Vol. 15 - Num. 59
Originales
Cribado visual en Atención Primaria, ¿cómo se realiza?
Ramona Martín Martína, José Ángel Bilbao Sustachab, Antoni Collado Cucòc
aServicio de Pediatría. ABS Marià Fortuny. Reus. Tarragona. España.
bMédico. CAP Riudoms. Riudoms. Tarragona. España.
cMédico Adjunto. CAP Riudoms. Riudoms. Tarragona. España.
Correspondencia: R Martín. Correo electrónico: rmartin@grupsagessa.com
Cómo citar este artículo: Martín Martín R, Bilbao Sustacha JA, Collado Cucò A. Cribado visual en Atención Primaria, ¿cómo se realiza? Rev Pediatr Aten Primaria. 2013;15:221-7.
Publicado en Internet: 11-09-2013 - Número de visitas: 34937
Resumen
Introducción: la ambliopía es la causa más común de pérdida de visión prevenible en los países desarrollados, la padece el 2-5% de la población. El estrabismo afecta al 3-6%. El objetivo primordial del programa de cribado visual es detectar precozmente estos defectos.
Objetivos: constatar la existencia de material básico en las consultas para realizar cribado visual y evaluar los conocimientos básicos que deberían tener los profesionales que lo realizan.
Material y métodos: evaluación de la existencia del material en las consultas y los conocimientos básicos recomendados por la Asociación Española de Pediatría de Atención Primaria. Se realizó mediante una encuesta de 29 preguntas. Los resultados fueron sometidos a análisis estadístico: análisis descriptivo, bivariante mediante T-test y análisis de la varianza.
Resultados: contestaron nuestra encuesta 56 personas: 40 médicos y 16 enfermeras de 15 Áreas Básicas de Salud. Ausencia de material en consultas: 32,1% optotipo, 51,8% gafas con lentes +2 dioptrías, 10,7% oftalmoscopio. Desconocimiento de la utilidad del material: 71,4% distancia lectura optotipo, 71,4% dirección lectura optotipo, 60,7% optotipo adecuado a la edad, 35,7% gafas con lentes +2 dioptrías. Desconocimiento de los criterios de derivación: 92,9% agudeza visual a los cuatro años, 53,6% estrabismo fijo, 53,6% estrabismo latente, 33,9% anisometropía. Respuestas correctas de los médicos: 49,89%. Respuestas correctas de las enfermeras: 37,23%.
Conclusiones: se constatan la falta de material adecuado en las consultas y el desconocimiento del personal sobre cómo usarlo. Se pone de manifiesto el desconocimiento del desarrollo visual normal, las exploraciones que se deben realizar y los motivos de derivación. Y se observan diferencias en el cribado si este lo realiza el médico o la enfermera. La falta de conocimientos es similar en nuestro entorno.
Palabras clave
● Agudeza visual ● Ambliopía ● Cribado visual ● EstrabismoINTRODUCCIÓN
La ambliopía es la causa más común de pérdida de visión prevenible en los países desarrollados. La padece el 2-5% de la población general. El estrabismo afecta al 3-6%; de estos, del 33 al 50% desarrollará ambliopía. Se estima que hasta el 20% de los niños de cualquier edad padece defectos de refracción significativos.
Durante los primeros seis años de vida, las vías visuales son moldeables. Para el desarrollo visual, el cerebro debe recibir, de forma simultánea, imágenes igualmente focalizadas y claras de ambos ojos para “aprender” a ver. Cualquier factor que interfiera en el proceso de aprendizaje visual del cerebro provocará una reducción de la agudeza visual (AV).
Detectar precozmente cualquier defecto es el objetivo primordial que justificaría el programa de cribado visual. Trataremos de analizar cómo se lleva a cabo en Atención Primaria.
Objetivos
- Constatar la existencia de material básico en las consultas para realizar el cribado visual.
- Evaluar los conocimientos básicos que deberían tener los profesionales que realizan el cribado visual, según las recomendaciones de 2008 del grupo PrevInfad de la Asociación Española de Pediatría de Atención Primaria (AEPap).
MATERIAL Y MÉTODOS
Se diseñó una encuesta para la evaluación de la existencia del material en las consultas y los conocimientos básicos recomendados por PrevInfad. Se formularon 29 preguntas; siete sobre el material y 22 sobre exploraciones consideradas básicas en las recomendaciones de PrevInfad, motivos y edades de derivación al oftalmólogo.
