Vol. 15 - Num. 59
Original Papers
Severe bronchiolitis in infants under six months is a major risk factor for recurrent wheezing
Lorena Pérez Cida, Belén San José Valienteb, Víctor Quintero Calcañoc, Gema Díaz Lópezc, Juan Mesa Guzmánc, Alfonso Cañete Díazc, Alfredo Tagarro Garcíac
aCoordinadora de Investigación Clínica. Hospital Universitario Infanta Sofía. San Sebastián de los Reyes. Madrid. España.
bBioestadística. Investigación Biomédica. Hospital Universitario Infanta Sofía. San Sebastián de los Reyes. Madrid. España.
cHospital Universitario Infanta Sofía. San Sebastián de los Reyes. Madrid. España.
Correspondence: L Pérez. E-mail: lperez_ec@yahoo.es
Reference of this article: Pérez Cid L, San José Valiente B, Quintero Calcaño V, Díaz López G, Mesa Guzmán J, Cañete Díaz A, et al. Severe bronchiolitis in infants under six months is a major risk factor for recurrent wheezing. Rev Pediatr Aten Primaria. 2013;15:229-37.
Published in Internet: 05-09-2013 - Visits: 24651
Abstract
Background: several individual and epidemiological risk factors have been associated with recurrent wheezing after acute bronchiolitis (AB). Few research studies focus on very young infants under six months old.
Objectives: to find what risk factors are associated with recurrent wheezing in young infants (<6 month-old) hospitalized with moderate to severe acute bronchiolitis (AB) at our setting.
Material and methods: a prospective-retrospective, observational study was designed and carried out from January 2009 to December 2011 in a secondary care hospital. Eighty previously healthy patients aged 7-180 days, hospitalized with a first episode of acute moderate AB, were studied.
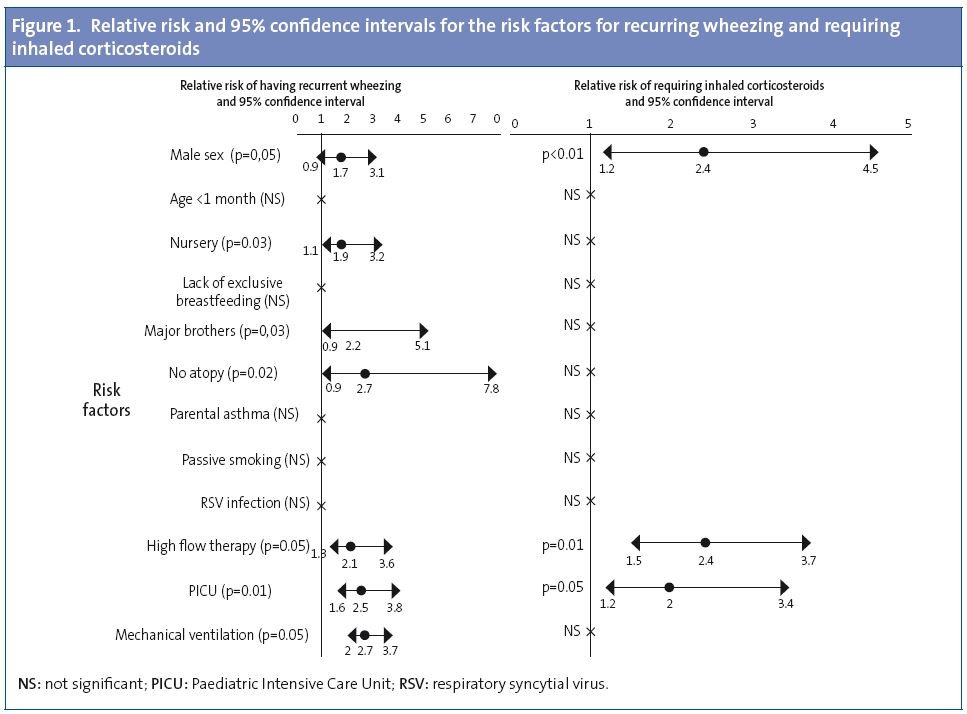
Results: the mean age of infants was 69±42 (range 7-180) days. Crude analysis of relative risk (RR) for recurrent wheezing showed an increased RR in males (p=0.05, RR=1.7 CI 95%: 0.9-3.1), patients in daycare (p=0.03, RR=1.9 CI 95%: 1.1-3.3), with elder siblings (p=0.03, RR=2.2 CI 95%: 0.9-5.1), high-flow therapy (p=0.05, RR=2.1 CI 95%: 1.3-3.6), critical care (p=0.01, RR=2.5 CI 95%: 1.6-3.8), and mechanical ventilation (p=0.05, RR=2.7 CI 95%: 2.0-3.7). After multivariate analysis, daycare attention (OR: 6.06, CI 95%: 1.4-25; p=0.013) and having elder siblings (OR: 4.1, CI 95% 1.1-14.5, p=0.029) were found to be independent risk factors for recurrent wheezing.
