Vol. 24 - Num. 96
Original Papers
Knowledge of health professionals from the Region of Murcia (Spain) about breastfeeding
Rocío Díaz Córcolesa, Esther Ruiz Chércolesb
aPediatra. Consultorio local Los Garres. Los Garres. Murcia. España.
bPediatra. CS María Jesús Hereza. Leganés. Madrid. España.
Correspondence: R Díaz. E-mail: rocio040491@gmail.com
Reference of this article: Díaz Córcoles R, Ruiz Chércoles E. Knowledge of health professionals from the Region of Murcia (Spain) about breastfeeding . Rev Pediatr Aten Primaria. 2022;24:e363-e371.
Published in Internet: 30-11-2022 - Visits: 10747
Abstract
Introduction: low rates of duration of breastfeeding are a public health problem. The training of health personnel is essential for their promotion. Objective: to investigate the knowledge and skills in breastfeeding of Primary Care health professionals and pediatric residents.
Material and method: distribution of two questionnaires on breastfeeding, aimed at Primary Care health personnel (Survey on Knowledge of Breastfeeding, ECoLa) and pediatric residents (adapted questionnaire).
Results: 19 resident surveys and 47 Primary Care health professionals. Residents' average score: 18.57 points. Average score of Primary Care professionals: 19.6 points. 15.8% of residents consider that breastfeeding is the best food for the newborn, even if the mother is malnourished. 10.5% of the residents and 59.6% of the Primary Care health professionals know that the 'watered down milk' is the milk from the beginning of the intake. 10.5% of residents consider that pacifiers do not interfere with breastfeeding. 10.5% stop breastfeeding if the mother takes amoxicillin. 26.3% think that the first dose should be 3 hours after delivery. 31.9% do not know that exclusive breastfeeding with formula carries an increased risk of morbidity and mortality. 52.6% do not recommend breastfeeding if the mother is a carrier of hepatitis B.
Conclusions: the training of health professionals in breastfeeding is essential, the questionnaires may indicate gaps that must be addressed through training.
Keywords
● BreastfeedingINTRODUCTION
The World Health Organization (WHO) recommends breastfeeding (BF) for infants, exclusive until age 6 months and complemented with other foods through at least age 2 years.1
Human milk contains all the essential ingredients for the adequate growth and development of the infant, not only from a nutritional standpoint. Breastfeeding protects the health of the infant and the mother in the short, medium and long term, and strengthens their attachment.2-5 Breastfeeding promotion policies have been proven to have social, economic and environmental benefits.6
The current low duration trends in BF are considered a public health problem. Global targets have been established to achieve a prevalence of exclusive breastfeeding (EBF) through age 6 months of at least 50% worldwide. At present, in Spain, based on the National Health Survey of 2017, nearly 40% of women have maintained EBF at 6 months.7
Some of the risk factors associated with absence of initiation or early discontinuation of BF are low educational attainment, young maternal age, primiparity, multiple birth, caesarean delivery, prolonged labour, medicated childbirth, insufficient support in the household, workplace or by health care services, perceived low milk supply, latch problems, mastitis and the impact of marketing on the general population and health care collective. In this regard, the International Code of Marketing of Breast-milk Substitutes promulgated in the 34th session of the World Health Assembly of the WHO and later accepted by the industry seeks the regulation of the marketing and distribution of these products to health care professionals and maternity wards, restricting their use to cases in which it is necessary.
Mothers stay very short periods in the maternity ward, and most BF support is delivered at the primary care (PC) level. The lack of knowledge and skills on BF of health care professionals can have a negative impact on BF initiation and maintenance. The education of parents before and after childbirth is a key contributor to successful BF.8-11
In 1991, the WHO and the United Nations Children's Fund (UNICEF) published the Ten Steps to Successful Breastfeeding to promote BF in hospitals in what was named the Baby-Friendly Hospital Initiative, currently known in Spain as the Iniciativa para la Humanización de la Asistencia al Nacimiento y la Lactancia (IHAN). The system proposed by the IHAN is evidence-based and has proven effective in increasing BF rates and duration.2-6
Given the importance of training health care professionals on BF, the aim of our study was to assess the knowledge and skills on BF of PC clinicians and medical residents in paediatrics in the Region de Murcia, Spain.
MATERIAL AND METHODS
We conducted a cross-sectional descriptive study between January and April 2022. In this period, we distributed 2 questionnaires to assess knowledge on BF: one for health care workers in various PC centres in the Region of Murcia (paediatricians, family physicians, nurses and midwives) and another adapted for medical residents in paediatrics.
