Vol. 25 - Num. 97
Original Papers
Variations and different perceptions in vitamin d supplementation in the pediatric age in Spain
Diego de Sotto-Estebana, Guiomar Pérez de Nanclares Lealb, M.ª José Alcázar Villarc, Silvia Marín del Barriod, Lorena Miñones Suáreze, Eduard Mogas Viñalsf, Isolina Riaño Galáng, Luis Antonio Castaño Gonzálezh, José M.ª Martos Telloi, Grupo Metabolismo Fosfocálcico de la Sociedad Española de Endocrinología Pediátrica (SEEP)
aServicio de Pediatría. Clínica Rotger. Palma. Islas Baleares. España.
bLaboratorio de Genética Molecular. Hospital Universitario Araba-Txagorritxu. Vitoria. Álava. España.
cServicio de Pediatría. Hospital Universitario de Fuenlabrada. Fuenlabrada. Madrid. España.
dEndocrinología Pediátrica. Servicio de Pediatría. Hospital Sant Joan de Déu. Barcelona. España.
eEndocrinología Pediátrica. Servicio de Pediatría. Hospital Reina Sofia. Tudela. Navarra. España.
fEndocrinología Pediátrica. Servicio de Pediatría. Hospital Universitario Vall d´Hebron. Barcelona. España.
gServicio de Pediatría. Hospital Universitario Central de Asturias. Oviedo. Asturias. España.
hInstituto BioCruces. Endocrinología Pediátrica. Servicio de Pediatría. Hospital Universitario Cruces. Barakaldo. Vizcaya. España.
i Endocrinología Pediátrica. Servicio de Pediatría. Hospital Universitario Virgen de La Arrixaca. Murcia. España.
Correspondence: D de Sotto-Esteban. E-mail: sottomartin@gmail.com
Reference of this article: de Sotto-Esteban D, Pérez de Nanclares Leal G, Alcázar Villar MJ, Marín del Barrio S, Miñones Suárez L, Mogas Viñals E, et al. Variations and different perceptions in vitamin d supplementation in the pediatric age in Spain . Rev Pediatr Aten Primaria. 2023;25:e1-e13.
Published in Internet: 21-03-2023 - Visits: 15000
Abstract
Introduction: rickets is a global health problem. Vitamin d deficiency has become a pandemic, its interest has increased due to its implication in multiple extraskeletal actions.
Material and methods: a survey was conducted by e-mail among Spanish paediatricians to study their attitude regarding prophylactic vitamin D supplementation.
Results: 83% of pediatricians have vitamin D prophylaxis policies in their area. 61.6% start prophylaxis in the first two weeks, 81.5% maintain it the first year. 57.2% search for vitamin D deficiency, especially if they work in a hospital.
Conclusions: vitamin D prophylaxis policies are uniform. More than a half of Spanish pediatricians conduct a systematic search for vitamin D deficiency in their patients with risk factors during childhood and adolescence.
Keywords
● Rickets prophylaxis ● Spanish pediatricians ● Survey ● Vitamin D deficiencyINTRODUCTION
Vitamin D plays a key role in calcium-phosphorus metabolism and bone mass accrual.1 The main source of vitamin D is its synthesis in the skin through sunlight exposure. The definition of vitamin D deficiency is based on the measurement of the plasma levels of 25-hydroxyvitamin D (calcifediol). The active metabolite, calcitriol (1-25(OH)D3), has a very short half-life, so its plasma levels are very low and change late in the development of deficiency, which poses a barrier to its use as an indicator of vitamin D levels.1-5
In recent years, a growing body of evidence supports the importance of vitamin D in extraskeletal functions. Vitamin/hormone D is involved in the direct or indirect regulation of approximately 2000 genes and in the pathogenesis of infectious diseases, allergies, autoimmune diseases, cardiovascular disease, mental disorders, diabetes and tumours1,3; observational studies have also found an association between higher vitamin D concentrations and an improved course in several chronic diseases.1 The prevalence of vitamin D deficiency is increasing in populations of all ethnicities and geographical regions, and some authors have referred to it as an important global health problem.3,4
Rickets continues to be a health problem in developing countries2 and is experiencing a resurgence in Spain in relation to immigration.6,7
When it comes to the cut-off levels used to define vitamin D deficiency,1-7 there is sufficient evidence to support threshold levels in adults, some evidence to support its diagnosis in adolescents and much scarcer data for children.8,9 Thus, when it comes to the paediatric population, there is no evidence to support the establishment of calcium absorption thresholds in relation to vitamin D levels i10; there are even few studies on the subject of bone health.11,12
