The knowledge of paediatricians about laryngomalacia: is it always a trivial disease?
Juan Valencia Ramosa, Alicia Mirás Veigaa, María L. Alonso Álvarezb, Fernando Gómez Sáeza, Pedro P. Oyágüez Ugidosa, Isabel del Blanco Gómeza, Ana Navazo Eguíac
aUnidad de Cuidados Intensivos Pediátricos. Hospital Universitario de Burgos. Burgos. España.
bNeumología-Unidad de Trastornos Respiratorios del Sueño. Hospital Universitario de Burgos. Burgos. España.
cOtorrinolaringología. Hospital Universitario de Burgos. Burgos. España.
Correspondence: J Valencia. E-mail: jvalenra@gmail.com
Reference of this article: Valencia Ramos J, Mirás Veiga A, Alonso Álvarez ML, Gómez Sáez F, Oyágüez Ugidos PP, del Blanco Gómez I, et al. The knowledge of paediatricians about laryngomalacia: is it always a trivial disease? Rev Pediatr Aten Primaria. 2016;70:e63-e72.
Published in Internet: 31-05-2016 - Visits: 36509
Abstract
Background and aims: a national survey was designed to analyze the knowledge and approach of pediatricians to laryngomalacia, due to the perception that some severe cases were overlooked.
Materials and methods: this is a national, transversal, descriptive and analytical study, conducted through an on-line survey. We designed a 16 item questionnaire, and targeted both primary care and specialty pediatricians. The variables included professional data filiation, general knowledge, diagnosis and management of laryngomalacia.
Results: 233 surveys were answered. The most common approach in a case of suspected laryngomalacia was expectant (54.1%), no differences were found in terms of pediatricians experience, neither by years of time worked, nor by the number of laryngomalacia cases previously assisted. Level of general knowledge shown by participants was higher than 89%, while it decreased to 57% when analyzing items covering severe laryngomalacia. 67% were aware of the additional tests to perform in severe cases, and 73.3% were alert for possible comorbidities. 85.6% agreed that non-invasive ventilation is useful in patients with severe laryngomalacia.
Conclusions: the survey shows that laryngomalacia is a well-known condition, although there is not a clear consensus in the initial approach nor in the tools used by pediatricians to base its management. Though the knowledge in general concepts and diagnostics is suitable, it decreases in more specific concepts related to cases of severe laryngomalacia. It would be desirable that clinical guidelines and protocols were developed, to standardize management of laryngomalacia.
Keywords
● Fibroscopy ● Laryngomalacia ● Noninvasive ventilation ● Sleep disorders ● SurveyINTRODUCTION
Traditionally, paediatricians have conceived of laryngomalacia as a disease related to maturation that has no impact on the patient. However, laryngomalacia is severe in up to 20% of children, which can lead to complications such as sleep apnoea-hypopnoea syndrome (SAHS), chest wall deformity, failure to thrive, etc.1
Laryngomalacia refers to the inward collapse of the supraglottic structures during the inspiratory phase of respiration. Its actual incidence is unknown. Its epidemiology is not well established,2 but it is the most common cause of stridor in newborns, affecting 45% to 75% of all infants with congenital stridor.3 As for its aetiology, it has been proposed that it is caused by a defect in the maturation of pharyngolaryngeal structures. Based on the high prevalence of neuromuscular disorders in these patients4 and published case series on laryngomalacia secondary to neurologic abnormalities,5 the theory that currently prevails is that of a neuromuscular aetiology.
