Vol. 19 - Num. 74
Original Papers
Frequent users in Paediatric Emergency Departments: Are parents solely to blame?
Roi Piñeiro Péreza, Cristina Muñoz Archidonab, María de la Parte Canchob, Marina Mora Sitjàb, Diego Hernández Martínc, Esther Casado Verrierc, Iván Carabaño Aguadod
aServicio de Pediatría. Hospital Universitario General de Villalba. Collado Villalba. Madrid. España.
bServicio de Pediatría. Hospital General de Villalba. Collado-Villalba. Madrid. España.
cServicio de Pediatría. Hospital General de Villalba. Collado Villalba. Madrid. España.
dSección de Gastroenterología, Hepatología y Nutrición Pediátrica. Servicio de Pediatría. Hospital Universitario 12 de Octubre. Madrid. España.
Correspondence: R Piñeiro. E-mail: roi.pineiro@quironsalud.es
Reference of this article: Piñeiro Pérez R, Muñoz Archidona C, de la Parte Cancho M, Mora Sitjà M, Hernández Martín D, Casado Verrier E, et al. Frequent users in Paediatric Emergency Departments: Are parents solely to blame? Rev Pediatr Aten Primaria. 2017;19:137-45.
Published in Internet: 07-06-2017 - Visits: 15513
Abstract
Introduction: there is little information regarding the abuse of consultations in the Pediatric Emergency Departments (PED). The aims of the study are to determine the characteristics of frequent users in a public general hospital, and to estimate the concerns of parents guided by responses to a telephone survey.
Patients and methods: a descriptive, cross-sectional, unicentric and local study was conducted from January to December 2015. All children ≤ 14 years visiting Pediatric Emergency Departments ≥ 10 times were included. Through a telephone interview, parents were asked whether or not they would go to the Emergency Room for 25 supposed clinical cases. SPSS v22.0® was used for statistical analysis.
Results: 21 children (52.2% males) visited PED ≥ 10 times, involving 246 clinical cases (1.17% of total emergencies). Median age was 1.5 years. The ratio of the number of visits at Primary Care vs. PED” was < 1 in 38%. Admission was required only in 9 of 246 (3.65%) children. Visits that could not be solved at Primary Care were observed only in 74 cases (30.1%). Reasons for a pediatric visit and personal history were related.
Conclusions: to determine which patients are frequent users is an easy task. To contact the parents of these children and to provide health education could be a feasible and efficient chance, which would be accepted by the population, it also would improve the perceived quality and could save costs to the National Health System. This kind of visits promoting health education are part of a project which will be implemented in our hospital in 2017.
Keywords
● Children ● Community surveys ● Emergency Service ● Health resources ● Medical overuseINTRODUCTION
Urgency and emergency are terms used in everyday language, both in the medical field and the general population. However, their definitions are multiple and quite vague.
According to the Spanish dictionary of the Real Academia Española,1 an emergency is a “dangerous situation that calls for immediate action.” The American Medical Association (AMA) defines it as a situation that poses an immediate threat to the life of the patient or the physiologic function of an organ,2 and the World Health Organization (WHO) as a situation in which lack of medical care can lead to death within minutes, so that delivery of first aid by any party is of vital importance.3
According to AMA, an urgent situation is one that requires immediate medical care in the opinion of the patient, the family, or individual who is requesting the care.2 The WHO defines an urgent situation as an acute health problem of variable severity perceived as requiring immediate care by the affected individual or his or her family.3 Within this framework, all visits to emergency departments would be considered necessary, and frequent users would be those individuals who perceived the need for care very often.4 The WHO also defines urgent situations as health problems with a slow progression that are not necessarily life-threatening but need to be treated within 6 hours to prevent further complications.3
The fact is that with these definitions, even medical professionals have difficulty determining when there is a real medical emergency, since anything could be an emergency if the definition were based solely on the judgment of the patient. This is how paediatric emergency departments operate today, serving as large health facilities that manage various diseases with different degrees of severity that are rarely life-threatening. By means of triaging systems, waiting times for receiving care are established based on actual patient acuity.