In recent years, different scientific and professional societies have issued recommendations concerning the circumstances under which it is indicated to measure vitamin D levels and the thresholds to be applied to define deficiency, more recently addressing aspects related to its extraskeletal actions. In the consensus document for the Italian population, Saggese et al. made a thorough review of the literature,5 and reported that the most frequently published threshold used to define vitamin D deficiency was 20 ng/ml (50 mmol/L), including some articles that defined an intermediate status of insufficiency as a range between 20 and 30 ng/ml; the Global Consensus on nutritional rickets proposed a lower threshold.2 The Spanish Association of Pediatrics (AEP) has proposed a threshold of 20 ng/ml.13
Spain is also consistent with the global trend by which a large percentage of the population has vitamin D deficiency; it has also been described in the paediatric population in several regions, although not uniformly, in newborns, infants, children and adolescents, even in areas of the Mediterranean coast and the south with sufficient UV radiation.14-20
There is an adequate consensus regarding the indications of treatment for rickets, although there may be differences in the recommended treatment2; however, there is no consensus on the indications for prophylaxis and treatment in asymptomatic individuals with low vitamin D levels.
Given the greater growth rate in the first year of life, recommendations also tend to focus on the prevention of rickets in this stage, and, in addition to general recommendations about lifestyle, the main international organizations started to recommend vitamin D prophylaxis (Institute of Medicine,21 Endocrine Society3, Global Consensus2, American Academy of Pediatrics22); with small variations, the most frequent recommendation is oral vitamin D supplementation at a dose of 400 IU/day for all infants, independently of the feeding modality, in the first year of life.
Since maternal vitamin D deficiency always has an impact on the newborn2 and the half-life of 25 OH vitamin D is of only 2 weeks, prophylaxis should also include pregnant women and be initiated in the newborn at birth.
In Spain, the AEP has also issued similar recommendations,13 specifically, supplementation with 400 IU of vitamin D a day in infants up to age 1 year. The working group on prevention in childhood and adolescence (PrevInfad) of the Spanish Association of Primary Care Paediatrics (AEPap)23 has also made recommendations on the subject, although they are not universal and have not been updated in recent years.
Few studies have focused on the level of knowledge of health care professionals regarding health care interventions, the associated adherence and the factors that may affect their implementation. A recent survey conducted in Spain on the use and knowledge of pseudosciences in paediatric providers evinced that a considerable number of Spanish paediatricians recommended to parents the use of treatments not supported by evidence in their children.24
This situation motivated us to carry out an online survey of paediatricians nationwide to analyse aspects related to vitamin D. The primary objective was to assess the degree of adherence to the guidelines for vitamin D prophylaxis in Spain. The secondary objectives included analysing the awareness and particularities of the implementation of this intervention among paediatric providers and assessing the association between the characteristics of health care professionals and the adherence to different aspects of the current recommendations.
MATERIAL AND METHODS
We conducted a descriptive study through a nationwide online survey by means of the Google Docs platform of the practices and perceptions regarding vitamin D supplementation in the paediatric age group. We distributed the questionnaire through the mailing list of the AEP between 13/10/21 and 30/11/21, sending an initial email followed by a reminder. Inclusion required answering every item of the questionnaire with the exception of one which was optional.
Participation in the survey was anonymous and voluntary, guaranteeing the protection of the data, and the questionnaire was distributed to the paediatricians included in the mailing list of the AEP, requesting that they forward it to family physicians and general practitioners working with the paediatric population, as they are not included in this mailing list. We calculated that given the total number of members of the AEP, which we estimated at 12 219, we would need 983 to respond to obtain results representative of the population with a precision of 3%, a level of confidence of 95% and using the most conservative estimate for the expected proportion (p = 1−p).