There is a high prevalence of respiratory comorbidities in patients with laryngomalacia, such as laryngeal dyskinesia, vocal fold paralysis, subglottic stenosis and tracheomalacia,6 which are more frequent in severe cases.7
Most infants with laryngomalacia have mild symptoms and a benign course of disease that resolves by the age of 12 to 24 months.3
The diagnosis is based on clinical findings, reserving diagnostic tests for severe cases. The disease may present with comorbidities, most frequently gastroesophageal reflux and neurologic involvement. Other conditions that impact its prognosis are the presence of synchronous airway lesions, congenital heart disease or genetic syndromes or abnormalities.8
The management of laryngomalacia depends on its severity, which is not determined by the severity of stridor, but by the degree of airway obstruction. Thus, the spectrum can be divided into mild, moderate and severe.9 Mild disease accounts for 40% of the cases and typically presents with inspiratory stridor that usually resolves spontaneously under watchful waiting. Moderate disease accounts for another 40% of cases and typically presents with digestive comorbidities, frequently requiring anti-reflux treatment. Lastly, there are severe cases in which surgery is indicated, usually a supraglottoplasty.8 Signs of severity include poor weight gain (due to feeding difficulties and the increased basal metabolism associated to breathing difficulties), episodes of respiratory distress with intercostal or xyphoid retraction, obstructive sleep apnoea and episodes of suffocation.2 Some patients with severe laryngomalacia may develop pectus excavatum10 due to the intense xyphoid retractions, and even chronic respiratory failure leading to pulmonary hypertension and heart failure.11
Therefore, patients with severe laryngomalacia require a flexible fiberoptic laryngoscopic examination of the upper and lower airways to confirm the diagnosis, assess the degree of obstruction and rule out synchronous airway lesions,6 and performance of respiratory polygraphy to determine the apnoea/hypopnoea index (AHI).12 Patients with a high AHI require active therapeutic measures, which may include curative surgical treatment (supraglottoplasty)8 or the temporary administration of noninvasive mechanical ventilation (NIMV), which allows the patient to maintain an adequate breathing pattern while laryngomalacia improves over time.
Since we had the subjective impression that the severity of some serious cases of laryngomalacia in patients admitted to our unit had been previously underestimated, we thought it would be interesting to find out the extent to which this was true. To test our hypothesis, we designed a survey aimed at paediatricians working in any type of setting (primary care and hospital, and within the latter, in any subspecialty). We included adjunct physicians and paediatrics residents (MIR). Our goal was to learn the approach to the diagnosis and treatment of laryngomalacia of paediatricians, stratified by work setting: primary care (PC), hospital ward/outpatient services, paediatric intensive care unit (PICU), neonatal unit, and paediatric emergency department.
MATERIALS AND METHODS
We conducted a nationwide cross-sectional descriptive analytical study by means of a voluntary and anonymous online survey. The criterion for inclusion was to be a specialist in paediatrics or a medical resident (MIR) in paediatrics, and the study included both hospitalists and PC paediatricians. The questionnaire consisted of 16 items distributed in four sections: general knowledge, diagnosis, comorbidities and NIMV. We collected the data between January 10 and February 24, 2015. The variables under study were the respondent’s professional characteristics, general knowledge on laryngomalacia, knowledge on its diagnosis, and knowledge of its potential interdisciplinary management.
We disseminated the survey through the websites of different paediatrics associations: The Spanish Society of Outpatient and Primary Care Paediatrics (Sociedad Española de Pediatría Extrahospitalaria y Atención Primaria [SEPEAP]), the Asociación Vasca de Pediatría de Atención Primaria (Basque Association of Primary Care Paediatrics [AVPAP/AEPap]), the Paediatrics Society of Galicia (Sociedad de Pediatría de Galicia [SOPEGA]), the Paediatrics Society of Asturias, Cantabria y Castilla y León (Sociedad de Pediatría de Asturias, Cantabria y Castilla y León [SCCALP]) and the Spanish Society of Paediatric Intensive Care Medicine (Sociedad Española de Cuidados Intensivos Pediátricos [SECIP]). These websites featured a link to the survey that could be accessed by those paediatricians that voluntarily chose to respond. We published the survey online using Google Forms®.
We performed the statistical analysis with the software SPSS® 20.0 (SPSS Inc; Chicago, Illinois, United States). We have expressed the results of the descriptive analysis as absolute frequencies and percentages. For the purpose of comparison, we categorised paediatricians based on work setting (PC, hospital wards/outpatient services, PICU, Neonatology, and Paediatric Emergency Department), years of experience (0–5, 6–15, 16–25 or > 25, excluding years spent as residents in training) and the number of cases of laryngomalacia managed in the past (0, 1–5 or > 5). We compared the variables by means of one-factor ANOVA, using Snedecor’s F-test, and considered p-values of less than 0.05 statistically significant.