Conclusions: daycare attendance and having elder siblings were independently associated with recurrent wheezing. We suggest that severity of bronchiolitis (needing PICU, high flow therapy and mechanical ventilation) is a remarkable risk factor for recurrent wheezing one year after AB.
Keywords
● Asthma ● Atopic disease ● Bronchiolitis ● Recurrent wheezing ● Respiratory syncytial virusINTRODUCTION
Acute bronchiolitis (AB) is the acute infection of the lower respiratory tract, most commonly found in infants. It is defined in broad terms as a lower tract viral infection in children younger than two years. It has an annual incidence of 10-13% in infants and a hospital admissions rate of 2-5%, which has increased significantly in recent years1,2. AB is often more severe and has differential features in the youngest children, compared to older children 12 or 18 months of age. However, clinical research has rarely focused on the first episode of AB in very young infants below six months of age3.
The individual risk factors for severe AB are low birth weight, pre-term birth, and pre-existing chronic diseases (immunodeficiency, and lung, heart, or neurological diseases). The epidemiological and environmental risk factors known for AB are having older siblings, being a twin, passive smoking, being of Native American descent, overcrowding, nursery attendance, and high altitudes4,5.
Children who have had an early episode of AB are at greater risk for having recurrent wheezing episodes. Certain individual genetic, heart, lung, or immunological characteristics may increase the probability of recurrent wheezing associated to viral infections. Children born four months before the winter incidence peak are at greater risk of developing asthma compared to children born 12 months before the peak3. Some epidemiological studies have researched the risk factors for recurrent wheezing or asthma in children zero to three years of age. Pre-term birth, male sex, reduced lung function, exposure to cigarette smoke, respiratory syncytial virus (RSV) and rhinovirus infections, hospitalisation, a family history of asthma, nursery attendance, having older siblings, being fed with formula, and allergy-related factors are some of the identified determinants4-6.
The purpose of the study is to know which risk factors are associated to recurrent wheezing a year following the discharge of infants younger than six months who were previously healthy and were admitted to the hospital for moderate-to-severe AB in our geographical area.
MATERIALS AND METHODS
Population
Retrospective observational study done at Hospital Universitario Infanta Sofía (HUIS). We followed up for a year a cohort of infants admitted to the hospital with their first episode of AB. The recruitment period went from January 2009 to December 2010 (two years). Eligible participants were previously healthy children zero to six months of age, admitted to and discharged from the hospital with a code for AB (491.22) in the International Classification of Disease (9th revision). Every patient participated after we obtained the corresponding informed consent. The AB diagnosis was done on the basis of clinical criteria by hospital paediatricians with over five years of experience. The need to hospitalise the patient was determined by one or more of the following factors: oxygen saturation <94%, difficulty breathing, refusing food, apnoea, septic appearance, or alterations in consciousness. Age alone was not a criterion for admission to the hospital. Initially, all patients that met the inclusion criteria were included in the study. The exclusion criteria were pre-term birth before 35 weeks of gestation, congenital hearth disease, chronic lung disease or neuromuscular disease that could affect lung function, immunodeficiency, and a previous history of wheezing or AB.
Geographical location
The centre where the study was carried out was the HUIS, a secondary care hospital in San Sebastián de los Reyes, Madrid, Spain. The estimated population served by the hospital is 330,000 people, 15% of which are children. Critical patients are transferred to a tertiary care hospital 20 km away (Hospital Universitario La Paz [HULP]).
Risk factors
Based on the literature, the risk factors we evaluated were sex, age, lack of exclusive breastfeeding, nursery attendance, having one or more older siblings, atopy, eosinophilia with counts higher than 400/mm3, asthma in one or both parents, exposure to cigarette smoke (parental smoking), RSV infection, and severity of the episode. We studied the item “requiring oxygen therapy during hospital stay”, but also evaluated severity levels that have not been described before as risk factors, such as needing high flow oxygen therapy, admission to the Paediatric Intensive Care Unit (PICU), and requiring mechanical ventilation.
