Vol. 18 - Num. 72
Originales
Adecuación del diagnóstico y tratamiento de la faringoamigdalitis aguda a las guías actuales
Roi Piñeiro Péreza, Diego Hernández Martínb, Miguel Ángel Carro Rodríguezb, Esther Casado Verrierb, Resurrección Reques Cosmeb, Iván Carabaño Aguadoc
aServicio de Pediatría. Hospital Universitario General de Villalba. Collado Villalba. Madrid. España.
bServicio de Pediatría. Hospital General de Villalba. Collado Villalba. Madrid. España.
cSección de Gastroenterología, Hepatología y Nutrición Pediátrica. Servicio de Pediatría. Hospital Universitario 12 de Octubre. Madrid. España.
Correspondencia: R Piñeiro. Correo electrónico: roi.pineiro@quironsalud.es
Cómo citar este artículo: Piñeiro Pérez R, Hernández Martín D, Carro Rodríguez MA, Casado Verrier E, Reques Cosme R, Carabaño Aguado I. Adecuación del diagnóstico y tratamiento de la faringoamigdalitis aguda a las guías actuales. Rev Pediatr Aten Primaria. 2016;18:317-24.
Publicado en Internet: 23-11-2016 - Número de visitas: 25722
Resumen
Introducción: la faringoamigdalitis aguda (FAA) es una de las enfermedades más comunes en la infancia. El manejo diagnóstico y terapéutico es sencillo y, desde 2011, está consensuado. El objetivo principal es analizar la adecuación al consenso en un hospital de media complejidad, donde trabaja uno de los autores de dicho documento de consenso.
Pacientes y métodos: estudio descriptivo, transversal, unicéntrico y de ámbito local. Se realiza un análisis retrospectivo de los informes de alta y pruebas complementarias en todos los niños ≤ 14 años diagnosticados de FAA en Urgencias Pediátricas. Periodo: del 1 de enero al 31 de diciembre de 2015.
Resultados: se analizan 176 FAA (el 52,3%, niñas). La valoración clínica se realiza siempre mediante la escala de McIsaac. El 46,5% recibieron antibióticos antes de la realización de una técnica de detección rápida de antígeno estreptocócico o cultivo, en todos ellos. El 100% de los antibióticos y dosis prescritas se ajustaron al consenso. Los intervalos de dosis y la duración del tratamiento fueron adecuados en > 85% de los casos. Las prescripciones inadecuadas fueron pautadas por solo dos de los 17 pediatras del hospital.
Conclusiones: la adecuación es superior a lo descrito en otras series. El uso apropiado de antibióticos puede mejorar mediante la formación continuada y regular por parte de pediatras especializados en enfermedades infecciosas. Además, se sugiere que los tratamientos inadecuados se analicen según prescriptor, para seleccionar qué facultativos deben recibir una formación específica. Es prioritario adecuar la prescripción de antimicrobianos en la FAA a la evidencia científica en nuestro país.
Palabras clave
● Streptococcus pyogenes ● Antibióticos ● Faringoamigdalitis ● Niños ● TratamientoINTRODUCCIÓN
En 2011 se publicó el primer documento de consenso nacional sobre el diagnóstico y tratamiento de la faringoamigdalitis aguda (FAA) en niños, con la colaboración de cuatro sociedades científicas pediátricas1. El objetivo principal fue difundir una serie de mensajes clave para los pediatras, médicos internos residentes (MIR) de Pediatría y médicos que atienden a niños. Se especificó que, dada la inespecificidad de los síntomas, sin el empleo de estudios microbiológicos, se tiende al sobrediagnóstico de la FAA estreptocócica, con la consiguiente prescripción innecesaria de antibióticos. Se remarcó además que era urgente y prioritario adecuar la prescripción de antimicrobianos a la evidencia científica en nuestro país.
Durante los últimos años, varios autores han estudiado la adecuación de la prescripción antibiótica en diferentes ámbitos pediátricos de Atención Primaria (AP) y especializada2-6, y también de forma específica en el caso de la FAA en niños7-9 y adultos10,11. Los resultados son dispares, en función del año de estudio y del ámbito analizado. La elaboración de documentos de consenso para el tratamiento de diversas enfermedades infecciosas pediátricas ha demostrado mejoría con respecto a los conocimientos teóricos de los pediatras en nuestro país2, y mejoría en la adecuación antibiótica en países como Francia5 o Italia6, aunque no en un pequeño estudio realizado en nuestro país en adultos11.