In 2003, M. C. Temboury Molina did a survey on the knowledge of BF of medical residents in paediatrics in several Spanish hospitals and found significant deficiencies in training.9 A little more than 10 years later, the Committee on Breastfeeding of the Asociación Española de Pediatría (AEP, Spanish Association of Pediatrics) validated the questionnaire on BF knowledge (known as ECoLa, for the Spanish Encuesta de Conocimientos en Lactancia).5 This was the questionnaire distributed to the PC professionals of the Region of Murcia, while we sent an adapted version to the medical residents. Both questionnaires were distributed via email and made accessible through the online Google Forms platform.
The adapted version of the questionnaire for medical residents comprised 24 items that contribute to the score (Appendix 1). The ECoLa questionnaire comprises 22 items that contribute to the score, for a maximum possible total score of 26 points (Appendix 2). It includes others from item 23 that do not contribute to the score. Questions 18 and 21 deserve particular attention because they are free-text fields:
- Item 18 asks for 5 aspects to consider in the assessment of a feeding (1 point per correct answer). Any aspects mentioned by the respondent included in the feeding observation form were considered valid (Appendix 3).5
- Item 21 assesses the ability to obtain quick and reliable information on drugs in the context of BF. The drug chosen for the purpose is adalimumab, since, while safe, it is described as incompatible in the summary of product characteristics until up to 5 months after the last injection. We considered e-Lactancia and LactMed valid resources.5
Both questionnaires explore different basic areas of knowledge and skills in BF: physiology of lactation, public health, problems in the early days, late problems, feeding assessment, maternal determinants and attitudes.
The statistical analysis was performed with MS Excel. We did a descriptive analysis of the variables. Categorical variables were expressed as proportions.
RESULTS
Analysis of the adapted questionnaire for residents (Appendix 4)
Responses: 19. Mean age: 27.4 years (range 25-32), 4 male (21%) and 15 female (79%); 4 in the first year of the residency, 3 in the second year, 6 in the third year and 6 in the fourth year.
Mean score: 18.57 points (over 24), 77.4% correct responses. By year of residency, first-year residents scored 18.25 points (76% correct responses), second-year residents 19 points (79.2% correct responses), third-year residents 19.5 points (81.2% correct responses) and fourth-year residents 17.8 points (74.3% correct responses).
Only 15.8% answered the first item correctly: even when the mother is malnourished, human milk is still the best possible food for the newborn. Most residents (89.5%) knew that BF should not be discontinued on account of the mother taking amoxicillin-clavulanic acid. As for the baby-friendly hospital initiative, 36.8% of residents had never heard of it.
In the item asking what “leche aguada” (“watery milk”, the Spanish term for foremilk) was, only 10.5% knew that it is the milk produced at the beginning of a feeding (Fig. 1).
| Figure 1. Knowledge on breastfeeding of health care professionals. Item 8: What is the scientific interpretation of what is commonly known as “watery milk”*? |
|---|
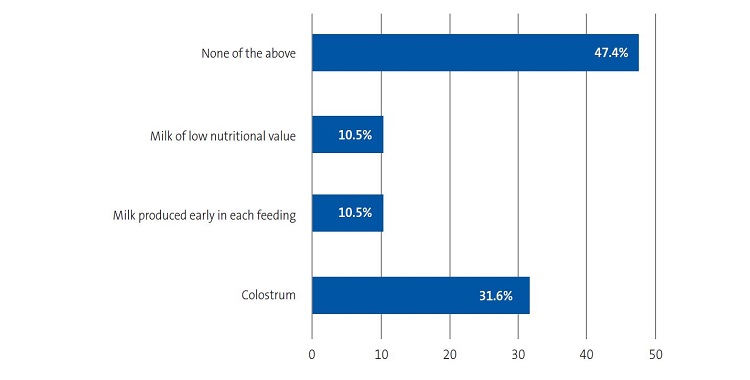 |

The amount of milk a women can produce depends on the frequency and vigour of feedings, an answer that was correctly selected by only 10.5% of residents (Fig. 2).
| Figure 2. Knowledge on breastfeeding of health care professionals. Item 9: The milk supply of a woman depends on: |
|---|
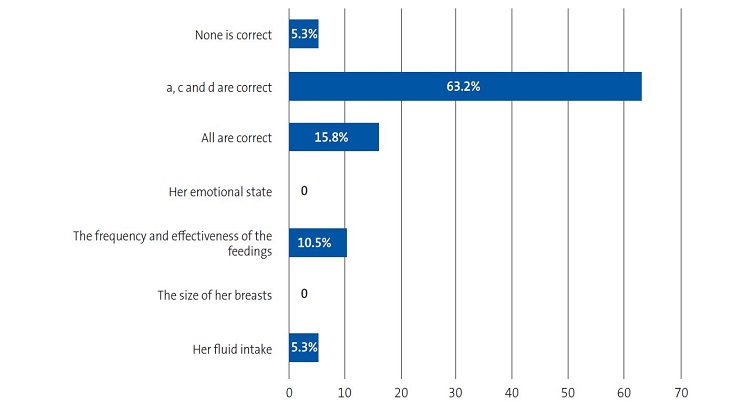 |

All respondents believed that the practice that is most helpful to promote BF in the maternity ward is to place the baby at the breast within 1 hour of birth, and 89.5% answered that the most accessible and effective strategy for nipple care is proper positioning.