Variables
The long-term primary variable was a “recurrent wheezing” diagnosis (yes/no), defined as three or more wheezing episodes in the year following discharge.
The long-term secondary variables were:
- "Emergency room visits" (yes/no): new visits to the emergency room (at the HUIS or the HULP), with a recorded diagnosis of AB, wheezing, or bronchospasm (BS) in the 12 months following discharge.
- "Wheezing episodes" (yes/no): wheezing episodes defined as a medical diagnosis of AB, BS, or medical prescription of bronchodilators in the year following discharge.
- "Inhaled corticosteroids" (yes/no): requiring treatment with inhaled corticosteroids prescribed by a physician in the year following discharge.
- "Readmission" (yes/no): readmissions due to AB/wheezing/BS.
Data collection
Twelve months after discharge, an independent researcher (LP) accessed the electronic clinical histories, which could be done in three ways: a) electronic clinical history records using the Selene® software (Siemens SA, Spain); b) the clinical history restricted access network of the tertiary referral hospital (HULP), and c) Horus® (Horus Group Inc, France), a restricted-access application that gives access to the records of primary care paediatricians. Patients whose histories had no notes, not even for immunisation visits, were considered "lost during the follow-up period". The data were confirmed and completed by means of a telephone survey carried out by two separate researchers (GD and JM). They were entered in a confidential database. This database was analysed by an expert in biostatistics (BS) who used the statistical package SPSS 19 (IBM® Inc, U.S.A.). This study was approved by an institutional committee of the hospital.
Statistical analysis
We have described qualitative data as absolute frequencies and percentages, and quantitative data as mean ± standard deviation, minimum, and maximum. We used the chi-squared test or Fisher’s exact test to compare qualitative data. The comparison of quantitative data between two groups was done by means of the Mann-Whitney U test. The association of risk factors with variables is shown as relative risk (RR) and 95% confidence interval (CI 95%). We performed a multivariate logistic regression analysis to study the relationship between the risk factors and the diagnosis of recurrent wheezing. The variables included in the models were those that came close to statistical significance (p<0.200). We used the log-rank test to compare quantitative data. All the statistical tests were considered essentially bilateral, and the significant p values <0.05.
RESULTS
Descriptive data
a) Recruitment
All children younger than six months with an AB diagnosis were considered for recruitment. Up to 102 infants were considered initially. Twenty-two were eventually excluded. One patient was excluded after developing a sequela following mechanical ventilation (glottic stenosis) that led to several readmissions, another for having congenital Marfan syndrome, and another one for having significant interventricular communication. Two others were excluded due to confusing data, and 17 dropped out during the follow-up period. In the end, we analysed the data for 80 previously healthy patients.
b) Baseline characteristics
Patient ages ranged from 7 days at the day of admission to 18 months at the end of follow-up. The average age of the whole cohort at the time of admission was 69±42 (range: 7-180) days. There were the following associated diagnoses: eight cases of atelectasis (10%), five of pneumonia (6.3%), four of otitis media (5%), one of gastroenteritis (1.3%) and one of influenza (1.3%). Antibiotics were given to 18 (22%) children.
A year later, 31 children (38.8%) had been diagnosed with recurrent wheezing. The average time elapsed between discharge and the diagnosis was 9.4 months.
