Vol. 21 - Num. 84
Original Papers
Sleep patterns of healthy children at age four: social factors and parenting styles
Clara M.ª Aymerich de Franchescia, Clara Miguel Miguelb, M.ª Luisa Arroba Basantac, Celina Arana Cañedo-Argüellesd, Luisa Cabello Ballesterose
aSección de Gastroenterología, Hepatología y Nutrición Pediátrica. Hospital Universitario 12 de Octubre. Madrid. España.
bEstudiante de Medicina. Universidad Complutense de Madrid. Madrid. España.
cDepartamento de Salud Pública y Materno-Infantil. Universidad Complutense de Madrid. Pediatra. CS Pozuelo-Emisora. Pozuelo de Alarcón. Madrid. España.
dPediatra. CS Paseo Imperial. Madrid. España.
eTécnico de Salud. Unidad Docente Multiprofesional de Atención Familiar y Comunitaria Noroeste. Madrid. España.
Correspondence: ML Arroba. E-mail: mlarroba@ucm.es
Reference of this article: Aymerich de Franchesci CM, Miguel Miguel C, Arroba Basanta ML, Arana Cañedo-Argüelles C, Cabello Ballesteros L. Sleep patterns of healthy children at age four: social factors and parenting styles. Rev Pediatr Aten Primaria. 2019;21:343-56.
Published in Internet: 31-10-2019 - Visits: 25780
Abstract
Introduction: we conducted a cross-sectional and descriptive study by means of a questionnaire in the paediatrics clinics of the Paseo Imperial and Pozuelo Estación primary care centres in Madrid with the aim of describing the sleep patterns of children born at term currently aged 4 years in 2 urban areas of the Community of Madrid and of analysing potential associations with various variables: parenting history and sleep habits and socioeconomic and family-related factors.
Material and methods: the study included 193 children, of who 111 (57.8%) had abnormal screening results; 94.9% slept 9 or more hours per night. When it came to the parenting history, 89.6% had been breastfed, 51.8% for more than 6 months, and 28.5% had coslept with parents. At the time of the study, 51% shared a room with siblings, while 9.9% slept with parents. Also, 57.8% use electronic devices for sleep induction.
Results: we found higher percentages of possible sleep disturbances in only children, children not attending a childcare centre, currently sleeping with parents, that engaged in reactive cosleeping or used electronic devices after dinner.
Conclusions: the prevalence of warning signs of sleep disorders was high, and given the long-term repercussions of these problems, it is important to have in place an adequate screening protocol to identify children with potential disturbances. Adequate awareness of identified associations would allow paediatricians to deliver educational interventions to susceptible families in order to prevent or resolve sleep abnormalities.
Keywords
● Parenting ● Sleep ● Surveys and questionnairesINTRODUCTION
Sleep problems in children are a frequent reason for consultation in primary care paediatrics clinics and cause anxiety to parents. Between ages 3 and 5 years, children sleep between 10 and 12 hours and naps are considered normal until age 3 or 4 years.1 It is estimated that 30% of children aged less than 5 years have some form of sleep disturbance.1 The reason for this high prevalence is that the calculation includes sleep disorders and problems sleeping, 1 sleep patterns that are considered inadequate by the parents, the child or the paediatrician in the absence of abnormalities in the physiological process of sleep1 that are therefore subjective perceptions influenced by culture2,3: a study conducted in 2010 reflects that parents of Asian children are more likely to believe their children have difficulty falling asleep and that they have a poor sleep quality compared to Caucasian parents.4
Sleep deprivation affects behaviour, mood and cognitive functioning.1 It is estimated that 10% of learning difficulties in children are caused by daytime fatigue.5,6 Sleep deprivation is also associated with obesity and insulin resitance7; 30-minute changes in sleep duration can have an impact on health.8
Multiple articles in the literature analyse sleep disturbances, but there are few studies assessing sleep in healthy children and the factors related to sleep quality.9 Twin studies have shown that environmental factors have a greater impact compared to genetic factors.1,2 Some of the risk factors for developing poor sleep habits identified in the literature include overly permissive or overly strict parental attitudes, prolonged breastfeeding to induce sleep and reactive cosleeping.1,10 It appears that children allowed to do reactive cosleeping go to bed later, have night awakenings at later hours and a shorter sleep duration compared to children that sleep alone.1,10 Another factor to consider is the use of electronic devices: the authors of a study conducted in Italy estimated that 39.1% of children aged 1 to 3 years used these devices before going to bed.1,5 This type of use reduces the total duration of sleep by about 0.25 hours due to a reduction in melatonin levels caused by exposure to the light emitted by these devices.5 The use of electronic devices is also associated with irregular bedtimes.11
When it comes to the association with the sociocultural context, a study in English children aged 3 years found better sleep hygiene behaviours and bed times in families with high socioeconomic status.2 These factors result in a longer duration of night-time sleep, but not in the overall sleep duration, as shorter night-time sleep can be compensated by longer daytime napping.2,5 A study conducted in 29 287 Asian and Caucasian children described cross-cultural differences in sleep habits and parental perception of sleep problems.4 A comparison of the non-Hispanic white and black residents of the same geographical area (southern Mississippi) suggested that night-time sleep duration is shorter in black children compared to white children, but that the former nap more during the day.12
The type of residential setting is another factor to consider. A study in the United States found that sleep duration is shorter in children residing in urban areas compared to children residing in non-urban areas.13
Culture and environment are important in the understanding and assessment of sleep duration and patterns,14 but few such studies have been conducted in the population residing in Spain.