Also, 79% correctly answered that the first feeding should take place immediately after birth, and 73.7% knew that more frequent feedings were associated with a reduced risk of jaundice. Of all respondents, 10.5% still believed that pacifiers do not interfere or hinder BF, 26.3% that the first feeding should occur at least 3 hours after birth, and 52.6% that hepatitis B-positive mothers should not breastfeed.
Analysis of the ECoLa questionnaire (Appendix 5)
Responses: 47. Mean age: 38.1 years (range 30-65), 6 male (12.8%) and 41 female (87.2%). Of all respondents, 23.4% had no children, 19.1% had one child, 40.4% two children and 17% three or more. Personal experience with BF was reported by 74.5%, with a median duration of BF of 27.5 months (range 1-96). As for the professional category, 76.5% were attending physicians (55.3% paediatricians, 21.3% family physicians) and 23.4% nurses (8.5% paediatric nurses, 12.7% general nurses and 2.1% midwives).
Mean score: 19.6 points (over 26), corresponding to a 75.5% correct response rate. By speciality, paediatric nurses answered 63.5% of items correctly, general nurses 66%, midwives 96.2%, family physicians 60.4% and paediatricians 84.6%.
Of all respondents, 31.9% were not aware that exclusive formula feeding is associated with an increased risk of morbidity and mortality. In the case supplementation is needed in the first few weeks of life, 80.9% answered correctly; it is generally not recommended to use a bottle for the purpose, with other options, such as a cup-feeding, relactation, finger-feeding, etc, being preferable. Still, 25.5% continued to believe that the newborn should be placed on a radiant warmer for weighing, calculation of the Apgar score and administration of ocular prophylaxis before being placed at the breast for the first feeding in the delivery room, and 27.7% did not think that a newborns needs to be awakened before every feeding after 15 hours post birth were infants at risk. Also, 76.6% believed that breast milk continues to be of high quality in the second year of life.
In the case of poor weight gain, 12.8% of respondents would prescribe supplementation; when it came to the “watery milk”, 59.6% knew that it is the foremilk produced at the beginning of each feeding. Of all respondents, 91.5% knew the current BF recommendations of the WHO.
In response to the item “Which of the following interventions is most important in a breastfeeding mother that has cracked nipples?”, 80.9% correctly answered that the most important intervention was observing a feeding (Fig. 3).
| Figure 3. Knowledge on breastfeeding of health care professionals. Item 16: Which of the following interventions is most important in a breastfeeding mother that has cracked nipples? |
|---|
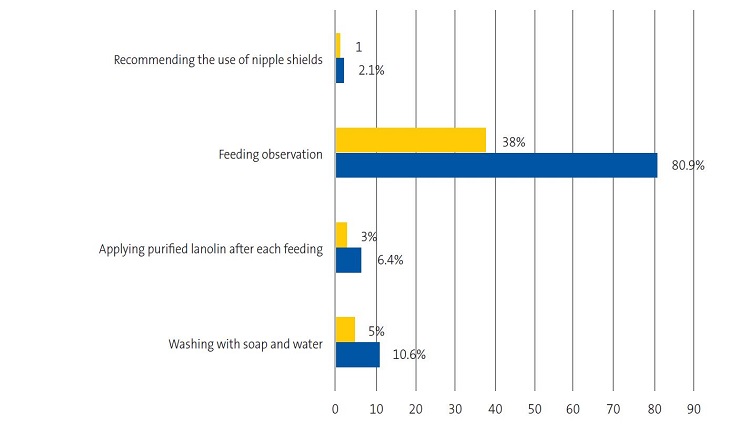 |

In the item presenting the clinical scenario of an infant aged 17 days brought to the emergency department by the parents due to inconsolable crying, 68.1% correctly answered that it was indicative of a growth spurt (Fig. 4).
