Vol. 25 - Num. 97
Originales
COVID-19 en Pediatría: descripción clínica y microbiológica de los pacientes ingresados en un hospital terciario
Celia Rasero Bellmunta, M.ª Carmen Vicent Castellóa, Amelia Herrero Galianaa, Javier González de Diosb
aServicio de Pediatría. Hospital General Universitario Dr. Balmis. Alicante. España.
bServicio de Pediatría. Hospital General Universitario Dr. Balmis. Alicante. Facultad de Medicina. Universidad Miguel Hernández. Alicante. Instituto de Investigación Sanitaria y Biomédica de Alicante (ISABIAL). España.
Correspondencia: C Rasero. Correo electrónico: celiarasero68@gmail.com
Cómo citar este artículo: Rasero Bellmunt C, Vicent Castelló MC, Herrero Galiana A, González de Dios J. COVID-19 en Pediatría: descripción clínica y microbiológica de los pacientes ingresados en un hospital terciario . Rev Pediatr Aten Primaria. 2023;25:21-30.
Publicado en Internet: 14-03-2023 - Número de visitas: 14859
Resumen
Introducción: desde el inicio de la pandemia por el virus SARS-CoV-2 una de las grandes cuestiones que se ha formulado es qué papel desempeñan los niños en el control y manejo de la pandemia y cómo esta les ha afectado. Hay mucha bibliografía acerca de los síntomas y complicaciones que puede presentar esta población, pero poca de cómo ha sido el curso clínico de la infección en los niños ingresados en hospitales de tercer nivel y su impacto asistencial.
Material y métodos: se han analizado descriptivamente las historias clínicas de los niños ingresados en el Hospital General Doctor Balmis de Alicante (España) desde enero de 2020 hasta julio de 2022. Se han analizado paralelamente los datos microbiológicos del SARS-CoV-2, variantes y linajes, desde agosto de 2021 hasta agosto de 2022.
Resultados: se analizaron un total de 114 niños ingresados con diagnóstico de infección por SARS-CoV-2, de los cuales la mayoría tenían menos de 12 meses y eran de procedencia española. Los ingresos se distribuyeron de forma cronológica siguiendo un modelo de “olas”, siendo el motivo más frecuente la constatación del virus SARS-CoV-2 en las pruebas realizadas. El tratamiento que más frecuentemente recibieron durante el ingreso fueron los antibióticos orales. La mayor parte de los niños no tenían comorbilidades y no desarrollaron complicaciones. La variante mayoritaria fue ómicron y el linaje el BA.1.
Discusión: los lactantes parecen ser más vulnerables a la infección por SARS-CoV-2 y las manifestaciones clínicas en este grupo de edad conllevan mayor probabilidad de ingreso. El desarrollo de complicaciones, necesidad de oxigenoterapia, ventilación mecánica e ingreso en UCI es mínimo en población pediátrica. El manejo de la infección difiere sustancialmente con el de los adultos, lo que se corresponde con tratamientos menos agresivos.
Palabras clave
● Diagnóstico ● Pediatría ● SARS-CoV-2 ● Tratamiento ● VariantesINTRODUCCIÓN
El 8 de diciembre de 2019 fue diagnosticado el primer caso de infección por SARS-CoV-2 en Wuhan, ciudad situada al sur de China1. Poco a poco se fueron diagnosticando más casos y se averiguó que habían tenido una exposición común en un mercado de marisco, pescado y animales vivos. Sin embargo, no fue hasta el 7 de enero de 2020 cuando el agente causal fue identificado. En España, el primer caso registrado fue el 31 de enero de 2021 y el 11 de marzo de ese año la OMS declaró el estado de pandemia. En España, el Gobierno decretó tres días más tarde, el 14 de marzo, el estado de alarma. Un mes más tarde habían sido diagnosticados en todo el mundo un total de 1 996 681 casos (177 633 en España), con un total de 127 601 fallecidos (18 579 en España). La cifra actual (noviembre de 2022) es de 548 935 393 casos (13 529 643 en España) y 6 350 765 fallecidos (115 239 en España). En esta pandemia, dos preguntas han sido claves en Pediatría: ¿cómo ha afectado a nuestra población pediátrica? y ¿son los niños un elemento fundamental en el control y manejo de la pandemia?
