Vol. 20 - Num. 80
Original Papers
How do our children sleep? Analysis of sleep disorders in children
María Álvarez Casañoa, Juana M.ª Ledesma Albarránb
aPediatra. CS Alcolea. Córdoba. España .
bPediatra. CS Delicias. Málaga. España.
Correspondence: M Álvarez . E-mail: mariaac22@hotmail.com
Reference of this article: Álvarez Casaño M, Ledesma Albarrán JM. How do our children sleep? Analysis of sleep disorders in children. Rev Pediatr Aten Primaria. 2018;20:365-70.
Published in Internet: 10-10-2018 - Visits: 19098
Abstract
Introduction: due the potential impact of sleep disorders in children, the aim of our study was to determine their prevalence in the healthy population.
Materials and methods: we conducted a cross-sectional observational descriptive study. The setting was the Delicias Primary Care Centre in Malaga (Spain). The study universe was the catchment population of this centre aged 2 to 14 years; out of the 2423 eligible patients, we selected 225, a sample size with a precision of 5%, assuming a proportion of 30%. We conducted a survey by applying a validated questionnaire with items rated on a Likert scale, the Bruni Sleep Disturbance Scale for Children. We also collected data for other variables, such as the presence of respiratory disease or the frequent use of aerosol therapy, to assess whether the prevalence of sleep disorders was higher in patients with respiratory problems due to the potential side effects of their medication.
Results: we found an overall prevalence of sleep disorders of 61% in our sample, with a predominance of sleep-wake transition disorders (38%), followed for sleep breathing disorders (18%). We found problems with sleep initiation in 17%, hyperhidrosis in 15%, disorders of arousal in 13% and excessive daytime sleepiness in 10%. Sleep latency lasted longer than 30 minutes in 23% of the sample.
Sleep latency lasted more than 30 minutes in 23% of children.
Conclusions: our study confirms that there is a high prevalence of sleep problems in the paediatric age group. Therefore, the role of the paediatrician in this aspect is of great importance.
Keywords
● Child ● Epidemiology ● Prevalence ● Sleep disordersINTRODUCTION
Sleep disorders are a frequent problem in the paediatric age group, yet most health professionals rarely assess their presence. The prevalence of these disorders in this age group has been estimated at 20% to 30%. Sleep is an essential function in the life of children, and there is growing evidence of the negative repercussions of sleep disturbances in this group, as they affect everyday life by their impact on cognition, mood, the ability to learn and family relationships. Few studies have been conducted on sleep disorders, and the education paediatricians receive on the subject is quite deficient, yet it is estimated that 4% of children are treated with hypnotic drugs at some point during childhood.
The aim of our study was to determine the prevalence of sleep disorders in a population of healthy preschool- and school-aged children managed in a primary care centre in Malaga that received care in the facility for reasons other than sleep. On the other hand, the number of children that frequently use inhaled β-adrenergic, anticholinergic or corticosteroid drugs has been increasing recently. Some of the potential adverse effects of these drugs are tachycardia, tremors, anxiety and nervousness. Thus, in this study we also analysed whether the prevalence of sleep problems was greater in children with respiratory problems requiring aerosol therapy due to those potential adverse effects.
MATERIALS AND METHODS
We conducted a prospective, cross-sectional descriptive study in the Delicias Primary Care Centre of the city of Malaga between May 2016 and February 2017.
The inclusion criteria were age 2 to 14 years, absence of chronic or acute disease that could interfere with sleep, and seeking care in the primary care centre for reasons other than sleep disturbances.
We excluded patients aged less than 2 years or more than 14 years, and patients with underlying disease that could affect sleep onset or maintenance, such as attention-deficit hyperactivity disorder, neurologic disease or thyroid disorders. We ought to note that the one disease that we did not exclude in this regard was asthma, as these patients were a specific target in our study. We also excluded patients treated with drugs that could alter sleep onset or maintenance, such as methylphenidate, systemic corticosteroids, benzodiazepines… We also excluded patients accompanied by a caregiver that was not acquainted with the sleep behaviour of the child because they did not regularly sleep in the same place as the child.
Out of a total eligible population of 2423 patients, we selected 225 to obtain a sample with a precision of 5% and an α level of 0.05, assuming a proportion of sleep disorders of 30%.
We performed a survey by the administration of a validated questionnaire consisting of close-ended, multiple-choice-single-answer questions, the Sleep Disturbance Scale for Children developed by Bruni. This scale is comprised of 27 items that assess for the presence of sleep disorders in the past 6 months. Its internal consistency is higher in controls (0.79) and remains at a satisfactory level in children with sleep disorders (0.71), and the test/retest reliability is satisfactory for the total (r = 0.71) and single item scores. The scale is composed of closed-ended questions rated on a Likert scale designed to detect potential disorders in different areas: initiating and maintaining sleep, disorders of arousal, sleep-wake transition disorders, sleep breathing disorders, excessive somnolence and sleep hyperhidrosis. Each of the 27 items is scored on a scale from 1 to 5, and the total score of the scale is obtained by adding all the item scores. A total score of 39 or greater suggests the presence of a sleep disorder.
