno26 analysed the appropriateness of antibiotic prescribing in a paediatric emergency department over a 1-year period in patients with infectious disease. The authors concluded that 49.3% of prescriptions were appropriate, and that inappropriate prescribing was most frequent in patients with AOM (chiefly in those aged less than 2 years), urinary tract infection and acute conjunctivitis. Csonka27 analysed outpatient antibiotic prescriptions in paediatric patients with AOM between 2014 and 2020 in Finland and concluded that antibiotic selection was correct in 80.1% of cases when the prescriber was a paediatrician, 67% when the prescriber was a general practitioner and, strikingly, 55.1% when it was an otorhinolaryngologist. Dube28 analysed the impact of 5 interventions implemented to improve prescribing in terms of the correct duration of antibiotherapy in patients with AOM in the emergency care setting, and found improvements ranging from 39% to 67% in the analysed outcomes. Table 3 presents the main findings of these studies in the management of AOM.
| Table 3. Summary of studies on the appropriateness of prescribing, results for cases of acute otitis media | |||
|---|---|---|---|
| Study | Setting | Outcomes analysed to assess appropriateness | Results |
| Malo12 | Primary care | Correct antibiotic selection | Appropriate in 41% of episodes |
| Croche25 | Hospital ED | Correct antibiotic selection. Dose. Course duration | 47.6% of regimens were inappropriate |
| García Moreno26 | Hospital ED | Correct antibiotic selection. Dose. Course duration | 55% of regimens for AOM were inappropriate |
| Csonka27 | Private outpatient clinics | Correct antibiotic selection | Percentage of appropriate selection stable through time (31.9% in 2014 to 31.3% in 2020) |
| Percentage of AOM cases managed with antibiotherapy. | Reduction in percentage of AOM cases managed with antibiotherapy (From 48.3% in 2014 to 41.4% in 2020) | ||
| Dube28 | Hospital ED | Course duration | 39% of appropriate prescribing at baseline increased to 67% after the implementation of 5 measures to support correct prescribing |
|
AOM: acute otitis media; ED: emergency department. |
|||

When we compared our data on appropriate prescribing to previous studies, the results were similar to the average findings, yet could improve significantly. The main limitation in the assessment of the appropriateness of the dosage involved the correct documentation of the weight of the patient in the records, which, had it been in place, could have led to better results. Another limitation concerned adequate diagnosis and its complexity (especially in the interpretation of otoscopy findings). To avoid potential bias due to the incorrect classification of serous otitis cases as suppurative AOM cases, we decided that the sample would only include patients with a diagnosis of suppurative AOM. Lastly, other limitations worth noting are that we did not verify adequate administration of antibiotherapy (actual consumption of the drug for the prescribed duration of treatment), the retrospective design of the study and the potential for erroneous data in the health records. Despite these limitations, the study also had strengths like the large number of included episodes and the inclusion of episodes through the review of electronic health records, which reduces the heterogeneity in data collection and is more objective.
Lastly, it is important to highlight that this study was conducted in the PC system of Araba, so the results may not be generalised to other geographical areas or to the hospital setting.
CONCLUSION
Analysing the adherence of antibiotherapy to current consensus-based guidelines in paediatric primary care is of utmost importance, as the PC setting is the initial point of contact of the paediatric population with the health care system. Poor adherence in the treatment of diseases for which there is evidence of antibiotic overuse, such as AOM and APT, will have a negative impact in the future in terms of antimicrobial resistance.
Despite the limitations of the study and the flaws in the data that could be improved, it provides a foundation to build on. Last of all, we ought to underscore the crucial importance of correct documentation in the PC electronic health records, to which end paediatricians should be given the necessary tools to facilitate the task, given the considerable workloads that they manage daily, so that in the future there will be more accurate data with which to carry out this kind of large-scale study.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
AUTHORSHIP
Author contributions: design and performance of the study, data analysis, writing and revision of the manuscript (MVM, JTRA), writing and revision of the manuscript, translation of the title, abstract and keywords (BBS), data collection and analysis, statistical analysis (SGGD).
ABBREVIATIONS
AEP: Asociación Española de Pediatría · AEPap: Asociación Española de Pediatría de Atención Primaria · AOM: acute otitis media aguda · APT: acute pharyngitis/tonsillitis · GABHS: group A beta-haemolytic Streptococcus · ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th revision · OM: otitis media · PC: primary care · RDT: rapid diagnostic test.