Access to the survey data was restricted to the researchers of this study.
RESULTS
Characteristics of respondents and experience in the management of laryngomalacia
We obtained responses from 233 paediatricians, of whom 86.6% (202/233) were adjunct specialists and 13.4% (31/233) residents in training (MIR). Of the former, 42% (98/233) worked in PC centres and the rest (135/233) in hospitals. Of those working in hospitals, 28.8% (39/135) were employed in secondary/local hospitals and the rest (96/135) in tertiary hospitals; 29.6% (40/135) worked in the wards and outpatient clinics, 22.2% (30/135) in PICUs, 11.1% (15/135) in neonatal units, and 11.1% (15/135) in paediatric emergency departments.
The years of professional experience in paediatrics were less than 5 in 24.5% of participants (57/203), 6 to 15 years in 33% (67/203), 16 to 25 years in 21.1% (43/203) and more than 25 years in 17.7%(36/203).
As for the resources on which paediatricians based the management of laryngomalacia, 30.9% based it on clinical guidelines (30.9%, 72/233), 27.5% on their prior clinical experience (64/233), 16.7% on protocols (39/233), 13.7% on guidelines and clinical experience (32/233), 4.3% on guidelines and protocols (10/233), 3.9% on guidelines, protocols and experience (9/233), and 2.6% on protocols and experience (6/233).
General knowledge on laryngomalacia
When asked about their initial approach to the management of a case of suspected laryngomalacia, 18.5% (43/232) reported referring the patient to Otorhinolaryngology, 15.5% (36/232) referring the patient to Pulmonology, 0.4% (1/232) referring the patient to the paediatric emergency department, 53.6% (125/232) using watchful waiting, and 11.2% (26/232) none of the above measures.
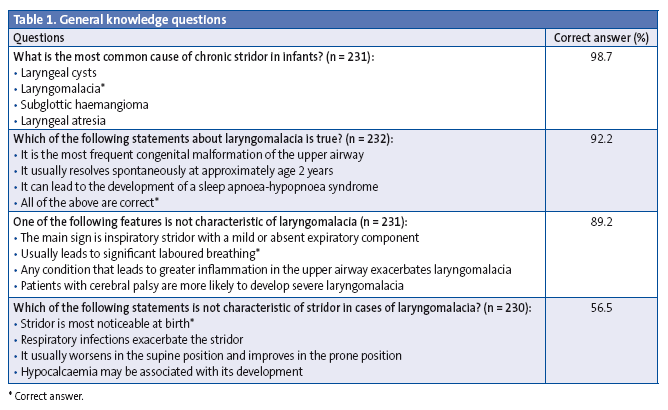
We asked four general knowledge questions. The first three addressed basic knowledge and were answered correctly by nearly 90% of respondents. Table 1 presents each of these questions and the percentage of correct answers to each. The percentage of correct answers to question 4, in responding that the statement that stridor in laryngomalacia is more pronounced at birth is incorrect, was 56.5% (130/230), while 1.7% of respondents did not think that respiratory infections exacerbated stridor, 24.9% did not think that hypocalcaemia may be associated with the development of laryngomalacia, and 16.3% believed that laryngomalacia improved in the supine position and worsened in the prone position, with all last three statements being incorrect.