On the subject of sleep disorders, environmental factors have been highlighted as the main causes of behavioural insomnia, or poor sleep due to inadequate sleep hygiene. The family structure has a significant impact on behavioural insomnia, for instance, the continuous absence of one of the parents, conflict between parents and children and young mothers with symptoms of depression.1,2,15 Other sleep disorders have a more complex aetiology in which environmental factors play a lesser role, with a stronger influence of biological factors such as the genetic makeup of the individual, circadian rhythm disorders and other factors associated with sex and age.1
The main aim of this study is to describe the sleep pattern of children born at term and aged 4 years in 2 urban areas in the Community of Madrid, and to analyse potential associations with different variables: parenting style and sleep habits and socioeconomic and family factors.
This study was motivated by the lack of data, overall and in the scientific literature, on the subjects under study, in addition to the substantial prevalence of sleep disorders and the significant impact of the latter on children and their families. Knowledge of the factors associated with sleep disturbances would allow identification of at-risk groups and the implementation of effective preventive measures.
MATERIALS AND METHODS
We conducted an observational descriptive study at the primary care level in the primary care centres of Paseo Imperial and Pozuelo of the Community of Madrid (Spain).
The population under study were children between their fourth and fifth birthdays that visited the participating primary care centres, met the inclusion criteria and none of the exclusion criteria and accepted to participated, enrolled consecutively until the desired sample size was achieved.
The criteria applied were the following:
- Inclusion criteria: children of either sex born to term in the catchment area of the Pozuelo Estación or Paseo Imperial primary care centres; that were 4 years old by the time of enrolment but aged less than 5 years and that sought paediatric care for any reason, consent of one parent to participate in the study.
- Exclusion criteria: preterm birth; neurodevelopmental disorders; need for medication that could alter or interfere with normal sleep maturation (anticonvulsants or melatonin); adoptees, children brought to the facility by a person other than a parent, language barrier.
We calculated the sample size needed for a 95% confidence level and a precision of 7% with an expected prevalence of sleep disturbances of 50% (worst case scenario, p = 0.5), finding that we needed to recruit approximately 196 patients.
We collected data on the following variables:
- Demographic characteristics and socioeconomic status of household: patient sex; maternal and paternal region of origin; current maternal and paternal age (in years); maternal and paternal educational attainment; current maternal and paternal employment status; household composition; current number of children in the household; characteristics of siblings and birth order of patient.
- Variables related to the personal health history, parenting style and sleep habits: breastfeeding, duration of breastfeeding (in months); age that the child stopped sleeping in the parents’ room; location where the child slept within parents’ room; room where the child was sleeping at the time of the study; approach to sleep when the child was a baby; age when the child stopped napping (in years); attendance to child care centres; sleeping in parental bed at least part of the night; use of electronic devices (television, tablet, smartphone) after dinner; reading before bed; need of parental presence to fall asleep.
- Primary outcomes: screening of sleep disturbances by means of the validated version in Spanish of the Bedtime problems, Excessive daytime sleepiness, Awakenings during the night, Regularity and duration of sleep, Snoring questionnaire (BEARS) (Table 1); current sleep duration.
| Table 1. Assessment tool for sleep problems in the paediatric population: BEARS scale, age 2-5 years | |
|---|---|
| 1. Bedtime problems | Does your child have any problems going to bed or falling asleep? |
| 2. Excessive daytime sleepiness | Does your child seem overtired or sleepy a lot during the day? Does your child still take naps? |
| 3. Awakenings during the night | Does your child wake up a lot at night? |
| 4. Regularity and duration of sleep | Does your child have a regular bedtime and wake time? What are they? |
| 5. Snoring | Does your child snore a lot or have difficulty breathing at night? |

Before starting to collect data, we conducted a pilot survey to assess the comprehensibility and validity of the Spanish adaptation of the questionnaire.
We entered the collected information in a database and analysed it with the software SPSS version 21. We performed a descriptive analysis of all the variables to detect abnormal values or other inconsistencies. We have described these variables with the statistics most fitting their nature, type and measurement scale: percentages for qualitative variables and central measure and dispersion statistics as applicable for qualitative variables. In the bivariate analysis, we used the χ2 test or Fisher exact test to compare qualitative data and compared means for quantitative data. We set a significant level of 0.05 for all tests.
Ethical considerations. Informed consent
We did not enter any identifiable information on the study participants in the database.
We informed all participants of the objectives of the study and the identity of the researchers (medical students) and requested their participation. The questionnaire was completed on an anonymous basis and we did not access patient health records to collect personal or clinical data.
The medical students were overseen by the paediatrician in charge of the clinic at all times (Order SSI/81/2017 of 19 January, by which students and residents in any of the health sciences have the duty to guarantee and safeguard the right to privacy of the patient). The questionnaires were administered and reviewed by the paediatricians of the participants.
We adhered to international regulations on data protection as well as current Spanish law (Organic Law 15/1999 of December 13 on the Protection of Personal Data, BOE 298 of December 14, 1999). The study was approved by the Clinical Research Ethics Committee of the Hospital Clínico San Carlos (internal project file number, 17/450-E_TFG) and the Local Research Committee of the Northeast Area of the Primary Care Administration of the Public Health System of Madrid (project file number, 06/2017).
RESULTS
Descriptive analysis of the sample under study
The study included 193 children (100 boys and 92 girls) in the paediatric caseloads of the Paseo Imperial (52.3%) and Pozuelo Estación (47.7%) primary care centres.
The median age of mothers was 39 years (23-49 years) and the median age of fathers was 40 years (24-61 years), with no significant differences between the caseloads of each of the 2 centres.