c) Risk factors
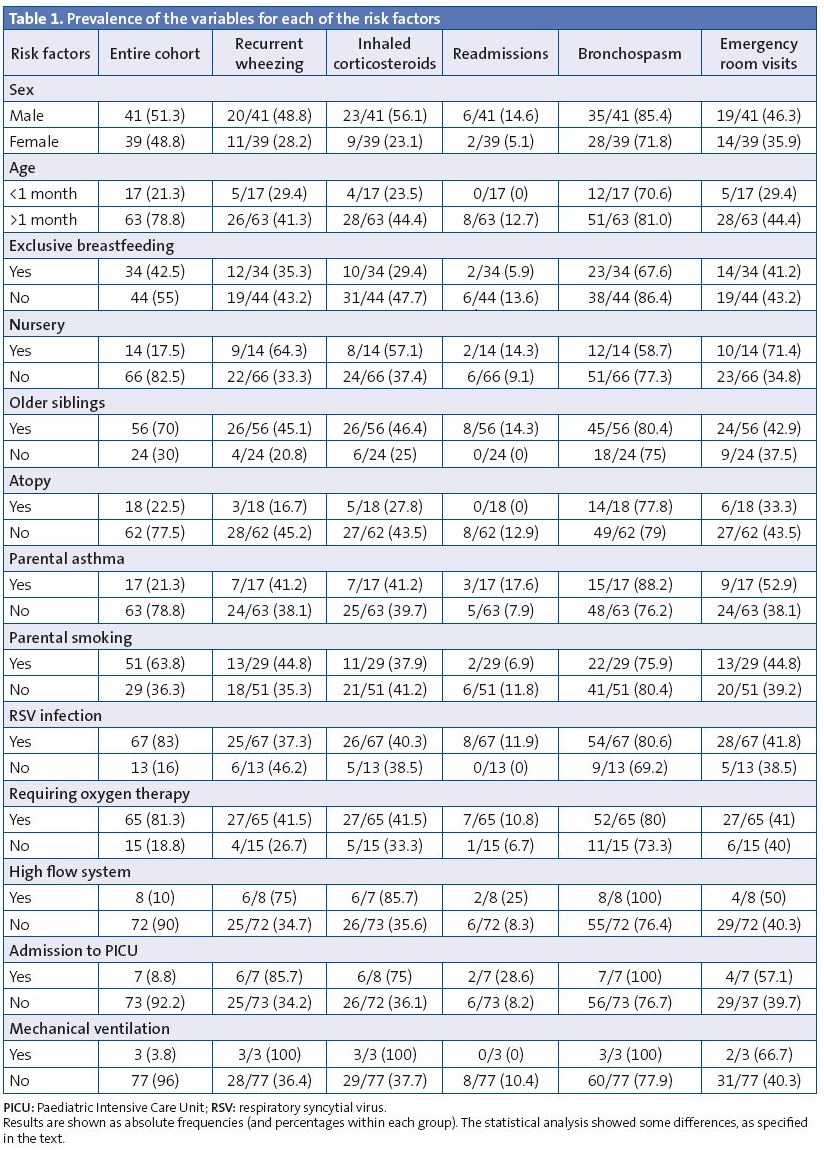
The frequencies of the risk factors in the entire cohort and of the long-term variables are shown in Table 1. We did not do a statistical analysis for eosinophilia, as only 36 patients had blood tests done. The number of new emergency room visits and the number of readmissions were too low to be analysed, so we only show them as dichotomous variables (yes/no).
Analysis
a) Risk factors
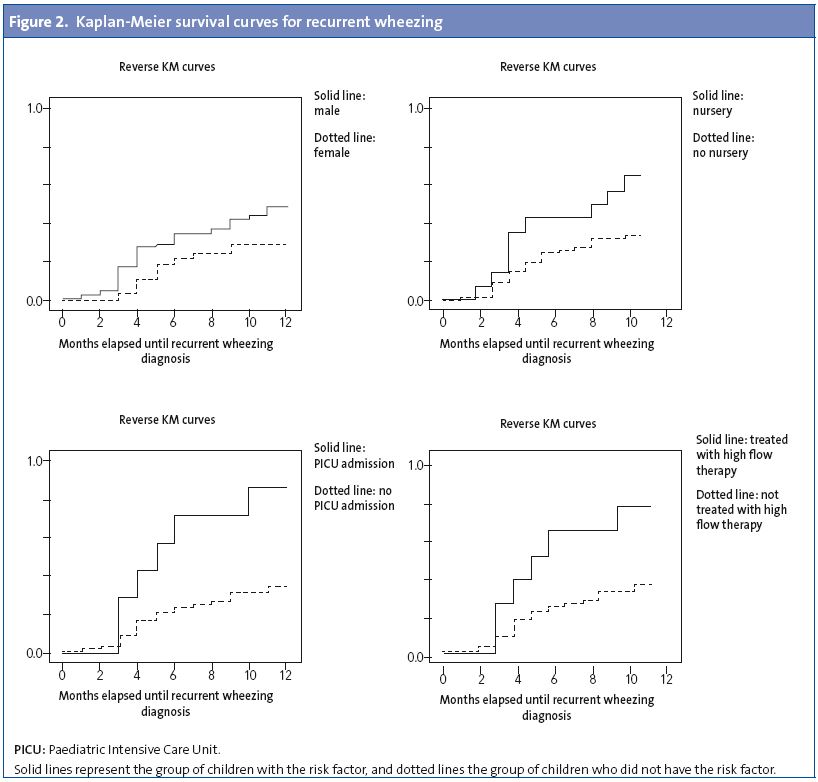
Figure 1 shows the RR for recurrent wheezing and the use of inhaled corticosteroids. We found that nursery attendance was a significant risk factor for emergency room visits (p=0.01; RR: 1.2; CI 95%: 1.02 to 3.02). The lack of exclusive breastfeeding was a risk factor that nearly reached statistical significance (p=0.04; RR: 1.2; CI 95%: 0.98 to 1.6) for wheezing episodes. Figure 2 shows the survival function of recurrent wheezing in relation to the significant risk factors. The multivariate analysis revealed that the following variables were independently associated to the following risk factors:
- “Emergency room visits” variable: nursery attendance (odds ratio [OR]: 4.6; CI 95%: 1.3 to 16.5; p=0.017).
