Hospital treatment of moderate-severe bronchiolitis, hypertonic or physiological saline? Analysis of risk factors associated with readmission
Mario Ferrer Vázqueza, Marta Álvarez Martína, Ana Delgado Vicentea, Laura Álvarez Chamorrob, Ricardo Tosca Seguraa
aUnidad de Neumología y Alergia Pediátricas. Hospital General Universitario de Castellón. Castellón de la Plana. España.
bPediatra. CS Cariñena. Vilarreal. Castellón. España.
Correspondence: M Ferrer . E-mail: maferrer@uji.es
Reference of this article: Ferrer Vázquez M, Álvarez Martín M, Delgado Vicente A, Álvarez Chamorro L, Tosca Segura R. Hospital treatment of moderate-severe bronchiolitis, hypertonic or physiological saline? Analysis of risk factors associated with readmission. Rev Pediatr Aten Primaria. 2019;21:e31-e40.
Published in Internet: 17-06-2019 - Visits: 37419
Abstract
Introduction: although numerous studies have been published to date on the subject of inpatient management of bronchiolitis and the promising outcomes obtained with hypertonic saline, this subject remains controversial.
Materials and methods: we conducted a prospective observational study to assess the effectiveness of 3% hypertonic saline compared to physiological saline in the inpatient management of bronchiolitis, understood as the achieved reductions in length of stay and clinical severity scores. In a second phase, we analysed the risk factors associated with readmission due to bronchospasm in the same sample of patients.
Results: we included 67 out of the 73 patients admitted with bronchiolitis in the analysis, of who 9 received physiological saline and 58 hypertonic saline, with or without an added bronchodilator. The mean length of stay was 6.07 ± 3.12 days in the physiological saline group and 6.67 ± 4.36 days in the hypertonic saline group. The mean severity score (Wood-Downes scale modified by Ferrés) was 3.67 ± 1.1 in the physiological saline group versus 3.16 ± 1.1 in the hypertonic saline group. In the second phase of the study, we found a readmission rate of 8.2%.
Conclusion: we did not find statistically significant differences between the two groups in the length of stay or in the improvement in the clinical severity score or duration of oxygen therapy. Although the sample size was small, we did not find any trends in our sample suggesting the actual presence of significant differences. The factors associated most strongly with readmission were age of less than 6 months, male sex, having older siblings and exposure to smoke in the household.
Keywords
● Bronchiolitis ● Bronchospasm ● Hypertonic saline solution ● Nebulizers ● PediatricsINTRODUCTION
Acute respiratory tract infections are the most frequent type of infectious disease in humans.1 In the field of paediatrics, acute bronchiolitis (AB) is the most frequent lower respiratory tract infection in infants,2 and it is the main reason for admission due to lower respiratory tract infection in children aged less than 2 years.3 This is particularly significant in infants aged less than 6 months, with this ag group amounting to up to 93% of total admissions due to AB in some case series.4 Thus, AB is important on account of the considerable morbidity it causes, in addition to the associated social and economic costs.5
The diagnostic criteria most widely accepted by current consensus guidelines are the classic criteria proposed by McConnochie, by which AB is defined as a first acute episode of respiratory distress with wheezing preceded by a cold-like illness of the upper respiratory tract (rhinitis, cough, with/without fever) in children aged less than 2 years, although it most frequently occurs in the first year of life, a period that is the main focus of many authors.3,4 A second or later episodes are known as recurrent wheezing or recurrent bronchospasm.6
It is important to differentiate AB from recurrent wheezing, since while they may be related due to the associated risk factors (increased risk of recurrent wheezing in childhood in patients with AB),5,7,8 the approach to management will differ depending on the characteristics of the patient.
