Vol. 25 - Num. 100
Original Papers
Social problems: high frequency, low training
M.ª Llanos de la Torre Quiraltea, Rafael Jiménez Alésb, Raquel Páez Gonzálezc, Nisa Boukichou Abdelkaderd, Antonio Gancedo Barandae, M.ª Luisa Poch Olivéf
aPediatra. CS Labradores. Logroño. España
bPediatra. CS La Roda de Andalucía. Sevilla. España.
cPediatra. CS 5B. Albacete. España.
dEstadística. Unidad de Ciencia del Dato. Innovación Sanitaria de Fundación Rioja Salud. Centro de Investigación Biomédica de La Rioja (CIBIR). Logroño. La Rioja. España.
eServicio de Pediatría. Hospital Universitario Fundación Alcorcón. Madrid. España
fServicio de Neuropediatría. Hospital San Pedro. Logroño. España
Correspondence: MLL de la Torre. E-mail: mpmjlj@gmail.com
Reference of this article: de la Torre Quiralte MLL, Jiménez Alés R, Páez González R, Boukichou Abdelkader N, Gancedo Baranda A, Poch Olivé ML. Social problems: high frequency, low training . Rev Pediatr Aten Primaria. 2023;25:389-98. https://doi.org/10.60147/a08fe31c
Published in Internet: 29-11-2023 - Visits: 9542
Abstract
Introduction: paediatric social disease in relation to socioeconomic inequities, dysfunctional family relationships, immigration, addiction, violence towards children, etc has been increasing. The aim of this paper is to analyse the importance of social disease in paediatric practice and describe the training and knowledge of providers on this subject and the perceived barriers to their involvement in these issues.
Methodology: multicentre study by means of an online survey with participation by 407 medical professionals. We analysed 11 social problems related to the family and school environment, poverty, immigration, substance use and violence.
Results: problems in the family or school environment were reported as frequent or highly frequent by approximately 50% of the respondents; problems related to immigration, bullying and poverty, by 20-30%; and problems related to violence or addiction by less than 10%. However, the percentage of respondents that reported receiving training (and having knowledge) were very low for all topics (the frequency of training was highest for gender violence and abuse). We analysed the results based on the care setting (hospital or primary care), geographical setting (urban or rural) and age of the provider. The greatest barrier reported by professionals in tackling these problems was precisely the lack of training.
Conclusions: paediatricians encounter social disease frequently in their everyday practice. For this reason, adequate and up-to-date training on the subject is required to detect and treat social disease like any other childhood problems. Some improvement strategies are proposed.
Keywords
● Family problems ● Paediatric training ● Poverty ● Social determinants of health ● Social problems ● ViolenceINTRODUCTION
In recent decades, paediatric social disease has increased enormously in association with socioeconomic inequities, dysfunctional family relationships, immigration, addiction, violence towards children, etc.1 This situation calls for a change in the management of children, currently focused on disease (and on acute conditions), to take into account social determinants of health, in a coordinated, multidisciplinary approach centred on the child and the surrounding environment.
Paediatricians are in a privileged position to identify red flags and risk factors. The intrinsic nature of social problems entails a significant degree of suffering in children and their families, which results in an increased demand for health care services. Observing the interactions of paediatric patients with their immediate environment during hospitalizations, routine visits to monitor growth and development (in the context of the child health prevention and promotion programme) and the management of acute conditions at the primary care (PC) level allows us to form a view of the child from a holistic perspective. This requires coordination between the different levels of care, as well as between family physicians (and nursing staff) and school, association and social services representatives to obtain a perspective that would allow the detection of adverse events and supporting children in overcoming them.
To achieve this, professionals need to be knowledgeable, want to engage, and have the ability to inquire (training, involvement, and resources).
The appropriate detection of social problems mistakenly considered 'minor' (caused by poverty or immigration, family problems, schoolmates or other children, an acrimonious parental separation, etc), which we frequently encounter in everyday practice, would allow an improved management of affected children and ameliorate to a large extent the very deleterious impact of these issues on their future adult lives. Most serious social problems (abuse, treatment, violence, addiction) are preceded by the lesser problems mentioned above.
The aim of our study was to assess the burden of social problems in current paediatric practice, the training and knowledge of clinicians on the subject and the perceived barriers to their management. The purpose was for the results to guide the development of strategies to improve patient care.
