Vol. 19 - Num. 74
Originales
Hiperfrecuentadores en Urgencias Pediátricas: ¿es toda la culpa de los padres?
Roi Piñeiro Péreza, Cristina Muñoz Archidonab, María de la Parte Canchob, Marina Mora Sitjàb, Diego Hernández Martínc, Esther Casado Verrierc, Iván Carabaño Aguadod
aServicio de Pediatría. Hospital Universitario General de Villalba. Collado Villalba. Madrid. España.
bServicio de Pediatría. Hospital General de Villalba. Collado-Villalba. Madrid. España.
cServicio de Pediatría. Hospital General de Villalba. Collado Villalba. Madrid. España.
dSección de Gastroenterología, Hepatología y Nutrición Pediátrica. Servicio de Pediatría. Hospital Universitario 12 de Octubre. Madrid. España.
Correspondencia: R Piñeiro. Correo electrónico: roi.pineiro@quironsalud.es
Cómo citar este artículo: Piñeiro Pérez R, Muñoz Archidona C, de la Parte Cancho M, Mora Sitjà M, Hernández Martín D, Casado Verrier E, et al. Hiperfrecuentadores en Urgencias Pediátricas: ¿es toda la culpa de los padres? Rev Pediatr Aten Primaria. 2017;19:137-45.
Publicado en Internet: 07-06-2017 - Número de visitas: 21952
Resumen
Introducción: existe poca información sobre el abuso de las Urgencias Pediátricas. El objetivo principal es determinar el perfil de los padres hiperfrecuentadores en un hospital de media complejidad y estimar el grado de preocupación de los padres según respuestas a una encuesta telefónica.
Pacientes y métodos: estudio descriptivo, transversal y unicéntrico. Se realiza un análisis retrospectivo de los informes de alta en niños ≤ 14 años con ≥ 10 consultas en Urgencias Pediátricas en el periodo desde el 1 de enero al 31 de diciembre de 2015. A través de entrevista telefónica, se preguntó a los padres si acudirían o no a Urgencias ante 25 supuestos clínicos. Análisis de datos mediante SPSS® v22.0.
Resultados: 21 niños realizaron ≥ 10 consultas, que suponen 246 episodios (1,17% del total de Urgencias). Edad mediana de 1,5 años; 52,2% varones. La relación entre el número de consultas en el centro de salud frente a Urgencias Pediátricas fue < 1 en el 38%. Solo nueve de 246 (3,65%) precisaron ingreso. Solo en 74 (30,1%) fue necesaria una atención que no hubiera podido ser solucionada en Atención Primaria. Se observa una relación entre los motivos de consulta y los antecedentes personales.
Conclusiones: determinar qué pacientes son hiperfrecuentadores es una tarea fácil. Contactar con los padres de estos niños y ofrecer consultas de educación sanitaria constituye una opción plausible y eficiente, que contaría con aceptación por parte de la población, mejoraría la calidad percibida y podría ahorrar costes al Sistema Nacional de Salud. Este tipo de consultas informativas constituyen parte de un proyecto que se implementará en nuestro hospital en 2017.
Palabras clave
● Encuestas comunitarias ● Niños ● Recursos sanitarios ● Servicio de Urgencias ● Uso excesivo de los servicios de saludINTRODUCCIÓN
Urgencia y emergencia son términos que se utilizan a diario, tanto en el colectivo médico como en la población general. Sin embargo, sus definiciones son múltiples y poco esclarecedoras.
Según el diccionario de la Real Academia Española1, emergencia significa “situación de peligro que requiere una acción inmediata”. Según la Asociación Médica Americana (AMA), se trata de aquella situación que pone en peligro inmediato la vida del paciente o la función de un órgano2. Y según la Organización Mundial de la Salud (OMS), emergencia es aquel caso en que la falta de asistencia conduciría a la muerte en minutos, por lo que la aplicación de primeros auxilios por cualquier persona es de importancia vital3.