Numerous interventional studies have been conducted to improve the management of AB, but there is still considerable controversy, and the current evidence is insufficient to determine which is the optimal approach to treat paediatric inpatients with moderate to severe bronchiolitis.9 Most of the disagreement revolves around the use of bronchodilators (salbutamol and epinephrine) inhaled or nebulised in solution in physiological saline (PS) (0.9%) or hypertonic saline (HS) (3%),9,10 as well as the use of systemic steroids11,12 or HS in isolation without a bronchodilator.13,14
We conducted an initial observational study in our hospital between January 2013 and March 2014.15 The study included patients admitted to hospital with AB, who were divided into 2 groups based on whether they were given 3% HS or PS, alone or with bronchodilators. We analysed the mean length of stay and found no significant differences between groups: 5.93 days (standard deviation [SD], ± 3) in the HS group versus 5.96 (SD, ± 2.64) in the PS group.
MATERIALS AND METHODS
Objectives
The primary objective of the first phase of the study was to assess whether 3% HS was more effective than PS for treatment of AB in terms of a reduction in length of stay. The secondary objectives were to compare the effectiveness of 3% HS versus PS in reducing symptoms, which we assessed by means of clinical severity scales administered at admission and daily thereafter.
The primary objective of the second phase of the study was to identify the risk factors associated with recurrent wheezhing16,17 and determine the readmission rate.
Study design
We conducted a prospective, observational, longitudinal cohort study without an intervention under real world conditions. The study was divided into 2 phases:
- First phase: patients admitted with a diagnosis of AB during the period under study, which were divided into 2 cohorts: patients treated with nebulised 3% HS and patients that received conventional treatment with nebulised PS. Both groups could receive other treatments with potential addition of bronchodilators to the nebulised saline, based on the judgment of the physician in charge. Saline, with or without a bronchodilator, was administered through a facemask and with medical air (except in patients that required oxygen therapy) at flow rates of 6-8 bpm, to a total volume of de 3% HS or PS of 3 ml.
- Second phase: readmissions of patients initially included in phase one of the study due to episodes of bronchospasm during the period under study. We analysed possible risk factors for readmission, as well as possible ongoing treatments or concomitant circumstances.
The allocation of patients to specific therapeutic approaches was not predetermined by the study protocol, but rather by customary clinical practice, and the decision to prescribe a specific drug was clearly separated from the decision to include the patient in the study. The study did not involve performance of any specific intervention, for either diagnosis or management, outside those used in everyday clinical practice.
The study was approved by the local ethics and clinical research committee.
Period under study
We collected data from September 1, 2015 through March 30, 2016 for the first phase, which corresponds to the period of the year with the highest incidence of respiratory illness, and collected data through June 30, 2016 for the second phase of the study. We extended the period under study for this second phase to try to include as many patients as possible for the full academic year that required readmission to the paediatrics ward of the Hospital General Universitario de Castellón.
Study universe and sample selection
The inclusion criteria for the first phase were: 1) patient aged less than 2 years admitted to our department with a diagnosis of AB based on the classic criteria accepted by the Spanish consensus-based guidelines3; and 2) initiation of nebulised treatment based on the judgment of the physician.
All patients underwent testing for detection of respiratory syncytial virus (RSV) in a nasal aspirate sample, as the test was available and included in the hospital admission protocol.
In the second phase, we included patients previously included in the first phase, in this instance through age 3 years, who required readmission during the study followup due to wheezing, bronchial spasms, obstructive bronchitis or illness related to secondary bronchial hyperresponsiveness.
Primary and secondary outcomes
In the first phase of the study, the primary outcome was the length of stay in days.
We also collected data for the following variables:
- Dichotomous variables: aerosol therapy, use of other treatments (bronchodilators, antibiotherapy, steroid therapy), demographic characteristics (smokers in the household, personal or family history of atopy, asthma, preterm birth before 35-32 weeks’ gestation, bronchopulmonary dysplasia, treatment with palivizumab, infection by RSV, sex, crowding, enrolment in child care centre, birth weight < 2500 g, maternal age < 25 years and older siblings).
