Vol. 24 - Num. 95
Original Papers
How is vision screening performed in primary care?
María Prieto Arcea, Mireya Orío Hernándezb, Marcello Belluscic, M.ª Elena Cabezas Tapiad, Manuel Praena Crespoe
aPediatra. CS San Agustín. Burgos. España.
bPediatra. CS Alcalde Bartolomé González. Móstoles. Madrid. España.
cPediatra. Unidad de Enfermedades Metabólicas. Hospital Universitario 12 de Octubre. Madrid. España.
dPediatra. CS de Villaviciosa de Odón. Villaviciosa de Odón. Villaviciosa de Odón. Madrid. España.
ePediatra. CS La Candelaria. Sevilla. España.
Correspondence: M Prieto . E-mail: mprietoar@saludcastillayleon.es
Reference of this article: Prieto Arce M, Orío Hernández M, Bellusci M, Cabezas Tapia ME, Praena Crespo M. How is vision screening performed in primary care? . Rev Pediatr Aten Primaria. 2022;24:e301-e312.
Published in Internet: 11-10-2022 - Visits: 15269
Abstract
Introduction: amblyopia is the most frequent cause of preventable vision loss in developed countries. Its prevention depends on early detection and treatment through adequate vision screening in childhood. Our objective was to describe the current situation in vision screening at the primary care level in Spain and its association with the training of professionals.
Material and methods: observational descriptive study via a remote survey of primary care paediatricians of their knowledge on visual development and vision screening techniques, equipment and training. We conducted a statistical descriptive and univariate analysis to assess the association between the training received and the level of knowledge.
Results: of all respondents, 79.3% answered the theoretical questions correction, 82.8% had standardised optotypes and 30.7% used the Lang test. Also, 72.7% knew the adequate distance and 76.6% the optimal height to assess visual acuity with optotypes. Fifty percent used the red reflex test, 68.3% the Hirschberg test and 44.5% the cover test in the appropriate check-ups. As regards training, 3.1% received it from their institutions, and 54.8% independently. Over 90% knew the criteria for referral to the ophthalmologist. We found differences in the scores of the respondents based on the training received.
Conclusion: we identified opportunities for improvement: the red reflex test should be performed during all infant check-ups and ocular alignment checked from 6 months, and the Lang test and standardised optotypes should be available and their use improved. Higher levels of theoretical and practical knowledge are positively correlated with the amount of training received by health professionals.
Keywords
● Amblyopia ● Strabismus ● Vision screening ● Visual acuityINTRODUCTION
The visual system, consisting of the retina, the optic nerve and the cerebral cortex, which is very immature at birth, undergoes gradual structural and functional development, approaching the adult state around the age of 6 years.1-3
Amblyopia (“lazy eye”) is the most common cause of preventable vision loss in developed countries, affecting 2-5% of the general population.4-7 It is defined as a unilateral or, very rarely, bilateral reduction in visual acuity (VA) that cannot be attributed to a structural impairment of the eye or of the visual pathways, but to abnormal processing of visual images by the brain during the critical period of visual development, giving rise to a functional reduction in VA.1,3
The most frequent cause of amblyopia is strabismus.1 Others are refractive errors (astigmatism, hypermetropia and myopia), nystagmus, and any cause of visual deprivation (such as congenital ptosis, retinoblastoma, congenital cataract or inappropriate occlusion therapy).3,4,7,8
Given that it is a problem of cerebral development, once visual maturation is complete, from the age of 6-8 years, the risk of developing amblyopia disappears and treating it will be less effective or even ineffective from that age. Hence the importance of early detection and treatment.1,7,8
Vision screening is part of health prevention care in children, but it varies greatly with regard to which tests are performed and at what age, as well as to ophthalmology referral criteria.1,3 In newborns and children up to age 2 years, the object of screening is early detection of serious eye problems such as congenital cataract or retinoblastoma,1,9 at preschool age it is to detect amblyopia and the risk factors for its development, and at school age, reduced VA due to refractive errors.1
There are few studies that analyse the state of vision screening in primary care in Spain, and the available evidence does not allow us to establish the best time to begin screening, nor which tests are the most suitable to avoid a visual problem going unnoticed, on the one hand, and unnecessary referrals, on the other.