- “Recurrent wheezing” variable: nursery attendance (OR: 6.06; CI 95%: 1.4 to 25; p=0.013) and having one or more older siblings (OR: 4.1; CI 95%: 1.1 to 14.5; p=0.029).
DISCUSSION
This paper presents a retrospective observational study with a cohort of children previously healthy admitted to the hospital with their first case of AB. We limited recruitment to children younger than six months because we believe that early AB has characteristics of its own compared to AB in older children. The risk for recurrent wheezing following an AB episode is inversely proportional to the age at the first AB episode, and it is higher in children younger than four months3. In spite of this, few studies have focused on AB in children younger than six months.
The primary variable in this study was “recurrent wheezing”. We included secondary variables to increase internal consistency, assuming that children with recurrent wheezing usually require treatment with inhaled steroids and that they present with more episodes that require bronchodilators or emergency room visits.
We considered as risk factors all of those previously identified as such, and added to them severity levels (requiring oxygen therapy, high-flow oxygen therapy, admission to the PICU, and mechanical ventilation). We excluded patients who had been born pre-term before 35 weeks of gestation. Nursery attendance and having older siblings were independently associated to recurrent wheezing in the multivariate analysis. The former also was associated with a higher number of emergency room visits. As we stated above, attending nursery was also a significant risk factor for recurrent wheezing, and having one or more older siblings nearly reached statistical significance. These two factors are strongly associated with higher rates of viral infection transmission. We know that infection with RSV or rhinovirus may trigger new episodes of wheezing in susceptible patients. Several studies have proven that wheezing caused by RSV and by rhinovirus in early childhood (0-3 years of age) are important predictors for the subsequent development of asthma (6-13 years)7.
Consistent with various observational data that suggest that male sex is a risk factor for recurrent wheezing, being male was associated with requiring inhaled corticosteroids in the univariate analysis (RR: 2.4; CI 95%: 1.2 to 4.5; p<0.01), and its association to being diagnosed with recurrent wheezing also had a nearly statistically significant p-value and RR (RR: 1.7; CI 95%: 0.9 to 3.1). Some studies have suggested that asthma may be an X-linked recessive disorder8. Males would develop the disease, while females might develop a milder form of it due to the inactivation of the X chromosome. Other studies have suggested a hormone-related influence9. We do not have a more detailed explanation for this tendency.
The study showed that the severity factors (the need for advanced respiratory care or admission to the PICU) were risk factors both for recurrent wheezing and for inhaled corticosteroid therapy. This result is both intuitive and makes sense from a biological standpoint. The greater the damage to the lung while it is still developing, the more severe the sequelae seem to be. Severity (described simply as “admission to the hospital”) has been mentioned in other works, but systematic reviews1 do not specify “mechanical ventilation”, “high-flow oxygen therapy” or “admission to the ICU” as risk factors, so we considered these findings a new discovery. These severity factors could not be subjected to multivariate analysis because the number of critically ill patients was small.
The results of the variables “recurrent wheezing” and “requiring inhaled corticosteroids” ought to be coherent, as a patient younger than 18 months with three or more wheezing episodes should probably be treated with inhaled corticosteroids. This coherence held for some of the risk factors (male sex, severe AB).
Parental smoking and a history of asthma in one or both parents did not appear to be risk factors for this age group, which differs from results published for children up to three years of age who developed asthma later on. This difference may be due to a lower degree of sensitisation to airborne allergens in very young children. We could not study other variables associated to allergies (eosinophilia, positive skin prick testing, elevated IgE, allergic rhinitis), but these results are consistent with Duff’s thesis that wheezing in most infants and young children who present with concurrent catarrhal episodes is non-atopic10.
