Vol. 25 - Num. 99
Original Papers
Assessment of physical activity domains and physical fitness components in 4-5 year old children in a health centre
Gaizka Legarra Gorgoñona, Yesenia García Alonsoa, Robinson Ramírez Véleza, Blanca Erice Echegarayb, Paula Moreno Gonzálezb, Mikel Izquierdoa, Alicia M.ª Alonso Martíneza
aGrupo de Investigacion E-FIT. Navarrabiomed. Hospital Universitario de Navarra. Universidad Pública de Navarra. Instituto de Investigación Sanitaria de Navarra (IdiSNA). Pamplona. Navarra. España.
bServicio de Pediatría. Hospital Universitario de Navarra. Navarrabiomed. Instituto de Investigación Sanitaria de Navarra (IdiSNA). Pamplona. Navarra. España.
Correspondence: AM Alonso. E-mail: aliciamaria.alonso@unavarra.es
Reference of this article: Legarra Gorgoñon G, García Alonso Y, Ramírez Vélez R, Erice Echegaray B, Moreno González P, Izquierdo M, et al. Assessment of physical activity domains and physical fitness components in 4-5 year old children in a health centre . Rev Pediatr Aten Primaria. 2023;25:261-8. https://doi.org/10.60147/3c63021d
Published in Internet: 05-07-2023 - Visits: 10582
Abstract
Introduction: lack of physical activity and sedentary lifestyles in children are associated with increased adiposity, low cardiovascular fitness, and risk of cardiovascular disease. On the other hand, adherence to physical activity recommendations is associated with improvements in mental health, decreased anxiety and depression, and healthier habits.
Objectives: to assess the relationship between different domains of physical activity and sedentary behaviour, measured objectively, and components of physical fitness in Spanish children aged 4 and 5 years.
Population and methods: cross-sectional study within the project “Observatory and intervention programme on physical exercise and lifestyles in families for children aged 4 to 5 years in primary care” (https://observatorioactividadfisica.es). Physical fitness was assessed with the PREFIT battery. To measure the amount and intensity of physical activity, participants wore a GENEActiv triaxial accelerometer on the non-dominant hand for 7 consecutive days, 24 hours a day.
Results: the study sample included 70 children (38 boys and 32 girls) with a mean age of 4.83 years (95% confidence interval [CI]). There were no significant differences in physical fitness between boys and girls, but we found differences in physical activity. Boys were physically active for longer durations and with higher intensity than girls. We also found a significant and strong association between the components of physical fitness and physical activity domains in children aged 4 and 5 years.
Conclusions: these findings highlight the importance of promoting active lifestyles from an early age and the need for structured training programs to reduce sedentary behaviour and improve physical fitness in this population.
Keywords
● Physical activity ● Physical fitness ● Preschoolers ● Sedentary lifestyleINTRODUCTION
Physical inactivity and sedentary behaviour are a global public health problem and the fourth most important risk factor for mortality worldwide. For children aged 3 or 4 years, World Health Organization (WHO) recommends a minimum of 180 minutes of moderate to vigorous physical activity a day and avoiding long periods of sitting.1-3 Sleep is also an important part of child health and it is recommended that young children in this age range sleep for 10 to 13 hours a day with adequate sleep quality.4 Lack of physical activity (PA) and sedentary lifestyles in children are associated with increased adiposity, decreased cardiorespiratory fitness and an increased risk of cardiovascular disease.5 On the other hand, adherence to PA recommendations is associated with improved mental health, decreased anxiety and depression and healthier habits.
In respect of fitness, low muscle mass and strength have been found to be associated with adverse health outcomes6 and early mortality.7 Furthermore, recent meta-analyses have found that a low level of fitness in childhood is associated with an increased risk of obesity and cardiometabolic disease in adulthood.8 Similarly, there is evidence that moderate levels of PA can be beneficial for health in young individuals at risk.9
As children grow, their level of PA decreases while sedentary behaviour increases (Ortiz-Sánchez et al.10). Physical inactivity and sedentary habits in school-aged children are associated with an increase in body fat, so that at least 1 in 3 children in Spain has excess weight,11 and also with decreased cardiorespiratory fitness, a risk of hypertension and high cholesterol levels.12 In opposition, adherence to PA recommendations is associated with improved mental health,13 lower levels of anxiety and depression14 and healthier lifestyles.15
Thus, it is important to monitor and record the amount of PA and its intensity, sedentary behaviour and sleep patterns in children, assessing them with objective measures. Recent studies have demonstrated that the greater the level of PA, the stronger its positive effects on health. For instance, Chunyi Fang et al. found an association between the daily step count and fitness in early childhood.16 Similarly, Migueles et al. reported that in children aged 4 years, vigorous physical activity (VPA) was positively correlated to changes in body composition and fitness.17 In light of the above, we conducted a study to analyse the association between the PA and sedentary behaviour (SB) domains, assessed objectively, and the components of PA in Spanish children aged 4 and 5 years.