Respecto al material que debe haber en toda consulta, se diseñaron las preguntas considerando lo propuesto por las recomendaciones de PrevInfad y el Programa de Actividades Preventivas y Promoción de la Salud en la Edad Pediátrica (PAPPS) de Cataluña 2008.
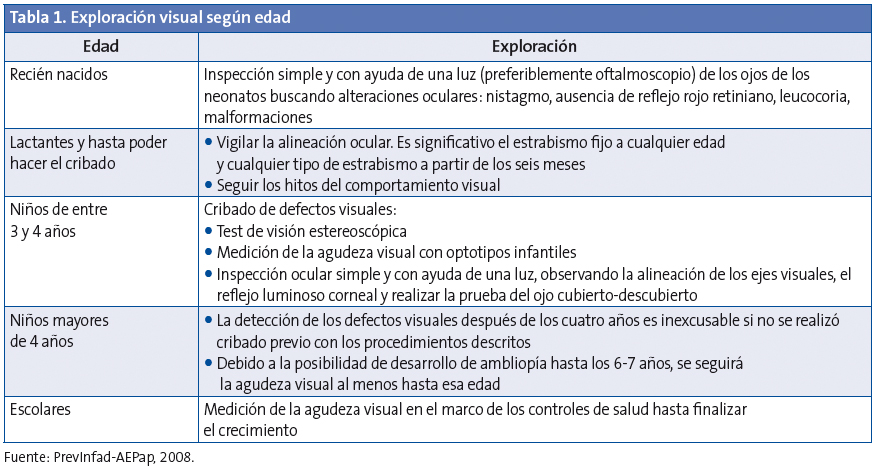
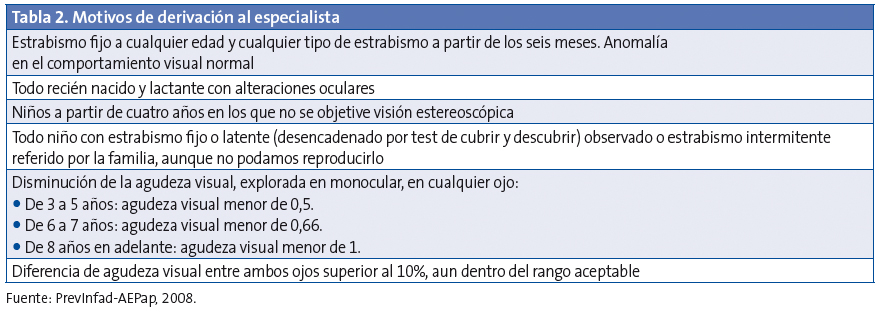
Para evaluar los conocimientos de los profesionales, se diseñaron preguntas basadas en las recomendaciones de PrevInfad, recogidas en las Tablas 1 y 2.
Los datos de la encuesta fueron sometidos al siguiente análisis estadístico: análisis descriptivo, análisis bivariante mediante T-test y análisis de la varianza.
RESULTADOS
El 78,87% de las personas a las que se lo solicitamos contestó nuestra encuesta; el 88,88% de los médicos (40 de 45) y el 61,53% de las enfermeras (16 de 26). De las 56 personas que respondieron, 40 eran médicos y 16 enfermeras pertenecientes a 15 Áreas Básicas de Salud (ABS) de Tarragona, del ámbito de gestión pública y privada, distribuidos de la siguiente manera: un 46,4% ABS de gestión pública, un 37,5% ABS de gestión privada 1, y un 16,1% ABS de gestión privada 2.
Los resultados de la encuesta se describen a continuación:
El 89,3% dispone de oftalmoscopio. El 32,1% no tiene optotipo. De los que tienen optotipo, el 37,5% tiene para cada edad (dibujos, cuadrados incompletos y alfabético); el 17,9% tiene alfabético y el 21,4% solo de dibujos.
El 89,3% desconoce el nombre del optotipo que utiliza (Wecker). El 71,4% desconoce la distancia a la que debe ser leído (2,5 metros). El 28,6% sabe que la lectura debe ser horizontal. El 48,2% lo leería de forma vertical y el 12,5% haría una lectura aleatoria.
El 64,3% conoce el optotipo más adecuado para los cuatro años (E de Snellen o similar), y el 60,7% el más adecuado para los seis años (alfabético).