The questionnaire (Figure 1) was structured in 3 sections following an initial item requesting consent:
- Characteristics of the participants (8 items: sex, age, professional profile, years of professional experience, clinical practice setting, employment in public/private/mixed care system, paediatric subspeciality or specific area, autonomous region/city of residence).
- Knowledge and attitudes regarding vitamin D prophylaxis in newborns and infants (11 items: existence or absence of healthcare policy regarding vitamin D prophylaxis and knowledge of it, perceived degree of adherence, timing of initiation, duration and monitoring of prophylaxis, target population, dosage form).
- Knowledge and attitudes on vitamin D deficiency diagnosis, prophylaxis and treatment in children and adolescents (6 items: diagnosis of rickets cases, routine assessment of vitamin D deficiency and in which cases, vitamin D dose used for prophylaxis in children and adolescents).
| Figure 1. Survey on the differences in vitamin D supplementation in the paediatric population in Spain and associated perceptions |
|---|
|
Dear colleague: We request your collaboration with the study “Variaciones y diferentes percepciones en la suplementación con vitamin D en la edad pediátrica en España”, which would consist in the completion of a brief questionnaire that would take no longer than 10-15 minutes of your time. The aim of the study is to establish the patterns of prescribing of vitamin D prophylaxis among paediatric providers in Spain and the potential determinants of this practice. Participation in the survey is voluntary. The responses are anonymous and the study will adhere to legislation on data protection at all times, and participation involves consent to the entry of the responses to a database for subsequent analysis and publication, with the access and use of the data for researchers restricted exclusively to the aforementioned purposes. This survey is part of a homonymous research project, which has been approved by the Research Ethics Committee of the Balearic Islands, in adherence with current legislation and the principles and regulations applicable to this type of study. If you have already received an invitation to participate in this study from a different source, we apologize and request that you do not submit an additional response. Should you deem it pertinent, we would be thankful if you helped us distribute this questionnaire by forwarding this email to other practitioners in the field of paediatrics. Thank you very much for your cooperation. |
|
Consent to participation: Yes/No |
|
Section 1. Demographic and professional characteristics:
|
|
Section 2. Vitamin D prophylaxis in the first year of life:
|
|
Section 3. Diagnosis and treatment of vitamin D deficiency in children and adolescents:
|

The degree of adherence to vitamin D prophylaxis in infants in the catchment area of each provider was categorised based on the provider’s estimations as follows: good adherence, ≥80% of cases; moderate adherence, 50-80% of cases and poor adherence, < 50%.
We conducted a descriptive univariate analysis of the categorical data (absolute frequency and percentage distributions) and a bivariate analysis by means of the chi-square test. We considered p values of less than 0,05 statistically significant. The statistical analysis was performed with the software SPSS version 23.
RESULTS
We received a total of 1298 responses (1 refusal to participate), amounting to 11% of the mailing list and 20.9% of the opened emails. Table 1 presents the questionnaire results regarding the characteristics of the professionals. Eighty percent were female (1039), the age group distribution was uniform save for the group aged less than 30 years, which was the least represented (4.9%). The distribution by years of experience was also relatively uniform. Paediatricians accounted for 99.2% of respondents, most were employed in the public health care system (79.5%), and more than half worked in primary care or outpatient clinic settings (59.6%); the autonomous communities with the highest representation were Madrid, Valencia, Catalonia and Andalusia.
| Table 1. Personal and professional characteristics of respondents based on survey results (n = 1298 responses), expressed as absolute frequencies and percentages | |
|---|---|
|
Sex:
|
|
|
Age range:
|
|
|
Professional experience:
|
|
|
Speciality:
|
|
|
Health care system:
|
|
|
Care setting:
|
|
|
Autonomous community/city in Spain: |
|
|
|
|
Paediatric subspeciality or field: |
|
|
|

As regards knowledge and perceptions regarding vitamin D prophylaxis in the first year of life (Table 2), most respondents reported that there was an established health care policy in their catchment area (83%) and 76.3% knew it in detail. Female respondents were aware of it more frequently than male respondents (77.96% vs. 69.5%, p <0.01). Also, 77.9% of respondents considered that adherence to prophylaxis in their catchment area was good.