METHODS
We conducted a multicentre study approved by the Clinical Research Ethics Committee of La Rioja (Ref. CEImLAR P.I. 532), for which the research team developed and validated an ad hoc questionnaire.2
The study had a cross-sectional descriptive design and was carried out through an online survey using the Google Forms platform. The questionnaire was distributed nationwide to physicians who provided cared to minors (paediatricians, family and community medicine practitioners and medical intern-residents [MIR] in those two specialities) through the mailing lists of the Asociación Española de Pediatría (AEP, Spanish Association of Pediatrics) and affiliated regional societies, the Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics), the Sociedad Española de Pediatría Social (Spanish Society of Social Paediatrics), Sociedad Española de Medicina de la Adolescencia (Spanish Society of Adolescent Medicine), Asociación MIR España (Spanish MIR Association) and Sociedad Española de Medicina de Familia y Comunitaria (Spanish Society of Family and Community Medicine) and the RedIRIS network Primary Care Paediatrics mailing list, which includes professionals in the aforementioned fields involved through different research groups, submitting a link to the questionnaire for its voluntary and confidential completion. The estimated size of the target population was 12 000,3,4 so a sample size of 373 responses would be required for a 95% confidence level. We obtained 407 valid responses. The questionnaire was available in June and July 2021.
The study was endorsed by the Sociedad Española de Pediatría Social.
The questionnaire was used to collect data on the sociodemographic characteristics of the respondents (Table 1) and the frequency and type of training on social problems and the perceived knowledge of the social problems affecting minors, all of it in relation to the last 3 years (Table 2). We also obtained data on the barriers perceived by clinicians in the management of social problems (Table 3).
| Table 1. Sociodemographic data | ||
|---|---|---|
| Total (407) | Age | |
| Sex | ||
| Male | 70 | 52 |
| Female | 335 | 46 |
| Declined to state | 2 | |
| Age | ||
| ≤47 years | 194 | |
| >47 years | 213 | |
| Care setting | ||
| Hospital, exclusively | 83 | 43 |
| Primary care, exclusively | 275 | 47 |
| Geographical setting | ||
| Urban | 352 | 47 |
| Rural | 53 | 48 |

| Table 2. Problems under study |
|---|
Responses of Likert scale ranging from 1 to 5
|
| Problems related to acrimonious parental separation (“Divorce”) |
| Other problems in the family (“Family”) |
| Problems related to school bullying (“Bullying”) |
| Other problems related to the school setting (“School”) |
| Problems related to parental substance abuse (“Addiction”) |
| Problems related to immigration (“Immigration”) |
| Problems related to poverty (“Poverty”) |
| Violence between parents or caregivers (minor exposed to violence, not against the minor and not meeting the definition of gender violence) (“Interparental violence”) |
| Gender violence (“GV”) |
| Sexual abuse (“Abuse”) |
| Other forms of violence against children from parents/family/caregivers (“Viol. against children”) |

| Table 3. Involvement |
|---|
“To what extent do you agree with the following statements about your involvement in the social problems or needs of the minors you provide care to?”
|
| I don’t have time (“No time”) |
| I don’t have the means to contact other professionals (“No means”) |
| Most professionals I have contacted have not been cooperative the times that I have attempted it (“No collaboration”) |
| I don’t know what resources may be available (“No resources”) |
| I think it falls in the scope of other professions (“Private life”) |
| I think it’s part of the private life of families and that they already tell me what they want me to know (“Private life”) |
| I am not comfortable asking those questions (“Uncomfortable”) |
| I am afraid of hearing the answers and not knowing what to do about them (“Afraid of answers”) |
| I do not think I’m adequately trained to address these problems (“Not trained”) |
| I consider that social paediatrics is a specific branch of paediatrics and that problems in this area should be managed by paediatricians trained in this subspeciality (“Social paediatrics”) |
| Social workers are in charge of assessing and managing social problems (social problems out of the scope of paediatrics) (“Social services”) |

The answers (rated on a Likert scale from 1 to 5) were analysed in relation to the following sociodemographic variables:
- Age of clinician: age < 47 years and age > 47 years (mean age for each answer).
- Care setting/level: hospital or primary care (excluding, for this analysis, responses from clinicians who worked in both settings).
- Characteristics of the catchment population: urban or rural setting (as defined by the National Institute of Statistics of Spain,5 using the postal code of the health facility).