El objetivo del presente estudio es analizar la adecuación respecto al diagnóstico y tratamiento de la FAA en niños, utilizando como referencia el consenso nacional1, en un hospital de media complejidad especialmente sensibilizado en el manejo adecuado de la FAA, donde trabaja uno de los autores del citado consenso.
PACIENTES Y MÉTODOS
Estudio descriptivo, transversal, unicéntrico y de ámbito local. Se realiza un análisis retrospectivo de los informes de alta y pruebas complementarias realizadas en todos los niños con una edad ≤ 14 años diagnosticados de FAA en la Unidad de Urgencias Pediátricas, en el periodo del 1 de enero al 31 de diciembre de 2015.
- Criterios de inclusión: niños ≤14 años con juicio diagnóstico al alta codificado, según sistema interno del hospital y basado en la Clasificación Internacional de Enfermedades, décima versión (CIE-10), como: “faringitis aguda”, “amigdalitis aguda”, “fiebre escarlatina” o “angina estreptocócica”.
- Criterios de exclusión: 1) pacientes mal codificados, en los que tras revisar el informe de alta se ha considerado que no se tratan de casos de FAA o escarlatina con FAA; 2) diferencia inferior a una semana entre dos o más diagnósticos de FAA o escarlatina en un mismo paciente, en cuyo caso se agrupó en un solo episodio, y 3) episodios diagnosticados de escarlatina sin asociar FAA.
Se han recogido las siguientes variables: sexo; edad; juicio diagnóstico; fecha del diagnóstico; médico responsable del alta; uso previo de antibióticos; puntuación según escala de McIsaac12; utilización o no de test de detección rápida (TDR) de antígeno estreptocócico y, en su caso, resultados; solicitud o no de cultivo de exudado faringoamigdalar y, en su caso, resultados; prescripción o no de antibióticos al alta y, en su caso, antibiótico seleccionado; dosis pautada; intervalo entre dosis y duración del tratamiento; y presencia de complicaciones durante los seis meses siguientes al diagnóstico.
El análisis descriptivo de las variables cualitativas se concreta mediante el cálculo de las distintas frecuencias relativas. No existen datos cuantitativos puesto que las variables temporales se agruparon por rangos. El análisis de heterogeneidad se realiza mediante test de χ2 o el test exacto de Fisher para frecuencias esperadas menores de cinco. El análisis de los datos se realiza mediante el programa estadístico SPSS® v22.0.
RESULTADOS
En 2015, se atendieron 20 996 urgencias pediátricas. De ellas, 199 fueron codificadas como FAA o escarlatina. Se descartaron 23 según criterios de exclusión: nueve episodios de escarlatina sin FAA, siete codificaciones inadecuadas y siete segundas o terceras consultas por el mismo cuadro durante un periodo menor de siete días.
Se analizaron finalmente 176 FAA (0,84% del total de Urgencias). De ellas, 22 asociaron exantema escarlatiniforme a los signos de FAA; 52,3% eran niñas; 23,9% de edad < 3 años (edad mediana 4,5 años). No existieron diferencias significativas respecto a la estación del año (p = 0,23).
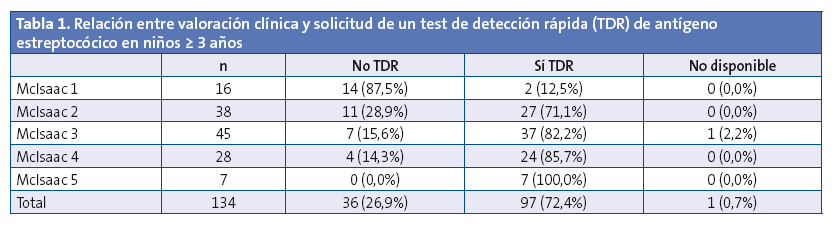
En los 134 niños ≥ 3 años, se realizó la evaluación clínica mediante la puntuación de McIsaac, con un resultado ≥ 2 en el 88,1%. Se solicitó un TDR de antígeno estreptocócico en el 72,4%. En la Tabla 1 se muestra la relación entre dicha petición y la valoración clínica. Se pidió TDR al 81,4% de los niños con una puntuación ≥ 2. Entre los niños con puntuación de McIsaac ≥ 2 en los que no se pidió TDR ni cultivo, en el 75% de los casos el motivo fue que ya estaban siendo tratados con antibióticos, sin realización previa de estudios microbiológicos. De ellos, el 75% había sido prescrito en AP y el 25% en clínicas privadas. Además, dichos antibióticos fueron inadecuados en el 42% de los casos (tres niños con azitromicina y dos con amoxicilina-clavulánico).