- Categorical qualitative variables: ethnicity, trimester of birth.
- Ordinal quantitative variables: score in clinical prediction rule (Wood-Downes modified by Ferrés); although the evidence supporting the use of a severity scale in patients with bronchiolitis is insufficient, this scale is widely used, 18 which is why we include it in our study.
- Discrete quantitative variables: duration of oxygen therapy (in days) and age (in months).
In the second phase, the primary outcome was the number of readmissions. We analysed this outcome taking into account the variables studied in the previous phase, analysing their role as risk factors, also adding the presence or absence of treatment for an underlying condition and the mean length of stay during the initial hospitalization.
Although both phases may have overlapped in time, we analysed them separately.
Statistical analysis
For the first phase, we performed a descriptive analysis of the variables under study, summarising the data as percentages or means or medians. The null hypothesis was the absence of difference in the mean length of stay between the two groups. We tested the assumption of normality by means of the Kolmogorov-Smirnov test.
In the bivariate analyses, we first assessed the correlation between the use of PS or HS and clinical improvement (clinical severity scale) by means of the Student t test. Subsequently, we analysed the association between different risk factors and length of stay by means of the Student t test in case of qualitative variables and linear regression in case of quantitative variables. We used multivariate linear regression to analyse the association of different risk factors and length of stay, calculating the odds ratio. We controlled for potential confounders and interactions.
When it came to the second phase of the study, given the small sample size, we simply performed a descriptive analysis of the children that were readmitted.
We calculated the statistics with the corresponding 95% confidence intervals. We defined statistical significance as a p-value of less than 0.05. The statistical analysis was performed with the software SPSS® version 22.
RESULTS
General data
Between September 1, 2015 and March 30, 2016, a total of 73 patients aged less than 2 years were admitted to our hospital with a diagnosis of AB. Of this total, 46 were boys (63%) and 27 girls (37%). Extending the followup period through September 30, 2016, a total of 6 patients were readmitted due to bronchospasm (8.2 %).
First phase
Table 1 summarises the risk factors and epidemiological characteristics of the patients. None of the patients in the sample had been born before 32 weeks’ gestation or had lung malformations, cystic fibrosis, immunodeficiency, bronchopulmonary dysplasia or neuromuscular or metabolic disorders.
| Table 1. Epidemiological characteristics of the sample | |||||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Sex | Male Female |
46 27 |
63 37 |
Significant heart disease | 4 | 5.5 | |
| Age | <6 months 6-12 months >12 months |
63 9 1 |
86.3 12.3 5.4 |
Maternal age <25 years | 6 | 8.2 | |
| Trimester of birth | 1st trimester 2nd trimester 3rd trimester 4th trimester |
11 7 18 37 |
15.1 9.6 24.7 50.7 |
Crowding | 7 | 9.6 | |
| Ethnicity | Maghrebi Caucasian Roma Latin American |
6 61 5 1 |
8.2 83.6 6.8 1.4 |
History of atopy | Personal Familiar |
7 19 |
9.6 26 |
| Enrolment in child care services | 8 | 11 | Family history of asthma | 22 | 30.1 | ||
| Smoking in household | 32 | 43.8 | Infection by RSV | 43 | 58.9 | ||
| Older siblings | 45 | 61.6 | Prophylaxis with palivizumab | 3 | 4.1 | ||
| Preterm birth before 35-32 weeks | 8 | 11 | Admission to ICU | 3 | 4.1 | ||
| Birth weight <2500 g | 14 | 19.2 | |||||

Table 2 summarises the most common treatments used during the acute phase of bronchiolitis. Six patients received both types of saline solutions, so we considered them lost to followup in the analysis of the first phase of the study, although they were included in the analysis of the second. The analysis of the first phase included patients treated with PS or 3% HS with or without a bronchodilator and the type of bronchodilator, if one was used, among other treatments. Oxygen therapy was delivered with nasal prongs or a Venturi mask.