Tables 2 and 3 summarise the findings for qualitative variables.
| Table 2. Description of socioeconomic variables | |||||
|---|---|---|---|---|---|
| Variable | n | Answer | Frequency | % | |
| Parental country of origin | Mother | 193 | Spain | 170 | 88.1% |
| Not Spain | 23 | 11.9% | |||
| Father | 192 | Spain | 166 | 86.5% | |
| Not Spain | 26 | 13.6% | |||
| Parental educational attainment | Mother | 193 | Primary school | 1 | 0.5% |
| Secondary school | 24 | 12.4% | |||
| University | 168 | 87% | |||
| Father | 190 | Primary school | 5 | 2.6% | |
| Secondary school | 38 | 20% | |||
| University | 147 | 77.4% | |||
| Parental employment | Mother | 192 | Employed | 152 | 79.2% |
| Unemployed | 17 | 8.9% | |||
| Homemaker | 20 | 10.4% | |||
| Other | 3 | 1.6% | |||
| Father | 189 | Employed | 186 | 98.4% | |
| Unemployed | 0 | 0% | |||
| Homemaker | 2 | 1.1% | |||
| Otros | 1 | 0.5% | |||
| Family structure | 192 | Nuclear | 176 | 91.7% | |
| Single parent | 10 | 5.2% | |||
| Extended family | 3 | 1.6% | |||
| Other | 3 | 1.6% | |||

| Table 3. Description of parenting history and current sleep habits | ||||
|---|---|---|---|---|
| Variable | n | Answer | Frequency | % |
| Sibling order | 192 | Only child | 38 | 19.8% |
| First child | 61 | 31.6% | ||
| Middle child | 19 | 9.9% | ||
| Youngest child | 74 | 38.5% | ||
| Breastfeeding | 192 | Never | 20 | 10.4% |
| ≤6 months | 83 | 43.2% | ||
| >6 months | 89 | 46.2% | ||
| Age until which child slept in parents’ room | 193 | Never did | 4 | 2.1% |
| To 1 year (0-12 m) | 121 | 62.7% | ||
| To 2 years (24-36 m) | 39 | 20.2% | ||
| To 3 years (24-36 m) | 9 | 4.7% | ||
| To 4 years (36-48 m) | 2 | 1% | ||
| Still sleeping in parents’ room | 18 | 9.3% | ||
| Place where child slept in parents’ room | 193 | Separate crib | 134 | 69.4% |
| Bedside crib | 22 | 11.4% | ||
| Parental bed | 20 | 10.4% | ||
| Crib and parental bed | 13 | 6.7% | ||
| Never did | 4 | 2.1% | ||
| Method to get child to sleep | 191 | Held in arms or rocking | 100 | 52.4% |
| Alone | 70 | 36.6% | ||
| Other | 21 | 11% | ||
| Attendance to childcare centre | 193 | Yes | 162 | 83.9% |
| No | 31 | 16.1% | ||
| Type of room where the child currently sleeps | 192 | Own room | 74 | 38.5% |
| Shared with sibling | 98 | 51% | ||
| Shared with parents | 19 | 9.9% | ||
| Shared with other | 1 | 0.5% | ||
| Sleeps in parental bed part of the night | 193 | Always | 12 | 6.2% |
| Usually | 12 | 6.2% | ||
| Occasionally | 81 | 42% | ||
| Never | 88 | 45.6% | ||
| Use of electronic devices after dinner | 192 | Always | 7 | 3.6% |
| Usually | 25 | 13% | ||
| Occasionally | 79 | 41.1% | ||
| Never | 81 | 42.2% | ||
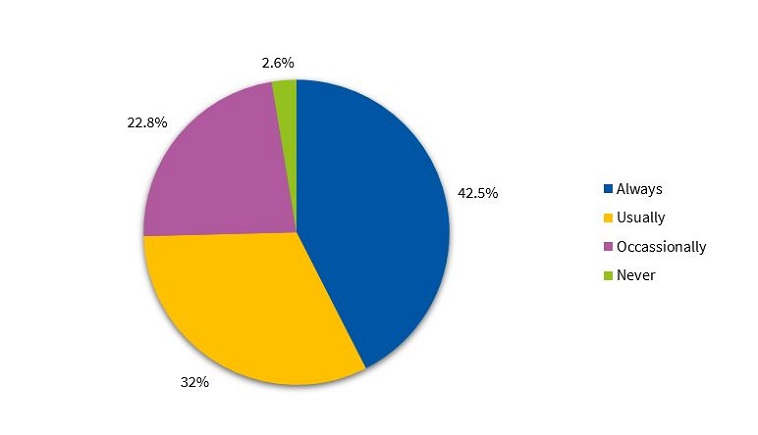
| Reading before bed | 193 | Always | 82 | 42.5% |
| Usually | 62 | 32.1% | ||
| Occasionally | 44 | 22.8% | ||
| Never | 5 | 2.6% | ||
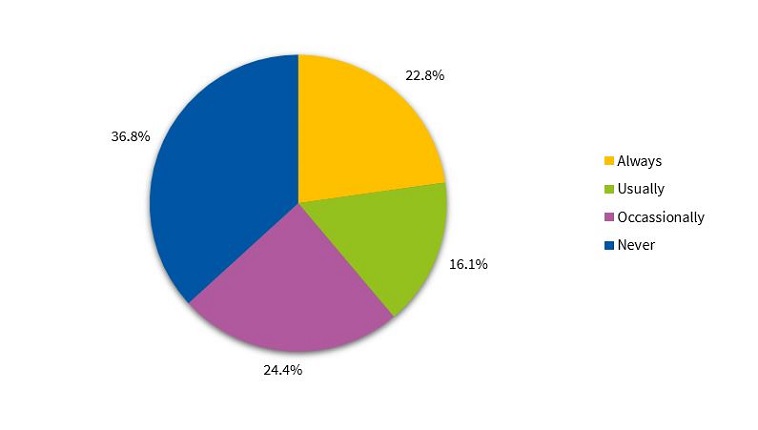
| Needs presence of a parent to fall asleep | 193 | Always | 44 | 22.8% |
| Usually | 31 | 16.1% | ||
| Occasionally | 47 | 24.4% | ||
| Never | 71 | 36.8% | ||
| Duration of night-time sleep | 193 | <9 hours | 10 | 5.2% |
| 9-10 hours | 114 | 59.1% | ||
| >10 hours | 69 | 35.8% | ||

As for socioeconomic characteristics, most parents in the study were Spanish (87.3%), had a university degree and were actively employed. The most frequent family structure was the nuclear family (91.7%). In addition, 20.7% of households had a single child, 53.4% 2 children, 18.1% 3 children and 6.4% had 4 or more children.