The analysis of the data was carried out with the statistical software JASP and R version 4.3.0. We compared responses by means of the Pearson correlation coefficient and the Mann-Whitney U test. Associations between scores were assessed by means of the Kendall tau-b correlation coefficient (Appendix A).
RESULTS
We obtained 407 responses, 90% (368) from paediatricians (rest: 26 paediatrics residents, 11 family physicians and 2 family medicine residents). Fifty percent of the total worked in the autonomous communities of Madrid, Andalusia or Catalonia, and other regions in Spain were less represented.
The main limitation of the study is that the sample was not selected at random, but obtained through the voluntary participation of 407 professionals, although the wide dissemination of the questionnaire allowed reaching nearly the entire target population.
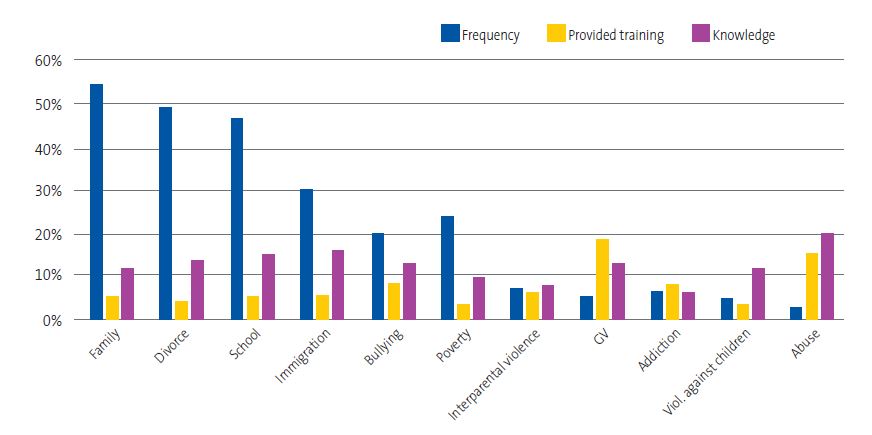
Concerning the frequency of social problems, respondents rated family problems, acrimonious parental separations and problems in the school setting as frequent or very frequent (50-60%). On the contrary, problems involving violence (against children or between the parents, abuse, gender violence) and parental addiction were considered infrequent or rare by most respondents (Fig. 1 and Table 4).
| Table 4. Responses | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frequency (4-5 points: frequent or very frequent) | ||||||||||||
| Primary care (274) | Hospital (83) | ≤47 years (194) | >47 years (213) | Urban (354) | Rural (51) | |||||||
| Family | 158 | 58% | 41 | 49% | 110 | 57% | 113 | 53% | 193 | 55% | 29 | 57% |
| Divorce | 145 | 53% | 32 | 39% | 92 | 47% | 109 | 51% | 175 | 49% | 25 | 49% |
| School | 135 | 49% | 31 | 37% | 97 | 50% | 94 | 44% | 166 | 47% | 24 | 47% |
| Immigration | 85 | 31% | 29 | 35% | 59 | 30% | 65 | 31% | 109 | 31% | 14 | 27% |
| Poverty | 65 | 24% | 23 | 28% | 54 | 28% | 44 | 21% | 86 | 24% | 11 | 22% |
| Bullying | 50 | 18% | 19 | 23% | 48 | 25% | 35 | 16% | 73 | 21% | 10 | 20% |
| Interparental violence | 16 | 6% | 8 | 10% | 15 | 8% | 14 | 7% | 25 | 7% | 4 | 8% |
| Parental addition | 11 | 4% | 12 | 14% | 19 | 10% | 8 | 4% | 25 | 7% | 2 | 4% |
| GV | 11 | 4% | 5 | 6% | 14 | 7% | 8 | 4% | 18 | 5% | 4 | 8% |
| Viol. against children | 9 | 3% | 7 | 8% | 13 | 7% | 7 | 3% | 18 | 5% | 2 | 4% |
| Abuse | 1 | 0% | 8 | 10% | 9 | 5% | 4 | 2% | 12 | 3% | 1 | 2% |
| Provided training (4-5 points: adequate or excellent) | ||||||||||||
| Primary care (274) | Hospital (83) | ≤47 years (194) | >47 years (213) | Urban (354) | Rural (51) | |||||||
| Family | 13 | 5% | 6 | 7% | 15 | 8% | 8 | 4% | 20 | 6% | 3 | 6% |
| Divorce | 12 | 4% | 2 | 2% | 8 | 4% | 10 | 5% | 16 | 5% | 2 | 4% |
| School | 13 | 5% | 6 | 7% | 11 | 6% | 12 | 6% | 22 | 6% | 1 | 2% |
| Immigration | 17 | 6% | 5 | 6% | 10 | 5% | 13 | 6% | 23 | 6% | 0 | 0% |
| Poverty | 5 | 2% | 6 | 7% | 9 | 5% | 5 | 2% | 13 | 4% | 1 | 2% |
| Bullying | 19 | 7% | 10 | 12% | 16 | 8% | 20 | 9% | 32 | 9% | 4 | 8% |
| Interparental violence | 16 | 6% | 8 | 10% | 8 | 4% | 19 | 9% | 26 | 7% | 1 | 2% |
| Parental addition | 20 | 7% | 10 | 12% | 14 | 7% | 19 | 9% | 28 | 8% | 4 | 8% |