MATERIAL AND METHODS
Study design and participants
We conducted a cross-sectional study in the framework of the project “Observatory and intervention programme on physical exercise and lifestyles in families for children aged 4 to 5 years in primary care” (https://observatorioactividadfisica.es). The sample consisted of 70 children (38 boys and 32 girls) with a mean age (95% confidence interval [CI]) of 4.83 years. We informed families about the objective of the study and obtained their informed consent to participation. Participants were recruited among the children aged 4 to 5 years in the catchment area of the Iturrama primary care centre. We excluded children with recent injuries or surgeries or in whom performance of the physical fitness tests were contraindicated. The study protocol adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Department of Health of Navarre (PI_2021/111). Half of the funding came from the Department of Health of the Government of Navarre and the other half from the European Regional Development Fund (ERDF).
Measurements and procedures
Anthropometric measurements: the height (cm), weight (kg) and BMI were measured according to the National Health and Nutrition Examination Survey (NHANES) procedures of the Centers for Disease Control and Prevention (CDC) by trained evaluators.18 The height was measured with a SECA 213 stadiometer accurate to 1 mm positioning the patient in the Frankfort plane, the weight with a Tanita DC-430MAS total body composition analyser accurate to 100 g with the patient in light clothing and barefoot. We calculated the BMI in kg/m2 using the measured weight and height, as established by the Sociedad Española para el estudio de la Obesidad (Spanish Society for the Study of Obesity, SEEDO). The waist circumference (cm) was measured with a SECA 201 girth measuring tape accurate to 1 mm.19
Accelerometry: to measure the amount and intensity of PA, we used GENEActiv triaxial accelerometer, which patients wore on the nondominant hand for 7 consecutive days (5 weekdays, 2 weekend days), 24 hours a day, with a logging frequency of 87.5 Hz. To determine the time spent in sedentary behaviour (SB), the levels of light physical activity (LPA), moderate physical activity (MPA), vigorous physical activity (VPA) and total physical activity (TPA), children were required to use the accelerometer for an average of 600 minutes while awake and 200 minutes during nighttime sleep each of the 7 days of the measurement period. We applied cut-off points established specifically for children aged 4 to 6 years: 56.3 milligravitational units (mg) for SB; 1856.3 mg for LPA; 191.6 mg for MPA; 695.8 mg for VPA. To extract the data, we used the software GENEActivPC (version 3.3). The processing and analysis of the data was performed with R-package GGIR. Sleep was detected by means of the algorithm published by Hees et al.20
Fitness: physical fitness was assessed with the PREFIT battery. It consists of 4 tests: handgrip strength (HGS), standing long jump (SLJ) with feet together, 4 x 10 m shuttle run (4 x 10 m) to assess speed and agility and PREFIT 20 m shuttle run. The tests were organised in a circuit in which the same researchers evaluated the same tests every time. Children performed the tests alone, except for the 20 m shuttle run, in which patients were organised in small groups of 6 to perform it. To assess upper body muscular strength (isometric grip strength), we used the adjustable Takei 5001® analogue dynamometer. The handgrip test was performed twice per hand, alternating hands, and recorded in kilograms (kg) of force, with measurements accurate to 100 g. Lower body muscular strength was assessed with the SLJ. Patients performed this test three times and we recorded the best result (cm). To assess speed and agility, we used the 4 x 10 m run, performed twice, allowing full recovery in between and recording the best result (lower time in seconds). To assess cardiorespiratory fitness, we used the adapted 20 m shuttle run. Patients performed this test once, and we recorded the number of completed shuttles. We calculated the overall fitness score (as a z-score) using the results of the HGS, SLJ, 4 x 10 m shuttle run (multiplying the result by −1) and the adapted 20 m shuttle run.