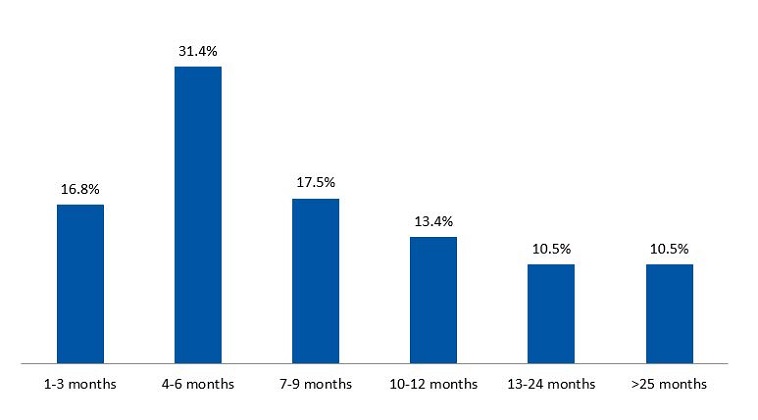
As for parenting variables, we found that 89.6% of children were breastfed, and that breastfeeding duration was longer than 6 months in 51.8% (Figure 1). Most children had slept in a separate crib in the parents’ room in the early years (69.4%), and 28.5% of parents practiced cosleeping. When it came to the approach used to put the child to bed, 52.2% of children fell asleep in a parent’s arms or being rocked, while 36.6% fell asleep on their own. We found that 83.9% attended a childcare centre.
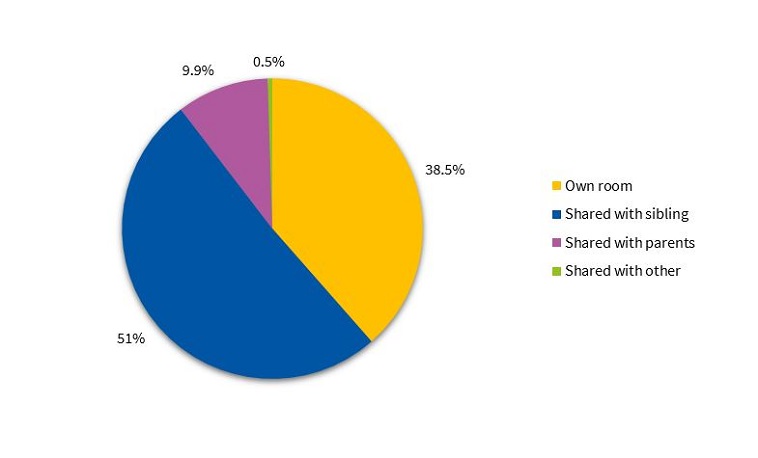
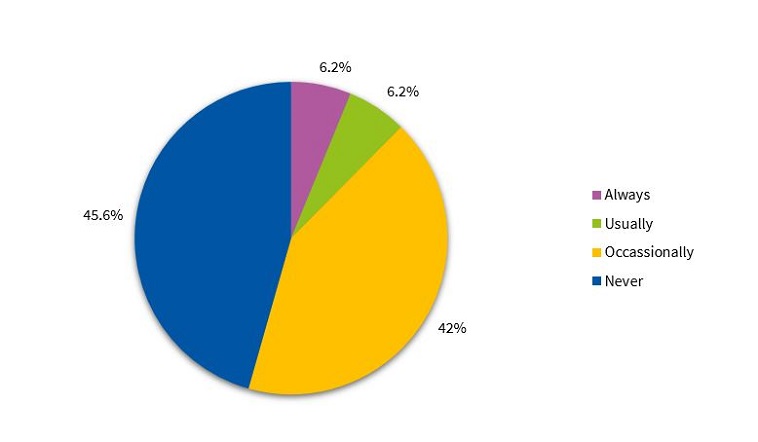
Our analysis of current sleep habits showed that a majority of children shared the bedroom with at least 1 sibling (51%), while 9.9% continued to share the bedroom with their parents (Figure 2). In addition, 45.6% never went to the parental bed during the night, whereas 42% did so on occasion (Figure 3).