En la infancia se suele adquirir la infección por exposición doméstica, ya que normalmente los adultos suelen actuar como caso índice. Parecen excretar el virus con cargas virales nasofaríngeas comparables o superiores a las de los adultos. Además de las secreciones nasofaríngeas, también hay excreción fecal durante varias semanas tras el diagnóstico, lo que podría suponer un reto para el control de la transmisión de la infección2,3.
La mayor parte de los niños suelen ser asintomáticos (en torno a un 15-42%) o sintomáticos con síntomas leves. Todavía se desconocen los mecanismos exactos por los que tienen un curso clínico más leve que los adultos y se han postulado varias teorías: que pueda deberse a una respuesta inmune menos intensa al virus con menor liberación de citoquinas; que la interacción entre el virus y el tracto respiratorio de los niños pueda conducir a una menor carga viral; que el receptor de la ACE2 (enzima convertidora de la angiotensina tipo 2) tenga un comportamiento diferente en los diferentes aparatos y sistemas respecto al de los adultos; que la respuesta de las mucosas en los niños sea más temprana; etc.
Los síntomas se suelen dividir en dos grandes grupos de edad: menores de 12 meses y mayores de 12 meses. En los niños menores de 12 meses los síntomas predominantes son rechazo de la alimentación, fiebre sin foco, bronquiolitis, apneas. En los mayores de 12 meses los síntomas son similares a los de los adultos: síntomas del tracto respiratorio (tos, rinorrea, dificultad respiratoria), síntomas gastrointestinales (diarrea, vómitos, dolor abdominal), manifestaciones neurológicas (cefalea, encefalopatía aguda, convulsiones, debilidad), síntomas cutáneos (erupciones maculopapulares, urticariales y vesiculares, livedo reticularis transitoria, descamación acral), síntomas cardiovasculares (insuficiencia cardiaca, arritmias, miocarditis, pericarditis, shock cardiogénico, embolia pulmonar), síntomas renales (lesión renal aguda)4.
En lo que respecta a las complicaciones, también son infrecuentes. Sin embargo, se deben conocer para detectar precozmente e intentar evitar las secuelas asociadas. El síndrome inflamatorio multisistémico en niños (SIMP, en inglés MIS-C) es una enfermedad rara pero grave asociada a la infección por SARS-CoV-2; las características clínicas incluyen fiebre persistente, hipotensión, síntomas gastrointestinales, erupción cutánea, miocarditis y hallazgos de laboratorio asociados con el aumento de la inflamación. El llamado “COVID largo” consiste en la persistencia de síntomas cuatro o más semanas tras la infección; los síntomas más frecuentes son fatiga, debilidad, dolor de cabeza, trastornos del sueño, dolor muscular y articular, problemas respiratorios, arritmias, alteración del sentido del olfato o del gusto.
Hay mucha bibliografía acerca de la infección por SARS-CoV-2 en la población pediátrica. Sin embargo, poco hay descrito acerca de cómo ha sido el curso clínico de la infección en los niños ingresados en hospitales de tercer nivel y cuál ha sido su impacto asistencial. El objetivo primario de este trabajo es describir las características clínicas y microbiológicas de la infección por SARS-CoV-2 en los pacientes pediátricos ingresados en el Hospital General Universitario Doctor Balmis de Alicante durante la pandemia (desde enero de 2020 hasta julio de 2022); y el objetivo secundario, valorar cuál ha sido el impacto clínico de la enfermedad COVID-19 en nuestro Servicio de Pediatría.
MATERIAL Y MÉTODOS
Se solicitó al Servicio de Admisión del hospital un registro de todos los pacientes pediátricos (≤14 años) ingresados con diagnóstico de infección por SARS-CoV-2 desde el inicio de la pandemia (enero 2020) hasta julio del año 2022.
Se recogió la información acerca de la edad, procedencia (España o extranjero), fecha de ingreso y alta, diagnóstico principal al ingreso, síntomas de consulta y durante la hospitalización (fiebre, tos, rinorrea, disnea, dolor abdominal, diarrea, náuseas, vómitos, rechazo ingesta, mialgias, cefalea…), comorbilidades, necesidad de ingreso en UCI (Unidad de Cuidados Intensivos), oxigenoterapia y ventilación mecánica, complicaciones, así como los tratamientos que recibieron.