| GV | 56 | 20% | 15 | 18% | 34 | 18% | 43 | 20% | 66 | 19% | 8 | 16% |
| Viol. against children | 11 | 4% | 2 | 2% | 5 | 3% | 9 | 4% | 13 | 4% | 1 | 2% |
| Abuse | 34 | 12% | 19 | 23% | 27 | 14% | 35 | 16% | 58 | 16% | 4 | 8% |
| Knowledge (4-5 points: adequate or excellent) | ||||||||||||
| Primary care (274) | Hospital (83) | ≤47 years (194) | >47 years (213) | Urban (354) | Rural (51) | |||||||
| Family | 35 | 13% | 12 | 14% | 13 | 7% | 36 | 17% | 43 | 12% | 6 | 12% |
| Divorce | 42 | 15% | 10 | 12% | 18 | 9% | 37 | 17% | 47 | 13% | 8 | 16% |
| School | 40 | 15% | 19 | 23% | 25 | 13% | 36 | 17% | 51 | 14% | 10 | 20% |
| Immigration | 51 | 19% | 15 | 18% | 22 | 11% | 44 | 21% | 63 | 18% | 3 | 6% |
| Poverty | 29 | 11% | 12 | 14% | 14 | 7% | 27 | 13% | 39 | 11% | 2 | 4% |
| Bullying | 35 | 13% | 15 | 18% | 19 | 10% | 35 | 16% | 49 | 14% | 5 | 10% |
| Interparental violence | 19 | 7% | 13 | 16% | 12 | 6% | 21 | 10% | 32 | 9% | 1 | 2% |
| Parental addition | 17 | 6% | 8 | 10% | 9 | 5% | 18 | 8% | 23 | 6% | 3 | 6% |
| GV | 37 | 14% | 14 | 17% | 20 | 10% | 34 | 16% | 44 | 12% | 10 | 20% |
| Viol. against children | 33 | 12% | 14 | 17% | 19 | 10% | 29 | 14% | 44 | 12% | 4 | 8% |
| Abuse | 50 | 18% | 26 | 31% | 36 | 19% | 47 | 22% | 77 | 22% | 5 | 10% |

Problems associated with immigration and poverty were generally given an intermediate frequency rating (a fourth of respondents rated them as frequent).
The differences were more marked based on the care setting: clinicians working at the primary care level reported a greater frequency of family and school problems, and a very low frequency of managing problems related to violence, abuse or addition (<5%, compared to 10% of hospital-based clinicians). Neither the age of the respondents nor the geographical setting where they worked (urban or rural) were associated with differences in the detection of these problems.
Due to the small size of each group, the differences between them were rarely statistically significant. Still, analysing the correlations between variables (Appendix A), we found that, in general, a greater frequency in the detection of some problems was associated with a greater probability of other problems being detected as well. The strongest correlation corresponded to immigration and poverty. The different variables concerning violence were also positively correlated to parental addiction. Family problems and acrimonious parental separation were also positively correlated to school problems. Lastly, immigration and poverty were positively associated with parental addiction and family problems.
The results evince the scarcity of the offered TRAINING, especially in relation to the problems encountered in the paediatric population. This was the case in every analysed group. Participants only reported receiving adequate training on gender violence (19%) and abuse (15%) (practically double the percentage compared to other social problems). In the hospital setting, the percentage of clinicians trained about social problems was greater compared to primary care (except for gender violence, for which training was more frequent at the primary care level).