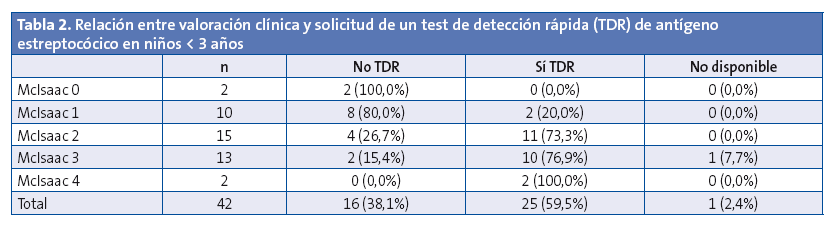
En los 42 niños < 3 años, se solicitó TDR al 59,5%. Aunque a esta edad el consenso1 no especifica que se utilicen criterios de McIsaac, se decidió emplear dicha escala para conocer en qué casos se pidió TDR (Tabla 2). Se solicitó TDR a un 83,3% de los niños con una puntuación ≥ 2.
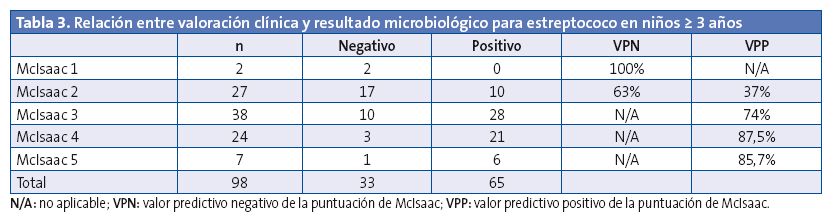
De los 122 TDR solicitados en total, 68 (55,7%) fueron positivos. No se realizó ningún cultivo en los casos positivos. En los casos de TDR negativo, se solicitó cultivo en niños con alta sospecha clínica de FAA estreptocócica, con puntuación de McIsaac ≥ 3, más otros dos casos por no disponibilidad de TDR; 8 de 27 cultivos (29,6%) fueron positivos, todos ellos para estreptococo beta-hemolítico del grupo A (EbhGA). No se aislaron estreptococos de los grupos C ni G. El TDR en niños con McIsaac ≥ 3 presentó un valor predictivo positivo del 70%.
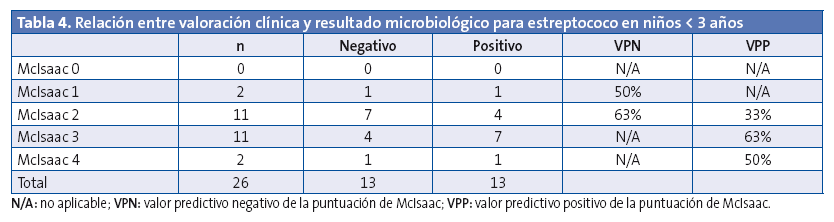
Teniendo en cuenta el resultado microbiológico positivo (TDR o cultivo), se relacionó con la escala de McIsaac (Tablas 3 y 4). Puede comprobarse como ningún corte en la puntuación de McIsaac ofrece resultados aceptables para tomar la decisión de iniciar antibioterapia teniendo en cuenta datos clínicos, tal y como el consenso1 recomienda no hacer.