Desde el Servicio de Microbiología de nuestro hospital (centro provincial de referencia para la secuenciación de las muestras de virus COVID-19) consultamos el resultado de las muestras secuenciadas en la población pediátrica, ingresada o no, en un periodo de un año (agosto de 2021 a agosto de 2022).
Para llevar a cabo el análisis descriptivo de los datos, se utilizó el programa R Commander.
RESULTADOS
Se contabilizaron un total de 161 pacientes ingresados desde el inicio de la pandemia con diagnóstico de infección por SARS-CoV-2 durante nuestro periodo de 31 meses de estudio. Se excluyeron del análisis aquellos pacientes ingresados en los cuales, tras consultar la historia clínica, el motivo de ingreso no era la infección por COVID-19, sino otros procesos, y el hallazgo del SARS-CoV-2 fue casual en el contexto de las pruebas realizadas al ingreso (ej.: preoperatorios). Tras este proceso de selección, la cifra total de pacientes pediátricos con enfermedad por COVID-19 fue de 114.
Variables analizadas
- Edad. El 49% de los niños ingresados en nuestro Servicio fueron menores de 12 meses (Tabla 1). Dentro de este grupo, el 60% tenían edades comprendidas entre 1 y 2 meses.
Tabla 1. Distribución de la frecuencia de las edades de 114 niños ingresados por COVID-19 hasta julio de 2022 Edad Frecuencia Porcentaje <12 meses 56 49% <1 mes 5 8% 1 mes 21 37% 2 meses 13 23% 3 meses 6 11% 4 meses 2 4% 5 meses 2 4% 6 meses 4 7% 7 meses 0 0% 8 meses 1 2% 9 meses 2 4% 10 meses 0 0% 11 meses 0 0% 1 año 10 9% 2 años 9 8% 3 años 8 7% 4 años 8 7% 5 años 3 3% 6 años 3 2% 8 años 2 2% 9 años 3 2% 10 años 3 3% 11 años 2 2% 12 años 2 2% 13 años 5 4% 
- Procedencia. El 74% de los pacientes habían nacido en España y el resto procedían de diferentes países del extranjero (Argelia, Colombia, Argentina, Ecuador, etc.).
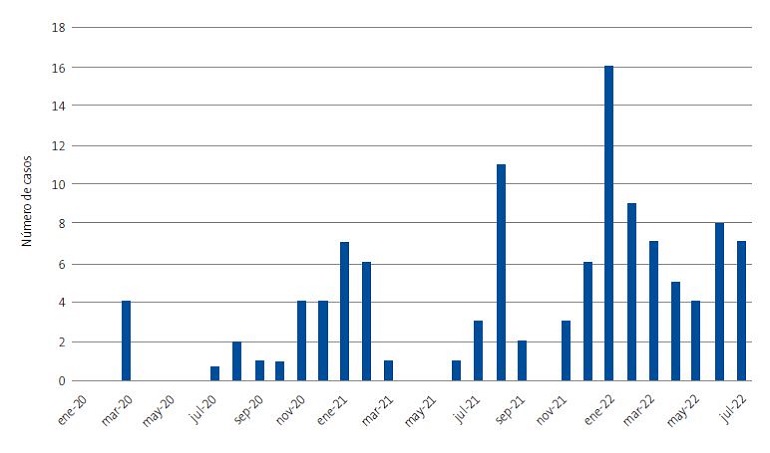
- Fechas y pacientes ingresados. La distribución cronológica de los pacientes ingresados siguió un modelo de “olas”, coincidiendo con aquellas que se han ido describiendo en la población general (Figura 1). El mes donde se constató el máximo número de ingresos fue en enero de 2022, con un total de 14, no habiendo ningún ingreso en los meses de enero y mayo de 2020 y mayo de 2021.
- Motivo de ingreso. La causa por la que ingresaron un 68% de los pacientes fue la constatación del virus SARS-CoV-2 en las pruebas realizadas, tal como se aprecia en la Tabla 2. Otros diagnósticos al ingreso fueron broncoespasmo (10%), síndrome febril (6%), gastroenteritis aguda (5%), neumonía (5%) y SIMP (MIS-C) (4%).