Our objectives are to describe knowledge of visual development and screening techniques among primary care paediatricians (PCPs) in Spain, as well as the availability of basic material and training needed to carry out a proper vision screening. We also aim to analyse the existing relationship between the training received by professionals and their level of basic knowledge, correct performance of the screening tests and appropriate ophthalmology referral.
MATERIALS AND METHODS
We designed a descriptive cross-sectional observational study, through a voluntary, non-remunerated survey, distributed online from 09/03/2020 to 26/04/2020.
Participants were recruited through the membership list of the Spanish Association of Primary Care Paediatrics (AEPap), specifying that only paediatricians and general practitioners working in primary care (PC) should answer the survey.
A questionnaire (Appendix 1) was designed, based on the recommendations of Previnfad (2016),1,10 AEPap (2020),4,11 the American Academy of Pediatrics, the American Academy of Ophthalmology, the American Association for Paediatric Ophthalmology and Strabismus and the American Association of Certified Orthoptists (2016).12,13 It consisted of 18 questions, of which seven explored theoretical knowledge, one concerned the professional responsible for vision screening, one the training received, two the availability of materials, five the correct performance of screening techniques and two appropriate referral to an ophthalmologist.
According to Ministry of Health data, in 2018 there were 6448 professional PCPs in Spain, from which a sample size of 261 professionals was calculated, for a confidence level of 90% and a margin of error of 5%.
Statistical analysis: the data obtained were subjected to descriptive analysis, on the one hand, and to univariate analysis, on the other, to assess the association between the training received by the professionals and correct theoretical knowledge and clinical practice. We analysed differences between categorical variables with the χ2 test and differences in the mean scores of each group with the ANOVA test for independent variables. A p value of less than 0.05 was considered significant.
RESULTS
We received the 304 questionnaires, of which 14 were excluded due to incomplete responses, so that 290 professionals were included in the study.
Of this total, 18.3% reported performing vision screening themselves, 16.9% that it was performed by nurses, and 64.8% both. Only 3.1% reported that having received formal training, that is, of a regular and institutional nature, while 54.8% had trained on their own, 23.8% had not received any training and 18.3% did not know this information.
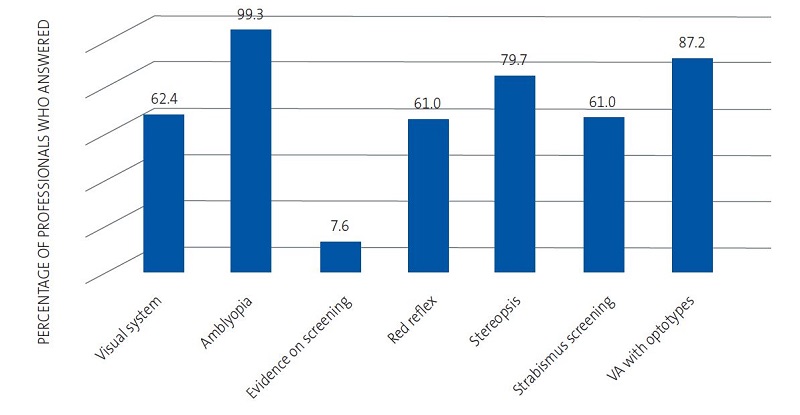
Of the seven theoretical questions, 2.1% of the participants gave the correct answer to all of them, 20.3% to 6, 30.3% to 5, 26.6% to 4, 15.9% to 3, 4.5% to 2, nobody answered only one correctly and the remaining 0.3% answered all the questions incorrectly. In all, 79.3% gave the right answers to more than half the questions asked (at least 4 of 7). The percentage of professionals that answered each theoretical question correctly is shown in Figure 1.
As regards the material used, 32.8% of the professionals had the Lang test and 25.9% used it routinely from 2 years of age, 4.8% only when VA could not be explored with optotypes due to lack of cooperation from the child, and 2.1% did not consider it useful. A total of 82.8% answered that they had standardised optotypes available, 10.3% that they did not, 4.1% only some days, and 2.8% did not know what kind of optotypes they used.