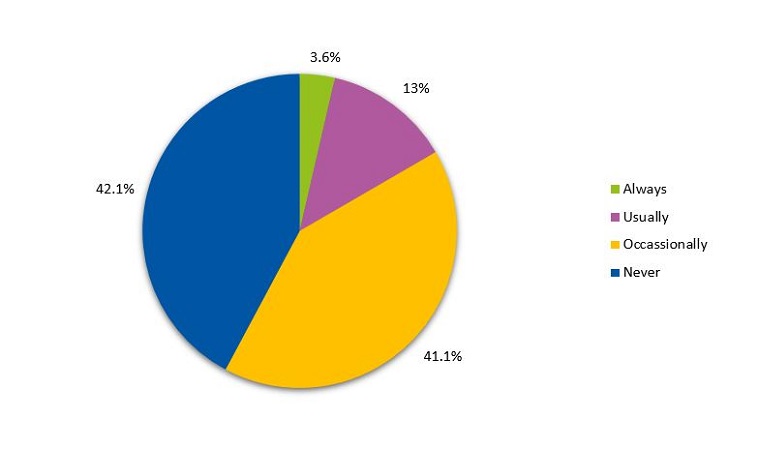
As for sleep induction, we found that 57.8% of children used electronic devices after dinner occasionally, regularly or always (Figure 4). Most children read before sleep every night (42.5%) (Figure 5). Also, 36.8% did not require the presence of a parent to fall asleep (Figure 6). Lastly, 37.5% of children still took naps.
When it came to current sleep patterns, we found that 57.8% of the children under study had a positive result in the BEARS questionnaire that indicated the possibility of a sleep disturbance. Table 4 presents the frequencies of positive answers for each sleep dimension. Of all children with a positive result of screening with the BEARS questionnaire, 62.2% only had 1 abnormal item, usually related to the persistence of daytime naps (Table 5). We found that the proportion of children with a positive result of screening with the BEARS questionnaire dropped to 37.71% if we excluded positive results due to persistence of napping.
| Table 4. Description of variables in positive screening with the BEARS questionnaire (n = 111) | ||||||
|---|---|---|---|---|---|---|
| Variable | n | Frequency of (+) answers | Percentage of (+) answers | Frequency of (–) answers | Percentage of (–) answers | |
| Bedtime problems | 111 | 21 | 18.9% | 90 | 81.1% | |
| Excessive daytime sleepiness | Sleepy or overtired | 110 | 11 | 10% | 99 | 90% |
| Daytime naps | 111 | 72 | 64.9% | 39 | 35.1% | |
| Frequent night awakenings | 110 | 27 | 24.5% | 83 | 75.45% | |
| Irregular sleep | 111 | 10 | 9% | 101 | 91% | |
| Snoring | 111 | 22 | 19.8% | 89 | 80.2% | |

| Table 5. Distribution of results of BEARS by number of abnormal items | |
|---|---|
| Number of abnormal items | Percentage of total children with + BEARS screening |
| 1 item | 62.2% |
| 2 items | 28.8% |
| 3 items | 5.4% |
| 4 items | 2.7% |
| >4 items | 0% |

In regard to the duration of night-time sleep, 59.1% of the sample slept between 9 and 10 hours, 35.8% more than 10 hours and 5.2% less than 9 hours.
Analysis of variables based on the BEARS questionnaire
When we analysed the association between the different variables under study and sleep patterns in children aged 4 years, we found a higher proportion of children with positive BEARS results in the following subsets: only child (84.2%); sleeping in the parents room from birth to present (70.6%); not attending a childcare centre (67.7%); currently sharing the room with parents (73.7%) or sleeping in a room of their own (65.8%); usually sleeping in the parental bed (75%); daily use of electronic devices after dinner (85.7%); regularly requiring the presence of a parent to fall asleep (68.2%); parents with a lower educational attainment and unemployed mother (76.5%) (Tables 6 and 7).
| Table 6. Percentage of positive BEARS screenings by socioeconomic variable | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | n | Answer | Frequency of (+) BEARS | Percentage of (+) BEARS | Frequency of (–) BEARS | Percentage of (–) BEARS | p | |
| Parental country of origin | Mother | 192 | Spain | 92 | 54.1% | 78 | 45.9% | >0.05 |
| Not Spain | 19 | 86.36% | 3 | 13.64% | ||||
| Father | 191 | Spain | 93 | 56.4% | 72 | 43.6% | >0.05 | |
| Not Spain | 17 | 65.4% | 9 | 34.6% | ||||
| Parental educational attainment | Mother | 192 | Primary school | 1 | 100% | 0 | 0% | >0.05 |
| Secondary school | 15 | 62.5% | 9 | 37.5% | ||||
| University | 95 | 59.9% | 72 | 43.1% | ||||
| Father | 189 | Primary school | 4 | 80% | 1 | 20% | >0.05 | |
| Secondary school | 27 | 71.1% | 11 | 28.9% | ||||
| University | 78 | 57.7% | 68 | 42.3% | ||||
| Parental employment | Mother | 191 | Employed | 83 | 55% | 68 | 45% | >0.05 |
| Unemployed | 13 | 76.5% | 4 | 23.5% | ||||
| Homemaker | 12 | 60% | 8 | 40% | ||||
| Other | 2 | 66.7% | 1 | 33.3% | ||||
| Father | 188 | Employed | 106 | 57.3% | 79 | 42.7% | >0.05 | |
| Unemployed | 0 | 0% | 0 | 0% | ||||
| Homemaker | 1 | 50% | 1 | 50% | ||||
| Other | 1 | 100% | 0 | 0% | ||||
| Family structure | 191 | Nuclear | 99 | 56.6% | 76 | 43.4% | >0.05 | |
| Single parent | 6 | 60% | 4 | 40% | ||||
| Extended family | 2 | 66.7% | 1 | 33.3% | ||||
| Other | 3 | 100% | 0 | 0% | ||||

| Table 7. Percentage of positive BEARS screenings by parenting history and sleep habits | |||||||
|---|---|---|---|---|---|---|---|
| Variable | n | Answer | Frequency of (+) BEARS | Percentage of (+) BEARS | Frequency of (–) BEARS | Percentage of (–) BEARS | P |