In this context, who would be considered a frequent user? What number of emergency visits per year would be excessive? There is no consensus on this point, in general or in the specific field of paediatric emergency care.4 The first step we need to take to optimise the use of paediatric emergency services in Spain is to determine the characteristics and needs of the parents that generate a greater demand for health care, to then work on interventions that would lead to a more efficient use of health resources in these patients.4
The primary objective of our study was to establish the profile of parents who were frequent users of paediatric emergency services in a secondary level hospital in the autonomous community of Madrid. The secondary objectives were to analyse the use of primary care services of these parents, determine the number of visits that were actually necessary, and estimate the level of anxiety of parents in relation to different hypothetical clinical situations posed to them in a telephonic survey.
PATIENTS AND METHODS
We conducted a local, single-centre, cross-sectional descriptive study. We performed a retrospective review of the discharge summaries and diagnostic tests performed in all children aged 14 years or younger that made 10 or more visits to the paediatric emergency department between January 1 and December 31, 2015. We chose the cut-off point of 10 visits because that is the number used to define frequent users in similar studies.5
- Inclusion criteria: children aged 14 years or younger that made 10 or more visits to the Paediatric Emergency Department in 2015.
- Exclusion criteria: children born in 2015; adolescents that turned 15 years old in 2015.
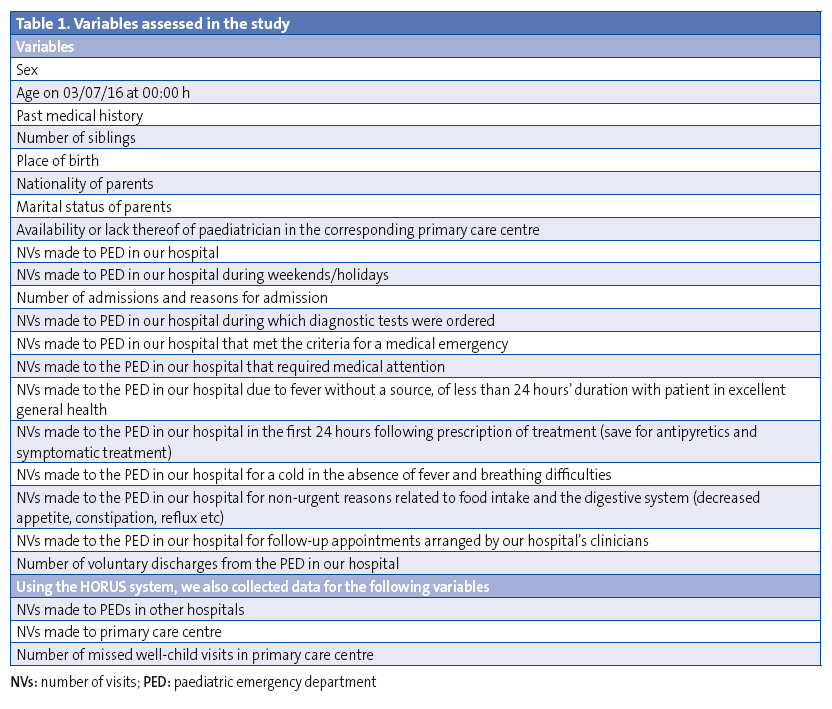
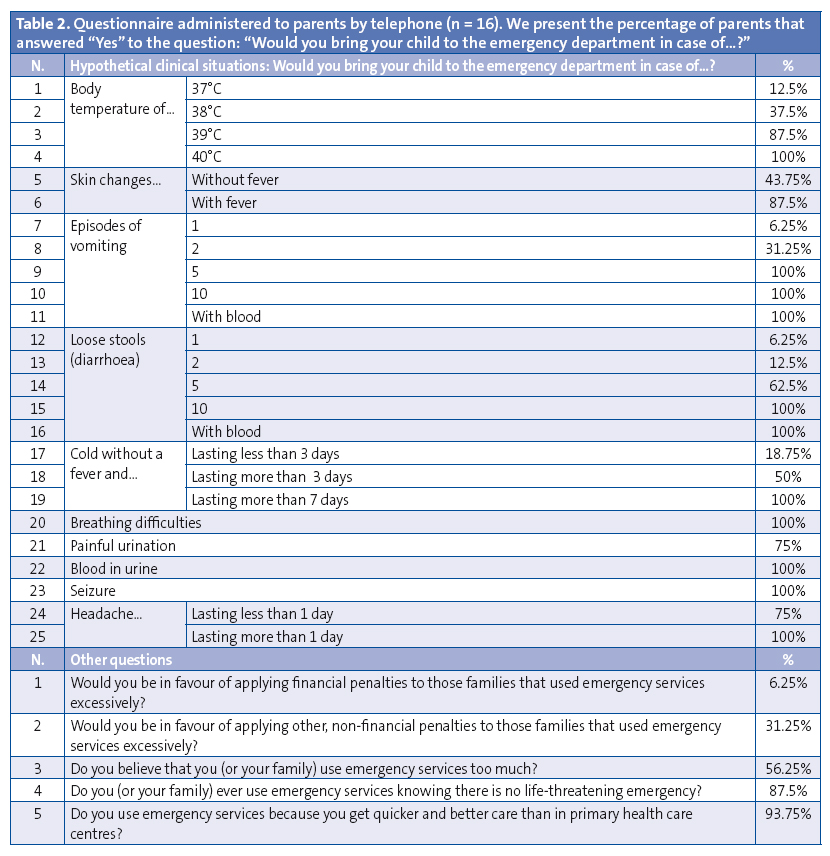
Table 1 presents the variables analysed in the study. We made telephone interviews and, after obtaining verbal consent, asked parents whether they would visit the emergency department in case of 25 different hypothetical situations, which are listed in Table 2. We also asked five other questions regarding the use of paediatric emergency services. Parents were only allowed to answer Yes or No. Five households chose not to participate in the survey.