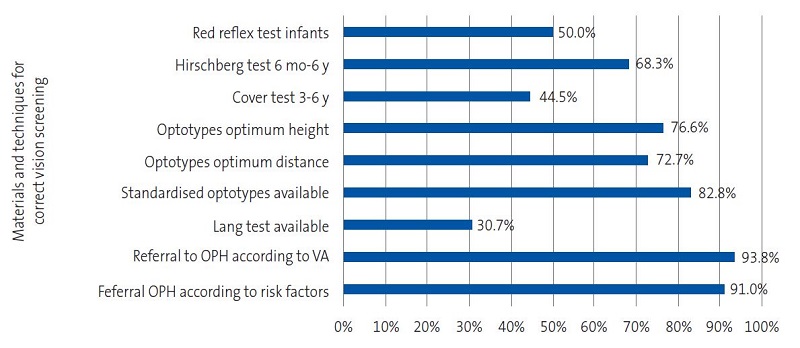
As for screening tests, 50% performed the red reflex test in all infants, 26.2% only up to age 6 months, 21.4% up to age 1 month, and 2.4% did not perform it. The Hirschberg test was performed by 68.3% in all examinations from 6 months to 6 years of age, 24.8% in all examinations regardless of age, 5.9% only from 3 years and 1% exclusively at the age of 6 years. A total of 44.5% used the cover test in examinations between the ages of 3 and 6 years, 32.4% in all examinations from 6 months, 16.9% only when the Hirschberg test was pathological, and 6.2% did not use it. To explore VA with optotypes, 72.7% placed the child at the distance in metres marked by the last row of optotypes and 76.6% put the optotypes in the child’s horizontal plane of vision (Figure 2).
The criteria for ophthalmology referral from PC according to risk factors for visual disorders and results of vision screening were known to 91% and 93.8% of the professionals respectively (Figure 2).
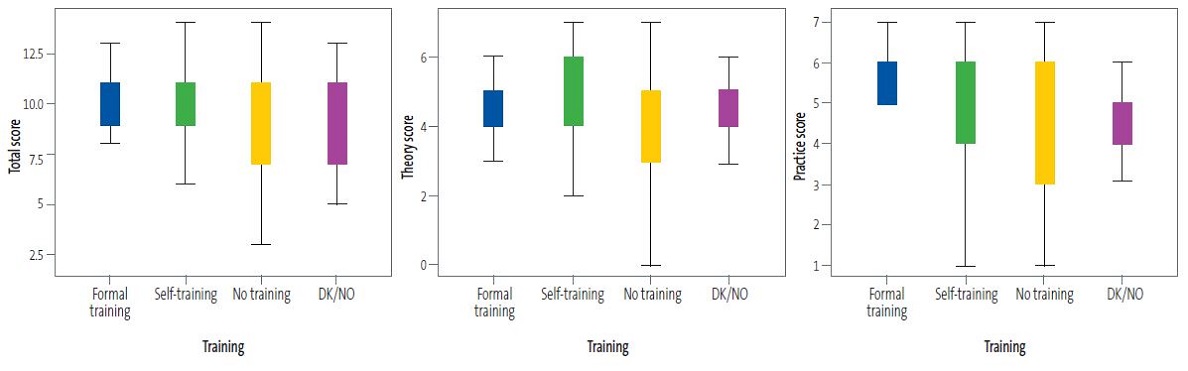
We analysed the relationship between the type of training received by the professionals, distinguishing 4 groups (formal training, self-training, don’t know/no opinion [DK/NO], no training), and their theoretical knowledge, correct performance of the screening tests and referral to an ophthalmologist, analysing the mean score of correct answers to 14 questions in the questionnaire (7 theoretical and 7 practical). We observed statistically significant differences on account of the performance in the practical section (Table 1 and Figure 3).