Statistical analysis
We have expressed continuous variables as mean ± standard deviation. We assessed normality by means of the Kolmogorov-Smirnov test and found significant differences between sexes in the objective measurement of PA. We performed a linear regression analysis to assess the associations between fitness (independent variables: HGS, SLJ, 4 x 10 m test, 20 m shuttle run and fitness z-score) and PA domains (independent variables: LPA, MPA, VPA, MVPA, TPA and SB). We performed an analysis of covariance adjusted for sex, age and BMI to test this association. All the analysis were performed with the statistical package for the social sciences (IBM SPSS Statistics 26 for Windows; SPSS Inc., Chicago, USA) and we established the level of significance at α = 0.05.
RESULTS
Table 1 presents the characteristics of the participants (anthropometric measurements, components of fitness and PA domains) by sex. The final sample included 70 children with a mean age of 4.83 years (±0,49). The table shows the characteristics of the patients by sex. We did not find significant differences in the anthropometric measurements or fitness components. However, we did find significant differences in the amount of MPA, VPA and MVPA between boys and girls (MPA p = 0.002; VPA p = 0.001; MVPA p = 0.001).
| Table 1. Characteristics of the sample | ||||
|---|---|---|---|---|
| Girls (n = 32) | Boys (n = 38) | Full sample (n = 70) | p-value | |
| Anthropometric parameters | ||||
| Age | 4.77 (±0.49) | 4.87 (±0.49) | 4.83 (±0.49) | 0.407 |
| Height (cm) | 106.7 (±4.95) | 108.9 (±4.92) | 107.9 (±5.02) | 0.070 |
| Weight (kg) | 18.59 (±2.97) | 19.80 (±3.83) | 19.25 (±3.49) | 0.150 |
| Body mass index (kg/m2) | 16.25 (±1.53) | 16.62 (±2.36) | 16.45 (±2.02) | 0.448 |
| Waist circumference (cm) | 53.5 (±3.16) | 54.9 (±6.18) | 54.3 (±5.04) | 0.240 |
| Components of physical fitness | ||||
| Handgrip strength (kg) | 7.92 (±1.82) | 8.48 (±2.05) | 8.22 (±1.96) | 0.240 |
| Standing long jump (cm) | 87.81 (±17.23) | 86.46 (±26.20) | 87.01 (±22.28) | 0.808 |
| 4 x 10 m speed/agility test (s) | 15.18 (±1.20) | 15.35 (±1.79) | 15.27 (±1.54) | 0.677 |
| PREFIT 20 m shuttle run test (shuttles) | 28.79 (±10.67) | 30.53 (±11.92) | 29.73 (±11.31) | 0.548 |
| General fitness (z-score) | 0.09 (±2.67) | 0.13 (±2.75) | 0.11 (±2.69) | 0.959 |
| Accelerometry | ||||
| LPA (min/day) | 295.64 (±38.31) | 289.64 (±26.32) | 292.35 (±31.92) | 0.465 |
| MPA (min/day) | 79.97 (±19.27) | 99.06 (±26.91) | 90.80 (±25.58) | 0.002 |
| VPA (min/day) | 12.40 (±4.79) | 18.82 (±8.87) | 16.04 (±8.01) | 0.001 |
| MVPA (min/day) | 92.37 (±22.56) | 117.89 (±35.05) | 106.84 (±32.66) | 0.001 |
| TPA (min/day) | 388.01 (±53.15) | 407.72 (±44.60) | 399.19 (±49.10) | 0.104 |
| Sedentary behaviour (min/day) | 515.94 (±61.60) | 522.49 (±142.70) | 519.66 (±114.17) | 0.818 |
| Adherence to AP recommendations (%) | 26 (86.67%) | 38 (100%) | 64 (94.1%) | 0.020 |
| Sleep (hours/day) | 8.93 (±0.75) | 8.97 (±0.70) | 8.95 (±0.72) | 0.850 |
| Rest | 0.81 (±0.05) | 0.82 (±0.05) | 0.81 (±0.05) | 0.486 |
| Adherence to sleep recommendations (%) | 29 (96.67%) | 36 (94.74%) | 65 (95.59%) | 0.700 |
| Total duration of measurement (days) | 6.76 (±0.68) | 6.99 (±0.0) | 6.89 (±0.46) | 0.044 |

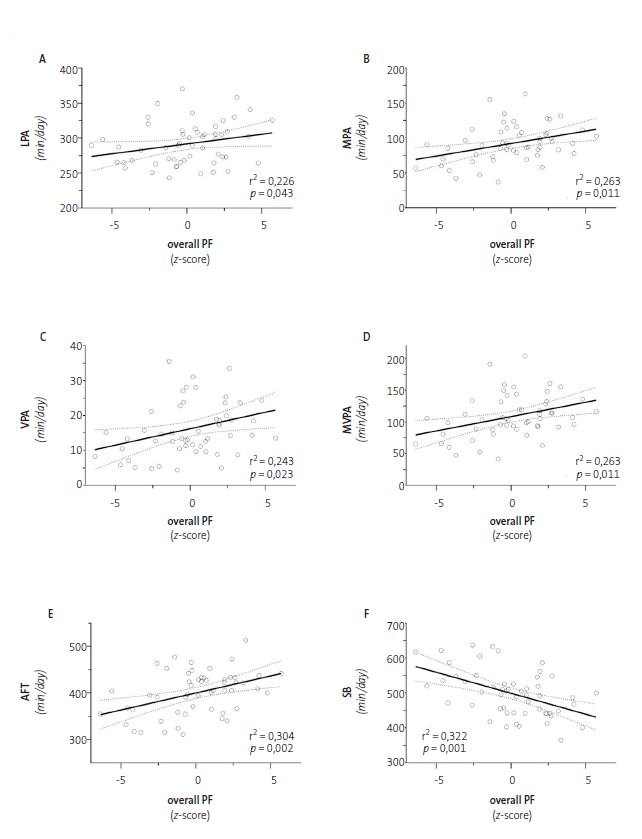