Según la AMA, urgencia es toda aquella condición que, en opinión del paciente, su familia, o quien quiera que asuma la responsabilidad de la demanda, requiere una asistencia sanitaria inmediata2. La OMS define urgencia como la aparición de un problema de salud de gravedad variable que genera la conciencia de necesidad inminente de atención por parte del sujeto que lo sufre, o de su familia3. Partiendo de esa base, todas las visitas realizadas a los Servicios de Urgencias tienen carácter necesario, y el paciente hiperfrecuentador sería aquel que percibe esa necesidad de asistencia de forma muy repetida4. Según la OMS, urgencia también es definida como la patología cuya evolución es lenta y no necesariamente mortal, pero que debe ser atendida en seis horas como máximo para evitar complicaciones mayores3.
Lo cierto es que, con estas definiciones, resulta incluso complicado para el colectivo médico determinar cuándo existe una urgencia médica real, pues si todo depende de la opinión del paciente, todo puede ser una urgencia. De tal manera funcionan hoy en día los Servicios de Urgencias Pediátricas, como grandes centros de salud que atienden diversas patologías de gravedad variable, que en muy pocas ocasiones suponen un compromiso vital. Gracias a los sistemas de triaje, los tiempos de atención se adaptan a las diferentes situaciones reales de emergencia.
Y en esta situación, ¿quién es un hiperfrecuentador? ¿Cuál es el número de visitas al año en urgencias que se considera excesivo? No existe consenso en este punto, tampoco en el ámbito de Urgencias Pediátricas4. El primer paso para optimizar el uso de las Urgencias en niños en nuestro país es conocer las características y necesidades de aquellos padres que generan un mayor número de demanda sanitaria, para trabajar posteriormente en planes de actuación que posibiliten una mayor eficiencia en términos de salud para estos pacientes4.
El objetivo principal de nuestro estudio es determinar el perfil de los padres hiperfrecuentadores en un Servicio de Urgencias Pediátricas en un hospital de media complejidad de la Comunidad de Madrid. Objetivos secundarios son analizar el uso de la Atención Primaria por parte de estos padres, estudiar el número de consultas que realmente fueron necesarias y estimar el grado de preocupación de los padres en función de diferentes situaciones clínicas planteadas a través de una encuesta telefónica.