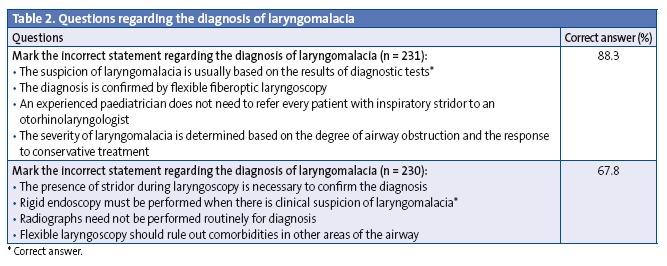
Questions 5 and 6 assessed knowledge pertaining to the diagnosis of laryngomalacia. The percentage of correct answers to question 5 was 88.3% (204/231), with most paediatricians agreeing that laryngomalacia is diagnosed on the basis of clinical manifestations. In question 6, which referred to the potential use of diagnostic tests, 67.8% (156/230) correctly answered that rigid endoscopy should not be used for diagnosis, while 27.8% (64/230) did not believe that the presence of stridor during laryngoscopy was necessary to confirm the diagnosis, 3.4% (8/230) believed that a chest radiography was required to confirm the diagnosis, and 0.9% (2/230) believed that the statement that flexible laryngoscopy had to rule out respiratory comorbidities was false, with the last three answers all being incorrect.
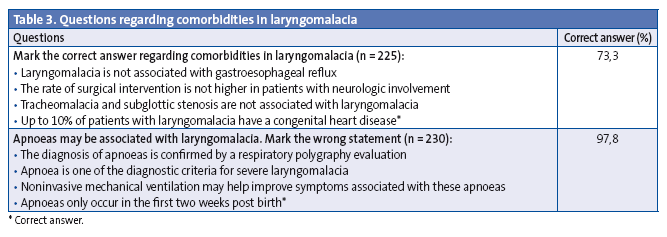
The questions that followed referred to comorbidities in laryngomalacia. Question 7 was answered correctly by 73.3% (165/225) of paediatricians that agreed that congenital heart diseases may be present in up to 10% of patients with laryngomalacia, with incorrect answers stating that laryngomalacia is not associated with reflux (selected as correct by 14.7%), that the percentage of patients with neurologic involvement that undergo surgery is not higher (selected as correct by 5.3%) and that tracheomalacia and subglottic stenosis are not associated with laryngomalacia (marked as correct by 6.7%). Question 8, which concerned apnoea, was answered correctly by 97.8% of respondents (225/230) that agreed that the presence of apnoeas is confirmed by means of respiratory polygraphy, that apnoea is one of the diagnostic criteria for severe laryngomalacia, and that NIMV could improve the symptoms associated with apnoeas.
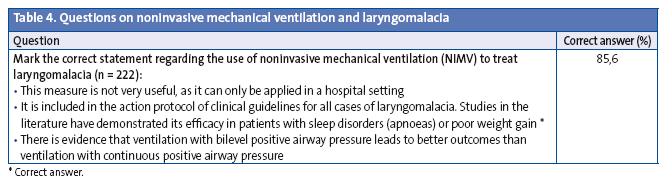
As for the management of laryngomalacia with NIMV, 85.6% (190/222) of respondents answered that NIMV is useful in patients with severe laryngomalacia in question 9.
Tables 1 through 4 provide more detailed information on the answers given to the questions posed in this survey arranged, arranged in sections pertaining to general knowledge, diagnosis, comorbidities and the use of NIMV.
 Comparison of answers based on the work setting of respondents
Comparison of answers based on the work setting of respondents
Table 5 shows the results of the comparison of the percentage of correct answers to each question by the work setting/subspecialty of the paediatricians. We did not find differences between paediatricians working in different settings in the answers to general knowledge questions (1, 2 and 3) and comorbidity questions (7 and 8). We did find differences by work setting in the answers to questions 4 (specific knowledge) and 5 (diagnosis), with higher percentages of correct answers to both questions in paediatricians working in neonatal units and to question 5 in emergency care paediatricians, although the differences were not statistically significant.
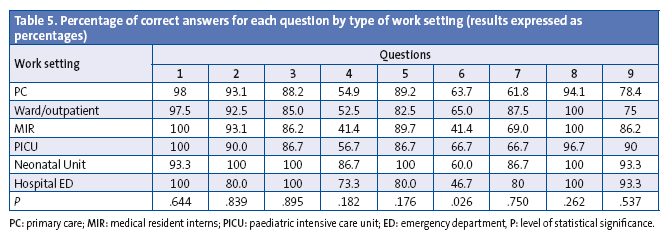
Question 6, which also referred to the diagnosis of laryngomalacia, was the only one in which we found statistically significant differences in the percentage of correct answers between paediatricians working in different settings (P = .026).