| Table 2. Treatments used | ||||||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Saline treatment | PS HS Lost to followup |
9 58 6 |
13.4 86.6 |
Only HS | 17 | 25 |
| Epinephrine + HS | 25 | 37.3 | Macrolides | 9 | 12.3 | |
| Epinephrine + PS | 2 | 3 | Intravenous corticosteroids | 3 | 4.1 | |
| Salbutamol + HS | 16 | 23.9 | Oxygen therapy | 36 | 49.3 | |
| Salbutamol + PS | 7 | 10.4 | Other antibiotics | 12 | 16.4 | |
| Only PS | 0 | 0 | ||||

We recorded the clinical severity scores (Wood-Downes scale modified by Ferrés18 at admission, from day 1 through 4 of admission and the mean), the duration of oxygen therapy in days and the length of stay. We highlight as most relevant the scores obtained on the second day of admission, as it provides additional information on the response to treatment and was measured under more homogeneous circumstances.
In the analysis of the clinical severity scores and the age of the patients, we found that 23 patients had mild bronchiolitis (score, 1-3 points), 43 moderate bronchiolitis (score, 4-7 points) and 3 severe bronchiolitis (score, 8-14 points). The ANOVA revealed that at the time of admission, patients with mild bronchiolitis had a mean age of less than 3 months, patients with moderate bronchiolitis a mean age of 5 months and patients with severe bronchiolitis a mean age of less than 2 months, although the differences were not statistically significant (p = 0.74).
Table 3 shows the length of stay values in relation to the different risk factors for bronchiolitis and the treatments received. We did not find statistically significant differences in length of stay based on the use of PS versus HS. We ought to highlight that in our study, we did not find an association between the detection of RSV and the length of hospitalization.
| Table 3. Risk factors associated with length of stay | ||||
|---|---|---|---|---|
| Mean ± SD (days) | p | 95 CI | ||
| Aerosol therapy | HS PS |
6.07 ± 3.12 6.67 ± 4.36 |
0.99 | -2.44 to 2.42 |
| Epinephrine | Yes No |
8.19 ± 4.07 4.93 ± 1.99 |
0.0005 | -4.95 to -1.5 |
| Salbutamol | Yes No |
5.81 ± 3.33 6.33 ± 3.32 |
0.52 | -1.09 to 2.12 |
| Intravenous steroids | Yes No |
10.33 ± 2.52 5.96 ± 3.23 |
0.024 | -8.15 to -0.59 |
| Macrolides | Yes No |
8.50 ± 4.23 5.67 ± 2.92 |
0.045 | -5.58 to -0.07 |
| Sex | Male Female |
6.11 ± 3.48 6.19 ± 3.05 |
0.92 | -1.68 to 1.5 |
| Older siblings | Yes No |
6.73 ± 3.34 5.18 ± 3.08 |
0.05 | -3 to 0 |
| Preterm birth 32-35 wk | Yes No |
7.13 ± 4.58 6.02 ± 3.14 |
0.52 | -4.596 to 2.45 |
| Exposure to smoke | Yes No |
6.53 ± 3.57 5.83 ± |
0.37 | -2.26 to 0.86 |
| RSV | Yes No |
6.72 ± 3.14 5.3 ± 3.02 |
0.07 | -2.96 to 0.12 |
| Allergy | Yes No |
6.19 ± 3.27 6.11 ± 3.36 |
0.92 | -1.7 to 1.5 |
| Birth weight <2500 g | Yes No |
7.14 ± 3.92 5.9 ± 3.14 |
0.21 | -3.19 to 0.709 |
| Maternal age <25 years | Yes No |
7 ± 3 6.06 ± 3.34 |
0.51 | -3.76 to 1.83 |
| Family history of asthma | Yes No |
6.32 ± 3.87 6.06 ± 3.07 |
0.76 | -1.95 to 1.4 |
| Crowding | Yes No |
6.8 ± 2.85 6.06 ± 3.36 |
0.55 | -3.43 to 1.83 |

We assessed the effectiveness of HS and PS. Table 4 shows that there were no significant differences between the 2 types of saline solution in terms of bronchiolitis symptom reduction, assessed by means of the severity score at admission and every day during hospitalization (Wood-Downes scale modified by Ferrés) and the duration in days of oxygen therapy.