We obtained the approval of the Ethics Committee of the regional reference hospital and the signed informed consent of parents, and the questionnaires were anonymised. The questionnaire was administered by the residents in paediatrics that were doing their primary care rotation in our centre at the time of the study. It was completed in the waiting room by the first-degree relative that accompanied the child.
In addition to the variables included in the scale, we collected data for other variables, such as the presence of respiratory disease, like asthma, or the frequent use of aerosol therapy (defined as at least 3 episodes in the past 3 months that required use of inhaled β2-adrenergic drugs). We did not include the information about aerosol therapy in the assessment of sleep, as we only took it into account for the purpose of classifying patients in different groups. Last of all, we entered the data obtained through the questionnaires in a database using the statistical software SPSS version 2.2.
We divided patients into 3 groups by age: 2-3 years, 4-6 years and 7-14 years. We made a descriptive analysis calculating the proportion of patients in each age group, sleep latency and the prevalence of each sleep disorder as well as of sleep disorders overall. We then performed an inferential analysis (Student t, ANOVA, χ2), making comparisons between the group of patients with asthma managed with aerosol therapy and all other patients, among others.
RESULTS
A total of 225 questionnaires were completed. We found a prevalence of sleep disorders in surveyed children of 61%. We classified participants by age into 3 groups: 2-3 years (12%), 4-6 years (37.7%) and 7-14 years (50.2%), applying the same categories used in the study by Pin Arboledas.
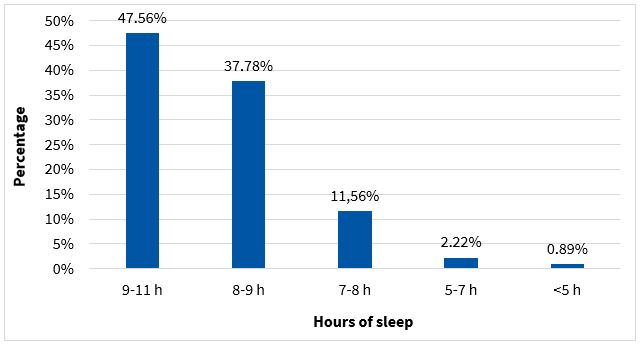
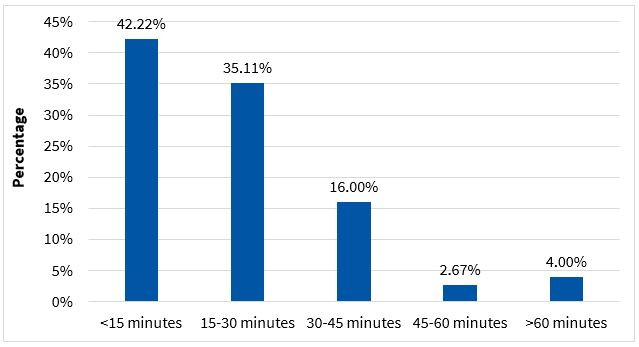
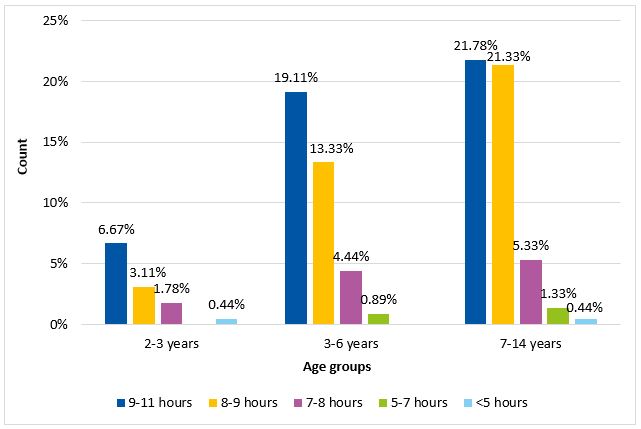
When it came to the duration of sleep, 14.6% of participants slept less than 8 hours (Fig. 1) and the analysis by age group showed that there were more disturbances in sleep duration in younger children (Fig. 2). As for sleep latency, it took 23% of children more than 30 minutes to fall asleep (Fig. 3).
| Figure 2. Association between age and duration of sleep. The proportion of patients with a duration of sleep considered pathological decreased with increasing age |
|---|
 |

The most frequent sleep disturbances were sleep-wake transition disorders (38%), followed by sleep breathing disorders (with suspicion of apnoea-hypopnoea in 18%). We also found problems with sleep onset in 17% of participants, nocturnal hyperhidrosis in 15%, disorders of arousal in 13% and excessive daytime sleepiness in 10%.
We also analysed the association between asthma and sleep disorders by means of the χ2 test, and found a p-value of 0.07, which does not support the hypothesis that the side effects of aerosol therapy are associated with a higher risk of sleep problems. We also analysed the association between aerosol therapy and each sleep disorder separately and found no significant association with any. We used ANOVA to assess the relationship between sleep duration and the presence of a sleep disorder and did not find a significant association.
DISCUSSION
The results our study revealed a high prevalence of sleep disorders in the paediatric population (61%).