Tabla 2. Motivos de ingreso de 114 niños ingresados por COVID-19 hasta julio de 2022 Diagnóstico Frecuencia Porcentaje Infección COVID-19 78 68% Broncoespasmo 11 10% Síndrome febril 7 6% Gastroenteritis aguda 6 5% Neumonía 6 5% SIMP (MIS-C) 5 4% MIS-C: multisystem inflammatory syndrome in children; SIMP: síndrome inflamatorio multisistémico en niños. 
- Síntomas de la infección por SARS-CoV-2. El síntoma más frecuente (al ingreso y durante el mismo) fue la fiebre, presente en un 72% de los niños; el segundo, la tos (54%); y en tercer lugar, la rinorrea (52%). Síntomas menos frecuentes fueron rechazo de la ingesta, diarrea, disnea, náuseas y vómitos, dolor abdominal, mialgias y cefalea (Tabla 3).
Tabla 3. Síntomas de la infección por SARS-CoV-2 en 114 niños ingresados por COVID-19 hasta julio de 2022 Síntomas Frecuencia Porcentaje Fiebre 83 72% Tos 61 54% Rinorrea 60 52% Rechazo ingesta 43 38% Diarrea 27 24% Disnea 27 24% Náuseas/vómitos 23 20% Dolor abdominal 9 8% Mialgias 7 6% Cefalea 4 4% 
- Comorbilidades. De todos los pacientes ingresados, solo un 23% presentó comorbilidades (Tabla 4). Las más frecuentes fueron las relacionadas con la inmunodepresión, tales como leucemias, linfomas, inmunodeficiencias primarias o tratamiento inmunosupresor tras un trasplante. Otras comorbilidades fueron neurológicas (síndrome de Rett, síndrome de West, malformaciones del sistema nervioso central), respiratorias (asma infantil), renales (pacientes monorrenos), psiquiátricas (depresión en tratamiento) y genéticas (síndrome L1, síndrome de Down).
Tabla 4. Distribución de comorbilidades y tipos en 114 niños ingresados por COVID-19 hasta julio de 2022 Comorbilidad Frecuencia Porcentaje No 89 77% Sí 25 23% Tipo de comorbilidad Inmunodepresión 12 46% Neurológica 5 19% Respiratoria 4 15% Infecciosa 1 4% Renal 1 4% Psiquiátrica 1 4% Otras* 2 8% *Se incluyen en “otras”: comorbilidades renales (pacientes monorrenos), psiquiátricas (depresión en tratamiento), genéticas (síndrome L1, síndrome de Down). 
- Necesidad de oxigenoterapia, ventilación mecánica e ingreso en UCI pediátrica. La mayor parte de los pacientes no necesitaron ingreso en UCI, oxigenoterapia ni ventilación mecánica (88,9 y 96%, respectivamente). De los 14 pacientes que precisaron ingreso en UCI, cinco de ellos presentaban comorbilidades concomitantes (asma infantil, síndrome de Rett, malformaciones del SNC, síndrome de Down y malaria grave), mientras que seis desarrollaron complicaciones (uno insuficiencia mitral, tres en forma de deshidratación grave con acidosis, dos con insuficiencia respiratoria). La forma de oxigenoterapia más utilizada fueron las gafas nasales (9 de los pacientes), seguido del oxígeno a alto flujo (5). De los cinco niños que precisaron ventilación mecánica, cuatro de ellos la requirieron de forma invasiva, precisando todos ingreso en UCI; solo a uno se aplicó ventilación mecánica no invasiva.
- Complicaciones. Según se muestra en la Tabla 5, se constató alguna complicación en el 16% de los pacientes. Las complicaciones más frecuentes fueron las respiratorias (45%), tales como neumonía (la más frecuente) e insuficiencia respiratoria. El resto de las complicaciones se distribuyeron en porcentaje similar: hematológicas (neutropenia, hiperbilirrubinemia), metabólicas (deshidratación, hipopotasemia), otorrinolaringológicas (otitis media aguda, sinusitis), cardiovasculares (insuficiencia mitral, insuficiencia cardiaca).
Tabla 5. Distribución de complicaciones y tipos en 114 niños ingresados por COVID-19 hasta julio de 2022 Complicaciones Frecuencia Porcentaje No 96 84% Sí 18 16% Tipo de complicaciones Respiratorias 8 44,5% Metabólicas 3 16,7% Hematológicas 2 11,1% Otorrinolaringológicas 2 11,1% Cardiovasculares 2 11,1% Otras* 1 5,5% *Se incluyen en “otras”: comorbilidades renales (pacientes monorrenos), psiquiátricas (depresión en tratamiento), genéticas (síndrome L1, síndrome de Down). 