Question 9, which concerned the use of NIMV, had the lowest response rate (n = 222), and was answered correctly more frequently by paediatricians working in emergency departments, PICUs and neonatal units, although the differences were not statistically significant.
Comparison of the approach to a case of laryngomalacia based on the number of cases seen previously and the years of professional experience
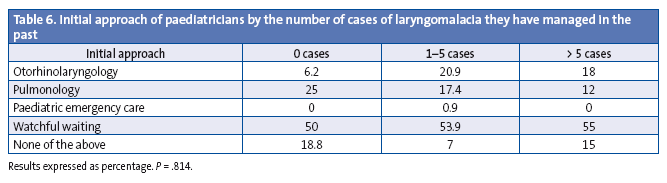
We did not find statistically significant differences in the initial approach of paediatricians based on the number of laryngomalacia cases that they had managed in the past, with the same percentage of paediatricians reporting management by watchful waiting in all categories (Table 6).
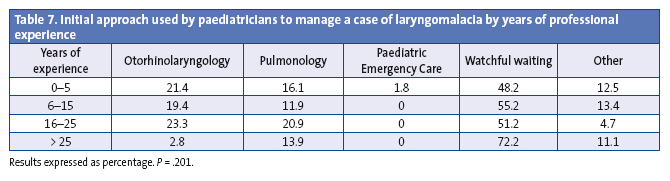
We also found no statistically significant differences in the initial approach based on the years of professional experience (Table 7), although the highest-seniority subset was the one that used watchful waiting most frequently (72.2%) and referred patients to Otorhinolaryngology least frequently (2.8%).
Tools (guidelines and/or protocols in different units and/or professional experience) used in the management of laryngomalacia based on years of work experience
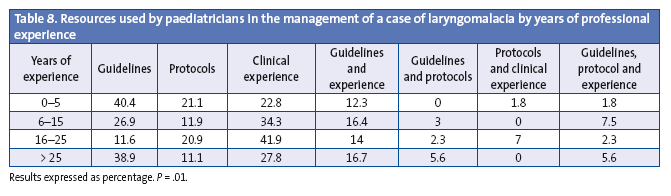
Table 8 shows that paediatricians that have been working for less than five years or more than 25 years base their management exclusively on their clinical experience less frequently than those with an intermediate seniority (22.8% and 27.8% vs 41.9% and 34.3%; P = .014). Less-experienced paediatricians used protocols and guidelines more frequently (40.4% and 21.1%, respectively).
DISCUSSION
Our survey reflects the overall knowledge and approach to laryngomalacia of paediatricians in Spain. Our sample was representative, as the study included both paediatricians working in PC and hospitals, with the latter including paediatricians in regional and tertiary care hospitals and with different subspecialties. The respondents also had different levels of professional experience.
When it came to the approach of respondents to laryngomalacia, the survey reflected a considerable variability, with the most frequent answer being watchful waiting. This suggests that there is no clear consensus on how to manage these patients, and that the prevailing approach is to watch and wait because the disease is considered a self-limiting maturational process. This was independent of the respondents’ professional experience in terms of the number of cases of laryngomalacia managed in the past or of the years spent working in the profession. While the percentage of paediatricians that reported a watchful waiting approach was highest in the group with more than 25 years of experience, the differences were not statistically significant, which supports the hypothesis that paediatricians uphold the traditional view of laryngomalacia as an uncomplicated disease.
Among the possible resources for the management of laryngomalacia, paediatricians most frequently reported using clinical guidelines, followed by their clinical experience. This was unexpected considering that there are no clinical guidelines on the management of these patients, and explains why up to 27.9% of respondents report managing them based solely on their own clinical experience.