Un 48,2% dispone de gafas con lentes +2 dioptrías. El 64,3% conoce el uso de las mismas (cribado de hipermetropía). El 50% sabe que la edad adecuada para el cribado es los seis años. El 41,1% lo haría a los cuatro años.
El 62,5% tiene test de Ishihara. El 89,3% conoce su utilidad para el cribado de la percepción de los colores; el 71,4% realizaría esta exploración entre los seis y los ocho años.
Aunque el 92,9% no tiene test para la visión estereoscópica, el 60,7% sabe que se utiliza para el despistaje de la ambliopía y la visión binocular. El 28,6% lo aplicaría a los tres años, edad mínima para que sea valorable.
El 7,1% conoce la AV motivo de derivación a los cuatro años, y el 71,4% la de los seis años.
El 60,7% derivaría preferentemente al oftalmólogo una diferencia de AV entre ambos ojos de 3 puntos; mientras el 33,9% priorizarían tener AV más bajas pero similares en ambos ojos.
El 46,4% considera patológico el estrabismo fijo desde el primer día de vida; el 25% lo considera patológico a partir de los seis meses y un 26,8% a partir de los 12 meses.
El 46,4% considera patológico un estrabismo latente a partir de los seis meses de vida y el 42,9% por encima de los 12 meses.
El 53,6% derivaría al especialista a un niño de tres meses con estrabismo fijo que vemos por primera vez; un 32,1% esperaría a los seis meses y un 12,5% lo haría a los 12 meses.
El 33,9% derivaría al especialista a un niño de seis meses que parece que desvía el ojo hacia afuera, aunque ello no se confirmara en la consulta, cuyos padres lo hubieran observado también en el domicilio. El 53,6% observaría la evolución.
El 58,9% conoce el uso del test de Hirschsberg. Se puede realizar a partir de los 4-6 meses, dato que conoce el 62,5%.
El 60,7% conoce la utilidad del test tapar-destapar. El 75% desconoce cuándo se puede realizar por primera vez.
El 78,6% utilizaría la exploración del reflejo rojo para discernir claridad de estructuras pupilares y descartar leucocoria.
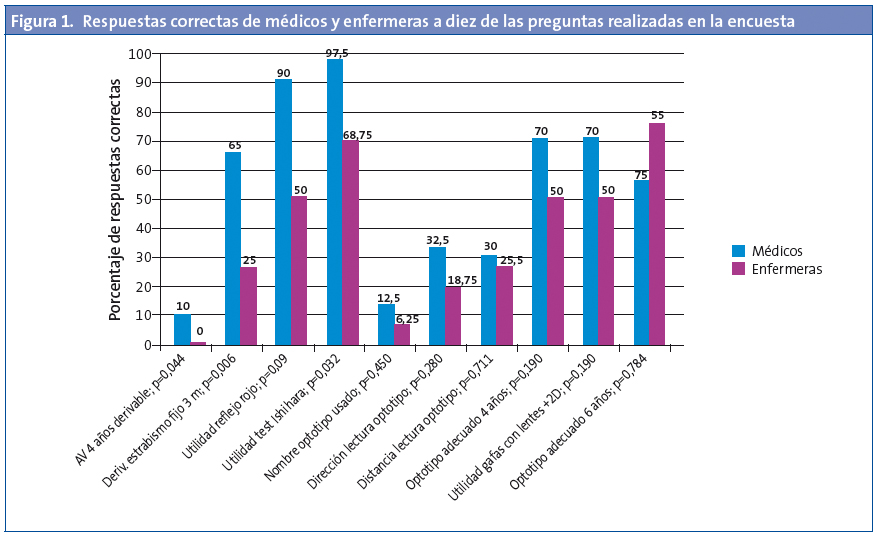
Para saber si la categoría profesional podría influir en las respuestas obtenidas, se realizó un análisis de los datos que constató una diferencia en el número total de aciertos entre médicos y enfermeras estadísticamente significativa (p=0,007).
Los médicos respondieron correctamente una media de 11,47 preguntas (49,89%; intervalo de confianza del 95% [IC 95%]: 45,20 a 54,58), con un rango de 3-16. Las enfermeras respondieron 8,56 preguntas de media (37,23%: IC 95%: 28,52 a 45,94) con un rango entre 3 y 16. En la Fig. 1 se pueden observar las respuestas correctas de médicos y enfermeras a diez de las preguntas realizadas.
