Vol. 15 - Num. 59
Original Papers
Vision screening in Primary Care: how it is performed?
Ramona Martín Martína, José Ángel Bilbao Sustachab, Antoni Collado Cucòc
aServicio de Pediatría. ABS Marià Fortuny. Reus. Tarragona. España.
bMédico. CAP Riudoms. Riudoms. Tarragona. España.
cMédico Adjunto. CAP Riudoms. Riudoms. Tarragona. España.
Correspondence: R Martín. E-mail: rmartin@grupsagessa.com
Reference of this article: Martín Martín R, Bilbao Sustacha JA, Collado Cucò A. Vision screening in Primary Care: how it is performed? Rev Pediatr Aten Primaria. 2013;15:221-7.
Published in Internet: 11-09-2013 - Visits: 34756
Abstract
Introduction: amblyopia is the most common cause of preventable vision loss in developed countries and it affects 2-5% of the general population. Strabismus affects 3-6%. The primary objective of the vision screening program is early detection of these defects.
Objectives: to verify the existence of basic material in the medical office for vision screening and to evaluate the basic knowledge that professionals who do it should have.
Material and methods: the assessment of the existence of material in the medical office and the basic knowledge recommended by the Spanish Association of Paediatric Primary Care was performed by a survey of 29 questions. The results were subjected to statistical analysis: descriptive analysis, bivariate analysis using t-test and analysis of variance.
Results: 56 people answered our survey: 40 doctors and 16 nurses from 15 Basic Health Areas. Material absence in surgeries: 32.1% optotype, 51.8% +2D lens, 10.7% ophthalmoscope. Ignorance of material utility: 71.4% reading distance optotype, 71.4% optotype reading direction, 60.7% optotype appropriate age, 35.7% +2D lens glasses. Ignorance referral criteria: 92.9% visual acuity at 4 years, 53.6% fixed strabismus, 53.6% latent strabismus, 33.9% anisometropia. Doctors correct answers: 49.89%. Nurses correct answers: 37.23%.
Conclusions: lack of suitable material in surgeries and staff ignorance of how to use it is assessed. Lack of knowledge about normal visual development, exams to carry out and reasons for referral are also revealed. There is difference in screening if it is done by the doctor or nurse. Lack of knowledge is similar in our environment.
Keywords
● Amblyopia ● Strabismus ● Vision screening ● Visual acuityINTRODUCTION
Amblyopia is the most common preventable cause of vision loss in developed countries. It affects 2 to 5% of the general population. Strabismus affects 3 to 6% of the latter; and out of those affected with strabismus 33 to 50% eventually develop amblyopia. It is estimated that up to 20% of children of all ages suffer from significant refractive errors.
In the first six years of life, visual pathways are malleable. During visual development, the brain must receive equally clear and focused images from each eye to “learn” how to see. Any factor interfering with the visual learning process of the brain will result in a decrease in visual acuity (VA).
Early detection of defects of any kind is the main purpose of having a vision screening programme. In this study we attempted to analyse how the screening is implemented in Primary Care.
OBJECTIVES
- Verifying whether medical offices have the basic materials needed to carry out vision screenings.
- Evaluating the basic knowledge that the professionals performing vision screens should have, as specified in the 2008 guidelines of the PrevInfad group of the Spanish Association of Primary Care Paediatrics (AEPap).
MATERIALS AND METHODS
We designed a survey to assess the availability of materials in the offices and the basic knowledge specified in the PrevInfad recommendations. We formulated 29 questions; seven were about materials and 22 about examinations that the PrevInfad guidelines considered basic, reasons for referral to the ophthalmologist, and age at time of referral.
As for the materials that should be available in every office, we designed the questions keeping in mind the recommendations of PrevInfad and the 2008 Catalonia Programme of Healthcare Promotion and Preventative Activities for Paediatric Ages (PAPPS).