The availability of training in any form of violence was associated with an increased frequency of detection of the different forms of violence considered in the analysis.
The representation of clinicians working in rural settings was small (53 de 407), but for all the social problems under study, the percentage that reported training on the subject was lower in rural versus urban clinicians, even though the reported frequency of the problems themselves was practically the same in both geographical settings.
In every group, only 10-20% of respondents reported having adequate knowledge about most of the problems (despite the scarcity of training opportunities, and considering the substantial frequency of these problems). The higher percentage of clinicians with self-reported knowledge compared to the percentage with access to training implies that clinicians are being trained through channels other than the official trainings offered through institutional educational programmes.
There were significant differences in reported knowledge, which was greater in: the hospital setting (for the variables of school problems, bullying, interparental violence and abuse), older professionals (family dysfunction, divorce, poverty) and the urban setting (immigration, interparental violence, abuse). Older professionals generally reported a higher level of knowledge for all aspects under study.
We found a positive correlation between a greater access to training on the analysed social problems and the self-perceived knowledge on those subjects.
Still, we must underscore that, overall, the reported availability of training and the self-perceived knowledge of social problems were poor.
According to the survey results, 54% of professionals noted that the main barrier to their involvement (Figure 2) in social problems was the lack of training on the subject and a lack of knowledge of the available resources to resolve or improve these problems (38%). One fourth of respondents reported that they did not feel comfortable exploring these issues and even worried that they would not know what to do about what they found out from the minors and their families. Lack of time was also a barrier reported by 28% of respondents.
| Figure 2. Involvement: barriers hindering involvement in social problems (4-5 point responses on a 1-5 point scale) |
|---|
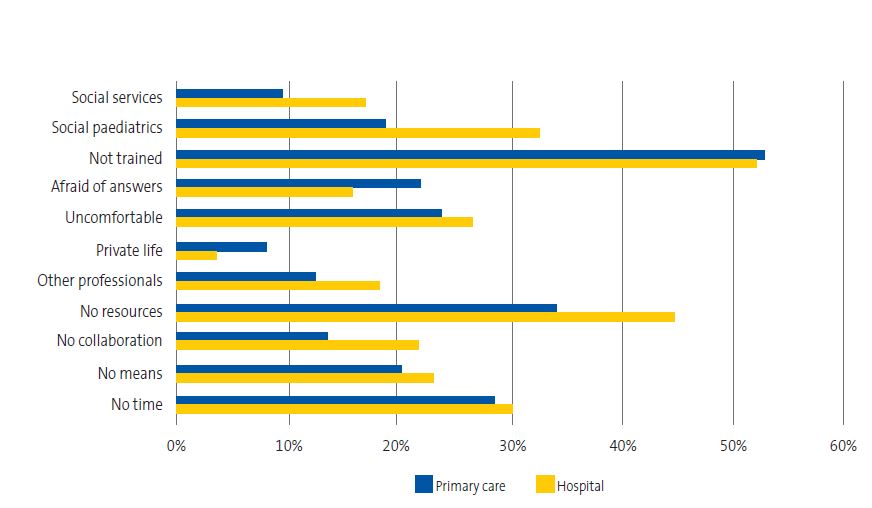 |

Only 11% of the sample considered that social problems were not within the scope of paediatric practice (compared to 71% who believed they were).
We found that clinician involvement increased with age (as knowledge increased).
In response to the item “I consider that social paediatrics is a specific branch of paediatrics and that problems in this area should be managed by paediatricians trained in this subspeciality”, 22% of participants expressed agreement (52% disagreed). This difference was more marked in the analysis stratified by care setting. Thirty-three percent of hospital clinicians responded that these issues should be managed by specialists in social paediatrics (another 33% disagreed). However, only 19% of primary care clinicians agreed with this stat3ement (and 57% disagreed).
Overall, the correlation analysis showed that the greater the training, the greater the reported knowledge; the greater the knowledge, the greater the frequency of detection and the degree of involvement (with fewer perceived barriers to the management of these problems).