De los 176 niños, 82 (46,5%) recibieron antibióticos: 64,6% fenoximetilpenicilina, 33% amoxicilina, 1,2% penicilina G benzatina y 1,2% josamicina (por hipersensibilidad conocida a betalactámicos). Es decir, el 100% de los tratamientos prescritos fueron adecuados según consenso1. En 14 niños se inició antibioterapia a pesar de TDR negativo, por decisión del facultativo responsable. De ellos, en los 8 en los que el cultivo fue negativo, se avisó a la familia para retirar el antibiótico.
Las dosis se ajustaron al consenso1 también en el 100%. Respecto a la duración del tratamiento oral, se pautaron diez días al 85,2% de los niños, es decir, lo recomendado según el consenso1. Otras pautas fueron ocho (12,3%) o siete días (2,5%). Al analizar los intervalos de dosis, las pautas fueron inadecuadas en nueve casos (11,1%), administrando penicilina o amoxicilina cada ocho horas, en lugar de cada 12 horas. Se detectó que las pautas inadecuadas fueron prescritas por solo dos facultativos del servicio. La tasa de complicaciones (supurativas locales y no supurativas) fue del 0%.
DISCUSIÓN
La FAA es una de las enfermedades más comunes en la infancia. La etiología más frecuente es vírica. El manejo diagnóstico y terapéutico es sencillo y está consensuado1. Los TDR deben estar disponibles en nuestro país, tanto en AP como en Especializada, y la clínica es la que debe guiar al pediatra para solicitar pruebas microbiológicas, pero no para decidir si se prescriben o no antibióticos. Sin embargo, la literatura médica muestra que el manejo clínico de la FAA se aleja bastante de lo recomendado por la evidencia científica.
Los resultados de una encuesta española13, publicados en 1999, mostraron que el 47,3% de los médicos consideraban el EbhGA como el agente etiológico más frecuente de las FAA, y solo el 20,5% consideraban que la etiología vírica era la más habitual. Además, entre estos últimos, un tercio afirmaba que pautarían antibióticos pese a considerar origen vírico. En esta situación, no sorprenden los resultados de Ochoa7 en 2003, estudio en el que se analizaron 1716 FAA en 11 Servicios de Urgencias Pediátricas españoles. En el 80,9% se prescribieron antibióticos, pero solo en nueve niños (0,5%) se solicitó TDR o cultivo. En los niños de mayores de tres años, el 75,9% recibieron antibioterapia. El 22,8% de las prescripciones se clasificaron como de primera elección (penicilina u otros antibióticos justificados por alergia a betalactámicos), 22,4% de uso alternativo (amoxicilina) y 54,8% inapropiadas (no indicado u otros antibióticos sin antecedente de alergia a betalactámicos).
En 2005, Herranz14 diseñó una encuesta dirigida a los pediatras de AP en Madrid. El 23,6% de los facultativos admitieron que prescribirían antibióticos siempre en la FAA, y el 40,2% que los indicarían con frecuencia. En 2010, Durán3 analizó 100 casos aleatorios de FAA en un Servicio de Urgencias Pediátricas de Barcelona. Se realizaron 60 TDR, siendo positivos el 41,7%. El 36% de las FAA recibieron antibióticos (el 11% amoxicilina-clavulánico, el 30% sin estudio microbiológico previo). En 2012, Fernández8 estudió 563 FAA en Urgencias Pediátricas de cinco hospitales y en 80 consultas de AP. No se especifican datos de confirmación microbiológica. La adecuación no fue mejor que la observada por Ochoa7, pues se prescribieron antibióticos al 75,5% de los niños (78,3% de los < 3 años). El tratamiento se consideró de primera elección en el 43,3% (penicilina o amoxicilina, u otros antibióticos justificados por alergia) e inadecuado en el 56% (no indicado u otros antibióticos sin antecedente de alergia).
En 2014, Malo4 analizó 40 806 FAA en AP en Aragón. Se prescribió antibioterapia al 75%, considerándolo adecuado en el 67% de los casos. Se pautó amoxicilina-clavulánico en el 25% de los casos. Los autores reconocen que los pediatras de dicha comunidad autónoma no usaban habitualmente el TDR. También en 2014, destaca el estudio de Fierro9 en 25 centros de salud, tras analizar 52 658 casos de FAA. Se comprobó que el 50% de los tratamientos inapropiados procedían de un mismo grupo de facultativos, en concreto del 8% de 222 médicos prescriptores. Los autores proponen que las intervenciones dirigidas hacia determinados facultativos podrían mejorar la adherencia a las recomendaciones de la evidencia científica. Aunque existan guías clínicas, parece evidente que algunos médicos no las utilizan. Detectar a dichos profesionales e implementar medidas para corregir prácticas inadecuadas podría mejorar el uso de antibióticos en nuestro país.