- Tratamientos recibidos. El 42% de los pacientes recibió tratamiento (Tabla 6), siendo más frecuente la antibioterapia oral (azitromicina, amoxicilina-clavulánico, ceftriaxona), seguido de corticoterapia oral y broncodilatadora (salbutamol y bromuro de ipratropio nebulizados e inhalados).
Tabla 6. Tratamientos recibidos en 114 niños ingresados por COVID-19 hasta julio de 2022 Tratamiento Frecuencia Porcentaje Antibiótico oral 25 29% Corticoides orales 13 15% Broncodilatadores 11 13% Corticoides intravenosos 7 8% IGG 6 7% HBPM 5 6% Remdesivir 3 4% AAS 3 4% Adrenalina nebulizada 3 4% Antibiótico intravenoso 2 2% AAS: ácido acetilsalicílico; HBPM: heparina de bajo peso molecular; IGG: inmunoglobulinas. 
Variantes y linajes del SARS-CoV-2 en la población pediátrica de la provincia de Alicante de agosto 2021 a agosto 2022
El Servicio de Microbiología de nuestro hospital nos facilitó un total de 197 muestras nasofaríngeas secuenciadas procedentes de población pediátrica (≤16 años), incluyendo datos acerca de la fecha de extracción, edad de los pacientes, sexo, lugar de extracción, variantes y linajes.
- Edad y sexo. Un 14% de las muestras analizadas procedían de lactantes <1 año, y el resto de las edades se distribuyeron en porcentajes similares (3-8%). La distribución entre sexos fue similar, un 49% hombres y un 51% mujeres.
- Procedencia de las muestras. La mayor parte de las muestras que se secuenciaron procedían de centros de salud de la provincia de Alicante (56%), mientras que el 26% procedía de las plantas de hospitalización del Hospital General Universitario Dr. Balmis, un 8% del Servicio de Urgencias de dicho hospital y el 10% restante de instituciones educativas.
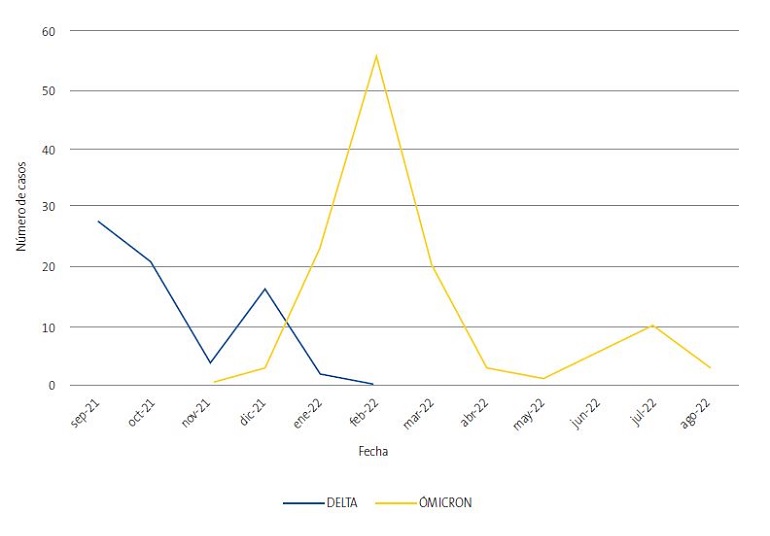
- Variantes SARS-CoV-2. En nuestro muestreo la variante mayoritaria fue la ómicron (un 63% de las muestras nasofaríngeas secuenciadas). El linaje más frecuente fue el BA.1 (un 20%), seguido del BA.2 (18%); menos frecuentes fueron el BA.1.1 (14%) y AY.4 (13,7%). En la Figura 2 se muestra la evolución temporal de las variantes del SARS-CoV-2. Se aprecia que, en los últimos meses de 2022, la variante predominante ha sido ómicron.