| Sibling order | 191 | Only child | 32 | 84.2% | 6 | 15.8% | 0.002 |
| First child | 33 | 54.1% | 28 | 45.9% | |||
| Middle child | 11 | 57.9% | 8 | 42.1% | |||
| Youngest child | 34 | 46.6% | 39 | 53.4% | |||
| Breastfeeding | 191 | Never | 12 | 60% | 8 | 40% | >0.05 |
| ≤6 months | 48 | 57.8% | 35 | 42.2% | |||
| >6 months | 50 | 56.8% | 38 | 43.2% | |||
| Age until which child slept in parents’ room | 192 | Never did | 1 | 25% | 3 | 75 | >0.05 |
| To 1 year (0-12 m) | 70 | 57.9% | 51 | 42.1% | |||
| To 2 years (24-36 m) | 20 | 51.3% | 19 | 48.7% | |||
| To 3 years (24-36 m) | 6 | 66.7% | 3 | 33.3% | |||
| To 4 years (36-48 m) | 2 | 100% | 0 | 0% | |||
| Still sleeping in parents’ room | 12 | 70.6% | 5 | 29.4% | |||
| Place where child slept in parents’ room | 192 | Separate crib | 77 | 57.5% | 57 | 42.5% | >0.05 |
| Bedside crib | 14 | 66.7% | 4 | 33.3% | |||
| Parental bed | 12 | 60% | 8 | 40% | |||
| Crib and parental bed | 7 | 53.8% | 6 | 46.2% | |||
| Never did | 1 | 25% | 3 | 75% | |||
| Method to get child to sleep | 190 | Held in arms or rocking | 56 | 56.6% | 43 | 43.4% | >0.05 |
| Alone | 43 | 61.4% | 27 | 38.6% | |||
| Other | 10 | 47.6% | 11 | 52.4% | |||
| Attendance to childcare centre | 192 | Yes | 90 | 55.9% | 71 | 44.1% | >0.05 |
| No | 21 | 67.7% | 10 | 32.3% | |||
| Type of room where the child currently sleeps | 191 | Own room | 48 | 65.8% | 25 | 34.2% | 0.052 |
| Shared with sibling | 48 | 49% | 50 | 51% | |||
| Shared with parents | 14 | 73.7% | 5 | 26.3% | |||
| Shared with other | 1 | 100% | 0 | 0% | |||
| Sleeps in parental bed part of the night | 192 | Always | 7 | 58.3% | 5 | 41.7% | >0.05 |
| Usually | 9 | 75% | 3 | 25% | |||
| Occasionally | 51 | 63% | 30 | 37% | |||
| Never | 44 | 50.6% | 43 | 49.4% | |||
| Use of electronic devices after dinner | 191 | Always | 6 | 85.7% | 1 | 14.3% | >0.05 |
| Usually | 15 | 60% | 10 | 40% | |||
| Occasionally | 46 | 58.2% | 33 | 41.8% | |||
| Never | 44 | 55% | 36 | 45% | |||
| Reading before bed | 192 | Always | 46 | 56.8% | 35 | 43.2% | >0.05 |
| Usually | 37 | 59.7% | 25 | 40.3% | |||
| Occasionally | 25 | 56.8% | 19 | 43.2% | |||
| Never | 3 | 60% | 2 | 40% | |||
| Needs presence of a parent to fall asleep | 192 | Always | 30 | 68.2% | 14 | 31.8% | >0.05 |
| Usually | 15 | 48.4% | 16 | 51.6% | |||
| Occasionally | 24 | 52.2% | 22 | 47.8% | |||
| Never | 42 | 59.2% | 29 | 40.8% | |||
| Duration of night-time sleep | 192 | <9 hours | 7 | 70% | 3 | 30% | 0.051 |
| 9-10 hours | 72 | 63.7% | 41 | 36.3% | |||
| >10 hours | 32 | 46.4% | 37 | 53.6% | |||

We found statistically significant differences between patients that were only children and patients that had siblings in the proportion of positive results of the BEARS questionnaire (p = .002).
As for the duration of night-time sleep, the BEARS questionnaire was positive in 70% of children that slept fewer than 9 hours, 63.7% of children sleeping 9 to 10 hours a night and 46.4% that slept more than 10 hours a night (p = .05).
We found that the BEARS questionnaire results were not associated with the duration of breastfeeding, where the child slept in the first months of life, the method used to put the child to sleep, reading before bed, family structure or parental age.
DISCUSSION
In healthy children aged 4 years, normal sleep consists of a night-time sleep period of approximately 10 hours that may be supplemented with daytime naps. According to previous studies, 10% of children sleep more than 12 hours and 10% less than 9.5 hours.16 In our study, we analysed the usual sleep pattern of children aged 4 years managed in 2 primary care centres in the region of Madrid using a validated screening tool. We chose the BEARS questionnaire because it is brief, extensive and easy to use in primary care settings. This questionnaire has been used in numerous studies and research projects in the English language, but few published studies have used the Spanish translation, which is recommended by guidelines.1,17 Bastida-Pozuelo and Sánchez-Ortuño conducted a study to validate this questionnaire by comparing it to the Children’s Sleep Habits Questionnaire (CSHQ), which is the reference test, and concluded that the Spanish translation of the BEARS questionnaire is a valid instrument for detection of sleep disturbances in children and adolescents.18 We chose not to use the CSHQ due to its extensive length and complexity and to the lack of established cut-off points to differentiate between abnormal and normal findings.