PACIENTES Y MÉTODOS
Estudio descriptivo, transversal, unicéntrico y de ámbito local. Se realiza un análisis retrospectivo de los informes de alta y pruebas complementarias realizadas en todos los niños con una edad ≤ 14 años que realizaron ≥ 10 consultas en Urgencias Pediátricas, en el periodo desde el 1 de enero al 31 de diciembre de 2015. Se decide utilizar dicho punto de corte en el número de visitas pues es la definición de hiperfrecuentador utilizada en otros estudios similares5.
- Criterios de inclusión: niños ≤ 14 años que durante el año 2015 realizaron ≥ 10 consultas en Urgencias Pediátricas.
- Criterios de exclusión: niños nacidos en 2015; adolescentes que en 2015 cumplieron 15 años.
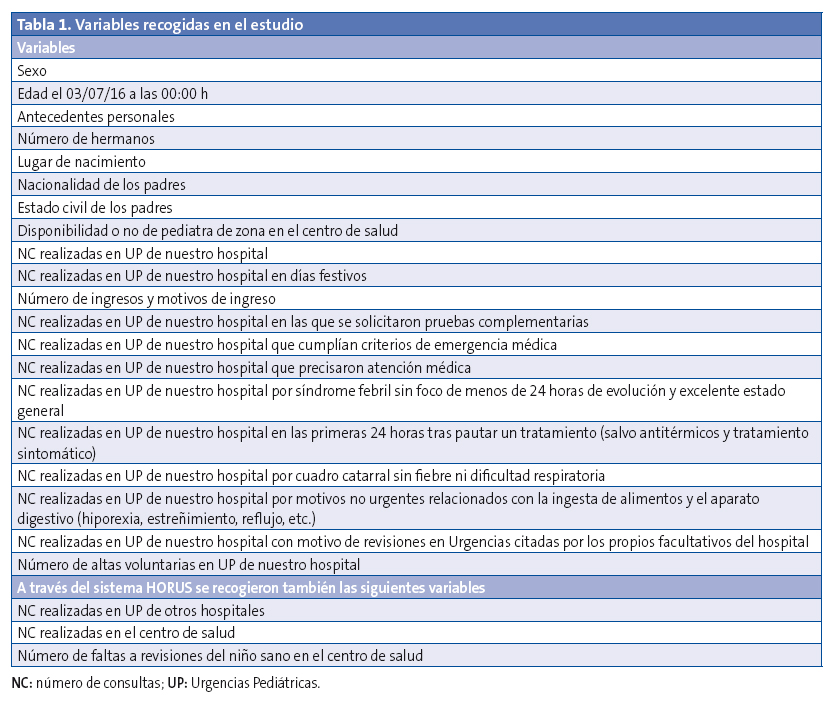
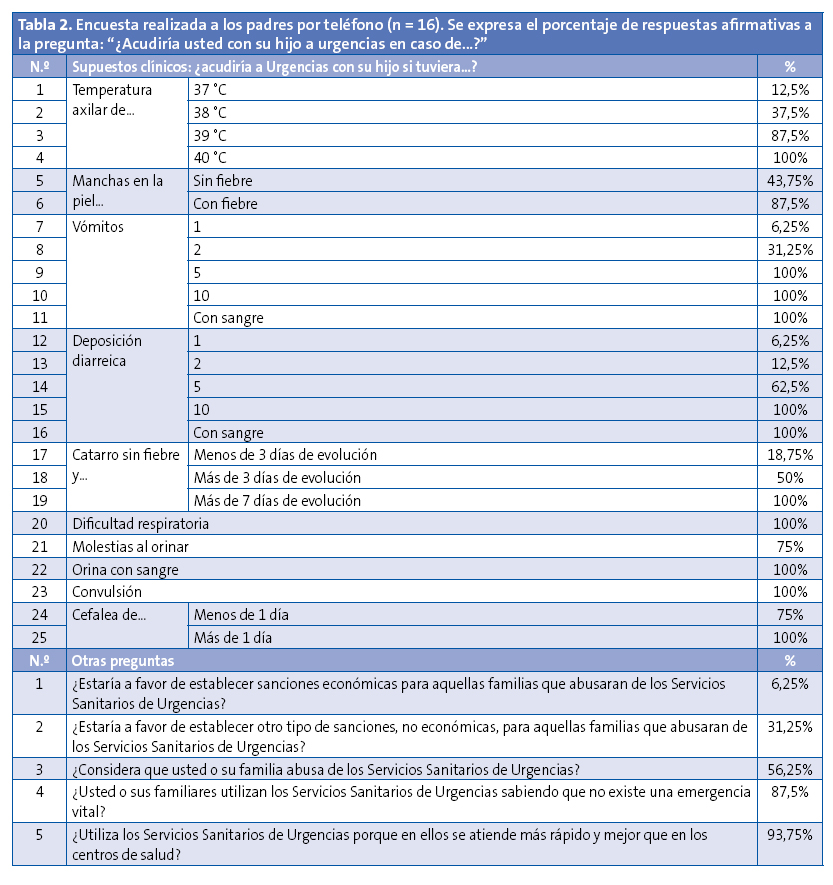
Las variables recogidas en el estudio se especifican en la Tabla 1. A través de entrevista telefónica, previo consentimiento verbal, se preguntó a los padres si acudirían o no a Urgencias ante 25 supuestos clínicos expuestos en la Tabla 2. Se realizaron además otras cinco preguntas sobre el uso de las Urgencias Pediátricas. Solo se permitió respuesta afirmativa o negativa. Cinco familias no quisieron responder a la encuesta.
El análisis descriptivo de las variables cualitativas se concreta mediante el cálculo de las distintas frecuencias relativas. El análisis de heterogeneidad se realiza mediante el test de χ2 o el test exacto de Fisher para frecuencias esperadas menores de 5. El análisis de los datos se realiza mediante el programa estadístico SPSS® v22.0 y mediante el programa informático Microsoft Excel® 2013.
RESULTADOS
Se identifican 21 niños que han realizado diez o más consultas en Urgencias Pediátricas de nuestro hospital durante el periodo de estudio. En 2015, se atendieron 20 996 urgencias pediátricas. De ellas, 246 (1,17%) fueron solicitadas por estos 21 niños, cuya mediana de visitas fue 11 (rango 10-17). El 30,9% de las consultas se realizaron en días festivos.