| Table 4. Clinical improvement with fluid therapy (in terms of score in WDF scale) | ||||
|---|---|---|---|---|
| Mean ± SD | p | 95 CI | ||
| Score at admission | PS HS |
4.33 ± 1.32 points 4.12 ± 1.76 points |
0.73 | -1.01 to 1.43 |
| Mean score | PS HS |
3.67 ± 1.1 points 3.16 ± 1.1 points |
0.2 | -0.28 to 1.30 |
| Oxygen therapy | PS HS |
2.33 ± 2.06 days 2.34 ± 3.55 days |
0.99 | -2.44 to 2.42 |

We conducted a bivariate analysis to assess the impact of risk factors on the length of stay, and found that length of stay was associated most strongly with age and the severity score on day 2 of admission: the lower the age and the higher the second-day severity score, the longer the length of stay; this association was significant for the latter risk factor.
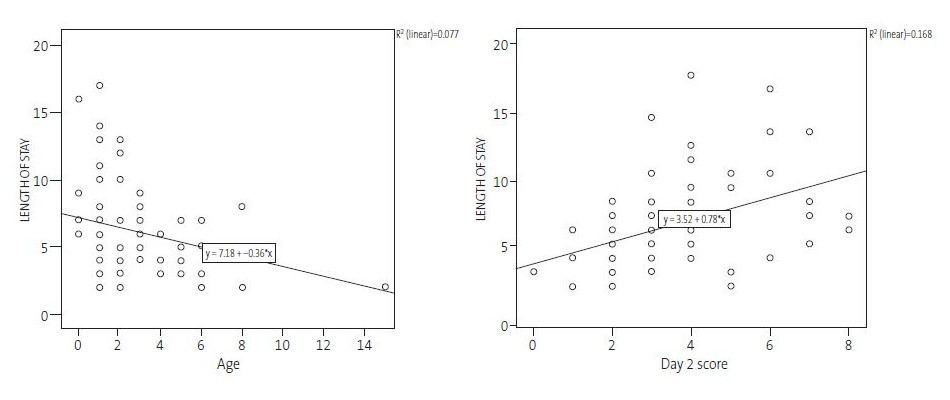
Figure 1 shows the linear correlation between age and the clinical severity score on day 2 of admission on one hand, and length of stay on the other: the length of stay decreased with increasing patient age (expressed in months), and increased with increasing clinical severity scores. With each month of age, the length of stay decreased by 0.36 days (95% confidence interval [95 CI]: 0/66 to 0.07, p = 0.02) and with each additional point in the clinical severity score, the length of stay increased by 0.78 days (95 CI: 0.36 to 1.21).
| Figure 1. Simple linear regression: age – length of stay and severity score on day 2 – length of stay |
|---|
 |

We included the most significant variables in the multivariate analysis and found that age and the clinical severity score at day 2 of admission continued to be significant. We did not find a significant association with any of the other variables or with the type of treatment received (PS versus HS).
We analysed the clinical severity score on the second day of admission, which we considered to be most representative, as it was available for nearly the entire sample and was calculated when treatment had already started.