DISCUSSION
The detection of social problems and their appropriate management can be taught as well as learned.6-8 The definition of paediatrics includes social paediatrics as a fundamental part of the specialty, as well as a biopsychosocial approach in the management of children and adolescents.9
Both the International Classification of Diseases of the World Health Organization (WHO) (ICD-11: https://icd.who.int/es) and the International Classification of Primary Care of the World Organization of Family Doctors (WONCA) (ICPC-2: www.who.int/standards/classifications/other-classifications/international-classification-of-primary-care) expanded the reasons for encounter with a biopsychosocial approach, offering codes to document social problems in health records. Thus, social problems should also be included in the basic training of those professionals who provide care for minors.10-12
The findings of our study show that there are some very frequent social problems for which little training is given and, therefore, are approached by clinicians with scarce knowledge and possibly with concern that they may manage them incorrectly, perhaps to the point that some may think that given the lack of training on the subject, these problems are outside the scope of paediatric practice.
The most frequent problems were not those involving violence against minors (fortunately), but circumstances in the immediate environment that affected children, as well as their families and their communities, so that the issues of the child may be overlooked among the problems of the family or community where the child lives (as may be the case of immigrant or Romani children).13
In children, these problems cause numerous symptoms, discomfort and suffering, and impact their psychological, emotional and social development, in addition to poorer academic performance and an increased risk of disease in the short, medium and long term. With this holistic and integrated perspective, paediatricians must gain detailed knowledge not only of the family but also the social environment of their patients, the local factors contributing to inequities or violations of children’s rights, the social support network and any gaps in it. They must also be aware of the positive influence of whatever support network is available, which affects the outcomes of these problems and how patients experience and cope with them,14 never forgetting that both risk and protective factors do not have a direct cause-effect relationship with these problems, but are associated with their probability.15
In fact, intervention and the provision of support to overcome these problems or minimise their deleterious impact would also help identify and reduce problems associated with abuse and violence against children.16,17
As regards the frequency of detection of social problems and the level of training and knowledge in specific care settings (hospital/primary care), we ought to mention that although 59% of the paediatrician positions of the national health system are allocated to the primary care level, paediatrics residency training chiefly takes place in the hospital, so that, in adherence to the official curriculum for the specialty, paediatrics residents spend only 6% of the residency period in PC.18,19
Perhaps the fact that more severe social problems (violence) end up being managed at hospital plays a part in the greater emphasis of medical training on these problems, when others are much more prevalent. One example is parental divorce (one of the most frequently detected problems, according to our findings), which has a profound impact on the lives of children, as it causes changes in their daily care and may entail changing schools, the introduction of new parental partners, which requires adaptation, etc, which in our practice may present in the form of behavioural problems, anxiety, abdominal pain, headache or poor academic performance.20
As is the case of any other disease, the first step in the management of these patients is to obtain a full history.21,22 The social history is a necessary part of the history-taking and health records, and should be the essential tool from which to approach health problems with a holistic perspective, to activate protection or prevention mechanisms in patients at risk, or simply to understand and interpret many of the presenting signs or symptoms in paediatric patients.
Thus, we found that social problems often converge, amplifying the deleterious impact. One obvious example is poverty, which is frequently associated with immigration, a single-parent family structure, addiction, violence…23-25 Neglect, understood as failure to meet a need resulting in harm, is the most frequent type of abuse, yet the least frequently detected.1 It is important to remember that neglect can exist beyond the material sphere (it is often emotional or social), so its detection requires active searching by professionals.
As health care professionals, we have the opportunity and the responsiblity to take these factors into account in our practice, given that, frequently, “the availability of good medical [or social] care tends to vary inversely with the need for it in the population served” (Inverse Care Law, Hart).26
We would never allow such low level of training and knowledge for a physical problem if it were this frequent among the children whom we serve. The assessment of vulnerability in order to protect minors is an ethical imperative for the entire community, but especially for those of us whose duty is the care of children and their families.27-29 The entire field of paediatrics is social paediatrics, as there cannot (nor should) be another way to understand paediatrics nor another way to approach childhood. Our lack of engagement (largely motivated by a lack of training, as evinced by our findings) makes us contribute to institutional child abuse.30
Our study evinced that the training received by health care professionals responsible for the management of paediatric patients and their perceived knowledge about social problems are far from sufficient to provide adequate care. Ideally, training on the subject would start at the undergraduate level, but at minimum it is essential that adequate education on the management of social problems is provided in the paediatrics speciality training programme.
For this reason, we consider the following necessary:
- Conceiving violence as a health problem (it would be easier to include it in training programs from the beginning).
- Increasing training on social determinants of health and adverse childhood experiences.
- Training of professionals who care for children on the development of healthy bonds with point persons, adequate interaction with the environment and emotional regulation
- Institution of home visiting programmes to meet the social circumstances of the minors managed in paediatric practice.