Edad mediana: 1,5 años (rango: de 7 meses a 11 años y 6 meses). El 52,2% eran varones, el 42,8% eran hijos únicos, el 38,1% tenían un hermano y el 19,1% dos hermanos o más. Todos eran españoles, salvo un niño nacido en Bulgaria. En el 61,9% de los casos los padres eran españoles. En el resto de los casos, al menos uno de los padres era de procedencia extranjera, fundamentalmente de Europa del Este (19%) y América Latina (14,3%). Solo en dos casos (9,5%) los padres estaban separados; el resto de familias fueron heteroparentales. No existieron diferencias significativas dentro de la misma serie con respecto a la existencia de hermanos, el país de origen de los padres o la situación familiar. No se pudieron comparar estos datos con los de los pacientes no hiperfrecuentadores, pues no se pudo disponer de dichos datos en todos los pacientes que acudieron a Urgencias durante el periodo de estudio.
El antecedente personal de interés más frecuente fue la presencia de sibilancias episódicas asociadas a infecciones respiratorias de vías altas (28,6%), seguido de alergia a las proteínas de leche de vaca (APLV) (14,3%). Hubo casos unitarios de enfermedad celíaca, antecedente de convulsión febril, trastorno por déficit de atención e hiperactividad, dermatitis atópica, giardiasis en periodo neonatal y retraso mental leve. No hubo antecedentes de enfermedades graves en ninguno de los niños, tampoco de ingresos previos en la Unidad de Cuidados Intensivos Pediátricos (UCIP), salvo un niño con un broncoespasmo moderado que estuvo 24 horas en un hospital privado y que realmente no cumplía criterios de ingreso en UCIP.
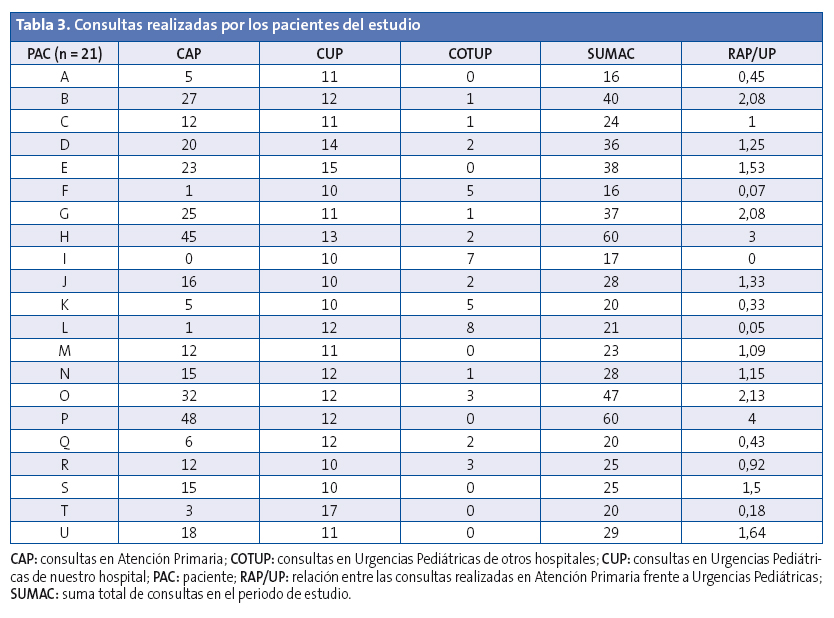
Todos los niños, salvo uno, tenían asignados un pediatra en el centro de salud. El niño que se consideró que no tenía asignado un pediatra es porque, en su lugar, la consulta ambulatoria era atendida por un médico de familia. Se contabilizaron 341 consultas en el centro de salud durante el periodo de estudio, sin incluir las visitas del programa de salud infantil, con una mediana de 15 (rango 0-48). Además, otras 43 consultas en otros Servicios de Urgencias Pediátricas, con una mediana de 1 (rango 0-8). Sumando todas las consultas, estos 21 niños utilizaron el sistema sanitario en 630 ocasiones, con una mediana de 25 (rango 16-60), es decir más de dos asistencias pediátricas al mes. La relación entre el número de consultas en centro de salud frente al número de consultas en Urgencias Pediátricas fue < 1 en el 38% de los niños.