Table 2 presents the results of the analysis of the association between fitness components and PA domains. We found that MPA, VPA and MVPA were significantly associated with HGS (p -values of 0.025, 0.010 and 0.017, respectively), SLJ (0.008, 0.021; and 0.008, respectively) y con 4 x 10 m (0.018, 0.05 and 0.019 respectively). On the other hand, TPA was significantly associated with the results in the SLJ (0.007) and the 4 x 10 m test (0.012). We did not find significant differences between the level of PA measured with the accelerometer and the results of the 20 m shuttle run. Furthermore, we found that the fitness z-score was significantly associated with all PA domains and SB: LPA (p = 0.043), MPA (p = 0.011), VPA (p = 0.023), MVPA (p = 0.011), TPA (p = 0. 002) and SB (p = 0.001), as can be seen in Figure 1.
| Table 2. Association between domains of physical activity and fitness expressed as z-scores | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Handgrip strength | Standing long jump | 4 x 10 m speed agility test | PREFIT 20 m shuttle run test | z-score | ||||||||||||||||
| Unstandardised coefficients | Unstandardised coefficients | Unstandardised coefficients | Unstandardised coefficients | Unstandardised coefficients | ||||||||||||||||
| B | 95% CI | r2 | p | B | 95% CI | r2 | p | B | 95% CI | r2 | p | B | 95% CI | r2 | p | B | 95% CI | r2 | p | |
| LPA | 0.002 | 0.006 | 0.401 | 0.784 | 0.148 | 0.100 | 0.277 | 0.145 | -0.011 | 0.007 | 0.092 | 0.127 | 0.054 | 0.050 | 0.092 | 0.282 | 0.024 | 0.011 | 0.226 | 0.043 |
| MPA | 0.018 | 0.008 | 0.448 | 0.025 | 0.322 | 0.117 | 0.154 | 0.008 | -0.20 | 0.008 | 0.147 | 0.018 | 0.031 | 0.061 | 0.075 | 0.619 | 0.037 | 0.014 | 0.263 | 0.011 |
| VPA | 0.065 | 0.024 | 0.463 | 0.010 | 0.885 | 0.375 | 0.127 | 0.021 | -0.053 | 0.027 | 0.118 | 0.050 | 0.142 | 0.196 | 0.079 | 0.474 | 0.108 | 0.046 | 0.243 | 0.023 |
| MVPA | 0.015 | 0.006 | 0.455 | 0.017 | 0.250 | 0.091 | 0.153 | 0.008 | -0.015 | 0.006 | 0.144 | 0.019 | 0.027 | 0.048 | 0.076 | 0.574 | 0.029 | 0.011 | 0.263 | 0.011 |
| TPA | 0.007 | 0.004 | 0.429 | 0.086 | 0.170 | 0.061 | 0.158 | 0.007 | -0.011 | 0.004 | 0.159 | 0.012 | 0.034 | 0.032 | 0.090 | 0.289 | 0.022 | 0.007 | 0.304 | 0.002 |
| SB | -0.003 | 0.002 | 0.422 | 0.132 | -0.045 | 0.025 | 0.092 | 0.081 | 0.003 | 0.002 | 0.091 | 0.130 | 0.001 | 0.016 | 0.071 | 0.960 | -0.17 | 0.005 | 0.322 | 0.001 |

DISCUSSION
The aim of the study was to analyse the association between PA domains assessed by accelerometry (LPA, MPA, VPA, MVPA, TPA and SB) and fitness components(HGS, SLJ, 4 x 10 m test and 20 m shuttle run) in young children aged 4 and 5 years. The results showed no significant differences in fitness between girls and boys, but did find differences in PA. We found longer duration and intensity of physical activity in boys compared to girls, which was consistent with the previous literature.18 This was reflected in the substantial adherence to PA recommendations, as only 4 out of 32 girls did not meet them (≥180 minutes of TPA and ≥60 min of MVPA).7 Our findings were similar to those reported by Quan et al., whose study found (like ours) that boys spent more time in MVPA and TPA than girls (117,89 min/day versus 92,37 min/day and 407.72 min/day versus 388.01 min/day, respectively).21