El uso de documentos de consenso ha demostrado cierta utilidad. Tal es el caso de Francia5, país donde en 2011 se publicó una guía clínica para el tratamiento de la otitis media aguda. El uso empírico de amoxicilina-clavulánico se redujo un 28,4% y el de cefpodoxima proxetilo un 34,3%. Sin embargo, no se redujo el porcentaje de otitis que recibieron antibióticos. Similares resultados fueron encontrados en Italia6. En nuestro país, Rico-Ferreira11 ha comprobado recientemente la falta de adherencia en adultos a las guías clínicas de FAA, y enfatiza la necesidad de implementar medidas que ayuden a minimizar este problema, así como realizar estudios cualitativos para comprender los motivos de esta inapropiada prescripción antibiótica y crear sistemas de alerta en las historias clínicas electrónicas que permitan actuar sobre aquellos facultativos en los que la prescripción resulta menos adecuada. De igual manera, Malo4 ha señalado que es necesario promover la formación continuada y aumentar la concienciación de los profesionales sanitarios en su responsabilidad como prescriptores. Además, proponen implicar a los padres en el proceso, rectificando falsos y extendidos mitos sobre las enfermedades respiratorias y los beneficios de la prescripción antibiótica.
Las prescripciones inadecuadas de antibióticos contrastan con el conocimiento teórico de los pediatras, según los resultados de la encuesta ABES sobre el uso empírico de antibióticos en niños en España2. Respondieron 1214 pediatras, y el 96% seleccionó penicilina o amoxicilina como tratamiento de elección de la FAA de probable origen bacteriano. El 3,6% eligió amoxicilina-clavulánico y solo el 0,4% azitromicina. Los autores ya reflejaron que, entre las limitaciones del estudio, la encuesta reflejaba solo la selección antibiótica frente a una serie cerrada de opciones, pero no la prescripción real. También definieron un posible sesgo de selección, derivado del procedimiento de captación, ya que la predisposición a contestar vía correo electrónico podría reflejar un perfil de pediatra específico. En cualquier caso, parece evidente que la discrepancia entre los conocimientos teóricos y la prescripción real, en el caso de la FAA, sí existe.
La principal limitación de nuestro estudio es que se han revisado las historias clínicas de forma retrospectiva, por lo que es posible que ciertas características no hayan quedado bien reflejadas en los informes de alta. Además, no en todos los casos de TDR negativo se realizó cultivo, por lo que es posible que algún diagnóstico de FAA estreptocócica haya pasado desapercibido. No obstante, se ha seguido la recomendación del consenso1, que indica recoger cultivo en caso de TDR negativo solo si existe alta sospecha clínica de origen estreptocócico o presencia de factores de riesgo. Otra limitación es la muestra, inferior a la de otros estudios similares y realizada en un solo centro sanitario.
A pesar de dichas limitaciones, los resultados de nuestra serie reflejan una excelente adecuación al consenso1. Solo un 46,3% de los niños recibieron antibióticos, todos tras estudio microbiológico. En el 100% de los tratados, los antimicrobianos fueron apropiados. Con respecto a la duración del tratamiento e intervalos entre dosis, la adecuación fue mayor del 85%. Los tratamientos inapropiados fueron prescritos por solo dos facultativos de los 17 que atendían Urgencias Pediátricas en 2015 en nuestro hospital.
Respecto a la etiología de la FAA, el EbhGA es el responsable del 48,5% de las FAA en niños ≥ 3 años, porcentaje similar aunque discretamente superior al descrito en la bibliografía, y del 31% en < 3 años, porcentaje significativamente superior a lo documentado1. Evidentemente, no es posible descartar cuántos resultados positivos podrían corresponder a niños portadores, pero ante la presencia de una clínica compatible con FAA, el resultado debe ser interpretado como causante de la enfermedad, y la evidencia actual recomienda el inicio de antibioterapia dirigida1.