| Table 1. Mean theoretical, practical and total scores according to the training received by the doctors | ||||
|---|---|---|---|---|
| N | Mean ± SD | p | ||
| Theory score |
Formal training Self-training No training DK/NO Total |
9 159 69 53 290 |
4.67 ± 1.32 4.60 ± 1.16 4.41 ± 1.38 4.47 ± 1.07 4.53 ± 1.20 |
0.668 |
| Practice score |
Formal training Self-training No training DK/NO Total |
9 159 69 53 290 |
5.44 ± 1.73 5.18 ± 1.14 4.52 ± 1.44 4.68 ± 1.27 4.94 ± 1.26 |
0.001 |
| Total score |
Formal training Self-training No training DK/NO Total |
9 159 69 53 290 |
10.11 ± 1.45 9.78 ± 1.79 8.93 ± 2.32 9.15 ± 1.98 9.47 ± 1.98 |
0.009 |

When we analysed the questions separately, we found statistically significant differences between the groups of doctors, based on their training, in the number of right answers to the questions on the optimum distance for testing of VA with optotypes (p = 0.037) and ophthalmology referral criteria according to the result of vision screening (p = 0.010) (Tables 2 and 3).
| Table 2. Correct answers to questions on theory according to the training received by the doctors | |||||||
|---|---|---|---|---|---|---|---|
| Formal training | Self-training | No training | DK/NO | Total | p | ||
| Theoretical question 1. Visual system | Correct |
6 66.7% |
100 62.9% |
39 56.5% |
35 66% |
180 62.1% |
0.71 |
| Incorrect |
3 33.3% |
59 37.1% |
30 43.5% |
18 34% |
110 37.9% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Theoretical question 2. Amblyopia | Correct |
9 100% |
158 99.4% |
67 97.1% |
53 100% |
287 99% |
0.36 |
| Incorrect |
0 0.0% |
1 0.6% |
2 2.9% |
0 0.0% |
3 1% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Theoretical question 3. Evidence on vision screening | Correct |
2 22.2% |
8 5% |
7 10.1% |
4 7.5% |
21 7.2% |
0.169 |
| Incorrect |
7 77.8% |
151 95% |
62 89.9% |
49 92.5% |
269 92.8% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Theoretical question 4. Red reflex | Correct |
4 44.4% |
105 66% |
38 55.1% |
30 56.6% |
177 61% |
0.242 |
| Incorrect |
5 55.6% |
54 34% |
31 44.9% |
23 43.4% |
113 39% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Theoretical question 5. Stereopsis | Correct |
8 88.9% |
119 74.8% |
54 75.5% |
40 75.5% |
221 76.2% |
0.768 |
| Incorrect |
1 11.1% |
40 25.2% |
15 21.7% |
13 24.5% |
69 23.8% |
||
|
Total |
9 | 159 | 69 | 53 | 290 | ||
| Theoretical question 6. Screening for strabismus | Correct |
5 55.6% |
97 61% |
41 59.4% |
34 64.2% |
177 61% |
0.939 |
| Incorrect |
4 44.4% |
62 39% |
28 40.6% |
19 35.8% |
113 39% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Theoretical question 7. VA testing | Correct |
8 88.9% |
145 91.2% |
58 84.1% |
41 77.4% |
252 86.9% |
0.062 |
| Incorrect |
1 11.1% |
14 8.8% |
11 15.9% |
12 22.6% |
38 13,1% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||

| Table 3. Correct answers to questions on practice according to the training received by the doctors | |||||||
|---|---|---|---|---|---|---|---|
| Formal training | Self-training | No training | DK/NO | Total | p | ||
| Practical question 12. Red reflex | Correct |
3 33.3% |
89 56% |
27 39.1% |
25 47.2% |
144 49.7% |
0.083 |
| Incorrect |
6 66.7% |
70 44% |
42 60.9% |
28 52.8% |
146 50.3% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Practical question 13. Hirschberg test | Correct |
7 77.8% |
115 72.3% |
39 56.5% |
37 69.8% |
198 68.3% |
0.110 |
| Incorrect |
2 22.2% |
44 27.7% |
30 43.5% |
16 30.2% |
92 31.7% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Practical question 14. Cover test | Correct |
3 33.3% |
72 45.3% |
31 44.9% |
21 39.6% |
127 43.8% |
0.812 |
| Incorrect |
6 66.7% |
87 54.7% |
38 55.1% |
32 60.4% |
163 56.2% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Practical question 15. VA optotypes distance | Correct |
9 100% |
121 76.1% |
49 71% |
32 60.4% |
211 72.8% |
0.037 |
| Incorrect |
0 0.0% |
38 23.9% |
20 29% |
21 39.6% |
79 27.2% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Practical question 16. VA optotypes height | Correct |
9 100% |
128 80.5% |
47 68.1% |
38 71.7% |
222 76.6% |
0.056 |
| Incorrect |
0 0.0% |
31 19.5% |
22 31.9% |
15 28.3% |
68 23.4% |
||
|
Total |
9 | 159 | 69 | 53 | 290 | ||
| Practical question 17. Referral to OPH according to risk factors | Correct |
9 100% |
144 90.6% |
60 87% |
48 90.6% |
261 90.0% |
0.618 |
| Incorrect |
0 0.0% |
15 9.4% |
9 13% |
5 9.4% |