We made a descriptive analysis of qualitative variables by calculating their corresponding relative frequencies. We tested for homogeneity with the chi square test, or, for cells with expected values of less than 5, Fisher’s exact test. The data were analysed with the statistical package SPSS® version 22.0 and with Microsoft Excel® 2013.
RESULTS
We identified 21 children that had made 10 or more visits to the paediatric emergency department of our hospital during the period under study. In 2015, the hospital received 20 996 paediatric emergency visits. Of this total, 246 (1.17%) were made by these 21 children, with a median of 11 visits (range, 10–17). Of all visits, 30.9% were made during weekends or holidays.
The median age was 1.5 years (range, 7 months–11 years and 6 months); 52.2% of the patients were male; 42.8% were single children; 38.1% had 1 sibling and 19.1% 2 or more siblings. All of the patients were Spanish, except for one born in Bulgaria. The parents of 61.9% of the children were both Spanish; in the remaining patients, at least 1 parent was a foreign national, most frequently from Eastern Europe (19%) and Latin America (14.3%). The parents of only 2 patients were separated (9.5%), and the rest of the families were heteroparental. We did not find any significant differences in our sample based on the number of siblings, the country of origin of the parents or the family structure. We could not compare these figures with those of patients that were not frequent users, as we could not retrieve these data for all the patients that visited the emergency department during the period under study.
Of the relevant findings in the personal histories of these patients, the most frequent was wheezing associated with upper respiratory tract infection (28.6%), followed by cow’s milk protein allergy (CMPA) (14.3%). There were isolated cases of celiac disease, past history of febrile seizures, attention-deficit hyperactivity disorder, atopic dermatitis, neonatal giardiasis and mild intellectual disability. None of the patients had a previous history of severe disease or admission to the paediatric intensive care unit (PICU), except for 1 boy that had been hospitalised for 24 hours in a private hospital with moderate bronchospasm that did not actually meet the criteria for admission to the PICU.