- Development of effective and efficient systems for coordination of primary and hospital-based care, involving nurses (including midwives), family physicians (children do not live on their own) and other specialised community-based services: social services, mental health, education and, if necessary, state law enforcement and protective services and the legal system.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
AUTHORSHIP
All authors contributed equally to the preparation of the published manuscript.
REFERENCES
- Romeo Biedma FJ, Horno Goicoechea P. Ver para proteger. Claves para comprender la violencia contra niños, niñas y adolescentes y para desarrollar medidas de protección eficaces. UNICEF España; Dirección de sensibilización y políticas de infancia. Área de incidencia política y estudios. 2022 [en línea] [accessed 09/08/2023]. Available at www.observatoriodelainfancia.es/oia/esp/descargar.aspx?id=7872&tipo=documento
- Jiménez Alés R, Páez González R, De la Torre Quiralte MLL, Poch Olivé ML, Boukichou Abdelkader N, Andrés Esteban EM. Creación y validación de un instrumento para cuantificar actitudes, conocimientos y dificultades en el abordaje de los problemas sociales. An Pediatr (Barc) 2023;98(6):418-26. https://doi.org/10.1016/j.anpedi.2022.12.010
- Ministerio de Sanidad. Portal Estadístico. Área de Inteligencia de Gestión. Sistema de Información de Atención Primaria (SIAP). Número de profesionales. Pediatría [online] [accessed 09/08/2023]. Available at: https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/S/sistema-de-informacion-de-atencion-primaria-siap
- Ministerio de Sanidad. Portal Estadístico. Área de Inteligencia de Gestión. Sistema de Información de Atención Especializada (SIAE). Número de profesionales. Pediatría [online] [accessed 09/08/2023]. Available at https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/S/siae
- Ministerio de Transportes, Movilidad y Agenda Urbana, 2021. Áreas Urbanas en España 2021. Madrid: Ministerio de Transportes, Movilidad y Agenda Urbana, 21-39 [online] [accessed 09/08/2023]. Available at https://cvp.mitma.gob.es/downloadcustom/sample/3152
- Hardcastle K, Bellis MA. Asking about adverse childhood experiences (ACEs) in general practice: evaluation findings from a pilot study in Anglesey. North Wales, Cardiff: Public Health Wales, 2019 [online] [accessed 09/08/2023]. Available at www.researchgate.net/publication/332222562_Asking_about_adverse_childhood_experiences_ACEs_in_General_Practice_Evaluation_findings_from_a_pilot_study_in_Anglesey_North_Wales
- Szilagyi M, Kerker BD, Storfer-Isser A, Stein RE, Garner A, O'Connor KG, et al. Factors Associated With Whether Pediatricians Inquire About Parents' Adverse Childhood Experiences. Acad Pediatr. 2016;16:668-75. https://doi.org/10.1016/j.acap.2016.04.013
- Thang C, Kucaj S, Forkey H, Lopez N, Ocampo A, Inkelas M, et al. Training Pediatric Interns to be Trauma-Responsive Providers by Adapting a National Evidence-Informed Curriculum for Pediatricians. Acad Pediatr. 2023;23:219-21. https://doi.org/10.1016/j.acap.2022.02.020
- Programa oficial de la especialidad de Pediatría y sus Áreas específicas [online] [accessed 09/08/2023]. Available at: www.boe.es/eli/es/o/2006/09/20/sco3148
- Martínez González C. Ser pediatra en tiempos de pandemia. Form Act Pediatr Aten Prim. 2022;15(1):1-3.
- Kerker BD, Storfer-Isser A, Szilagyi M, Stein RE, Garner AS, O'Connor KG, et al. Do Pediatricians Ask About Adverse Childhood Experiences in Pediatric Primary Care? Acad Pediatr. 2016;16:154-60. https://doi.org/10.1016/j.acap.2015.08.002
- Hardcastle K, Bellis MA, Sharp CA, Hughes K. Exploring the health and service utilisation of general practice patients with a history of adverse childhood experiences (ACEs): an observational study using electronic health records. BMJ Open. 2020;25:10. https://doi.org/10.1136/bmjopen-2019-036239
- Estrategia Nacional para la Igualdad, Inclusión y Participación del Pueblo Gitano 2021-2030. Ministerio de Derechos Sociales y Agenda 2030. Gobierno de España [online] [accessed 09/08/2023]. Available at www.mdsocialesa2030.gob.es/derechos-sociales/poblacion-gitana/estrategia-nacional/futura-estrategia.htm
- Sánchez Vázquez AR. Apego y experiencias adversas en la infancia. In: Problemas psicosociales en Pediatría. Continuum 2021 [online] [accessed 09/08/2023]. Available at https://continuum.aeped.es/modules/listado/1027
- Martínez Bernat l, Villar Villar G. Recién nacido con riesgo social. Pediatr Integral 2019;XXIII(3):154-160.