We found a statistically significant strong association between fitness components and PA domains in children. This was similar to the results of other studies that have linked VPA to body composition and physical fitness. For example, Jairo H. Migueles et al. found that an increase in VPA at the expense of activities of lower intensity in children aged 4 years was associated with body composition and physical fitness at the cross-sectional and longitudinal levels.17 In addition, Marja H. Leppänen et al., in a 12-month longitudinal study of healthy children aged 4 years in Sweden, found that greater levels of VPA and MVPA are associated with improved cardiorespiratory fitness outcomes, lower body muscular strength and physical fitness.22 Their results were similar to those reported by Fang et al.,23 who found a positive associations between the SLJ and MVPA, and a negative association between the 4 x 10 m test and AFMV.23 However, this study did not find a positive association between the 20 m shuttle run and MVPA, which may have been due to the sample size.
The main strengths of our study were the young age of the participants (mean age, 4.83 years) and the use of wrist accelerometers. These devices allowed the collection of objective measurements of PA that could not be obtained through questionnaires. However, we also ought to highlight some of the study limitations, such as its small sample size and the fact that all participants were recruited from the same primary care centre, which calls for caution in interpreting the results.
Our findings underscore the importance of promoting active lifestyles from an early age and the need for structured training programmes to reduce sedentary behaviour and improve physical fitness in this population. In the future, we will seek to increase the sample size and develop structured training programmes to reduce sedentary behaviour and increase PA (light, moderate, vigorous, moderate-vigorous). This would allow establishing whether increasing PA has an impact on fitness.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article. The study was partially funded by the Department of Health of the Government of Navarre, co-funded by the European Regional Development Fund (ERDF), 2014-2020 fund (Navarre).
AUTHORSHIP
Author contribution: study conception and design, data collection and manuscript writing (GLG, YGA, RMV, BEE, MI, AMAM), quantitative methods and patient recruitment, manuscript revision (GLG, YGA, BEE, PMG, AMAM).
ABBREVIATIONS
BMI: body mass index · HGS: handgrip strength · LPA: light physical activity · MPA: moderate physical activity · MVPA: moderate or vigorous physical activity · PA: physical activity · SLJ: standing long jump · TPA: total physical activity · VPA: vigorous physical activity · WHO: World Health Organization
REFERENCES
- Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451-62.
- Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. In: WHO [online] [accessed 29/06/2023]. Available at https://apps.who.int/iris/handle/10665/311664
- Alòs Colomer F, Puig-Ribera A. Inactividad física y sedentarismo. AMF. 2022;18(2):66-75.
- Mindell JA, Williamson AA. Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Med Rev. 2018;40:93-108.