According to the Clinical Practice Guideline for management of sleep disturbances in primary care paediatrics, the prevalence of sleep disorders is of 30%,1 and they are important due to the long-term impact they have on children and their families. Our study found a prevalence of 57.8% of positive results of screening using the BEARS questionnaire, which just constitute a red flag, as a positive result does not necessarily entail the presence of a sleep disorder. Thus, a positive result should lead to individualised assessment in the clinic with a comprehensive evaluation of the child and family.
The sample under study mainly comprised Spanish families with a high socioeconomic status, a nuclear family structure and 2 or more children. This was slightly above the average birth and fertility rates found by the Instituto Nacional de Estadística (National Institute of Statistics)19 (mean number of children per woman: 1.33).
The sample was very homogeneous, so our findings can mainly be generalised to populations of similar sociocultural characteristics. We found an inverse correlation between parental educational attainment and the prevalence of sleep abnormalities. Precarious employment, defined as unemployment as a source of stress in the family, was also associated with a higher percentage of abnormal results. These findings were similar to those of previous studies.2
We found an unexpectedly high prevalence of breastfeeding in our sample (89.6% overall and 51.8% with a duration of more than 6 months) compared to the data reflected by the National Health Survey of Spain (ENSE) for 2011/12 (72.2% at 6 weeks and 46.9% at 6 months).20 Previous studies have found an association between long duration of breastfeeding and an increased prevalence of sleep disturbances,1 but we did not find significant differences in the latter based on whether the children had or not been breastfeed or whether breastfeeding was maintained for less or more than 6 months.
Another salient finding was that 28.5% of the families reported spontaneous cosleeping that was not associated with low socioeconomic status or housing conditions. We define cosleeping as the child habitually sleeping on the same surface as the parents. There are no official data on the prevalence of cosleeping in Spain, but a recent study in 2 primary care centres in Madrid that included 317 children found a prevalence of 31.86%.21 We ought to highlight that we found no association between cosleeping in the early months of life and sleep abnormalities at age 4 years.
In terms of the evolution of sleep from the first years to age 4 years, most children left the parental bedroom and went on to share a room with siblings or moved into a room of their own. It is worth noting that 9.9% of the children continued to sleep in the parental bedroom at age 4 years. This is particularly relevant, as we found a higher percentage of abnormal results of the BEARS questionnaire in this subset of children (73.7%) and in children sleeping in a room of their own (65.8%) compared to children that shared a room with siblings (49%). These findings could be applied in primary care by encouraging shared bedrooms with siblings if possible, both to prevent and to remedy abnormal sleep patterns.
We found a higher prevalence of abnormalities in children that habitually go to the parental bed during the night and that need their presence to fall asleep, both aspects that can be considered indicators of reactive cosleeping. These findings were consistent with those of previous studies.1,10
We found that sleep abnormalities were more common in only children (p = .002). While this factor may not be modified, understanding its association with sleep abnormalities allows the paediatrician to identify these families, encourage a parenting style that fosters autonomy in the child and support parents so they feel confident in childrearing.
One of the aspects that has been most extensively studied to date is the use of electronic devices by children due to the social alarm generated by screen addiction. We found that 57.8% of the sample used screens for sleep induction, compared to the prevalence of 39.1% found by studies in other countries.5 Paediatric societies22 recommend limiting screen time to less than 1 hour a day in children aged more than 2 years and avoiding screens for an hour before going to bed. The high prevalence found in our study indicates a need for intervention by paediatricians, as we found a higher proportion of children with screenings that were positive for sleep abnormalities in the group that used screens habitually before bed (85.7%), which was consistent with previous studies.5,11
When it comes to sleep duration, it is recommended that children aged 4 years sleep between 10 and 12 hours a day.1 The most frequent duration of night-time sleep in this age group is 10 hours, which are supplemented with daytime naps.16 The hours of night-time sleep in children in our sample were at the lower limit of the recommendations: 94.9% slept 9 or more hours. However, this may be compensated in the total duration of sleep through the persistence of napping in 37.5% of the sample.
Although the questionnaire used in the study (BEARS) considers daytime napping indicative of sleep problems in this age group, naps are actually recommended until age 5 years.1 In cases where a positive result in the BEARS questionnaire is only due to napping, paediatricians must take a history to determine whether these naps are integrated appropriately in the routine of the child or give rise to problems in the household or child care setting, which would allow discrimination of patterns that are truly pathological. We estimated the prevalence of sleep disturbances excluding cases where abnormal results were due exclusively to the persistence of napping, which corresponded to 37.71% of children with a positive result in the BEARS questionnaire, a value that was consistent with previous studies.1
The purpose of this study was to identify environmental factors that can be acted on and also factors that, while not being modifiable, are associated with sleep disturbances. At present, families are expressing an eagerness to adopt optimal parenting approaches in rearing their children, and they convey these concerns to their paediatricians. Our findings suggest that screening instruments to detect warning signs of sleep disturbances can be useful to paediatricians for the purpose of implementing preventive measures (such as counselling parents regarding childrearing, promoting regular sleep times and an adequate sleep duration in children and advising against the use of electronic devices at early ages).
We ought to underscore that all other modifiable factors, such as reading before bed or the method used to put the child to bed, seemed to have a lesser impact on sleep patterns.
When considering further research on this subject, the limitations of the current study should be taken into account. First, despite the sample including 193 patients from 2 different health districts, the populations were homogeneous in certain aspects (family structure, nationality, parental employment status and age, etc), so we were unable to analyse the association of certain factors with sleep patterns. We also need to consider the possibility of recall bias, as the questionnaire includes items that refer to the first years of life that parents with children with sleep problems may remember more accurately.