| Table 2. Knowledge and opinions about vitamin D prophylaxis in the first year of life |
|---|
|
Existence of protocols for prevention of rickets through vitamin D prophylaxis:
|
|
Knowledge of health care policy regarding prophylaxis:
|
|
Degree of adherence to prophylaxis estimated by respondents:
|
|
Time of initiation of vitamin D prophylaxis in infants:
|
|
Duration of vitamin D prophylaxis:
|
|
Recommended vitamin D dose:
|
|
Assessment of adherence:
|
|
Target population for vitamin D prophylaxis:
|
|
Adherence to maternal vitamin D supplementation:
|
|
Type of preparation:
|
|
Knows price of recommended preparation:
|

Prophylaxis was initiated in the first 2 weeks post birth by 61.6% of respondents, and in the maternity ward by only 1.8%. Most respondents (86.5%) recommended prophylaxis for a full year after birth (in Asturias, 63.4% recommended it until 18 months post birth) and in all infants (91.5%), independently of the feeding modality (breastfeeding, formula, mixed) with a supplement containing only vitamin D in nearly all cases (97.7%) and knew its exact or approximate price (74.2%). Confirmation of adherence to prophylaxis was the norm (35.1% asked always and 41.7% nearly always).
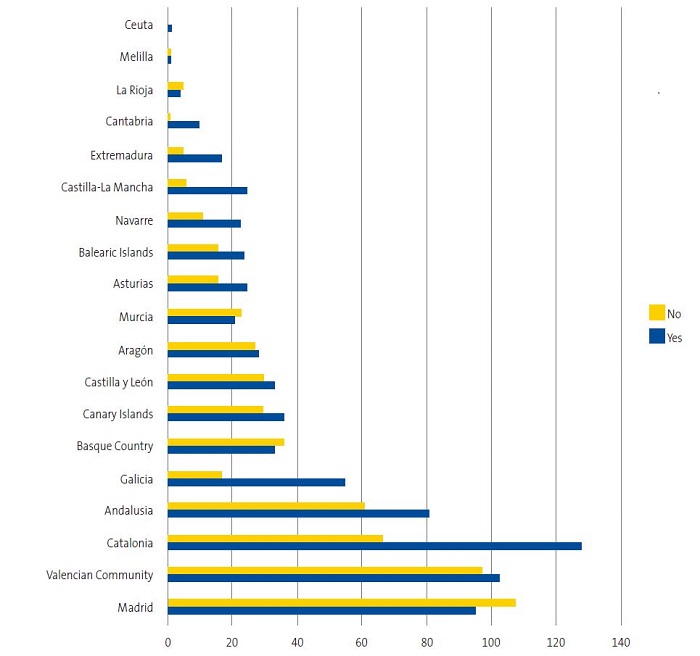
In relation to the approach in children and adolescents (Table 3), we ought to highlight that rickets is infrequent in Spain (83.7% of respondents had no cases of rickets in their caseloads). We found that 57.2% of respondents routinely ordered blood tests to screen for vitamin D deficiency in specific groups of patients. These patients mainly consisted of those with special diets, reduced sunlight exposure or with specific diseases, such as chronic kidney failure, short stature or malabsorption syndromes (Table 4). The proportion of clinicians who ordered blood tests for detection of vitamin D deficiency was greater in the hospital setting compared to the primary care setting (67.6% vs. 50.2%, p <0.01), in the group with 10-20 years of professional experience (67.2%, compared to approximately half in the rest of groups) and in the group aged 30 to 40 years, and varied widely between autonomous communities in Spain (Figure 2), although the response rate in some regions was substantially lower. As concerns the different paediatric subspecialities, rheumatologists, nephrologists, endocrinologists, gastroenterologists, haematologists/oncologists and neurologists were the specialists that ordered these tests most frequently (Table 5).
| Table 3. Knowledge and opinions about vitamin D prophylaxis in children and adolescents |
|---|
|
In the past year, how many of the patients you have managed directly had received a diagnosis of rickets secondary to deficiency?
|
|
Do you order blood tests to screen for vitamin D deficiency in your patients?
|
|
What vitamin D dose do you recommend for prophylaxis in adolescents?