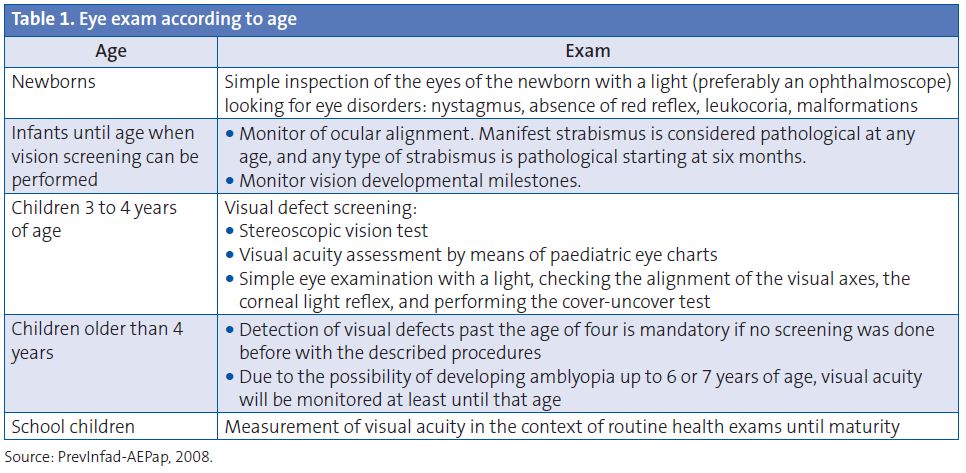
To evaluate the knowledge of healthcare professionals, we designed questions based on the PrevInfad guidelines, shown in Tables 1 and 2.

The survey dada were subjected to the following statistical analyses: descriptive analysis, bivariate analysis (t-test), and analysis of variance.
RESULTS
Of all the individuals we asked to participate in our survey, 78.87% responded; including 88.88% of the physicians (40 out of 45) and 61.53% of the nurses (16 out of 26). Out of the 56 individuals that participated, 40 were physicians and 16 were nurses working in the 15 Basic Healthcare Areas (BHA) of Tarragona, distributed in the following manner: 46.4% from publicly managed BHA centres, 37.5% from BHA centres run by private management organisation 1, and 16.1% from BHA centres run by private management organisation 2.
These were the results of the survey:
An ophthalmoscope was available to 89.3% of the centres. There was no optotype in 32.1% of them. Out of the sites that had an optotype, 37.5% had one for each age group (drawings, incomplete squares, and alphabet charts); 17.9% only had the alphabet chart, and 21.4% only had the drawings chart.
Of all respondents, 89.3% were unaware of the name of the optotype they used (Wecker). The percentage that did not know the distance from which the chart should be read (2.5 metres) was 71.4%. Among respondents, 28.6% knew the chart has to be read horizontally, 48.2% would have the patient read vertically, and 12.5% would have it read at random.
Furthermore, 64.3% knew which optotype was suitable for four-year-olds (Snellen E or a similar one), and 60.7% knew which was most suitable for six-year-olds (alphabet chart).
Frames with +2D lenses were available for 48.2% of respondents. Out of the latter, 64.3% knew how to use them (hypermetropia screening), 50% knew that the appropriate age to do the screening is six years, and 41.1% reported they would screen at four years of age.
The Ishihara test was available to 62.5% of respondents. Its purpose for the screening of colour vision defects was known by 89.3%; and 71.4% reported they would perform this test between six and eight years of age.
Although a stereoscopic vision test was not available to 92.9% of respondents, 60.7% knew it is used for early diagnosis of amblyopia and testing of binocular vision. Among the respondents, 28.6% would perform it at three years of age, the youngest age at which it can be applied.
The VA that warranted a referral at four years of age was known by 7.1%; while 71.4% knew the value for six years of age.
A difference of 3 points in the VA of both eyes would be given a priority referral by 60.7% of practitioners; while 33.9% would give priority referrals to patients with lower VA values similar for both eyes.