Estos datos evidencian tres escenarios diferentes, a los que se plantean posibles soluciones. En primer lugar, la situación que ya fue planteada por Malo4 y Rico-Ferreira11. Es muy probable que las actuaciones de formación continuada y concienciación sobre el uso de antibióticos tengan más éxito interviniendo directamente sobre determinados facultativos que utilizando consensos dirigidos a todos los pediatras. Por supuesto, estos consensos deben seguir marcando la pauta a seguir en nuestro país, pero como base teórica de lo que debe y no debe hacerse, sabiendo que muchos médicos no los leerán, y es en ellos sobre los que se debe actuar. Detectar a los facultativos que realizan un uso inadecuado es hoy más fácil con el registro electrónico de las historias clínicas. Se trata de una tarea sencilla que coordinadores de AP, jefes de Servicios de Pediatría y autoridades competentes deberían realizar para mejorar el uso de antibióticos en la FAA en nuestro país. Es un objetivo viable y, teniendo en cuenta la adecuación que existe, prioritario.
En segundo lugar, nuestro servicio no destaca porque todos los pediatras sean expertos en enfermedades infecciosas pediátricas y en concienciación sobre el uso de antibióticos. Sin embargo, forma parte del equipo uno de los autores del citado consenso1, que de forma regular instruye al servicio sobre el correcto manejo de la FAA en niños. Los resultados de nuestra serie muestran que es posible alcanzar la excelencia en el manejo de dicha patología. Correspondería a los especialistas en enfermedades infecciosas pediátricas de cada hospital o área de salud la formación continuada de sus propios compañeros de trabajo. Esta medida también podría ayudar de forma notable en la mejora del uso de antimicrobianos.
En tercer lugar, entre los resultados de nuestro estudio destaca un 31% de etiología estreptocócica en los niños < 3 años. A esta edad, el consenso1 menciona que las FAA estreptocócicas suponen < 10% de los casos y la fiebre reumática es excepcional en países desarrollados. La decisión de tratamiento antibiótico deberá ser individualizada y solo si existe clínica compatible con estreptococosis. Sin embargo, aunque excepcional, la posibilidad de una enfermedad invasiva por EbhGA está bien documentada en neonatos y lactantes pequeños, con una mortalidad que oscila entre el 2-8%. Aunque hay factores de riesgo descritos para desarrollar dicho cuadro, hay casos publicados sin presentar factores predisponentes15. Dada la potencial gravedad de una enfermedad invasiva por EbhGA, quizá sería oportuno plantear una búsqueda más activa de dicho microorganismo en niños < 3 años, guiada por puntuaciones clínicas similares a la de McIsaac12, quien ya ponderó los criterios de Centor según edad, con el objetivo de poder diagnosticar y tratar a estos pacientes sin que la decisión se base en valoraciones individuales de cada pediatra, que como se ha demostrado, se traducen en un aumento no justificado de la prescripción antibiótica.
En resumen, se presenta la adecuación al consenso1 sobre diagnóstico y tratamiento de la FAA en un hospital de media complejidad, con resultados superiores a lo descrito en otras series. Una posible explicación sería la formación continuada y regular por parte de uno de los facultativos de dicho servicio, experto en el manejo de dicha patología y autor del citado consenso. Además, se plantea una posible solución al uso inapropiado de antibióticos en nuestro país, en el caso de la FAA, que se centra en el análisis de las prescripciones inadecuadas y en la formación específica de determinados facultativos. Finalmente, se propone la posibilidad de revisar el consenso de 2011 con respecto al diagnóstico y tratamiento de la FAA en niños < 3 años.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS: AP: Atención Primaria · CIE-10: Clasificación Internacional de Enfermedades, décima versión (en inglés, International Statistical Classification of Diseases and Related Health Problems [ICD]) · EbhGA: estreptococo betahemolítico, grupo A · FAA: faringoamigdalitis aguda · MIR: médico interno residente · TDR: test de detección rápida.