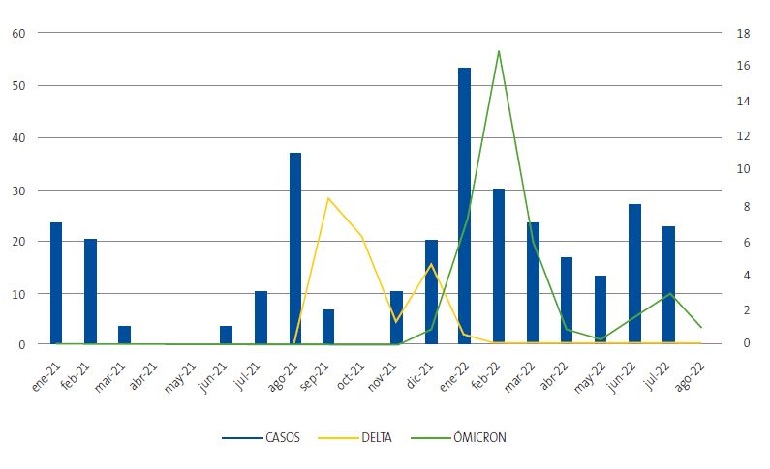
- Si tenemos en consideración la distribución temporal de los ingresos en nuestro servicio (Figura 1) junto con la distribución temporal de las variantes del SARS-CoV-2 en nuestra junto con la distribución temporal de las variantes del SARS-CoV-2 en nuestra provincia en población pediátrica, obtenemos la Figura 3. Se puede observar que tras las olas de verano de 2021 e invierno de 2022 el número de muestras secuenciadas ha aumentado al mismo tiempo que el número de casos ingresados, con un cierto decalage en la secuenciación.
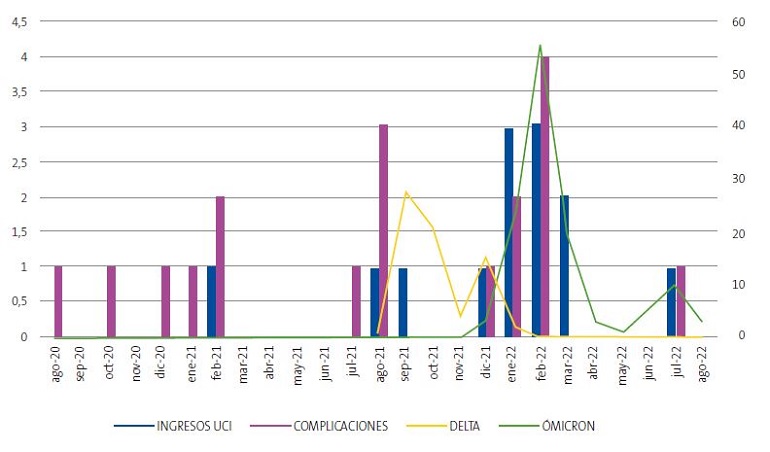
Por último, teniendo en cuenta la distribución temporal de las variantes y los casos considerados graves (gravedad definida por ingreso en UCI y desarrollo de complicaciones), obtenemos la Figura 4. Se observa cómo la variante ómicron en los meses de invierno de 2022 asoció mayor número de pacientes ingresados en UCI y mayor número de pacientes con complicaciones, en comparación con la variante delta.
DISCUSIÓN
La bibliografía acerca de la infección por SARS-CoV-2 en los niños es abundante, pero poco hay descrito acerca de la evolución temporal de la infección en los pacientes pediátricos ingresados en hospitales de tercer nivel durante la pandemia. Una aproximación a esta información la ha aportado el documento elaborado por el Comité/Grupo de Pediatría Basada en la Evidencia de la AEP y AEPap4. Según dicho documento, los lactantes parecen ser más vulnerables a la infección; esto está en concordancia con nuestro estudio, ya que los lactantes fueron el grupo de edad que precisó más ingresos. A este hecho se suma que los niños menores de 12 meses presentan mayor riesgo de ingreso, ya que las manifestaciones clínicas de la infección por SARS-CoV-2 (fiebre sin foco aparente, rechazo de la alimentación, apneas…) suponen criterios establecidos de hospitalización5. Los lactantes con edades comprendidas entre 1-2 meses fueron los que más ingresaron, ya que la edad comprendida entre 1-3 meses (siempre acompañada de una valoración clínica) se ha considerado uno de estos criterios de ingreso. Sin embargo, no parece estar del todo claro que la infección por SARS-CoV-2 produzca cuadros respiratorios graves en estas edades, tales como bronquiolitis aguda. De hecho, durante la pandemia se ha observado un descenso drástico de bronquiolitis, así como de ingresos en UCI pediátrica causados por VRS (entre otros)6, probablemente en relación con las medidas de aislamiento llevadas a cabo, y que ha dificultado la transmisión de todo tipo de infección vírica.