Second phase
Of the 73 patients admitted in the first phase of the study, 6 were readmitted during the followup. Table 5 presents the main demographic characteristics of these patients. We ought to highlight that only 1 of these patients had infection by RSV in the initial admission and that none was receiving maintenance treatment. The mean length of stay after admission for a first episode in these 6 patients was of 5 days, with a median clinical severity score in the first admission of 3 (which was the same in the second day).
| Table 5. Epidemiological characteristics of readmitted patients | ||||
|---|---|---|---|---|
| N | % | <6 months | Sex M/F | |
| Age <6 months | 4 out of 6 | 66.66% | 3/1 | |
| Fourth trimester of year | 3 out of 6 | 50% | 3 out of 3 (100%) | 3/0 |
| Male sex | 5 out of 6 | 83.33% | 3 out of 5 | |
| Child care centre | 1 out of 6 | 16.67% | no | 1/0 |
| Older siblings | 4 out of 6 | 66.67% | 3 out of 4 | 3/1 |
| Preterm birth >32 wk | 0 | 0 | 0 | 0 |
| Preterm birth <32 wk | 0 | 0 | 0 | 0 |
| Birth weight <2500 g | 2 out of 6 | 33.33% | 2 out of 2 (100%) | 1/1 |
| Significant heart disease | 0 | 0 | 0 | 0 |
| Maternal age <25 years | 0 | 0 | 0 | 0 |
| Crowding | 1 out of 6 | 16.67% | 1 out of 1 | 1/0 |
| PHx of atopy | 0 | 0 | 0 | 0 |
| FHx of atopy | 3 out of 6 | 50% | 2 out of 3 | 3/0 |
| Exposure to smoke | 4 out of 6 | 66.67% | 3 out of 4 | 3/1 |
| FHx of asthma | 2 out of 6 | 33.33% | 2 out of 2 | 2/0 |
| HS | 4 out of 6 | 66.66% | 3 out of 4 | 4/0 |
| PS | 2 out of 6 | 33.33% | 1 out of 2 | 1/1 |
| Palivizumab | 0 | 0 | 0 | 0 |

DISCUSSION
There is still considerable controversy and a dearth of data on the optimal approach to the management of children hospitalised due to bronchiolitis, which requires intervention at the local level and comparisons between hospitals of each cohort of patients, data that could be later used in multicentre studies or systematic reviews.
A systematic review about HS19 published in 2013 reported initial results that were promising; it seemed at that point that an effective, safe and inexpensive treatment had been found. But later on, the controversy regarding its routine use re-emerged in several studies and guidelines.20-23
At present, the routine clinical practice of different hospitals, our own among them, includes the use of nebulised bronchodilators in PS or 3% HS or the use of nebulization without bronchodilators as a therapeutic trial, in addition to supportive measures such as standard and high-flow oxygen therapy, nutritional management and hydration.
First phase
As expected, 83% of the patients admitted due to AB were aged less than 6 months. Given the age of the patients and that the prescription of fluid therapy depended on the judgment of the clinician in charge, 86% were treated with 3% HS. The small sample size in our study and the difference between the number of patients given 3% HS versus PS made it difficult to find statistically significant differences and also precludes the generalization of results to the general population. Nevertheless, we believe that obtaining samples in our hospital and analysing the subsequent results will contribute significantly to the management of disease in our hospitalised patients, and that the findings may be useful to other health care facilities and researchers.
When we analysed the association of different epidemiological factors with length of stay, we did not find statistically significant differences, even in the case of RSV infection, but we ought to mention that the presence of older siblings corresponded to a p-value that neared the threshold of significance, with children without siblings having longer lengths of stay. On the other hand, our analysis of the treatment received revealed that patients treated with nebulised adrenaline, intravenous steroids and non-macrolide antibiotics had longer lengths of stay. This is probably because the patients that received these treatments were younger and had higher severity scores, and were therefore more ill. We found that age and the severity score on the second day of admission were the factors most strongly correlated with length of stay: younger age and a higher severity score were associated with longer stays.
Second phase
We analysed the episodes of recurrent wheezing, which are frequent after bronchiolitis. Given the considerable prevalence and impact of readmission, it is important to thoroughly investigate the risk factors associated with it that lead to its occurrence.