29 10.0% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||
| Practical question 18. Referral to OPH according to examination | Correct |
9 100% |
154 96.9% |
59 85.5% |
47 88.7% |
269 92.8% |
0.010 |
| Incorrect |
0 0.0% |
5 3.1% |
10 14.5% |
6 11.3% |
21 7.2% |
||
| Total | 9 | 159 | 69 | 53 | 290 | ||

DISCUSSION
Performing vision screening correctly requires having the right material, knowing how and when to use it, and knowing the characteristics of the visual system in each stage of childhood, the warning signs, and when to refer patients to a specialist.5
In this study, nearly 80% of the professionals answered more than half the questions on theoretical knowledge correctly. However, only 8% responded correctly to the question related to evidence in vision screening. In this connection, ocular inspection and the red reflex test in newborns and infants do not meet the criteria for being considered as screening tests, since they have not been evaluated prospectively and there are no data available on their validity. However, the impact of potentially serious disorders, such as congenital cataract or retinoblastoma, and the proven effectiveness of each of these interventions to improve their prognosis justify their inclusion in the examinations of newborns and infants.7,10 At preschool age, the object of vision screening is to detect abnormalities during the period of visual development and prevent amblyopia or treat it early if it is already established. Although there are no studies comparing the benefits of screening versus non-screening, its performance between the ages of 3 and 5 years is recommended because there is sufficient evidence on the validity of screening tests and the effectiveness of treating amblyopia in this age range.7,10,14 With regard to children of school age and adolescents, vision screening has low performance in detecting pathology. Testing VA offers a good sensitivity and specificity for the detection of myopia, but is imprecise for detecting hypermetropia and astigmatism. There is no evidence that treating refractive errors in asymptomatic children improves the result compared to treatment initiated after symptoms have appeared, and finding mild refractive errors could cause unnecessary referrals. In conclusion, there is not sufficient evidence to establish a balance between the benefit and risk of screening for refractive errors in schoolchildren and adolescents.7,10
Given the evidence that exists for detection of serious diseases in infants and of amblyopia in children aged 3-5 years, vision screening is one of the preventive activities in primary care paediatrics (PCP).3.1% of the professionals surveyed had received formal training in performing it, 54.8% had self-trained and 23.8% had received no training at all for this purpose. As for the remaining 18.3% who did not know this information, they were probably the same doctors who answered that they themselves did not carry out screening.
In assessing newborns one should ask about risk factors for visual disorders, perform an eye inspection, examine the pupils and test the red reflex.8,12,13. From 3 months, the ability to fix and follow an object should be present.12,13 To examine the red reflex (Brückner test), we focus on each pupil individually with the ophthalmoscope at a distance of 45-75 cm, with the largest circular light and little ambient light, and then on both eyes simultaneously.10,12,13 The red reflex should be bright reddish-orange (light grey in dark-skinned people) and symmetrical in colour, intensity and clarity in the two eyes. Asymmetries, a dull or dim reflex, absence of reflex or a white reflex (leukocoria) are grounds for referral to an ophthalmologist.10 Although testing the red reflex in examinations of newborns and infants is recommended,7,10 only 50% of participants in the study did so.
Stereopsis (binocular vision) develops between 3 and 6 months of life and requires normal development of vision and correct alignment of the two eyes.1 Strabismus and severe ametropias can cause poor stereopsis. This is why a child with adequate depth perception is unlikely to have a serious visual problem.4 There are various tests to evaluate it, and the Lang test is suitable in PC, as it is quick, easy and useful in small children, even 2-year-olds,2,4 but it was only available to 30.7% of the participants in the study.