In our geographical area, children with AB caused by RSV and AB caused by other viruses did not have different outcomes. Other studies with larger samples have published a greater number of admissions to the PICU in patients with an RSV infection2. Patients with high-risk factors for severe RSV-induced AB (pre-term birth, congenital heart disease) were excluded from our study, which could account for this inconsistency.
It is interesting that passive smoking was not associated to wheezing. We ought to note that there was a high proportion of parents who smoked in this study. This means that a selection bias may have occurred.
There are several limitations to this study. The population of the study is relatively small. The evidence obtained from a non-randomised observational study has limitations. Clinical interventions may not have been absolutely uniform. They were not performed by the researchers, but by various physicians who may have followed different diagnostic and treatment criteria. We cannot state with certainty that all wheezing episodes were actually recorded. Emergency room visits may have been due to various factors other than the severity of the condition.
The strengths of this study are that the population is well defined, there was a low attrition rate, the follow-up was complete, the analysis thorough, and the coherence between various long-term variables.
CONCLUSIONS
- Nursery attendance and having older siblings were associated independently to recurrent wheezing.
- The results suggest that acute illness is a considerable risk factor for recurrent wheezing a year after AB.
- As paediatricians, we must be aware of the higher risk for recurrent wheezing in children with this profile in order to foresee potential complications.
CONFLICT OF INTERESTS
The authors declare having no conflict of interests in relation to the preparation and publication of this paper.
ACRONYMS: AB: acute bronchiolitis • BS: bronchospasm • HUIS: Hospital Universitario Infanta Sofía • HULP: Hospital Universitario La Paz • CI 95%: 95% confidence interval• OR: odds ratio • RR: relative risk • PICU: Paediatric Intensive Care Unit • RSV: respiratory syncytial virus.
BIBLIOGRAPHY
- González de Dios J. Conferencia de Consenso en bronquiolitis aguda. Epidemiología. Revisión de la evidencia científica. An Pediatr (Barc). 2010;72(3):222-40.
- García CG, Bhore R, Soriano-Fallas A, Trost M, Chason R, Ramilo O, et al. A. Risk factors in children hospitalized with RSV bronchiolitis versus non-RSV bronchiolitis. Pediatrics. 2010;126(6):e1453-60.
- Wu P, Dupont WD, Griffin MR, Carroll KN, Mitchel EF, Gebretsadik T, et al. Evidence of a causal role of winter RSV infection during infancy in early childhood asthma. Am J Respir Crit Care Med. 2008;178:1123-9.
- McConnochie KM, Roghmann KJ. Parental smoking, presence of older siblings, and family history of asthma increase risk of bronchiolitis. Am J Dis Child. 1986;140(8):806-12.
- Kusel MM, de Klerk NH, Kebadze T, Vohma V, Holt PG, Johnston SL, et al. Early-life respiratory viral infections, atopic sensitization, and risk of subsequent development of persistent asthma. J Allergy Clin Immunol. 2007;119(5):1105-10.
- Colin AA, McEvoy C, Castile RG. Respiratory morbidity and lung function in preterm infants of 32 to 36 weeks’ gestacional age. Pediatrics. 2010;126(1):115-28.
- Kotaniemi-Syrjanen A, Vainionpaa R, Reijonen TM, Waris M, Korhonen K, Korppi M. Rhinovirus-induced wheezing in infancy–the first sign of childhood asthma? J Allergy Clin Immunol. 2003;111(1):66-71.
- Mandhane, PJ, Greene JM, Cowan JO, Taylor DR, Sears MR. Sex differences in factors associated with childhood-and adolescents-onset wheeze. Am J Respir Crit Care Med. 2005;172:45-54.
- Herr M, Just J, Nikasinovic L, Foucault C, Le Marec AM, Giordanella JP, et al. Influence of host and environmental factors on wheezing severity in infants: findings from the PARIS birth cohort. Clin Exp Allergy. 2012;42(2):275-83.
- Duff AL, Pomeranz ES, Gelber LE, Price GW, Farris H, Hayden FG, et al. Risk factors for acute wheezing in infants and children: viruses, passive smoke, and IgE antibodies to inhalant allergens. Pediatrics. 1993;92(4):535-40.