In 2006, a prospective observational study was conducted in the Hospital de Cabueñes (Gijon)17 with the aim of identifying the risk factors for poor outcomes and readmission with recurrent wheezing in young children. In the group of readmitted patients, there was a higher proportion of girls (a finding that diverges from other reports in the literature and with our study), smoking parents and a prolonged length of stay in the first hospital admission, and all of these differences were statistically significant. The rate of readmission during the followup period of this study was 5.8%.17
In our sample, 6 out of the 73 patients that were admitted with an initial episode were readmitted, corresponding to a readmission rate of 8.2%, which was slightly higher. The epidemiological factors most frequently identified in the cases of readmission in our sample were male sex, age of less than 6 months, smoking in the household and the presence of older siblings.
Our findings were pretty consistent with those reported in the previous literature.24 One of the risk factors for readmission that was not identify in our study was atopy, which is considered a good indicator of the response to certain treatments (salbutamol, inhaled steroids) but may not be a good predictor of readmission. This may suggest the presence of a different underlying physiological mechanism in atopic patients that renders them more vulnerable to the development of asthma but, on the other hand, would also result in an improved response to inhaled steroids, which would in turn improve the management of these patients while reducing the readmission rate. These ideas are currently being debated and researched.
CONCLUSIONS
There are still more doubts than certainties in the management of AB, and we have yet to find a treatment that is truly effective or generalizable. In our reduced sample, we did not find significant differences in length of stay or improvement of daily clinical severity scores between treatment with HS and treatment with PS. While the sample was small, we also did not find any trends in our results suggesting there could be real significant differences between these two treatments. Lastly, the factors most strongly associated with readmission were age of less than 6 months, male sex, having older siblings and smoking in the household.
While we await new treatments of demonstrated efficacy and effectiveness based on antivirals, immunotherapy or phenotype-based approaches, it would be useful to conduct further studies to correctly analyse the currently available supportive measures and symptomatic treatments aimed at improving clinical manifestations in our patients, and also to improve our ability to predict, prevent and treat recurrent cases.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
AB: acute bronchiolitis · BE: bronchospasm · CI: confidence interval · HS: hypertonic saline · PS: physiologic saline · RSV: respiratory syncytial virus · SD: standard deviation.
REFERENCES
- Calvo Rey C, García García ML, Casas Flecha I, Pérez Breña IP. Infecciones respiratorias virales. In: Asociación Española de Pediatría [online] [accessed 07/06/2019]. Available at https://www.aeped.es/sites/default/files/documentos/irsv.pdf
- American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics 2006;118:1774-93.
- Ochoa Sangrador C, González de Dios J, Grupo de Revisión del Proyecto aBREVIADo. Conferencia de consenso sobre bronquiolitis aguda (II): epidemiología de la bronquiolitis aguda. Revisión de la evidencia científica. An Pediatr (Barc). 2010;72:222.e1-222.e26.
- Ramos-Fernández JM, Pedrero-Segura E, Gutiérrez-Bedmar M, Delgado-Martín B, Cordón-Martínez AM, Moreno-Pérez D, et al. Epidemiología de los ingresos por bronquiolitis en el sur de Europa. An Pediatr (Barc). 2017;87:260-8.
- González de Dios J, Ochoa Sangrador C, Grupo de Revisión del Proyecto aBREVIADo. Conferencia de consenso sobre bronquiolitis aguda (I): metodología y recomendaciones. An Pediatr (Barc). 2010;72:221.e1-221.e33.
- Sigurs N, Gustafsson PM, Bjarnason R, Lundberg F, Schmidt S, Sigurbergsson F, et al. Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am J Respir Crit Care Med. 2005;171:137-41.
- Stein RT, Sherrill D, Morgan WJ, Holberg CJ, Halonen M, Taussig LM, et al. Respiratory syncytial virus in early life and risk of wheeze and allergy by age 13 years. Lancet. 1999;354:541-5.