- Olavarrieta Bernardino S, Fernandez Mendoza J. Sueño y estrés: relación con la obesidad y el síndrome metabólico. Rev Esp Obesidad. 2007;5(2):77-90.
- Orsso CE, Tibaes JRB, Oliveira CLP, Rubin DA, Field CJ, Heymsfield SB, et al. Low muscle mass and strength in pediatrics patients: Why should we care? Clin Nut. 2019;38(5):2002-15.
- McGrath R, Johnson N, Klawitter l, Mahoney S, Trautman K, Carlson C, et al. What are the association patterns between handgrip strength and adverse health conditions? A topical review. SAGE Open Med. 2020;8:205031212091035.
- Garciá Hermoso A, Ramírez Vélez R, Garciá Alonso Y, Alonso Martínez AM, Izquierdo M. Association of Cardiorespiratory Fitness Levels During Youth With Health Risk Later in Life: A Systematic Review and Meta-analysis. JAMA Pediatr. 2020;174(10):952-60.
- Janssen I, LeBlanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40.
- Antonio Ortiz Sánchez J, Del Pozo Cruz J, María Alfonso Rosa R, Gallardo Gómez D, Álvarez Barbosa F. Efectos del sedentarismo en niños en edad escolar: revisión sistemática de estudios longitudinales (Effects of sedentary school-age children: a systematic review of longitudinal studies). Retos. 2021;40:404-2.
- Casas R, Santiago E, Santos FG. Estudio sobre la situación de la obesidad infantil en España. DKV Instituto vida saludable. 2017. In: Observatorio de la Infancia y Adolescencia de Andalucía [online] [accessed 29/06/2023]. Available at www.observatoriodelainfancia.es/oia/esp/documentos_ficha.aspx?id=5810
- Yuksel HS, Şahin FN, Maksimovic N, Drid P, Bianco A. School-based intervention programs for preventing obesity and promoting physical activity and fitness: A systematic review. Int J Environ Res Public Health. 2020;17(1):347.
- Ortega JP, Martínez Santos R. Physical activity during leisure time and its relation with some mental health indicators in Spain. Salud Mental. 2011;34(1):45-52.
- Brosnahan J, Steffen LM, Lytle l, Patterson J, Boostrom A. The Relation Between Physical Activity and Mental Health Among Hispanic and Non-Hispanic White Adolescents. Arch Pediatr Adolesc Med. 2004;158(8):818-23.
- Hobza V, Maracek M, Hamrik Z. Organized Sport Activities of 11 to 15-Year-Old Adolescents: Trends from 2010-2018 and Socioeconomic Context. Int J Environ Res Public Health. 2022;19(10):6074.
- Fang C, Zhang J, Zhou T, Li l, Lu Y, Gao Z, et al. Associations between daily step counts and physical fitness in preschool children. J Clin Med. 2020;9(1):163.
- Migueles JH, Delisle Nyström C, Leppänen MH, Henriksson P, Löf M. Revisiting the cross-sectional and prospective association of physical activity with body composition and physical fitness in preschoolers: A compositional data approach. Pediatr Obes. 2022;17(8):e12909.
- Anthropometry Procedures Manual. National Health and Nutrition Examination Survey. 2007 [online] [accessed 29/06/2023]. Available at www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf
- SEEDO’2000 consensus for the evaluation of overweight and obesity and the assessment of obesity management. Med Clin. 2000;115(15):587-97.
- Van Hees VT, Sabia S, Anderson KN, Denton SJ, Oliver J, Catt M, et al. A novel, open access method to assess sleep duration using a wrist-worn accelerometer. PLoS One. 2015;10(11):e0142533.
- Quan M, Zhang H, Zhang J, Zhou T, Zhang J, Zhao G, et al. Are preschool children active enough in Shanghai: An accelerometer-based cross-sectional study. BMJ Open. 2019;9(4):e024090.
- Leppänen MH, Henriksson P, Delisle Nyström C, Henriksson H, Ortega FB, Pomeroy J, et al. Longitudinal physical activity, body composition, and physical fitness in preschoolers. Med Sci Sports Exerc. 2017;49(10):2078-85.
- Fang H, Quan M, Zhou T, Sun S, Zhang J, Zhang H, et al. Relationship between Physical Activity and Physical Fitness in Preschool Children: A Cross-Sectional Study. Biomed Res Int. 2017;2017:9314026.