|

| Table 4. Reasons reported by Spanish paediatric providers for ordering measurement of vitamin D serum levels (respondents could choose more than one answer) |
|---|
|

| Figure 2. Ordering of blood test for assessment of vitamin D deficiency by autonomous community or city in Spain |
|---|
 |

| Table 5. Frequency of testing for vitamin D deficiency by paediatric subspeciality | ||||
|---|---|---|---|---|
| Paediatric subspeciality | Yes | No | Total | % |
| Primary care | 329 | 323 | 652 | 50.4 |
| Neonatology | 58 | 54 | 112 | 57.8 |
| Gastroenterology, hepatology and nutrition | 73 | 14 | 87 | 83.9 |
| Endocrinology | 59 | 18 | 77 | 7.6 |
| Paediatric general inpatient care | 41 | 21 | 62 | 66.1 |
| Emergency care | 19 | 32 | 51 | 37.3 |
| Nephrology | 35 | 9 | 44 | 79.5 |
| Paediatric palliative care | 10 | 13 | 23 | 43.5 |
| Cardiology | 11 | 12 | 23 | 47.8 |
| Infectious diseases | 15 | 7 | 22 | 68 |
| Neurology | 17 | 5 | 22 | 77.2 |
| Haematology/oncology | 17 | 4 | 21 | 81 |
| Pulmonology | 12 | 9 | 21 | 57.1 |
| Immunology, allergy | 12 | 9 | 21 | 57.1 |
| Rheumatology | 10 | 0 | 10 | 100 |
| Other | 26 | 24 | 50 | 52 |
| Total | 743 | 555 | 1298 | 57.2 |

The majority of respondents recommended a dose of 400 IU of cholecalciferol for vitamin D prophylaxis (87.4%), but did not recommend prophylaxis during adolescence.
DISCUSSION
The profile of the participants was very similar to the profile of the members included in the mailing list of the AEP (12 219 members, 8144 female), with the exception that there was a higher proportion of female respondents (80% in our survey vs. 66.7% in the mailing list) and a low participation by the youngest age group (4.9% of respondents compared to 15.9% of the mailing list). Most of the female respondents were employed in the primary care system, and the most populous autonomous communities in Spain were the most heavily represented.
In practically the entire territory of Spain, the administration of cholecalciferol for prevention of rickets and vitamin D deficiency is an established public health policy, and approximately 3 out of 4 respondents reported knowing the policy in detail.
Given the lack of uniform and reliable records for the purpose of assessing adherence, we decided to assess the degree of adherence based on the perceptions of health care professionals, as was done in a European survey of experts on the subject.25 In our survey, 77.9% of respondents considered adherence good (that is, that more than 80% of parents adhered to the recommendation).
As for the timing of initiation of prophylaxis, 61.6% of providers reported they started it within 2 weeks of birth. In newborns, vitamin D levels are equivalent to maternal levels at the end of pregnancy, and the half-life of 25-hydroxycalciferol is 2 weeks, so, as a general rule, prophylaxis should be started in these first 2 weeks post birth.2,25 Only 1.8% reported initiation of prophylaxis in the maternity ward, which was found to be associated with greater adherence to the recommendation in the European survey. Most respondents recommended vitamin D supplementation for the entire first year of life, as is generally recommended (in Asturias, vitamin D prophylaxis is indicated for the first 18 months of life). In addition, routine prophylaxis was recommended for all infants, independently of feeding modality, which has also been found to be associated with improved adherence.25 Most providers prescribed preparations containing only vitamin D, which was a positive finding, as they are much cheaper.
Adherence is influenced by both patient-related and provider-related factors. In the survey on the factors influencing adherence to vitamin D prophylaxis sponsored by the Bone and Growth Plate Working Group of the European Society for Paediatric Endocrinology (ESPE),25 adherence improved when parents were informed at birth before discharge from the neonatal unit, all babies received supplementation, there was a policy to provide financial support to families to acquire vitamin D supplements and adherence monitoring was incorporated into child health check-up visits.
As regards the approach implemented during childhood and adolescence, we ought to underscore that rickets is an infrequent diagnosis in Spain (83.7% of respondents did not have any patients with rickets). We found that 57.2% of providers ordered blood tests routinely to screen for vitamin D deficiency in specific groups of patients. Chief among these groups were patients with special diets, with low sunlight exposure or with diseases such as chronic kidney failure, short stature or malabsorption syndromes (Table 5).