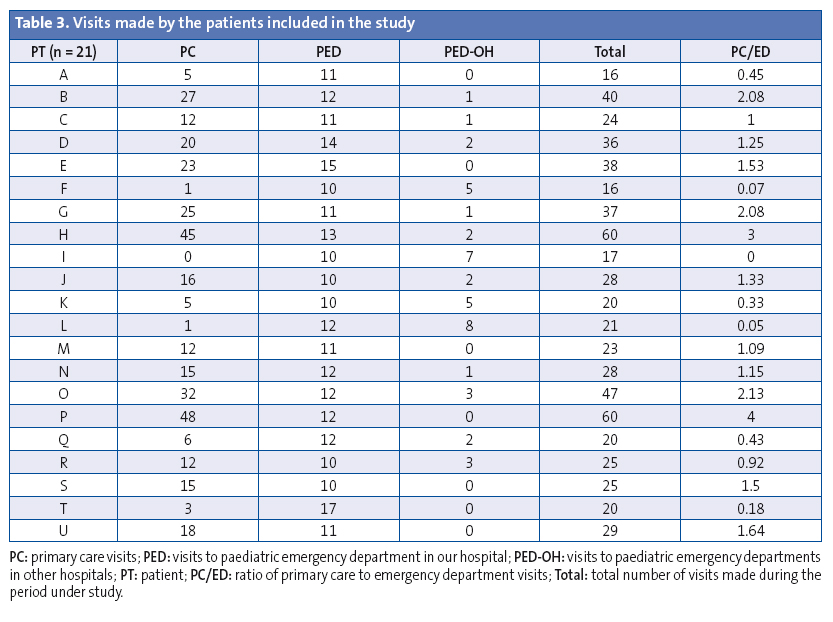
All children, except one, had an assigned paediatrician in a primary care centre. The one exception corresponded to a child that received services in a site in which outpatient care was delivered by a family physician instead of a paediatrician. We found records for 341 visits to the primary care centre in the period under study, excluding the visits corresponding to the well-child programme, with a median number of 15 visits (range, 0–48). Furthermore, the patients made 43 visits to other paediatric emergency departments, with a median of 1 visit (range, 0–8). Adding all of these visits, these 21 children used the public health system 630 times, making a median of 25 visits (range, 16–60), which amounts to more than 2 paediatric care visits a month. The ratio of the number of visits to the primary care centre to the number of visits to paediatric emergency departments was less than 1 in 38% of the patients.
Of the 246 visits to the paediatric emergency department, 9 (3.65%) resulted in hospital admission for the following reasons: 2 cases of acute gastroenteritis with mild dehydration; assessment of vomiting in a patient with CMPA; febrile seizures; bronchospasm that did not require supplementary oxygen; pharyngotonsillitis with difficulty swallowing solids; assessment of episodes of psychogenic dizziness; paracetamol poisoning; and performance of endoscopy for extraction of a foreign body from the oesophagus. In 52.2% of cases, the main reason for admission was the anxiety of the family. The median length of stay in the paediatric ward was 48 hours (range, 24 hours to 6 days), and none of the patients experienced complications. The percentage of emergency visits that resulted in hospital admission in our hospital in 2015 was 2.15%. The proportion of admissions was slightly higher in frequent users, although the difference was not statistically significant (P = .107).
Of the 246 visits to the paediatric emergency department, 76 (30.9%) led to performance of diagnostic tests. The reason for the visit was considered a medical emergency in only 9 patients (3.65%), and only 74 of the visits to the emergency department (30.1%) were considered warranted as the chief concern could not have been resolved in primary care (mostly due to the need for diagnostic tests).
Seventy-five visits (30.5%) concluded with a diagnosis of fever without a source of less than 24 hours’ duration and the patient in excellent general health. In 77 visits (31.3%), the clinical diagnosis was upper respiratory tract infection without fever or respiratory difficulties. In 69 instances (28%), the patient returned with the same concern within 24 hours, despite prescription of specific treatment in the previous visit (usually antibiotics, steroids or bronchodilators) with the recommendation of making a follow-up visit to the primary care centre within 48-72 hours. None of the repeat visits led to a change in the existing diagnosis or prescribed treatment. Forty visits (16.3%) were made for non-urgent concerns related to food intake and the digestive system (decreased appetite, constipation, reflux, etc). The patient returned to the emergency department for reevaluation following the recommendation of the discharging physician in only 6 cases (2.4%), all of which concerned infants aged less than 3 months in non-working days.