The percentage of correct answers to the first three questions, which concerned general knowledge on laryngomalacia, was high; however, it dropped to 56.5% in question 4, which addressed more specific knowledge and focused on severe cases, showing that paediatricians have a general understanding of what laryngomalacia is, but are less knowledgeable when it comes to severe cases of the disease, which may account for up to 20% of the total9 and may lead not only to severe airway obstruction but also to feeding disorders, and are the cases in which surgery is indicated based on the scientific literature.3 The percentage of correct answers was also low (67.8%) for question 6; this question had to do with diagnostic tests, which are indicated precisely in more severe cases, reinforcing the notion that paediatricians are least knowledgeable about severe laryngomalacia.
Although severe cases theoretically require care in a hospital setting, we did not observe any differences in the knowledge of laryngomalacia between paediatricians working in different settings except in question 6, in which the percentage of correct answers was higher in respondents working in neonatal units and emergency departments, a difference that we could not account for.
The last question, which explored the use of NIMV in the management of laryngomalacia, is the one that paediatricians answered the least frequently (222/233), possibly because most of the respondents do not use NIMV. As expected, the percentage of correct answers was higher in paediatricians that are familiar with the use of NIMV, such as those working in PICUs, neonatal units and emergency departments. As for treatment, there are two possible approaches: medical and surgical. Surgery is indicated in cases of severe laryngomalacia or failure of medical treatment. Surgery has evolved from the first resections of the excess of mucosa of the aryepiglottic folds proposed by Variot in 1898 to the endoscopic techniques used today,14 which are not completely free of complications.15 Until now, the use of NIMV has been proposed as an adequate treatment for patients with severe laryngomalacia complicated by SAHS, poor weight gain or extreme cases with pulmonary hypertension, when the patient cannot undergo surgery or as a bridge to the intervention.3,16
There are few published data on the use of NIMV as the sole treatment in cases of severe laryngomalacia. In 2001, Fauroux et al published a study in which they used NIMV as an alternative to tracheostomy, as NIMV, in particular pressure support associated with positive end-respiratory pressure, had been recognised as an efficient treatment for upper airway obstruction associated with alveolar hypoventilation.16
Since our hospital cannot perform surgeries of the respiratory tract, in cases of suspected severe laryngomalacia the PICU arranges the performance of a polysomnogram to assess for the presence of secondary apnoeas and a fiberoptic laryngoscopic examination of the upper and lower airways to determine the degree of obstruction. Sleep apnoea-hypopnoea is diagnosed if the AHI is 3 or greater. However, there is no consensus for the diagnosis of laryngomalacia, and treatment is indicated based on the presence of SAHS and symptom severity.12,17
In this manner, we identify the patients in whom NIMV is indicated and determine the pressure needed to prevent the collapse of the airway. Patients that require it are discharged for at-home management with NIMV, after educating parents on its use. Performance of prospective randomised double-blind studies would be beneficial, as they would allow comparing the outcomes of surgery and management with NIMV.
CONCLUSIONS
The traditional notion of laryngomalacia as a maturational process that is self-limiting and resolves spontaneously continues to prevail among paediatricians, regardless of their work setting (PC or Inpatient), the years of professional experience and the number of patients with laryngomalacia that they have treated. The disparity in the initial approach to its management, the fact that one out of every four paediatricians treats these patients empirically and a reduction in the percentage of correct answers to questions concerning more severe presentations evince the uncertainty that surrounds this disease. Clinical guidelines and protocols should be developed to facilitate the standardisation of the management of laryngomalacia, underscoring the need to identify patients with severe disease requiring a thorough evaluation and treatment with NIV or supraglottoplasty.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS: AHI: apnoea/hypopnoea index • AVPAP/AEPap: Asociación Vasca de Pediatría de Atención Primaria (Basque Association of Primary Care Paediatrics) • MIR: medical residency intern • NIMV: noninvasive mechanical ventilation • PC: Primary Care • PICU: Paediatric Intensive Care Unit • SAHS: sleep apnoea-hypopnoea syndrome • SCCALP: Sociedad de Pediatría de Asturias, Cantabria y Castilla y León (Society of Paediatrics of Asturias, Cantabria and Castilla y León) • SECIP: Sociedad Española de Cuidados Intensivos Pediátricos (Spanish Society of Paediatric Intensive Care Medicine) • SEPEAP: Sociedad Española de Pediatría Extrahospitalaria y Atención Primaria (Spanish Society of Ambulatory and Primary Care) • SOPEGA: Sociedad de Pediatría de Galicia (Society of Paediatrics of Galicia.