REFERENCES
- Piñeiro Pérez R, Hijano Bandera F, Álvez González F, Fernández Landaluce A, Silva Rico JC, Pérez Cánovas C, et al. Consensus document on the diagnosis and treatment of acute tonsillopharyngitis. An Pediatr (Barc). 2011;75(5):342.e1-13. https://doi.org/10.1016/j.anpedi.2011.07.015
- Piñeiro Pérez R, Álvez González F, Baquero-Artigao F, Cruz Cañete M, De la Flor I Bru J, Fernández Landaluce A, et al; Grupo Colaborador de Faringoamigdalitis Aguda en Pediatría. Diagnosis and treatment of acute tonsillopharyngitis. Consensus document update. An Pediatr (Barc). 2020;93(3):206.e1-206.e8. https://doi.org/10.1016/j.anpedi.2020.05.004
- Del Castillo F, Baquero Artigao F, De la Calle Cabrera T, López RoblesMV, Ruiz Canela J, Alfayate Miguelez S, et al. Consensus document on the aetiology, diagnosis and treatment of acute otitis media. An Pediatr (Barc). 2012;77(5):345-8. https://doi.org/10.1016/j.anpedi.2012.05.026
- Esposito S, Blasi F, Bosis S, Droghetti R, Faelli N, Lastrico A, et al. Aetiology of acute pharyngitis: the role of atypical bacteria. J Med Microbiol. 2004;53:645-51. https://doi.org/10.1099/jmm.0.05487-0
- Bisno AL, Gerber MA, Gwaltney JM Jr, Kaplan EL, Schwartz RH. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America. Clin Infect Dis. 2002;35(2):113-25. https://doi.org/10.1086/340949
- Pérez R, Pavez D, Rodríguez J, Cofré J. Recommendations for diagnosis and etiological treatment of acute streptococcal pharyngotonsilitis in pediatrics. Rev Chilena Infectol. 2019;36(1):69-77. https://doi.org/10.4067/S0716-10182019000100069
- Engel ME, Cohen K, Gounden R, Kengne AP, Barth DD, Whitelaw AC, et al. The Cape Town Clinical Decision Rule for Streptococcal Pharyngitis in Children. Pediatr Infect Dis J. 2017;36(3):250-5. https://doi.org/10.1097/INF.0000000000001413
- Kalra MG, Higgins KE, Perez ED. Common Questions About Streptococcal Pharyngitis. Am Fam Physician. 2016;94(1):24-31.
- Cubero Santos A, García Vera C, Lupiani Castellanos P. Guía de Algoritmos en Pediatría de Atención Primaria. Faringoamigdalitis. AEPap. 2015 [online] [accessed 31/01/2024]. Available at https://algoritmos.aepap.org/algoritmo/13/faringoamigdalitis
- Nakao A, Hisata K, Fujimori M, Matsunaga N, Komatsu M, Shimizu T. Amoxicillin effect on bacterial load in group A streptococcal pharyngitis: comparison of single and multiple daily dosage regimens. BMC Pediatr. 2019;19(1):205. https://doi.org/10.1186/s12887-019-1582-8
- Martins Moreira Anjos l, Barros Marcondes M, Ferreira Lima M, Lia Mondelli A, Politi Okoshi M. S. Streptococcal acute pharyngitis. Rev Soc Bras Med Trop. 2014;47(4):409-13. https://doi.org/10.1590/0037-8682-0265-2013
- Malo S, Bjerrum l, Feja C, Lallana MJ, Poncel A, Rabanaque MJ. Antibiotic prescribing in acute respiratory tract infections in general practice. An Pediatr (Barc). 2015;82(6):412-6. https://doi.org/10.1016/j.anpedi.2014.07.016
- Piñeiro Pérez R, Hernández Martín D, Carro Rodriguez MA, Casado Verrier E, Reques Cosme R, Carbaño Aguado I. Adecuación del diagnóstico y tratamiento de la faringoamigdalitis aguda a las guías actuales. Rev Pediatr Aten Primaria. 2016;18:317-24.