Eye alignment must be tested in every examination and is especially important up to 6-7 years of age.6,10 Two methods of screening for strabismus are the Hirschberg test and the cover test.15 The first consists of observing the corneal reflex from a light located about 40 cm from the eye, with the patient looking at the light source. The reflex should be symmetrical and centred on the pupil; in children with strabismus it is asymmetrical and decentred in the eye with strabismus.10,13,16. It is a quick test, useful from 6-12 months onwards,2,8,13 which can also detect pseudostrabismus.4,8,10,14 The cover test is more precise15, but more complex, because it requires an experienced examiner and a cooperative patient, which can usually be achieved from the age of 3-4 years.4,8,10 With the child’s gaze fixed on an object, we occlude one eye and observe the behaviour of the uncovered eye. The test is positive if the eye makes a corrective movement to focus on the object. Variants of this test can be used to diagnose phorias (latent strabismus).10,13,15,16 The Hirschberg and cover tests are performed by 68.3% and 44.5% of surveyed doctors in the examinations as indicated.
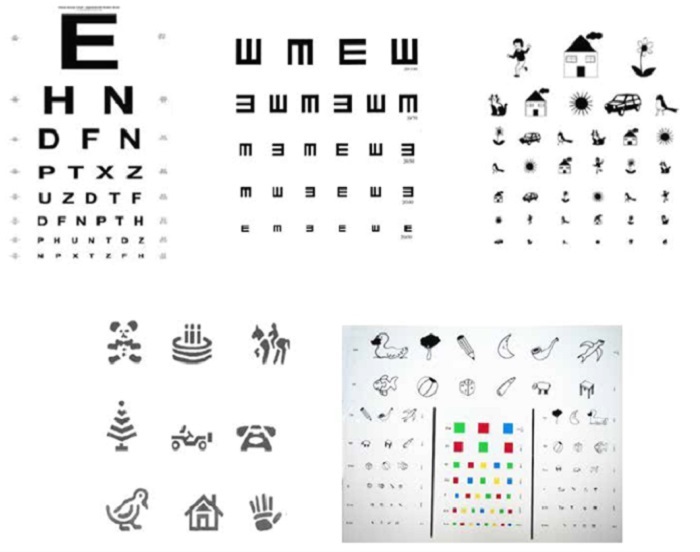
The method of choice for performing vision screening between the ages of 3 and 5 years is direct measurement of VA with standardised optotypes.7 The other tests (Hirschberg test, cover test, Lang test) can supplement, but must not replace, measurement of VA.7,11
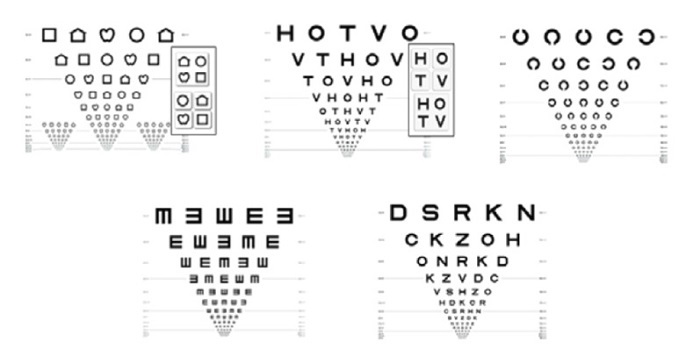
The use of standardised optotypes according to the Bailey and Lovie criteria is currently recommended (Figure 4) because they measure VA more precisely and reliably; however, in regular clinical practice the use of non-standardised optotypes is still very common (Figure 5).7 Optotypes must be placed in the child’s horizontal plane of vision and at the distance marked on the line corresponding to VA of 1,16,17 a practice carried out correctly by 76.6% and 72.7% of the professionals respectively. Each eye is tested separately. Use of the “critical line” is a useful alternative to reading the whole table of optotypes: the child must correctly identify most of the optotypes in the line that they should be capable of seeing at their age.13,17
More than 90% of those surveyed knew the ophthalmology referral criteria10,17 (Tables 4 and 5).