CONCLUSION
We found a high prevalence in children of positive results of screening with the BEARS questionnaire, which is very relevant in primary care paediatrics practice due to the potential long-term repercussions of sleep disturbances in childhood. We recommend considering the development of appropriate screening protocols to identify children at risk.
We found few associations between parenting behaviours and sleep patterns at age 4 years. We did not find any differences based on the type or duration of feeding in infancy or spontaneous cosleeping.
Paediatricians must respect the parenting style of the parents and promote educational measures that foster autonomy in the child while avoiding recommendations on changing the duration of breastfeeding or spontaneous cosleeping with the purpose of improving future sleep patterns in children. However, the use of electronic devices in children should be discouraged, as there is evidence that the amount of time spent on these devices substantially exceeds the maximum recommended by paediatric associations.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
BEARS: Bedtime problems, Excessive daytime sleepiness, Awakenings during the night, Regularity and duration of sleep, Snoring · CSHQ: Children’s Sleep Habits Questionnaire · PCC: primary care centre.
REFERENCES
- Grupo de trabajo de la Guía de Práctica Clínica sobre Trastornos del Sueño en la Infancia y Adolescencia en Atención Primaria. Guía de Práctica Clínica sobre Trastornos del Sueño en la Infancia y Adolescencia en Atención Primaria. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad, Política Social e Igualdad. Unidad de Evaluación de Tecnologías Sanitarias de la Agencia Laín Entralgo; 2011. Guías de Práctica Clínica en el SNS: UETS no. 2009/8. Available at https://portal.guiasalud.es/wp-content/uploads/2018/12/GPC_489_Trastorno_sue%D0%B4o_infadol_Lain_Entr_compl.pdf
- Jones C, Ball H. Exploring socioeconomic differences in bedtime behaviours and sleep duration in English preschool children. Inf Child Dev. 2014;23:518-31.
- Owens JA. Behavioral sleep problems in children. In: UpToDate [online] [accessed 29/10/2019]. Available at www.uptodate.com/contents/behavioral-sleep-problems-in-children
- Mindell JA, Sadeh A, Kwon R, Goh DYT. Cross-cultural differences in sleep of preschool children. Sleep Med. 2013;14:1283-9.
- Brambilla P, Giussani M, Pasinato A, Venturelli L, Privitera F, Miraglia Del Giudice E, et al. Sleep habits and pattern in 1-14 years old children and relationship with video devices use and evening and night child activities. Ital J Pediatr. 2017;43:7.
- Pin Arboledas G, Cubel Alarcon M, Martín González G, Lluch Rosello A, Morell Salort M. Hábitos y problemas con el sueño de los 6 a los 14 años en la Comunidad Valenciana. Opinión de los propios niños. An Pediatr (Barc). 2011;74:103-15.
- Matthews KA, Pantesco EJM. Sleep characteristics and cardiovascular risk in children and adolescents: an enumerative review. Sleep Med. 2016;18:36-49.
- Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 2003;74:444-55.
- Galland BC, Mitchell EA. Helping children sleep. Arch Dis Child. 2010;95:850-3.
- Li S, Jin X, Yan C, Wu S, Jiang F, Shen X. Bed- and room-sharing in Chinese school-aged children: Prevalence and association with sleep behaviors. Sleep Med. 2008;9:555-63.
- Magee CA, Lee JK, Vella SA. Bidirectional relationships between sleep duration and screen time in early childhood. JAMA Pediatr. 2014;168:465-70.
- Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2-to 8-year-old children. Pediatrics. 2005;115:225-32.
- Botino CJ, Rifas-Shiman SL, Kleinman KP, Oken E, Redline S, Gold D, et al. The association of urbanicity with infant sleep duration. Health Place. 2012;18:1000-5.
- Bathory E, Tomopoulos S. Sleep regulation, physiology and development, sleep duration and patterns, and sleep hygiene in infants, toddlers, and preschool-age children. Curr Probl Pediatr Adolesc Health Care. 2017;47:29-42.
- Pascual M, Estivill E, Albares J. Trastornos del sueño en la infancia. An Pediatr Contin. 2007;5:302-7.
- Pin G, Ugarte R. Lo que el pediatra de Atención Primaria debería saber sobre el sueño. Rev Pediatr Aten Primaria. 2010;12:s219-s230.
- Pin G, Ugarte R. Taller de sueño infantil. Herramientas para su interpretación por el pediatra de Atención Primaria. Rev Pediatr Aten Primaria. 2009;11:s399-s404.
- Bastida-Pozuelo MF, Sánchez-Ortuño MM. Preliminary analysis of the concurrent validity of the Spanish translation of the BEARS sleep screening tool for children. J Psychiatr Ment Health Nurs. 2016;23:513-20.
- España en cifras 2017. In: Instituto Nacional de Estadística [online] [accessed 29/10/2019]. Available at www.ine.es/prodyser/espa_cifras/2017/index.html#1
- Encuesta Nacional de Salud de España 2011/12. Resultados detallados nacionales y por comunidades autónomas. In: Ministerio de Sanidad, Servicios Sociales e Igualdad. Portal Estadístico del SNS [online] [accessed 29/10/2019]. Available at www.msssi.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2011/encuestaResDetall2011.htm
- Martín Martín R, Sánchez Bayle M, Teruel de Francisco MC. El colecho en nuestro medio: estudio de casos y controles en las consultas pediátricas de Atención Primaria. Rev Pediatr Aten Primaria. 2017;19:15-21.
- AAP Council on Communications and Media. Media and young minds. Pediatrics. 2016;138:e20162591.