- Ochoa C, Inglada l, Eiros JM, Solís G, Vallano A, Guerra l. Spanish Study Group on Antibiotic Treatments. Appropriateness of antibiotic prescriptions in community-acquired acute pediatric respiratory infections in Spanish emergency rooms. Pediatr Infect Dis J. 2001;20(8):751-8. https://doi.org/10.1097/00006454-200108000-00007
- Fleming-Dutra KE, Hersh AL, Shapiro DJ, Bartoces M, Enns EA, File Jr TM, et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011. JAMA. 2016;315(17):1864-73. https://doi.org/10.1001/jama.2016.4151
- Barbieri E, De Luca M, Minute M, D´Amore C, Ciofi Degli Atti ML, Martelossi S,et al. Impact and Sustainability of Antibiotic Stewardship in Pediatric Emergency Departments: Why Persistence Is the Key to Success. Antibiotics (Basel). 2020;9(12):867. https://doi.org/10.3390/antibiotics9120867
- Blanco MV, Hamdy RF, Liu CM, Jones H, Montalbano A, Nedved A. Antibiotic Prescribing Patterns for Pediatric Urgent Care Clinicians. Pediatr Emerg Care. 2022;38(9):1538-40. https://doi.org/10.1097/PEC.0000000000002809
- Messina F, Clavenna A, Cartabia M, Piovani D, Bortolotti A, Fortino I, et al. Antibiotic prescription in the outpatient paediatric population attending emergency departments in Lombardy, Italy: a retrospective database review. BMJ Paediatr Open. 2019;3(1):000546. https://doi.org/10.1136/bmjpo-2019-000546
- Monasta l, Ronfani l, Marchetti F, Montico M, Vecchi Brumatti l, Bavcar A, et al. Burden of disease caused by otitis media: systematic review and global estimates. PLoS One. 2012;7(4):36226. https://doi.org/10.1371/journal.pone.0036226
- Ubukata K, Morozumi M, Sakuma M, Takata M, Mokuno E, Tajima T, et al. Etiology of Acute Otitis Media and Characterization of Pneumococcal Isolates After Introduction of 13-Valent Pneumococcal Conjugate Vaccine in Japanese Children. Pediatr Infect Dis J. 2018;37(6):598-604. https://doi.org/10.1097/INF.0000000000001956
- Schilder AG, Chonmaitree T, Cripps AW, Rosenfeld RM, Casselbrant ML, Haggard MP, et al. Otitis media. Nat Rev Dis Primers. 2016;2(1):16063. https://doi.org/10.1038/nrdp.2016.63
- American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113(5):1451-65. https://doi.org/10.1542/peds.113.5.1451
- Lieberthal AS, Carroll AE, Chonmaitree T, Ganiats TG, Hoberman A, Jackson MA, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):964-99. https://doi.org/10.1542/peds.2012-3488
- López Martín D, Piñeiro Pérez R, Martínez Campos l, Ares Álvarez J, De la Calle Cabrera T, Jiménez Huerta I, et al. Actualización del documento de consenso sobre etiología, diagnóstico y tratamiento de la otitis media aguda y sinusitis. An Pediatr (Barc).2023;28(5):362-72. https://doi.org/10.1016/j.anpedi.2023.03.003
- Croche Santander B, Campos Alonso E, Sánchez Carrión A, Marcos Fuentes l, Diaz Flores I, Vargas JC, et al. Adecuación de la prescripción de antimicrobianos en población pediátrica en un servicio de urgencias hospitalario. An Pediatr (Barc). 2018;88(5):259-65. https://doi.org/10.1016/j.anpedi.2017.06.001
- García-Moreno FJ, Escobar-Castellanos M, Marañón R, Rivas-García A, Manrique-Rodríguez S, Mora-Capín A, et al. Adecuación de la prescripción de antimicrobianos en procesos ambulatorios atendidos en Urgencias. An Pediatr (Barc). 2022;96(3):179-89. https://doi.org/10.1016/j.anpedi.2020.11.019
- Csonka P, Palmu S, Paula Heikkilä P, Huhtala H, Korppi M. Outpatient Antibiotic Prescribing for 357,390 Children With Otitis Media. Pediatr Infect Dis J. 2022;41(12):947-52. https://doi.org/10.1097/INF.0000000000003693
- Dube AR, Zhao AR, Odozor CU, Jordan K, Garuba FO, Kennedy A, et al. Improving Prescribing for Otitis Media in a Pediatric Emergency Unit: A Quality Improvement Initiative. Pediatr Qual Saf. 2023;8(1):625. https://doi.org/10.1097/pq9.0000000000000625
Comments
This article has no comments yet.