BIBLIOGRAFÍA
- Piñeiro Pérez R, Hijano Bandera F, Álvez González F, Fernández Landaluce A, Silva Rico JC, Pérez Cánovas C, et al. Documento de consenso sobre el diagnóstico y tratamiento de la faringoamigdalitis aguda. An Pediatr (Barc). 2011;75:342.e1-342.e13.
- Piñeiro Pérez R, Calvo Rey C, Medina Claros AF, Bravo Acuña J, Cabrera García L, Fernández-Llamazares CM, et al. Uso empírico de antibióticos en niños en España. Resultados de una Encuesta Pediátrica Nacional 2012 (Estudio ABES). An Pediatr (Barc). 2013;79:32-41.
- Durán Fernández-Feijóo C, Marqués Ercilla S, Hernández-Bou S, Trenchs Sainz de la Maza V, García García JJ, Luaces Cubells C. Calidad de la prescripción antibiótica en un servicio de urgencias pediátrico hospitalario. An Pediatr (Barc). 2010;73:115-20.
- Malo S, Bjerrum L, Feja C, Lallana MJ, Poncel A, Rabanaque MJ. Prescripción antibiótica en infecciones respiratorias agudas en Atención Primaria. An Pediatr (Barc). 2015;82:412-6.
- Levy C, Pereira M, Guedj R, Abt-Nord C, Gelbert NB, Cohen R, et al. Impact of 2011 French guidelines on antibiotic prescription for acute otitis media in infants. Med Mal Infect. 2014;44:102-6.
- Palma S, Rosafio C, Del Giovane C, Patianna VD, Lucaccioni L, Genovese E, et al. The impact of the Italian guidelines on antibiotic prescription practices for acute otitis media in a paediatric emergency setting. Ital J Pediatr. 2015;41:37.
- Ochoa Sangrador C, Vilela Fernández M, Cueto Baelo M, Eiros Bouza JM, Inglada Galiana L, Grupo Español de Estudio de los Tratamientos Antibióticos. Adecuación del tratamiento de la faringoamigdalitis aguda a la evidencia científica. An Pediatr (Barc). 2003;59:31-40.
- Fernández González N, Herrero-Morín JD, Solís Sánchez G, Pérez Méndez C, Molinos Norniella C, Pardo de la Vega R, et al. Variabilidad e idoneidad en el tratamiento antimicrobiano de las faringoamigdalitis agudas pediátricas en Asturias, España. Arch Argent Pediatr. 2012;110:207-13.
- Fierro JL, Prasad PA, Localio AR, Grundmeier RW, Wasserman RC, Zaoutis TE, et al. Variability in the diagnosis and treatment of group a streptococcal pharyngitis by primary care pediatricians. Infect Control Hosp Epidemiol. 2014;35:S79-85.
- Lázaro A, Ochoa C, Inglada L, Eiros JM, Martínez A, Vallano A, et al. Practice variation and appropriateness study of antimicrobial therapy for acute pharyngotonsillitis in adults. Enferm Infecc Microbiol Clin. 1999;17:292-9.
- Rico-Ferreira P, Palazón-Bru A, Calvo-Pérez M, Gil-Guillén VF. Nonadherence to guidelines for prescribing antibiotic therapy to patients with tonsillitis or pharyngotonsillitis: a cross-sectional study. Curr Med Res Opin. 2015;31:1319-22.
- McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE. Empirical validation of guidelines for the management of pharyngitis in children adults. JAMA. 2004;291:1587-95 [Erratum en JAMA. 2005;294:2700].
- Ripoll Lozano MA, Orero González A, Prieto Prieto J. Etiología y tratamiento de elección de las infecciones respiratorias en Atención Primaria. Opinión de los médicos. Aten Primaria. 1999;23:296-300.
- Herranz Jordán B, Pérez Martín C. Encuesta sobre prescripción de antibióticos en infecciones respiratorias pediátricas. Rev Pediatr At Prim. 2005;28:19-40.
- Plana Fernández M, López Gil A, Gomà Brufau AR, Solé Mira E, Bringué Espuny X. Enfermedad invasiva por Streptococcus pyogenes en lactante sano de 38 días. An Pediatr (Barc). 2007;66:540-1.