Most respondents recommended a dose of cholecalciferol of 400 IU for vitamin D prophylaxis during childhood, and did not recommend prophylaxis during adolescence.
Some of the risk factors for vitamin D deficiency are dark/black skin, reduced sunlight exposure, low dietary intake, being born to a mother with risk factors for vitamin D deficiency, breastfeeding, chronic diseases such as chronic kidney failure, liver failure and/or cholestasis or malabsorption syndrome, prolonged use of medication such as antiepileptic drugs, steroids or antifungals and obesity.1,5-9
In agreement with the international literature, studies in Spain have studied vitamin D deficiency in these groups, evincing an association with factors such as breastfeeding,26 obesity,27-31 allergy,32 infectious disease,33,34 atopy,35 blood disorders36 and antiepileptic medication,37 among others.
We ought to keep in mind that while experts recommend vitamin D supplementation in many of these risk groups, the current evidence is insufficient to support routine blood testing for screening of vitamin D deficiency in these patients and, needless to say, there is no evidence supporting routine testing in the healthy population.38,39 It is important to be aware of what is supported by evidence and what aspects require further research, as reflected by the recent review by a French consensus group.40.
As health care professionals, we do not always implement recommendations that we know to be sufficiently supported by evidence and, on the other hand, sometimes implement practices that are not based on evidence.
There are several significant limitations to our study, chief of which are the following: the response rate tends to be small in surveys, and respondents tend to be more motivated and interested in the subject of the survey compared to nonrespondents. We also used a subjective parameter, the perception of providers, to estimate the degree of parental adherence to vitamin D supplementation in their children for prophylaxis. We ought to mention the disparity in the results concerning the number of paediatricians who do not recommend vitamin D prophylaxis in the 2 items that address this aspect (7 versus 48 paediatricians), which could be due to factors related to the design of the questionnaire or with respondent fatigue or lack of concentration.
To conclude, the highlights of our survey are that health policies regarding prophylactic supplementation with vitamin D in the first year of life are fairly homogeneous throughout Spain, that are well known and that adherence to these recommendations is considered good. On the other hand, up to 57.2% of paediatricians in Spain actively screen for vitamin D deficiency by performing blood tests in some of their patients, despite the lack of evidence in support of this practice.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article. Partial, very summarised results of the study were presented as an oral communication at the Congress of the Sociedad Española de Endocrinología Pediátrica held in May 2022 in Oviedo, Spain.
AUTHORSHIP
Author contributions: study protocol design, research and manuscript writing (DSE), development of study protocol and original article for publication (rest of authors).
The study was approved by the Research Ethics Committee of the Balearic Islands (file: CEI IB 4510/21PI). It was conducted in adherence with data protection laws, and the researchers had exclusive access to the data, which were only used for the purposes of the study.
ACKNOWLEDGMENTS
We thank Oana Bulilete for her help with the research design and the statistical analysis.
REFERENCES
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-81.
- Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101:394-415.
- Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M. Drug and therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics. 2008;122:398-417.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-30.
- Saggese G,Vierucci F, Prodam F, Cardinale F, Cetin I, Chiappini E, et al. Vitamin D in pediatric age: consensus of the Italian Pediatric Society ant the Italian Society of Preventive and Social Pediatrics,jointly with the Italian Federation of Pediatricians. Ital J Pediatr. 2018;44:51.
- Yeste D, Carrascosa A, Grupo Interhospitalario para el estudio del Raquitismo Carencial en Cataluña (GIERCC). Raquitismo carencial en la infancia: análisis de 62casos [Nutritional rickets in childhood: analysis of 62 cases]. Med Clin (Barc). 2003;121:23-7.
- Sánchez Muro JM, Yeste Fernández D, Marín Muñoz A, Fernández Cancio M, Audí Parera l, Carrascosa Lezcano A. Niveles plasmáticos de vitamina D en población autóctona y en poblaciones inmigrantes de diferentes etnias menores de 6 años de edad. An Pediatr (Barc). 2015:316-24.
- Atapattu N, Shaw N, Högler W. Relationship between serum 25-hydroxyvitamin D and parathyroid hormone in the search for a biochemical definition of vitamin D deficiency in children. Pediatr Res. 2013;74:552-6.