Según la literatura4, el síntoma más frecuente de la infección por SARS-CoV-2 en niños es la fiebre (55,8%), seguido de la tos (42,2%); estos datos son similares a los observados en la población pediátrica ingresada en nuestro hospital. El resto de la sintomatología se distribuyó en porcentajes más dispares respecto a lo descrito en la literatura. Esto podría deberse a que, al ser el tamaño muestral de nuestro estudio limitado, en los síntomas menos frecuentes puede haber mayor variabilidad descriptiva respecto a estudios con mayor tamaño muestral.
Otro aspecto importante que cabe destacar es la diferencia entre el manejo clínico de la infección entre adultos y la población pediátrica. En nuestra población pudimos observar que los medicamentos que han constituido la piedra angular del tratamiento de la infección en adultos, tales como los corticoides intravenosos, heparina de bajo peso molecular y remdesivir, en los niños no fueron los más utilizados (solo en un 9, 6 y 4%, respectivamente). En nuestra muestra, los antibióticos orales han sido el tratamiento más utilizado (29%), siendo estimado su uso en los pacientes adultos ingresados en torno al 55-85%, probablemente debido a la mayor gravedad de la infección por SARS-CoV-2 (mayores tasas de sobreinfección)7. Esto refleja una de las diferencias fundamentales en el manejo y es que, en la edad pediátrica, la actitud terapéutica suele ser menos agresiva y existen menos estudios que demuestren la efectividad de los medicamentos utilizados en la edad adulta para el control de la infección por COVID-195. Además, en la población pediátrica en general suele haber menos complicaciones, lo que explicaría una menor necesidad de tratamientos agresivos. En nuestro estudio, la gravedad se definió fundamentalmente por la necesidad de ingreso en UCI, oxigenoterapia y ventilación mecánica, siendo requeridas únicamente en un 12, 12 y 4% de los pacientes, respectivamente. Estos datos concuerdan con los encontrados en la literatura4,8, en la cual se describe que en torno a un 11,6% de los niños ingresados por COVID-19 precisaron ingreso en UCI, y un 4% precisó ventilación mecánica invasiva.
En lo que respecta a las variantes del SARS-CoV-2, en este estudio se ha podido observar que, tras las olas de verano de 2021 e invierno de 2022, el número de muestras secuenciadas ha aumentado al mismo tiempo que el número de casos ingresados (con un cierto decalaje en la secuenciación). Lo más probable es que esto se deba a que, tras la observación clínica de un aumento del número de casos ingresados, se procedió a aumentar el número de muestras secuenciadas para el estudio microbiológico en cuestión.
Según la literatura9, parece que la variante delta está asociada a una mayor gravedad, pero menor infectividad, mientras que la variante ómicron presenta mayor potencial de infectividad con menor gravedad de los casos. En nuestro estudio, desde agosto de 2021, la variante ómicron ha sido la predominante, observando paralelamente un mayor número de ingresos en UCI y desarrollo de complicaciones. Este hecho, no está en contraposición con lo descrito en la literatura, ya que faltan datos acerca de cuál fue la variante predominante desde enero de 2020 hasta julio de 2021, inclusive.
Los datos descritos en el presente artículo están supeditados a las limitaciones de los estudios descriptivos retrospectivos. En primer lugar, la no aleatorización previa de la muestra podría incurrir en un sesgo de selección, ya que los pacientes que ingresan pueden no ser representativos de la población pediátrica general (por posibilidad de acceso a los recursos hospitalarios, distribución geográfica de la población pediátrica, etc.). Por ello, en el presente estudio no se pretende establecer causalidad, sino más bien realizar un análisis descriptivo. En segundo lugar, la información procedente de los informes de hospitalización podría estar incompleta, además de que algunos datos están sujetos a una variabilidad interobservador (por ejemplo, determinar la presencia o no de disnea). Además, los criterios de gravedad (oxigenoterapia, ventilación mecánica, necesidad de ingreso en UCI) no están unificados en las sociedades científicas y cada servicio hospitalario los adapta a sus necesidades.