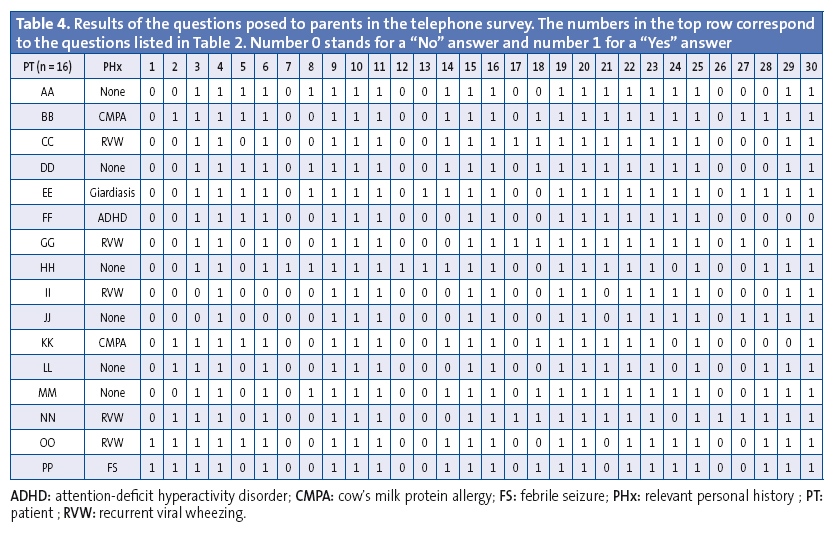
As for the telephone survey, Table 2 presents the number of parents that answered “Yes” to the question “Would you bring your child to the emergency department in case of…?” for each clinical situation. Table 3 summarises the visits made by the patients included in our study, which are represented by a letter code unaccompanied by information on their sex, age or medical history to prevent their identification. Table 4 presents the answers to the questions made in the telephone survey, using letter codes that are different and unrelated to the codes used in Table 3.
DISCUSSION
There are few paediatric case series on the subject of frequent users in the medical literature.5-8 Furthermore, these studies established different cut-off points to define frequent use and different study periods, which poses challenges to their comparison. These limitations are compounded by those intrinsic to retrospective studies, which may hinder collection of some of the data. Nevertheless, the availability of a computerised patient management system and the electronic health records database minimise this limitation, and sufficed to achieve the objectives of our study. On the other hand, since ours was a single-centre study, its findings must be interpreted with caution. At any rate, the cases that we analysed allowed the identification of some of the characteristics of frequent users in our health area and of their parents.
For instance, the characteristic profile of patients that were frequent users in our study was similar to the one described by Rivas5: children aged less than 2 years that did not require diagnostic tests or urgent treatment in nearly 70% of cases, and that were discharged home in more than 96% of the visits.
There are two characteristic patterns in our study that have not been analysed in the existing Spanish literature. On one hand, there are the parents that hardly use primary care services, with a ratio of primary care visits to emergency visits of less than 1. This is most marked in patients F and L, with ratios near zero, and even a ratio of zero in patient I, who made 10 visits to the emergency department of our hospital and another 7 to other emergency departments and no visits to the corresponding primary care centre. On the other hand, there are the parents that use both primary care and specialty services frequently. The most salient patients in this group were H and P, each of who made 60 medical visits in one year, excluding well-child visits.
Another relevant aspect was the importance of the personal history of the patient. For instance, the mother of patient PP, who had a history of febrile seizures, reported that she would seek emergency care for any changes in body temperature, even for 37°C, independent of the associated symptoms or the general health of the child. The only patients that would visit the emergency department for a cold of less than 3 days’ duration in the absence of fever were CC, GG and NN, all of who had a history of recurrent wheezing. Visits for mild gastrointestinal symptoms (light vomiting or loose stools) were habitual in patient EE, who had a history of intestinal giardiasis in the neonatal period.
Little research has been done on the frequent user phenomenon, especially in paediatrics. Although it would be difficult to establish the actual health care costs of the public health system in Spain, since they depend on each autonomous community, the cost of a visit to a primary care centre without diagnostic tests ranges between 30 and 70 euro, while an emergency department visit, also without diagnostic tests, can cost the government between 140 and 400 euro.9-11 Thus, a visit to the emergency department for an issue that could have been resolved in primary care corresponds to an excess cost of at least 70 and up to 370 euro. In the paediatric emergency department of our hospital alone, considering that nearly 70% of visits could have been managed equally well in a primary care centre, between 12 040 and 63 640 euro could have been saved based on the differences calculated above. Although this is only an approximation, if this calculation was made for all of Spain, the savings could add to millions of euro for paediatric services alone.