Nueve de las 246 (3,65%) consultas en Urgencias Pediátricas precisaron ingreso, por los siguientes motivos: dos casos de gastroenteritis aguda con deshidratación leve, estudio por vómitos en contexto de APLV, crisis febril, broncoespasmo sin precisar oxigenoterapia, faringoamigdalitis con dificultades para la ingesta de sólidos, estudio por mareos de origen psicógeno, intoxicación por paracetamol y endoscopia para extracción de cuerpo extraño (piedra) en el esófago. En el 52,2% de los casos, el motivo principal de ingreso fue la ansiedad por parte de la familia. La mediana de tiempo de estancia en la planta de Pediatría fue 48 horas (rango de 24 horas a 6 días) y no hubo ninguna complicación. El porcentaje de ingresos en nuestro hospital en 2015 sobre todas las Urgencias atendidas fue del 2,15%. Existió una tendencia a favor del ingreso entre los hiperfrecuentadores, aunque no fue significativa (p = 0,107).
Setenta y seis de las 246 (30,9%) consultas en Urgencias Pediátricas precisaron realizar algún tipo de prueba complementaria. Solo en nueve pacientes (3,65%) se consideró que podría existir una emergencia médica y solo en 74 (30,1%), que fuera necesaria una atención en Urgencias que no hubiera podido ser solucionada en Atención Primaria (fundamentalmente por la necesidad de realizar pruebas complementarias).
Setenta y cinco consultas (30,5%) se resolvieron con diagnóstico de síndrome febril sin foco de menos de 24 horas de evolución y excelente estado general. En 77 episodios (31,3%), el juicio clínico fue de infección respiratoria de vías altas sin fiebre ni dificultad respiratoria. Sesenta y nueve casos (28%) consultaron en menos de 24 horas por el mismo motivo, a pesar de que se había pautado previamente un tratamiento específico (generalmente antibióticos, corticoides o broncodilatadores) y se había recomendado una revaloración en su centro de salud en un plazo de 48-72 horas. En ninguna de estas reconsultas se modificó el diagnóstico ni el tratamiento previamente prescrito. Se realizaron 40 consultas (16,3%) por motivos no urgentes relacionados con la ingesta de alimentos y el aparato digestivo (hiporexia, estreñimiento, reflujo, etc.). Solo en seis casos (2,4%) el paciente volvió a ser valorado en Urgencias por recomendación del facultativo que entregó el alta, todos ellos menores de tres meses y durante periodos festivos.
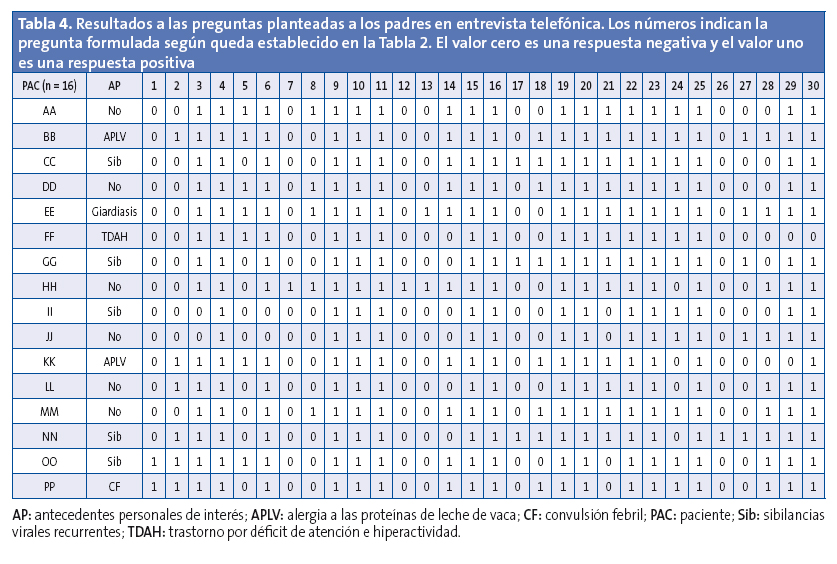
Con respecto a la entrevista telefónica, en la Tabla 2 se especifica en porcentaje el número de respuestas afirmativas a la pregunta “¿Acudiría usted con su hijo a urgencias en caso de…?”. En la Tabla 3 se muestran las consultas realizadas por los pacientes del estudio, a los que se codifica con letras y sin especificar sexo, edad ni antecedentes personales para evitar su posible identificación. En la Tabla 4, con una codificación de letras diferente, y no relacionada con la anterior, se muestran los resultados a las preguntas planteadas en la encuesta telefónica.