Manifest strabismus was considered pathological since birth by 46.4% of practitioners, 25% thought it was pathological starting at six months, and 26.8% starting at 12 months.
Latent strabismus was considered pathological starting at six months from birth by 46.4% of practitioners, while 42.9% considered it was pathological after 12 months of age.
A three-month-old child seen for the first time and presenting with manifest strabismus would be referred to a specialist by 53.6% of practitioners, while 32.1% would wait for six months of age, and 12.5% would do it after 12 months of age.
A six-month-old child with an eye suspected to turn outwards would be referred to a specialist by 33.9% of practitioners, even if this could not be seen during the visit, if the parents had reported seeing it at home; 53.6% would monitor its evolution.
Of all practitioners, 58.9% knew how to use the Hirschberg test, and 62.5% knew that it can be used in children as early as 4 to 6 months after birth.
The purpose of the cover-uncover test was known by 60.7% of practitioners, though 75% did not know the minimum age at which it could be administered.
The red reflex examination would be used by 78.6% to assess for the transparency of ocular media and to rule out leukocoria.
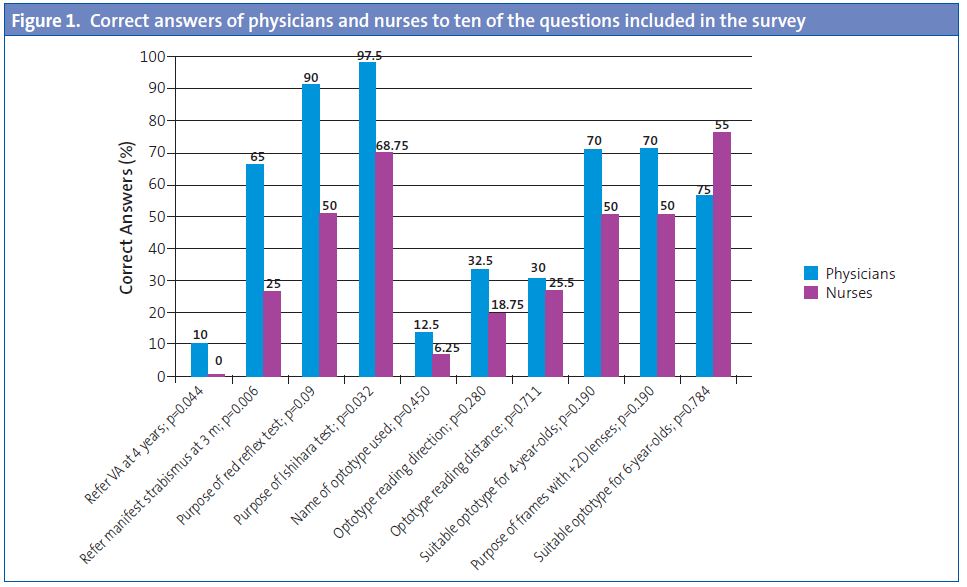
To learn whether the job category could influence the answers we performed an analysis that showed a statistically significant difference in the total number of correct answers for physicians and for nurses (p = 0.007).
On average, physicians answered 11.47 questions correctly (49.89%; 95% confidence interval [CI 95%]: 45.20 to 54.58), and the range was 3-16. Nurses answered 8.56 questions correctly on average (37.23%: CI 95%: 28.52 to 45.94) and the range was 3 to 16. Figure 1 shows the answers of physicians and nurses to ten of the survey questions.