Our study aimed at obtaining a general perspective on the prominence of these disorders and on how they may go unnoticed by both family members, who do not usually report these symptoms during medical visits, and health professionals, who do not tend to specifically explore these issues during the history taking.
Among the limitations of the study, we ought to highlight the scarcity of the available literature, in terms of both original and review articles, on sleep disorders in the paediatric age group, as well as the heterogeneity of the instruments used in different studies to assess for these problems, chosen arbitrarily due to the lack of an established gold standard. In this study, we chose the Bruni scale because it has been validated, although it forced us to exclude patients aged less than 2 years. Similarly, when it came to conducting the survey, there was the limitation that the questionnaire was administered to parents by different individuals that had not been specifically trained to do so and may not have understood the scale well, and also the setting where it was administered, which was probably not the most suitable.
The American Academy of Paediatrics has reported that the prevalence of sleep disorders in the paediatric age group ranges between 20% and 30%. However, other studies have described prevalences of up to 45%. In our study, the estimated prevalence of sleep disorders was 61%. The discrepancies between studies is remarkable, and they may stem from the use of different instruments in the assessment of sleep as well as differences in sample size. Comparing our results with those of other series would be difficult, as different criteria have been applied to diagnose sleep disorders, to which we must add the subjectivity of questionnaire responses and the differences in the age ranges and sizes of the samples under study.
CONCLUSIONS
Our study found a greater-than-expected prevalence of sleep disorders in the paediatric age group, as high as 61% in the surveyed children. Therefore, the role of the paediatrician on this issue is essential, and we must emphasise the need that paediatricians routinely assess for sleep disturbances when they take a patient’s history.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
REFERENCES
- Alberola López S, Pérez García I, Casares Alonso I, Cano Garcinuño A, Andrés de Llano JM. C-2. Estudio de las características del sueño en niños preescolares de nuestro medio. Rev Pediatr Aten Primaria. 2010;12:e57.
- American Academy of Sleep Medicine. International classification of sleep disorders, third edition: diagnostic and coding manual. Westchester (ILL): American Academy of Sleep Medicine; 2014.
- Bruni O, Octaviano S, Guidetti V, Romoli M, Innocenzi M, Cortesi F, et al. The Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251-61.
- Estivill E. Situación actual de los trastornos del sueño en niños. Rev Pediatr Aten Primaria. 2002;4:563-5.
- Giménez Badia S, Albares Tendero J, Canet Sanz T, Jurado Luque MJ, Madrid Pérez JA, Merino Andreu M,et al. Trastorno de retraso de la fase del sueño y del despertar. Síndrome de retraso de fase. Rev Pediatr Aten Primaria. 2016;18:129-39.
- Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The children’s sleep habits questionnaire in toddlers and preschool children. J Dev Behav Pediatr. 2008;29:82-8.
- Gradisar M, Dohnt H, Gardener G, Paine S, Starkey K, Menne A, et al. A randomized controlled trial of cognitive-behavior therapy plus bright light therapy for adolescent delayed sleep phase disorder. Sleep. 2011;34:1671-80.
- Hernández Delgado MJ, García Rebollar C. Estudios sobre los hábitos del sueño en niños. Rev Pediatr Aten Primaria. 2006;8:334-6.
- Herzog R, Cunningham-Rundles S. Pediatric asthma: natural history, assessment, and treatment. Mt Sinai J Med. 2011;78:645-60.
- Pedemonte V, Gandaro P, Scavone C. Trastornos del sueño en una población de niños sanos de Montevideo. Primer estudio descriptivo. Arch Pediatr Uruguay. 2014:85:4-8.
- Pin Arboledas G, Soto Insuga V, Jurado Luque MJ, Fernández Gomáriz C, Hidalgo Vicario I, Lluch Rosello A. Insomnio en niños y adolescentes. Documento de consenso. An Pediatr (Barc). 2017;86:165.e1-165.e11.
- Pin Arboledas G, Ugarte Libano R. Lo que el pediatra de Atención Primaria debería saber sobre el sueño. Rev Pediatr Aten Primaria. 2010;12:s219-s230.
- Pin Arboledas G, Ugarte Libano R. Taller de sueño infantil. Herramientas para su interpretación por el pediatra de Atención Primaria. Rev Pediatr Aten Primaria. 2009;11:s399-s404.
- Suárez P, Ortiz P, Ayala Curiel J. El sueño en la infancia. Rev Pediatr Aten Primaria. 2002;4:639-55.
- Tomás Vila M, Miralles Torres A, Beseler Soto B. Versión española del Pediatric Sleep Questionnaire. Un instrumento útil en la investigación de los trastornos del sueño en la infancia. Análisis de su fiabilidad. An Pediatr (Barc). 2007;66:121-8.
- Wilhelmsen-Langeland A, Saxvig IW, Pallesen S, Nordhus IH, Vedaa Ø, Lundervold AJ,et al. A randomized controlled trial with bright light and melatonin for the treatment of delayed sleep phase disorder: effects on subjective and objective sleepiness and cognitive function. J Biol Rhythms. 2013;28:306-21.