- Pinto Rubio M, Zabaleta Rueda A, Gorrotxategi Gorrotxategi P. Las experiencias adversas en la infancia. Detección precoz y prevención de sus consecuencias. Form Act Pediatr Aten Prim. 2023;16:49-53.
- Conn AM, Szilagyi MA, Jee SH, Manly JT, Briggs R, Szilagyi PG. Parental perspectives of screening for adverse childhood experiences in pediatric primary care. Fam Syst Health. 2018;36:62-72. https://doi.otg/10.1037/fsh0000311
- Fernández-Cuesta Valcarce M.A., Villaizán Pérez C. Incremento de la rotación del residente de pediatría por el centro de salud, ¿una opción para mitigar la crisis de la pediatría de atención primaria? An Pediatr (Barc) 2022;97:77-8. https://doi.org/10.1016/j.anpedi.2022.06.018
- Green C, Stein REK, Storfer-Isser A, Garner AS, Kerker BD, Szilagyi M, et al. Do Subspecialists Ask About and Refer Families with Psychosocial Concerns? A Comparison with General Pediatricians. Matern Child Health J. 2019;23:61-71. https://doi.org/10.1007/s10995-018-2594-y
- Mardomingo MJ, Seijo. Psicopatología de los hijos en los procesos de ruptura de pareja. In: Fariña Rivera F, Ortuño Muñoz P (eds.). La gestión positiva de la ruptura de pareja con hijos. Valencia: Tirant lo Blanch; 2020.
- Pérez Candás JI, Grupo de Pediatría Social y Comunitaria AEPap. Programa de identificación del riesgo psicosocial en la infancia y la adolescencia (II). Form Act Pediatr Aten Prim. 2022;15:153-60.
- Gancedo Baranda A (ed.). Manual para la atención a situaciones de Maltrato Infantil. Madrid: Editorial Grupo 2 Comunicación Médica; 2021 [online] [accessed 09/08/2023]. Available at https://seup.org/pdf_public/gt/Maltrato_infantil.pdf
- UNICEF. Diagnóstico de la situación de la infancia en España antes de la aplicación de la Garantía Infantil Europea, Oficina Regional de UNICEF para Europa y Asia Central, Ginebra, 2021. [accessed 09/08/2023]. Available at www.unicef.org/eca/sites/unicef.org.eca/files/2021-11/Spanish Deep Dive Literature review ES.pdf
- Llano JC. El estado de la pobreza. 12º Informe AROPE. Seguimiento de los indicadores de la Agenda UE 2030 (2015-2022). Madrid, Red Europea de Lucha contra la Pobreza y la Exclusión Social, 2022, 257 [online] [accessed 09/08/2023]. Available at www.eapn.es/estadodepobreza/
- Singh G, Zhu H, Cheung CR. Public health for paediatricians: Fifteen-minute consultation on addressing child poverty in clinical practice Arch Dis Child Educ Pract Ed 2021;106:326-32. https://doi.org/10.1136/archdischild-2020-319636
- Hart JT. The inverse care law. Lancet. 1971; 27:405-12. https://doi.org/10.1016/S0140-6736(71)92410-X
- Páez González R, Martínez González C. Frikípatas. Rev Pediatr Aten Primaria. 2023;25:e47-e48.
- Beck AF, Klein MD. Moving From Social Risk Assessment and Identification to Intervention and Treatment. Acad Pediatr. 2016;16(2):97-8. https://doi.org/10.1016/j.acap.2016.01.001
- Pérez Candás, JI. Programa de identificación del riesgo psicosocial en la infancia y la adolescencia (I). Form Act Pediatr Aten Prim. 2022;15(3):111-8.
- Salamanca García l. El maltrato institucional a los-as niños-as. Una aproximación desde la praxis socioeducativa con niños-as en desventaja. Revista de Educación Social 2018;27:176-202.