A possible solution after the identification of parents that are frequent users would be to invest more in health education, addressing specific unwarranted fears in parents. For instance, we could schedule a visit with patient PP to explain that there is no evidence that antipyretics can prevent febrile seizures, that febrile seizures are a benign condition and that the key is to know how to act at home as opposed to seeking urgent care with any increase in body temperature. Or educating the parents of children with recurrent wheezing on the signs of respiratory distress that they need to watch for, the administration of bronchodilators and the fact that nebulised drugs do not offer significant advantages compared to inhaled drugs. Can we blame it all on the parents? Many of them knowingly overuse emergency services, but are we, as paediatricians, ready to manage frequent users? The general educational campaigns on the inadequate use of emergency services do not address the concerns that lead parents to abuse the system. Perhaps a selective search for frequent users and offering education on the health issues in their children that concern them most could reduce overuse of emergency services.
In short, the excessive use of paediatric emergency services does not seem to be a problem that needs to be prioritised in Spain, and there seems to be no short-term solution for it other than penalising patients that make unwarranted visits to hospitals in some way. Penalties always have the greatest impact on those that are most vulnerable, economically or otherwise, for instance individuals with limited access to information. It is easy to identify frequent users thanks to the computerised management systems that are currently available. Contacting the parents of these children and offering health education sessions is an accessible, feasible and efficient option that would be well received by a subset of the population, improving the perceived quality of care and potentially reducing costs for the national health system. Such educational visits are part of a project that will be implemented in our hospital in 2017.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS AMA: American Medical Association · CMPA: cow’s milk protein allergy · PICU: Paediatric Intensive Care Unit · WHO: World Health Organization.
REFERENCES
- Real Academia Española. Diccionario de la lengua española [online] [accessed 01/06/2017]. Available at www.rae.es
- American Medical Association [online] [accessed 01/06/2017]. Available at www.ama-assn.org/ama
- Glossary of terms used. In: World Health Organization [online] [accessed 01/06/2017]. Available at www.who.int/hia/about/glos/en/index2.html
- Grupo de Trabajo de Indicadores de Calidad de la Sociedad Española de Urgencias de Pediatría. Servicios de urgencias: indicadores de calidad de la atención sanitaria. An Pediatr (Barc). 2004;60:569-80.
- Rivas A, Manrique G, Butragueño L, Mesa S, Campos A, Fernández V, et al. Hiperfrecuentadores en urgencias. ¿Quiénes son? ¿Por qué consultan? An Pediatr (Barc). 2017;86:67-75.
- Sansa L, Orús T, Juncosa S, Barredo M, Travería J. Frecuentación de los servicios de urgencias hospitalarios: motivaciones y características de las urgencias pediátricas. An Esp Pediatr. 1996;44:97-104.
- Neuman MI, Alpern ER, Hall M, Kharbanda AB, Shah SS, Freedman SB, et al. Characteristics of recurrent utilization in pediatric emergency departments. Pediatrics. 2014;134:e1025-31.
- Alpern ER, Clark AE, Alessandrini EA, Gorelick MH, Kittick M, Stanley RM, et al. Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21:365-73.
- Sevillano EG. Consulta con el médico: 39 euros. In: El País [online] [accessed 01/06/2017]. Available at http://ccaa.elpais.com/ccaa/2012/08/19/madrid/1345407250_069569.html
- Vallejo S. ¿Cuánto cuesta la Sanidad? In: Granada Hoy [online] [accessed 01/06/2017]. Available at www.granadahoy.com/article/granada/569079/cuanto/cuesta/la/sanidad.html
- Santiago EA. Una consulta médica en un centro de salud cuesta 69 euros, y una urgencia hospitalaria, 362. In: La Voz de Galicia [online] [accessed 01/06/2017]. Available at https://goo.gl/R7cLl9
Comments
This article has no comments yet.