| Table 4. Criteria for referral to ophthalmology in children with risk factors for visual disorders (PrevInfad 2016)10,17 |
|---|
|

| Table 5. Criteria for referral to ophthalmology in children without risk factors (PrevInfad 2016)10,17 | |
|---|---|
| 0-5 months |
|
| 6-35 months |
|
| 3 years* | Monocular visual acuity less than 0.4 logMAR (2/5 Snellen, 0.4 decimal). Should correctly identify most of the optotypes in the 0.4 decimal line. |
| 4 years* | Monocular visual acuity less than 0.3 logMAR (1/2 Snellen, 0.5 decimal). Should correctly identify most of the optotypes in the 0.5 decimal line. |
| ≥5 years* | Monocular visual acuity less than 0.2 logMAR (2/3 Snellen, 0.63 decimal). Should correctly identify most of the optotypes in the 0.63 decimal line. |
|
Any alignment defect or the absence of stereoscopic vision is also a reason for referral. *The frequency of visual disorders is higher in uncooperative children. Between the ages of 3 and 5 years, the impossibility of evaluating VA with optotypes is a reason for referral to the ophthalmologist. |
|

Our results partially differ from those found in one of the few studies published on paediatric vision screening in PC in Spain.5 That study highlights lack of material and ignorance of methodology, visual development, testing required according to age and reasons for referral to ophthalmology on the part of professionals responsible for vision screening. With regard to material, over 80% of the participants in our study answered that standardised optotypes were available to them and nearly a third had the Lang test, compared to a third with age-appropriate optotypes and less than 10% with a test for evaluating stereoscopic vision in the study by Martín et al.5 Nearly 75% of those participating in our study performed VA assessment correctly with optotypes, compared to one third in the aforementioned study. Screening for strabismus was carried out properly by approximately one-third of the professionals in both studies. In ours, the doctors showed a higher level of theoretical knowledge and of ophthalmology referral criteria, which were known to over 90% of the professionals. These differences may be due, in part, to the fact that our survey was aimed solely at doctors; in the study by Martín et al., however, both doctors and nurses participated, and the latter’s knowledge was significantly worse. Moreover, that study was published in 2013, and it is possible that in the years that have elapsed the level of knowledge of professionals, and the provision of material, have improved.
We have not found any studies in Spain that analyse the relationship that exists between the training of professionals and the correct performance of vision screening. Our results show statistically significant differences in the total score to the detriment of the practical part, whereby professionals who had received formal training had the best scores, following by those who had self-trained. The questions on testing VA with optotypes and correct referral to a specialist are those in which these differences were found.
The importance of these results lies in the fact that ophthalmology is one of the specialities to which most patients are referred from PC, both in paediatrics18 and in general practice.19,20 Furthermore, we know that measuring VA with standardised optotypes is the method of choice for performing vision screening between the ages of 3 and 5 years,10,11 and there is sufficient evidence of the validity of screening and the effectiveness of treating amblyopia in that age range.7,10,14 The fact that there is a relationship between performing it correctly and the training received reaffirms the need for formal training aimed at all PCP professionals responsible for vision screening.
As a limitation of this study, we ought to highlight that the sample was obtained consecutively with a non-probability approach and consisted of all the professionals who answered the questionnaire in full, so that it may not have been representative, which may limit the generalisation of the conclusions.
CONCLUSIONS
Testing the red reflex in newborns and infants to screen for serious diseases, having standardised optotypes available and improving the technique of using them, extending the use of the Lang test and optimising tests for detecting strabismus are areas of improvement in vision screening in PC.
Our results support that proper training of professionals contributes to a higher level of theoretical and practical knowledge. Therefore, in addition to the necessary equipment and supplies, training should be provided to those professionals who perform vision screening in PC to optimise early detection of visual problems in childhood and enable timely and appropriate treatment.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
AEPap: Spanish Association of Primary Care Paediatrics. DK/NO: don’t know/no opinion. PC: primary care. PCP: primary care paediatrics/paediatrician; VA: visual acuity.
SUPPLEMENTARY MATERIAL
Appendix 1. Available at: https://pap.es/files/1117-4706-fichero/RPAP_1910_Anexo_encuesta_EN.pdf
REFERENCES
- García Aguado J, Esparza Olcina MJ, Galbe Sánchez-Ventura J, Martínez Rubio A, Mengual Gile JM, et al. Cribado de alteraciones visuales (parte 1). Rev Pediatr Aten Primaria. 2014;16:173-94.