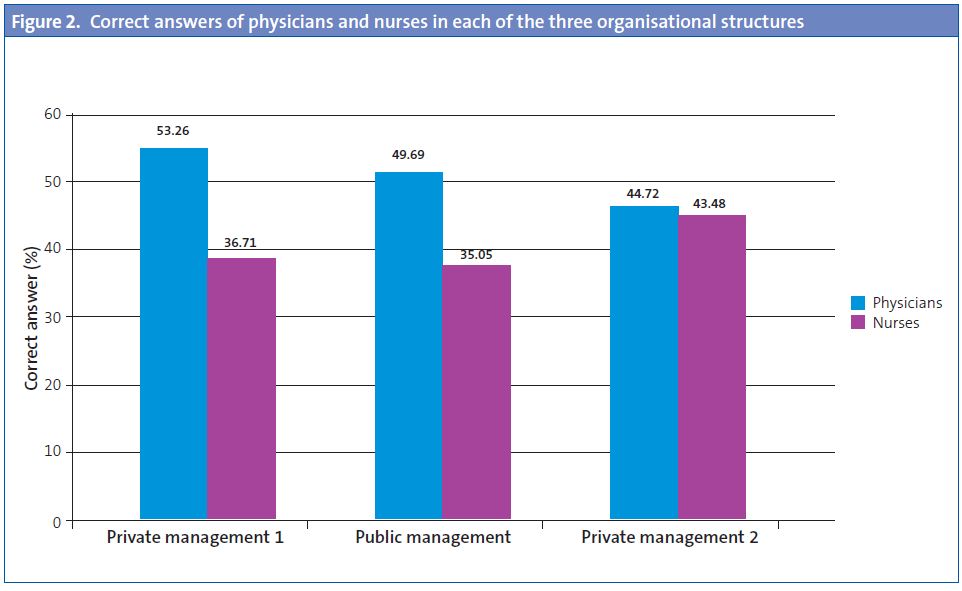
To know whether the work environment of the professionals, that is, whether they worked in a publicly managed centre or in a centre of one of the two privately managed organisations, could influence the results, we compared the answers for the three organisations. Table 3 shows these results. We did not find any statistically significant differences between the three (p=0.922).
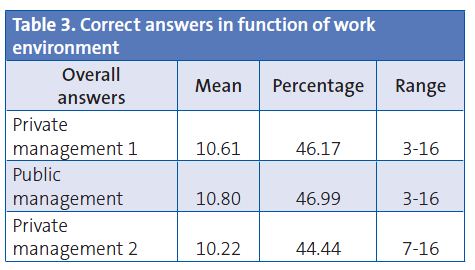
We analysed whether there were differences among professionals working in each of the different work environments. Neither the percentage of correct answers of physicians nor that of nurses showed statistically significant differences between these organisations (p=0.482 and p=0.859, respectively). Figure 2 gathers the correct answers of physicians and nurses in each of the three types of centres.
DISCUSSION
The essential requirements to perform a vision screening correctly are having access to adequate materials, knowing how to use them, and understanding the characteristics of vision in each age group, what the red flags are, and when to refer to a specialist. This can hardly be achieved when a third of respondents have no optotypes and only a little over a third has optotypes for each age group. Two thirds of practitioners did not know how far the child had to read the chart from, nor in which order. Nurses performed the screening in many BHA, but less than a fifth of them knew the reading order, and only one fourth knew the reading distance.
We could add to all of the above the disadvantages that come with the optotype that they were using (Wecker).
According to the guidelines of the PrevInfad group, practitioners ought to use, ideally, optotypes that allow the determination of the full range of VA; that is, charts going from 0.1 to 1 on the decimal scale. This is possible in optotypes that have at least ten rows, such as the Snellen chart, or the new logarithmic optotypes. The charts must be read from the top down, with each row being read horizontally and skipping none of the letters, first with each eye separately, and then with both at the same time. It is considered that a row has been read correctly if the patient does not make more than two mistakes in it. The VA will be that corresponding to the row above the row the patient fails to read.
The optotype available at the centres is not any of those recommended by the Catalonia PAPPS (Allen, Pigassou, Snellen E). We learned that the optotype available was the Wecker drawing or alphabet chart, or both. The Wecker chart does not cover the full range of VA. This can cause some problems when it comes to diagnosing an anisometropia. Its diagnosis requires a 10% or greater acuity difference between both eyes, or a difference of three or more rows in the full decimal scale. In the Wecker optotype, the last two rows correspond to 0.66 and 1. That means that there is a difference of more than 3 points between them. If a child sees the 0.66 row with one eye and the 1 row with the other, the physician has to make a referral to an ophthalmologist. But this chart does not let us know whether the child could read one of the intermediate VA rows with one of his eyes, for instance, the 0.8 row (since the chart does not have one), which would have made the referral unnecessary.