Como conclusión, en el Servicio de Pediatría del Hospital General Universitario Dr. Balmis el mayor número de ingresos por COVID-19 fue principalmente de lactantes <12 meses, mayoritariamente con edades comprendidas entre 1-2 meses. El síntoma más frecuente fue la fiebre, seguido de la tos y la rinorrea. La comorbilidad más frecuente detectada fue la inmunodepresión. Y la mayor parte de los pacientes no requirieron oxigenoterapia, ventilación mecánica ni ingreso en UCI. La variante ómicron es la variante del SARS-CoV-2 predominante en los últimos meses en la población pediátrica de la provincia de Alicante. Paralelamente, aunque no podemos precisar si de forma causal por la falta de datos antes comentada, se ha observado un aumento de la población pediátrica que ha desarrollado complicaciones y ha requerido ingreso en UCI. Esto puede deberse a un sesgo temporal entre el análisis de los niños ingresados en nuestro servicio (llevado a cabo desde el inicio de la pandemia, enero de 2020) y el análisis microbiológico (que comienza en agosto de 2021).
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
RESPONSABILIDAD DE LOS AUTORES
Todos los autores han contribuido de forma equivalente en la elaboración del manuscrito publicado.
ABREVIATURAS
MIS-C: multisystem inflammatory syndrome in children · SIMP: síndrome inflamatorio multisistémico en niños · UCU: unidad de cuidados intensivos · VRS: virus respiratorio sincitial.
BIBLIOGRAFÍA
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-20.
- Lu X, Zhang l, Du H, et al. SARS-CoV-2 Infection in Children. N Engl J Med. 2020;382:1663-5.
- Deville JG, Song E, Ouellette CP. COVID-19: Clinical manifestations and diagnosis in children. En: UpToDate; 2022 Aug [en línea] [consultado el 31/08/2022]. Disponible en www.uptodate.com/contents/covid-19-clinical-manifestations-and-diagnosis-in-children#H1359939953
- Comité/Grupo de Pediatría Basada en la Evidencia de la AEP y AEPap. COVID-19 en Pediatría: valoración crítica de la evidencia. En: AEPap [en línea] [consultado el 15/11/2022]. Disponible en www.aepap.org/grupos/grupo-de-pediatria-basada-en-la-evidencia/biblioteca/covid-19-en-pediatria-valoracion-critica-de-la-evidencia
- Alteri C, Scutari R, Costabile V, Colagrossi l, Yu La Rosa K, Agolini E, et al. Epidemiological characterization of SARS-CoV-2 variants in children over the four COVID-19 waves and correlation with clinical presentation. Sci Rep. 2022;12:10194.
- SEIP, SEUP, SECIP. Documento de manejo clínico del paciente pediátrico con infección por SARS-CoV-2. Extracto del Documento de Manejo Clínico del Ministerio de Sanidad [en línea] [consultado el 15/11/2022]. Disponible en www.aeped.es/sites/default/files/b26-11-_aep-seip-secip-seup._documento_de_manejo_clinico_del_paciente_pediatrico.pdf
- Aguilera Alonso D, Eplaza C, Sanz Santaeufemia FJ, Grasa C, Villanueva Medina S, Melendo S, et al. Antibiotic Prescribing in Children Hospitalized With COVID-19 and Multisystem Inlfammatory Syndrome in Spain: Prevalence, Trends, and Associated Factors. J Pediatr Infect Dis Soc. 2022;11:225-8.
- Tagarro A, Cobos Carrascosa E, Villaverde S, Sanz Santaeufemia FJ, Grasa C, Soriano Arandes A, et al. Clinical spectrum of COVID-19 and risk factors associated with severity in Spanish children. Eur J Pediatr. 2022;181:1105-15.
- Andina Martínez D, Alonso Cadenas JA, Cobos Carrascosa E, Bodegas E, Oltra Benavent M, Plazaola A, et al. SARS-CoV-2 acute bronchiolitis in hospitalized children: Neither frequent nor more severe. Pediatr Pulmonol. 2022;57:57-65.