ACKNOWLEDGMENTS
We want to thank the Paediatric Intensive Care Unit and Dr Mirás in particular for her efforts and patience. Also, the Department of Pulmonology-Sleep Unit and the Department of Otorhinolaryngology for their close cooperation and contributions to the manuscript. Lastly, we thank Dr Cilla for her disinterested collaboration.
REFERENCES
- Richter GT, Wootten T, Rutter MJ, Thompson MD. Impact of supraglottoplasty on aspiration in severe laryngomalacia. Ann Otol Rhinol Laryngol. 2009;118:259-66.
- Ayari S, Aubertinb G, Girschig H, Van Den Abbeeled T, Mondaine M. Pathophysiology and diagnostic approach to laryngomalacia in infants. Eur Ann Otorhinolaryngol Head Neck Dis. 2012;129:257-63.
- Richter GT, Thompson DM. The surgical management of laryngomalacia. Otolaryngol Clin North Am. 2008;41:837-64.
- Richter GT, Thompson DM. Laryngomalacia. En: Haver K, Brigger M, Hardy S, Hartnick CJ, (eds). Pediatric aerodigestive disorders. San Diego: Plural Publishing; 2009. p. 165-87.
- Archer SM. Acquired flaccid larynx. A case report supporting the neurologic theory of laryngomalacia. Arch Otolaryngol Head Neck Surg. 1992;118:654-7.
- Mancuso RF, Choi SS, Zalzal GH, Grundfast KM. The search for the second lesion. Arch Otolaryngol Head Neck Surg. 1996;122:302-6.
- Dickson JM, Richter GT, Meinzen-Derr J. Secondary airway lesions in infants with laryngomalacia. Ann Otol Rhinol Laryngol. 2009;118:37-43.
- Landry AM, Thompson DM. Laryngomalacia: disease presentation, spectrum, and management. Int J Pediatr. 2012:753526.
- Thompson DM. Abnormal sensorimotor integrative function of the larynx in congenital laryngomalacia: a new theory of etiology. Laryngoscope. 2007;117:1-33.
- Lane RW, Weider DJ, Steinem C. Laryngomalacia. A review and case report of surgical treatment with resolution of pectus excavatum. Arch Otolaryngol. 1984;110:546-51.
- Jacobs IN, Teague WG, Bland Jr JW. Pulmonary vascular complications of chronic airway obstruction in children. Arch Otolaryngol Head Neck Surg. 1997;123:700-4.
- Alonso-Álvarez ML, Canet T, Cubell-Alarco M, Estivill E, Fernández-Julián E, Gozal D, et al. Documento de consenso del síndrome de apneas-hipopneas durante el sueño en niños. Arch Bronconeumol. 2011;47:2-18.
- Thorne MC, Garetz SL. Laryngomalacia: Review and Summary of Current Clinical Practice in 2015. Paediatr Respir Rev. 2016;17:3-8.
- Senders CW, Navarrete EG. Laser supraglottoplasty for laryngomalacia: are specific anatomical defects more influential than associated anomalies on outcome? Int J Pediatr Otorhinolaryngol. 2001;57:235-44.
- Ayari S, Aubertin G, Girschig H, Van Den Abbeele T, Denoyelle F, Couloignier V, et al. Management of laryngomalacia. Eur Ann Otorhinolaryngol Head Neck Dis. 2013;130:15-21.
- Fauroux B, Pigeot J, Polkey MI, Roger G, Boulé M, Clément A, et al. Chronic stridor caused by laryngomalacia in children: work of breathing and effects of noninvasive ventilatory assistance. Am J Respir Crit Care Med. 2001;15:164:1874-8.
- Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130:e714-55.