- Maguire JL, Birken C, Thorpe KE, Sochett EB, Parkin PC. Parathyroid hormone as a funtional indicator of vitamin D sufficiency in children. JAMA Pediatr. 2014;168:383-5.
- Abrams SA, Hicks PD, Hawthorne KM. Higher serum 25-hydroxivitamin D levels in school-age children are inconsistently associated with increased calcium absorption. J Clin Endocrinol Metab. 2009;94:2421-7.
- Golden NH, Abrams SA; Committee on Nutrition. Optimizing bone health in children and adolescents. Pediatrics. 2014;134:e1229-43.
- Fu Y, Hu Y, Quin Z, Zhao Y, Yang Z, Li Y, et al. Association of serum 25-hydroxivitamin D status with bone mineral density in 0-7 year-old children. Oncotarget. 2016;7:80811-9.
- Martínez Suárez V, Moreno Villares JM, Dalmau Serra J, Comité de Nutrición de la Asociación Española de Pediatría. Recomendaciones de ingesta de calcio y vitamina D: posicionamiento del Comité de Nutrición de la Asociación Española de Pediatría. An Pediatr (Barc). 2012;77:57.e1-8.
- De Sotto Esteban D, Ursina B, Ferrés l, Torbado P, Yáñez AM. Niveles de vitamina D y factores de riesgo asociados en recién nacidos sanos de Mallorca. Rev Esp Endocrinol Pediatr. 2015;6:51-60.
- Rodríguez-Rodríguez E, Aparicio A, López-Sobaler AM, Ortega RM.Vitamin D status in a group of Spanish schoolchildren. Minerva Pediatr. 2011;63:11-18.
- Togo A, Espadas Maciá D, Blanes Segura S, Sivó Díaz N, Villalba Martínez C ¿Existe déficit de vitamina D en los niños de una ciudad soleada en el Mediterráneo? An Pediatr (Barc). 2016;84:163-9.
- Fernández Bustillo JM, Fernández Pombo A, Gómez Bahamonde R, Sanmartín López E, Gualillo O. Vitamin D levels in a pediatric population of a primary care centre: a public health problem? Nutr Hosp. 2015;32:1061-6.
- Ruiz Ocaña P, Carrasco Fernández C, Zopeque García N, Sáez Benito A, Novalbos Ruiz JP, Lechuga Sancho AM. Niveles de vitamina D al final de la estación invernal en una población escolar sana. Rev Esp Endocrinol Pediatr. 2014;5:19-27.
- Martínez Redondo I, García Romero R, Calmarza P, De Arriba Muñoz A, Rodríguez,Martínez G, Labarta Aizpún JI. Deficiencia de vitamina D en niños aragoneses sanos. Nutr Hosp. 2018;35:782-8.
- Rodríguez-Dehli AC, Riaño-Galán I, Fernández-Somoano A, Navarrete-Muñoz EM, Espada M, Vioque J, et al. Hipovitaminosis D y factores asociados a los 4 años en el norte de España. An Pediatr (Barc). 2017;86:188-96.
- Institute of Medicine (US). Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. Ross AC, Taylor CL, Yaktine AL, Del Valle HB (Eds.). Dietary reference intakes for calcium and vitamin D. Committee to review dietary reference intakes for calcium and vitamin D. Washington: National Academ Press; 2011 [online] [accessed 09/03/2023]. Available at www.ncbi.nlm.nih.gov/books/NBK56070/
- Golden NH, Abrams SA. Committee on Nutrition. Optimizing bone health in children and adolescents. Pediatrics. 2014;134:e1229-43.
- Pallás Alonso C, Ureta Velasco N, Alonso Díaz C; PAPPS Infancia y Adolescencia de semFYC. Suplementación de vitamina D en la infancia. Rev Pediatr Aten Primaria. 2012;44:682-3.
- Piñeiro Pérez R, Núñez Cuadros E, Cabrera García l, Díez López I, Escrig Fernández R, Gil Lemus MA, et al. (Comité de Medicamentos de la AEP). Resultados de una encuesta nacional sobre conocimiento y uso de pseudociencias por parte de los pediatras. An Pediatr (Barc). 2022;96:25-34.