DISCUSIÓN
Las series pediátricas publicadas sobre padres hiperfrecuentadores son escasas5-8. Además, los puntos de corte para definir la hiperfrecuentación y los periodos de estudio son diferentes, por lo que es complicado realizar comparaciones. A estas limitaciones hay que sumar las propias de los estudios retrospectivos, lo que ha podido dificultar la recogida de algún dato. Aun así, el hecho de disponer de un sistema informatizado de gestión de los pacientes y un registro electrónico de las historias clínicas de todos los niños minimizan esta limitación, y se han mostrado suficientes para cumplir los objetivos del estudio. Por otro lado, al tratarse de un estudio unicéntrico, las conclusiones han de aplicarse con cautela. En cualquier caso, los episodios recogidos permiten identificar algunas características de los padres y pacientes hiperfrecuentadores en nuestra área de salud.
Por ejemplo, el perfil característico del paciente hiperfrecuentador en nuestro estudio es similar al presentado por Rivas5: niños menores de dos años que no precisan pruebas complementarias ni tratamientos urgentes en casi el 70% de los casos, y reciben el alta a domicilio en más del 96% de las consultas.
Existen dos patrones característicos en nuestro estudio, que no han sido analizados en publicaciones previas en nuestro país. Por un lado, están los padres que no utilizan prácticamente los servicios sanitarios de Atención Primaria, con una relación entre el número de consultas en centro de salud frente a urgencias pediátricas < 1. Destacan los pacientes F y L, con valores cercanos a cero, e incluso el valor cero en el paciente I, quien realizó diez consultas en Urgencias de nuestro hospital y otras sieteen urgencias de otros hospitales por ninguna en su centro de salud. Por otro lado, están los padres que utilizan con frecuencia tanto los servicios de Atención Primaria como los de Atención Especializada. Entre ellos, destacan los pacientes H y P, con 60 consultas cada uno en solo un año, y sin contabilizar las visitas del niño sano.
Otro aspecto significativo es la importancia de los antecedentes personales del paciente. Por ejemplo, la madre del paciente PP, con antecedente de una convulsión febril típica, refiere que consultaría en Urgencias ante cualquier modificación en la temperatura corporal, incluyendo 37 °C, con independencia de los síntomas acompañantes y el estado general. Los únicos pacientes que consultarían en Urgencias por un catarro sin fiebre de menos de tres días de evolución son CC, GG y NN, todos ellos con antecedentes de sibilancias recurrentes. Las consultas por clínica digestiva banal (escasos vómitos o deposiciones diarreicas) fueron habituales en el paciente EE, con antecedente de una giardiasis intestinal en el periodo neonatal.
El fenómeno de la hiperfrecuentación está poco estudiado en general, y en particular en Pediatría. Aunque es complejo determinar el coste real de la asistencia médica en el Sistema Nacional de Salud, pues depende de cada comunidad autónoma, el importe de una atención médica sin pruebas complementarias en un centro de salud oscila entre los 30 € y los 70 €, mientras que la atención en Urgencias, también sin pruebas complementarias, puede suponer un gasto público9-11 entre los 140 € y los 400 €. De tal manera, una consulta en Urgencias que podría haber sido solucionada en Atención Primaria supone un sobrecoste que oscilaría entre los 70 € como mínimo y los 370 € como máximo. Solo en nuestro hospital, solo en Urgencias Pediátricas, y considerando que casi el 70% de las visitas se podrían haber resuelto de igual manera en el centro de salud, en 2015 se podrían haber ahorrado entre 12 040 € y 63 640 € según la diferencia calculada. Aunque se trata de una mera estimación, si este cálculo se realizara en toda España, el ahorro podría alcanzar millones de euros, y solo considerando los niños.