- González de Dios J, Ochoa Sangrador C, Grupo de Revisión de Proyecto aBREVIADo. Conferencia de Consenso sobre bronquiolitis aguda (IV): tratamiento de la bronquiolitis aguda. Revisión de la evidencia científica. An Pediatr (Barc). 2010;72:285.e1-285.e42.
- Ipek IO, Yalcin EU, Sezer RG, Bozaykut A. The efficacy of nebulized salbutamol, hypertonic saline and salbutamol/hypertonic saline combination in moderate bronchiolitis. Pulm Pharmacol Ther. 2011;24:633-7.
- Hartling L, Fernandes RM, Bialy L, Milne A, Johnson D, Klassen TP, et al. Steroids and bronchodilators for acute bronchiolitis in the first two years of life: systematic review and meta-analysis. BMJ. 2011;342:d1714.
- Ochoa Sangrador C, González de Dios J. Broncodilatadores y corticoides en la bronquiolitis aguda: adrenalina nebulizada y poco más. Evid Pediatr. 2011;7:42.
- Zhang L, Mendoza-Sassi RA, Klassen TP, Wainwright C. Nebulized hypertonic saline for acute bronchiolitis: a systematic review. Pediatrics. 2015;136:687-701.
- Florin TA, Shaw KN, Kittick M. Nebulized hypertonic saline for bronchiolitis in the emergency department: a randomized clinical trial. JAMA Pediatr. 2014;168:664-70.
- Wu S, Baker C, Lang ME. Nebulized hypertonic saline for bronchiolitis: a randomized clinical trial. JAMA Pediatr. 2014;168:657-63.
- Delgado A, Álvarez L, Álvarez M, Ferrer-Vázquez M. Suero salino hipertónico en el tratamiento de la bronquiolitis. ¿La nebulización ideal o una más? Bol Soc Val Pediatr. 2014;34:41.
- Gómez Carrasco JA. El asma en los primeros años de la vida y su relación con las infecciones virales. Rev Pediatr Aten Primaria. 2006;8:453-75.
- Fernández Fernández EM. Características epidemiológicas del lactante con primer episodio sibilante: ¿podemos identificar al niño con riesgo de episodio grave o de recidiva? Rev Esp Pediatr. 2008;64:447-51.
- Pérez Rodríguez MJ, Otheo de Tejada Barasoain E, Ros Pérez P. Bronquiolitis en Pediatría: puesta al día. Inf Ter Sist Nac Salud. 2010;34:311.
- Zang L, Mendoza-Saai RA, Wainwright C, Klassen TP. Nebulized hypertonic saline for acute bronchiolitis: a systematic review. Pediatrics. 2015;136(4):687-701.
- Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. American Academy of Pediatrics. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2015;136(4):687-701.
- Fuentes C, Cornejo G, Bustos R. Actualización en el tratamiento de bronquiolitis aguda: menos es más. Neumol Pediatr. 2016;11:65-70.
- National Collaborating Centre for Women’s and Children's Health (UK). Bronchiolitis: Diagnosis and Management of Bronchiolitis in Children. In: National Institute for Health and Care Excellence [online] [accessed 07/06/2019]. Available at http://www.neumologia-pediatrica.cl/wp-content/uploads/2017/07/tratamiento-broncoquiolitis.pdf
- Friedman JN, Rieder MJ, Walton JM; Canadian Paediatric Society, Acute Care Committee, Drug Therapy and Hazardous Substances Committee. Bronchiolitis: recommendations for diagnosis, monitoring and management of children one to 24 months of age. Paediatr Child Health. 2014;19:485-98.
- Pérez Cid L, San José Valiente B, Quintero Calcaño V, Díaz López G, Mesa Guzmán J, Cañete Díaz A, et al. La bronquiolitis grave en lactantes menores de seis meses es un factor de riesgo para las sibilancias recurrentes. Rev Pediatr Aten Primaria. 2013;15:229-37.