- Uday S, Kongjonag A, Aguiar M, Tulchinsky T, Högler W. Variations in infant and childhood vitamin D supplementation programs across Europe and factors influencing adherence. Endocr Connect. 2017;6:667-75.
- Cabezuelo Huerta G, Vidal Micó S, Abeledo Gómez A, Frontera Izquierdo P. Niveles de vitamina D en lactantes. Relación con la lactancia materna. An Pediatr (Barc). 2007;66:491-5.
- Durá Travé T, Gallinas Victoriano F, Chueca Guindulain MJ, Berrade Zubiri S, Moreno Gónzalez P, Malumbres Chacón M. Prevalencia de hipovitaminosis D y factores asociados en la edad infantojuvenil. Aten Primaria. 2018;50:422-9.
- Gutiérrez Medina S, Gavela Pérez T, Domínguez Garrido MN, Blanco Rodríguez M, Gracés C, Rovira A, et al. Elevada prevalencia de déficit de vitamina D entre los niños y adolescentes obesos españoles. An Pediatr (Barc). 2014;80:229-35.
- Rodríguez Rodríguez E, Aparicio A, Andrés P, Ortega RM. Moderate vitamin D deficiency and inflammation related markers in overweight/obese schoolchildren. Int J Vitam Nutr Res. 2014;84:98-107.
- Barceló A, Morell García D, Ribot C, De la Peña M, Peña Zarza JA, Alonso Fernández A, et al. Vitamin D as a biomarker of health in snoring children: a familial aggregation study. Pediatr Res. 2022;91:1176-81.
- Barja Fernández S, Aguilera CM, Martínez Silva I, Vázquez R, Gil Campos M, Olza J, et al. 25-hydroxyvitamin D levels of children are inversely related to adiposity assessed by body mass index. J Physiol Biochem. 2018;74:111-8.
- Segovia Ortí R, Barceló A, De Sotto Esteban D, Sanchís P, Pons J. Association between vitamin D status and allergen sensitization in pediatric subjects in the Balearic Islands. Pediatr Allergy Immunol. 2021;32:1183-9.
- Rey C, Sánchez Arango D, López Herce J, Martínez Camblor P, García Hernández I, Prieto B, et al. Vitamin D deficiency at pediatric intensive care admission. J Pediatr (Rio J). 2014;90:135-42.
- Cebey López M, Pardo Seco J, Gómez Carballa A, Martinón Torres N, Rivero Calle I, Justicia A, et al. Role of vitamin D in hospitalized children with lower tract acute respiratory infections. J Pediatr Gastroenterol Nutr. 2016;62:479-85.
- Sanmartín R, Pardos C, Doste D, Aguilera J, Alijarde R, Agón Banzo PJ, et al. The association between atopic dermatitis and serum 25-hydroxyvitamin D in children: Influence of sun exposure, diet, and atopy features-A cross-sectional study. Pediatr Dermatol. 2020;37:294-300.
- Garrido C, Cela E, Beléndez C, Mata C, Huerta J. Status of vitamin D in children with sickle cell disease living in Madrid, Spain. Eur J Pediatr. 2012;171:1793-8.
- Durá Travé T, Gallinas Victoriano F, Malumbres Chacón M, Moreno Gónzalez P, Aguilera Albesa S, Yoldi Petri ME. Vitamin D deficiency in children with epilepsy taking valproate and levetiracetam as monotherapy. Epilepsy Res. 2018;139:80-4.
- Martínez Suarez V, Dalmau Serra J. Hipovitaminosis D ¿una epidemia real? Pediatr Integral. 2020;24:351-5.
- Mengual Gil JM. Vitamina D por encima del año de vida, ¿es necesaria o está de moda? In: AEPap (ed.). Curso de Actualización Pediatría 2018. Madrid: Lúa Ediciones 3.0; 2018. p. 17-30 [online] [accessed 09/03/2023]. Available at www.aepap.org/sites/default/files/017-030_vitamina_d_por_encima_del_ano.pdf.
- Baccheta J, Edouard T, Laverny G, Bernardor J, Bertholet Thomas A, Castanet M, et al. Vitamin D and calcium intakes in general pediatric populations: A French expert consensus paper. Arch Pediatr. 2022;29:312-25.