If an optotype with rows for all the values of AV were available—for instance, the Snellen chart—the exam would be more accurate. However, this one needs to be read from a distance of 5 metres, and our offices are not that long, a fact that would affect the interpretation of the results.
CONCLUSIONS
- Our study evinces the lack of materials for visual screening in many offices, and the lack of knowledge of healthcare staff as to how to use them.
- We saw that healthcare professionals had poor knowledge of what constituted normal visual development in childhood, what exams need to be performed depending on the patient’s age, and the circumstances under which they should refer the patient to a specialist.
- The knowledge required for vision screening was low among all professionals, but there was a difference between physicians and nurses.
- The lack of knowledge on paediatric vision screening does not vary according to the work setting, and is similar throughout the whole area under study.
- Although primary care is the pillar of healthcare in our country, and preventative medicine should be its flagship, healthcare professionals in our environment are far from having sufficient knowledge to perform a vision screening correctly.
CONFLICT OF INTERESTS
The authors declare that they had no conflict of interests when it came to preparing and publishing this paper.
ACRONYMS: BHA: Basic Healthcare Areas • VA: visual acuity• CI 95%: 95% confidence interval • PAPPS: Programme of Healthcare Promotion and Preventative Activities
RECOMMENDED BIBLIOGRAPHY
- Angulo S, Saiz A, La Vid J, Fernández O, Martínez J, Cañamares S. Campaña de detección de la ambliopía mediante el test de Brückner: resultados finales. Arch Soc Esp Oftalmol. 1992;62(4):281-6.
- Delgado Domínguez JJ. Detección de trastornos visuales. Recomendación. En: Recomendaciones PrevInfad/PAPPS [on line] [updated 2007 july; consulted on 30/08/2013]. Available on www.aepap.org/previnfad/rec_vision.htm
- Farràs Cubells O. Screening oftalmológico en consulta de Atención Primaria. Congreso SEPEAP, Granada, 2006 [on line] [consulted on 30/08/2013]. Available onwww.sepeap.org/imagenes/secciones/Image/_USER_/Talleres_screening_oftalmologico.pdf
- Flores Visiedo CM. Detección precoz de la ambliopía. Pediatr Integral. 2005;9(6):419-25.
- Matilla MT, Buena G. Valoración de la agudeza visual en niños de edad preescolar. Gaceta Óptica. 2004;387:24-5.
- Mengual E, Hueso JR. Ambliopía. Actualización en oftalmología pediátrica, Vol 1. EUROMEDICE. Madrid: Ediciones Médicas S.L.; 2003. p. 17-29.
- Merino Moína M, Delgado Domínguez JJ. Grupo PrevInfad/PAPPS. Taller: Detección de problemas visuales en los niños: cuándo y cómo. I Jornadas de Actualización en Pediatría de Atención Primaria. Madrid, noviembre 2008 [on line] [consulted on 30/08/2013]. Available on www.ampap.es/docencia/pdf/taller_problemas_visuales.pdf
- Protocolo de Actividades Preventivas y de Promoción de la Salud en la Edad Pediátrica. Generalitat de Catalunya. Departament de Salut; 2008. p. 79-90.
- Puertas Bordallo D. Exploración del niño estrábico. Detección precoz. Pediatr Integral. 2002;6(7):585-94.
- Puertas Bordallo D. Problemas oftalmológicos en Atención Primaria. En: AEPap ed. Curso de Actualización Pediatría 2012. Madrid: Exlibris Ediciones; 2012. p. 413-28.
- Thompson JR. The incidence and prevalence of amblyopia detected in childhood. Public Health. 1991;69(6):796-8.