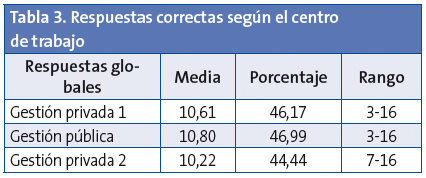
Para saber si el ámbito laboral de los profesionales, es decir, trabajar en un centro de gestión pública o en los diferentes centros de las dos entidades de gestión privada, podría influir en los resultados, se compararon las respuestas de las tres entidades. La Tabla 3 recoge estos resultados. No se observó diferencia estadísticamente significativa entre ellas (p=0,922).
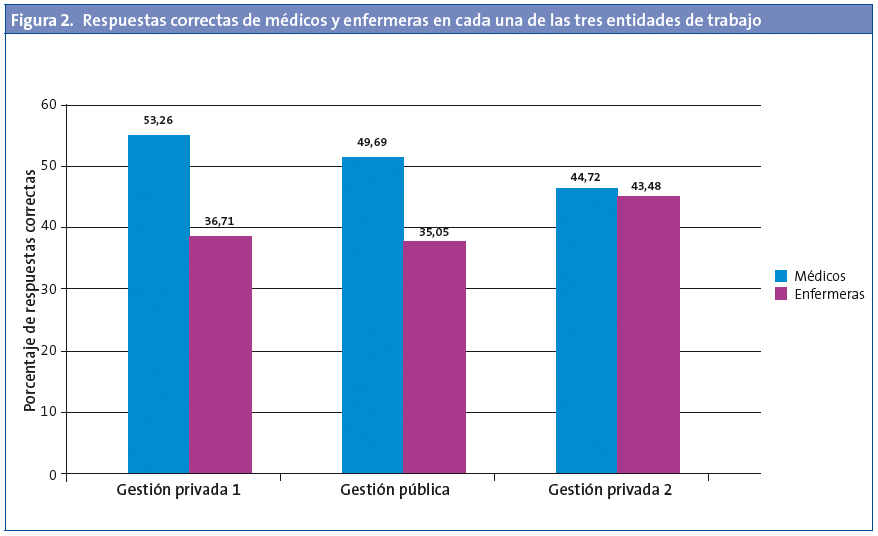
Se analizó si había diferencias entre las categorías profesionales en cada uno de los ámbitos laborales. Ni el porcentaje de aciertos de los médicos ni el de las enfermeras mostraron diferencias estadísticamente significativas entre entidades (p=0,482 y p=0,859, respectivamente). La Fig. 2 recoge las respuestas correctas de médicos y enfermeras en cada una de las tres entidades.
DISCUSIÓN
Para realizar un correcto cribado visual, lo fundamental es disponer del material adecuado, saber utilizarlo y conocer las características de la visión en cada edad, los signos de alarma y cuándo derivar al especialista. Difícilmente esto puede ser llevado a cabo cuandoun tercio de los encuestados no dispone de ningún optotipo y solo un poco más de un tercio dispone de optotipos para todas las edades. Dos tercios no conocen la distancia ni la dirección de lectura. Las enfermeras realizan el cribado en muchas ABS, pero menos de la quinta parte de ellas conoce la dirección de lectura y solo la cuarta parte conoce la distancia.
A lo anteriormente enumerado podríamos añadir los inconvenientes atribuibles al optotipo utilizado (Wecker).
Según las recomendaciones del grupo PrevInfad, lo ideal sería utilizar optotipos que permitan determinar todo el rango de la AV; es decir, desde 0,1 hasta 1 con la escala decimal. Esto es posible en aquellos que tienen al menos diez líneas, como el de Snellen, o los nuevos optotipos logarítmicos. Se debe empezar la lectura de arriba abajo, cada una de las líneas de forma horizontal, sin saltarse letras de la fila, cada uno de los ojos por separado, y posteriormente con ambos. Se considera una lectura correcta si no hay más de dos fallos por línea. La AV será la inmediatamente superior a la fila considerada fallida.