Una vez identificados los padres hiperfrecuentadores, una posible solución sería el refuerzo de la educación sanitaria, de forma específica según los miedos infundados de los progenitores. Por ejemplo, generar una consulta para el paciente PP, explicando que los antitérmicos no han demostrado ningún potencial para prevenir las convulsiones febriles, que se trata de un cuadro benigno y que lo importante es conocer cómo actuar en domicilio y no solicitar una consulta urgente ante cualquier elevación de la temperatura corporal. O informar a los padres de niños con sibilancias recurrentes cuáles son los signos de dificultad respiratoria que deben vigilar, cómo deben administrar los broncodilatadores y que la nebulización de fármacos no presenta ventajas significativas frente a la inhalación. ¿Es toda la culpa de los padres? Muchos de ellos utilizan de forma excesiva los Servicios de Urgencias de forma consciente, pero ¿estamos los pediatras preparados para hacer frente a los hiperfrecuentadores? Las campañas informativas generales sobre el uso inadecuado de los Servicios de Urgencias no resuelven las dudas que hacen a los padres abusar del sistema. Quizá una búsqueda selectiva de hiperfrecuentadores y una formación específica dirigida hacia los aspectos de la salud de sus hijos que les generan más preocupación, podrían reducir el abultado número de consultas en Urgencias.
En resumen, el uso excesivo de los Servicios de Urgencias Pediátricas no parece constituir un problema prioritario en nuestro país, ni se vislumbra una solución a corto plazo que no pase por sancionar, de alguna manera, a los pacientes que acudan sin motivo a los hospitales. Las sanciones siempre repercuten de forma negativa sobre los más débiles, ya sea desde el punto de vista económico u otros puntos de vista, como por ejemplo la posibilidad de acceso a la información. Determinar qué pacientes son hiperfrecuentadores es una tarea sencilla gracias a los sistemas informatizados de gestión de los que disponemos hoy. Contactar con los padres de estos niños y ofrecer consultas de educación sanitaria constituye una opción accesible, plausible y eficiente, que además contaría con aceptación por parte de la población, mejoraría la calidad percibida y podría ahorrar costes al Sistema Nacional de Salud. Este tipo de consultas informativas constituyen parte de un proyecto que se implementará en nuestro hospital en 2017.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS: AMA: Asociación Médica Americana · APLV: alergia a las proteínas de leche de vaca · OMS: Organización Mundial de la Salud · UCIP: Unidad de Cuidados Intensivos Pediátricos.
BIBLIOGRAFÍA
- Real Academia Española. Diccionario de la lengua española [en línea] [consultado el 01/06/2017]. Disponible en www.rae.es
- American Medical Association [en línea] [consultado el 01/06/2017]. Disponible en www.ama-assn.org/ama
- Glossary of terms used. En: World Health Organization [en línea] [consultado el 01/06/2017]. Disponible en www.who.int/hia/about/glos/en/index2.html
- Grupo de Trabajo de Indicadores de Calidad de la Sociedad Española de Urgencias de Pediatría. Servicios de urgencias: indicadores de calidad de la atención sanitaria. An Pediatr (Barc). 2004;60:569-80.
- Rivas A, Manrique G, Butragueño L, Mesa S, Campos A, Fernández V, et al. Hiperfrecuentadores en urgencias. ¿Quiénes son? ¿Por qué consultan? An Pediatr (Barc). 2017;86:67-75.
- Sansa L, Orús T, Juncosa S, Barredo M, Travería J. Frecuentación de los servicios de urgencias hospitalarios: motivaciones y características de las urgencias pediátricas. An Esp Pediatr. 1996;44:97-104.
- Neuman MI, Alpern ER, Hall M, Kharbanda AB, Shah SS, Freedman SB, et al. Characteristics of recurrent utilization in pediatric emergency departments. Pediatrics. 2014;134:e1025-31.
- Alpern ER, Clark AE, Alessandrini EA, Gorelick MH, Kittick M, Stanley RM, et al. Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21:365-73.
- Sevillano EG. Consulta con el médico: 39 euros. En: El País [en línea] [consultado el 01/06/2017]. Disponible en http://ccaa.elpais.com/ccaa/2012/08/19/madrid/1345407250_069569.html
- Vallejo S. ¿Cuánto cuesta la Sanidad? En: Granada Hoy [en línea] [consultado el 01/06/2017]. Disponible en www.granadahoy.com/article/granada/569079/cuanto/cuesta/la/sanidad.html
- Santiago EA. Una consulta médica en un centro de salud cuesta 69 euros, y una urgencia hospitalaria, 362. En: La Voz de Galicia [en línea] [consultado el 01/06/2017]. Disponible en https://goo.gl/R7cLl9