- Marès Bermúdez J, Van Esso Arbolave D. Detección precoz de los trastornos de refracción. Pediatr Integral. 2018;XXII:24-31.
- Solebo AL, Cumberland PM, Rahi JS. Whole-population vision screening in children aged 4-5 years to detect amblyopia. Lancet. 2015;385:2308-19.
- Díez del Corral Belda JM, Álvarez Alonso C. Oftalmología pediátrica para todos los días. In: AEPap (ed.). Congreso de Actualización Pediatría 2020. Madrid: Lúa Ediciones 3.0; 2020. p. 643-55 [online] [accessed 20/09/2022]. Available at www.aepap.org/sites/default/files/documento/archivos-adjuntos/congreso2020/643-656_oftalmologia.pdf
- Martín Martín R, Bilbao Sustacha JA, Colado Cucò A. Cribado visual en Atención Primaria, ¿cómo se realiza? Rev Pediatr Aten Primaria. 2013;15:221-7.
- Méndez Llatas M, Delgado Domínguez JJ. Oftalmología: exploración del niño estrábico; detección precoz. Detección precoz de los trastornos de refracción y ambliopía. Rev Pediatr Aten Primaria. Supl. 2011:163-80.
- García Aguado J. Lo que no puede perder de vista el pediatra (con la vista de los niños…). Rev Pediatr Aten Primaria. Supl. 2017:85-92.
- Loh AR, Chiang MF. Pediatric Vision Screening. Pediatr Rev. 2018;39:225-34.
- Macías Franco S, Rozas Reyes P. Patología congénita ocular. Pediatr Integral. 2018; XXII:6-15.
- García Aguado J, Galbe Sánchez-Ventura J, Martínez Rubio A, Mengual Gile JM, Merino Moína M, Pallás Alonso CR, et al. Cribado de alteraciones visuales (parte 2). Rev Pediatr Aten Primaria. 2015;17:57-67.
- García Aguado J. Guía de Algoritmos en Pediatría de Atención Primaria. Actividades preventivas en Oftalmología. AEPap. 2016 [online] [accessed 20/09/2022]. Available at https://algoritmos.aepap.org/algoritmo/31/actividades-preventivas-en-oftalmologia
- Visual System Assessment in Infants, Children, and Young Adults by Pediatricians. Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology. Pediatrics. 2016;137:28-30.
- Sean P. Donahue, Cynthia N Baker. Procedures for the Evaluation of the Visual System by Pediatricians. Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology. Pediatrics. 2016;137.
- Esparza Olcina MJ. Cribado de alteraciones visuales en niños de uno a cinco años: revisión sistemática para actualizar la recomendación de 2004 de la U.S. Preventive Services Task Force. Evid Pediatr. 2013;9:57.
- Merchante Alcántara M. Estrabismo y Ambliopía. Pediatr Integral. 2013;XVII:489-506.
- García Aguado J, Merino Moína M. Detección de alteraciones visuales en la infancia. Form Act Pediatr Aten Prim. 2011;4:111-5.
- García Aguado J, Sánchez Ruiz-Cabello FJ, Colomer Revuelta J, Cortés Rico O, Esparza Olcina MJ, Galbe Sánchez-Ventura J, et al. Valoración de la agudeza visual. Rev Pediatr Aten Primaria. 2016;18:267-74.
- Contreras Balada N, Gibert Agulló A, Linares Muñoz JM, Ponce Villacreces MC, Casamada Humet N, Sauvalle Soler M. Análisis de las derivaciones a la Atención Especializada desde la consulta de Atención Primaria. Rev Pediatr Aten Primaria. 2015;17:13-20.
- Prado Prieto l, García Olmos l, Rodríguez Salvanés F, Otero Puimed A. Evaluación de la demanda derivada en atención primaria. Aten Primaria. 2005;35:146-51.
- Báez Montilla JM, Sánchez Oropesa A, Garcés Redondo G, González Carnero R, Santos Béjar l, López de Castro F. Motivos y condicionantes de la interconsulta entre atención primaria y especializada. Semergen. 2013;39:89-94.