El optotipo del que disponen los centros no es ninguno de los recomendados por el PAPPS de Cataluña (Allen, Pigassou, E de Snellen). Se comprobó que el optotipo presente era el de Wecker de dibujos, el alfabético o ambos. Con él no es posible determinar todo el rango de la AV. Esto puede ocasionar problemas a la hora de diagnosticar una anisometropía. Para su diagnóstico se precisa una diferencia de visión de un 10% o más entre ambos ojos o tres líneas o más de diferencia de la escala decimal completa. En el optotipo de Wecker, las dos últimas líneas corresponden a 0,66 y a 1. Es decir, hay una diferencia de más de tres puntos. Si un niño ve con un ojo la fila de 0,66 y con el otro la de 1, deberíamos derivar al oftalmólogo. Pero no nos permite saber si con uno de los ojos sería capaz de leer filas intermedias de AV, por ejemplo 0,8 (porque no la tiene), que haría innecesaria dicha derivación.
Si dispusiéramos de un optotipo que tuviera filas para todos los rangos de AV, –como el de Snellen–, la exploración sería más precisa. Sin embargo, debe ser leído a cinco metros y nuestras consultas tienen una longitud menor, lo cual afectaría a la interpretación del resultado.
Conclusiones
- Nuestro estudio pone de manifiesto la falta de material para cribado visual en muchas consultas y el desconocimiento del personal sobre cómo usarlo.
- Hemos detectado un gran desconocimiento de los profesionales respecto a cuál es el desarrollo visual normal en la infancia, la exploración que se debe realizar según la edad y los motivos de derivación al especialista.
- Los conocimientos para el cribado visual son bajos en todos los profesionales pero existe una diferencia si quien la realiza es médico o enfermera.
- La falta de conocimientos de los profesionales para el cribado visual infantil no depende del ámbito laboral y es similar en todo nuestro entorno.
- Aunque la Atención Primaria es el pilar de la sanidad en nuestro país y la medicina preventiva debería ser estandarte de la misma, la preparación de los profesionales de nuestro entorno para llevar a cabo un correcto cribado visual está muy lejos de ser buena.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS: ABS: Áreas Básicas de Salud • AV: agudeza visual • IC 95%: intervalo de confianza del 95% • PAPPS: Programa de Actividades Preventivas y de Promoción de la Salud.
BIBLIOGRAFÍA RECOMENDADA
- Angulo S, Saiz A, La Vid J, Fernández O, Martínez J, Cañamares S. Campaña de detección de la ambliopía mediante el test de Brückner: resultados finales. Arch Soc Esp Oftalmol. 1992;62(4):281-6.
- Delgado Domínguez JJ. Detección de trastornos visuales. Recomendación. En: Recomendaciones PrevInfad/PAPPS [en línea] [actualizado en julio de 2007; consultado el 30/08/2013]. Disponible en www.aepap.org/previnfad/rec_vision.htm
- Farràs Cubells O. Screening oftalmológico en consulta de Atención Primaria. Congreso SEPEAP, Granada, 2006 [en línea] [consultado el 30/08/2013]. Disponible en www.sepeap.org/imagenes/secciones/Image/_USER_/Talleres_screening_oftalmologico.pdf
- Flores Visiedo CM. Detección precoz de la ambliopía. Pediatr Integral. 2005;9(6):419-25.
- Matilla MT, Buena G. Valoración de la agudeza visual en niños de edad preescolar. Gaceta Óptica. 2004;387:24-5.
- Mengual E, Hueso JR. Ambliopía. Actualización en oftalmología pediátrica, Vol 1. EUROMEDICE. Madrid: Ediciones Médicas S.L.; 2003. p. 17-29.
- Merino Moína M, Delgado Domínguez JJ. Grupo PrevInfad/PAPPS. Taller: Detección de problemas visuales en los niños: cuándo y cómo. I Jornadas de Actualización en Pediatría de Atención Primaria. Madrid, noviembre 2008 [en línea] [Consultado el 30/08/2013]. Disponible en www.ampap.es/docencia/pdf/taller_problemas_visuales.pdf
- Protocolo de Actividades Preventivas y de Promoción de la Salud en la Edad Pediátrica. Generalitat de Catalunya. Departament de Salut; 2008. p. 79-90.
- Puertas Bordallo D. Exploración del niño estrábico. Detección precoz. Pediatr Integral. 2002;6(7):585-94.
- Puertas Bordallo D. Problemas oftalmológicos en Atención Primaria. En: AEPap ed. Curso de Actualización Pediatría 2012. Madrid: Exlibris Ediciones; 2012. p. 413-28.
- Thompson JR. The incidence and prevalence of amblyopia detected in childhood. Public Health. 1991;69(6):796-8.