| Figure 4. Knowledge on breastfeeding of health care professionals. Item 17: A 17 day old infant is brought to the emergency room by the parents due to inconsolable crying… What does this suggest to you and how would you approach it? |
|---|
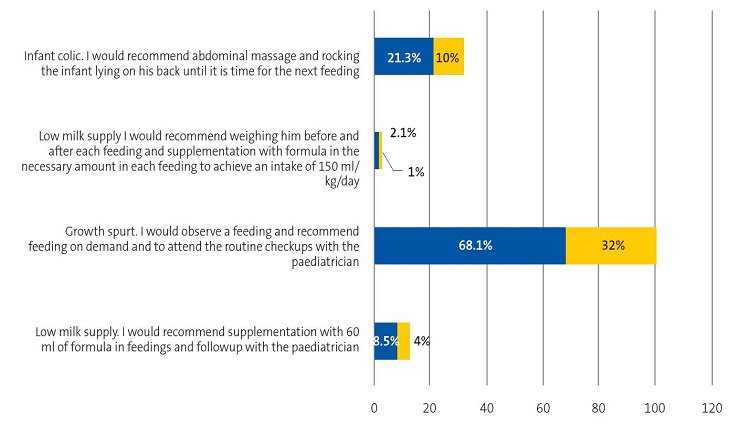 |

In the item that asked for 5 characteristics of a good latch, 121 answers (out of 235) were considered valid, including: lips curled out, absence of soreness, full cheeks, chin touching breast, relaxed mother, close contact, navel to navel, nose level with nipple, wide open mouth, lips around nipple and areola, absence of clicking sounds, baby appears satisfied. Six respondents did not answer this question.
Only 66% of respondents believed that providing free samples of starter formula to mothers in health care facilities was a violation of the International Code of Marketing of Breast-milk Substitutes.
In relation to trainings on BF, 48.9% of respondents had not participated in any. Of the 51.5% that had received trainings, 52.2% had only received one, 17.4% two, 13% three and 12.9% for or more (ranging from 2 to 100 hours). As to the most important source of knowledge on BF, 48.9% answered that it was trainings, 57.4% that it was books or articles, 6.4% the medical school curriculum, 7.4% older residents, attending physicians or co-workers and 74.5% personal experience. When it came to the perceived quality of the training on BF received in the past few years, only 17% considered it satisfactory and 10.6% very satisfactory (Fig.5).
| Figure 5. Knowledge on breastfeeding of health care professionals. Perceived quality of the education on breastfeeding received in the past few years of training |
|---|
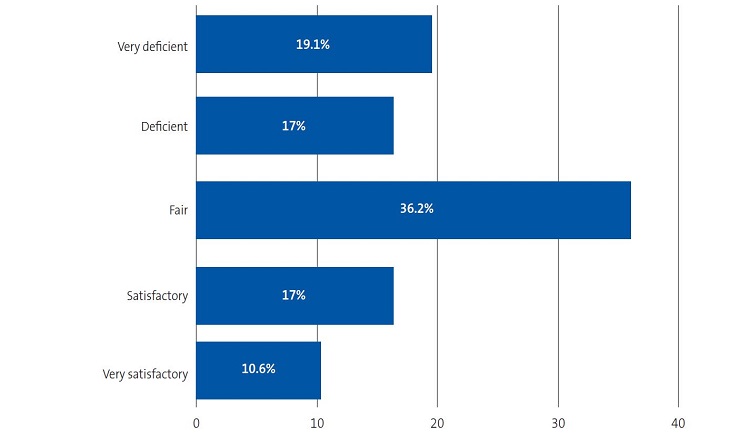 |

Of all respondents, 89.4% considered they should be experts in the diagnosis and management of BF problems. As for the reason, 61.7% said that this was a frequent reason for consultation, 70.2% that it would benefit patients and their families, and 61.7% that it is part of their jobs.
DISCUSSION AND CONCLUSIONS
Several studies have shown that clinical guidance can improve BF initiation rates and duration. However, there is also ample evidence of the deficient training of many paediatricians, both abroad12-14 and in Spain,9 and physicians in other specialities.15,16
In our study, the percentage of correct answers was similar in both groups, PC professionals and paediatrics residents (75.5% and 77.4%, respectively). The scores obtained in both groups were considered good or acceptable, based on the scoring recommendations of the authors of the questionnaires, who classified scores as: <50% very deficient, 50-70% deficient, 70-85% good, >85% excellent.5
We ought to mention that the Region de Murcia is currently in phase 2 of the IHAN initiative, so that the results of our study may be better compared to previous studies or to studies conducted in non-IHAN hospitals.
For instance, comparing our results with the nationwide study published in 2003 by M. C. Temboury Molina,9 we can see a significant improvement in the mean score. In the 2003 study, the residents I Murcia achieved a mean score of 14.22 points (below the national average) compared to 18.57 points in our study. However, we found it interesting that 36.8% of current residents still had not heard of the baby-friendly hospital concept.
The study by Gómez Fernández-Vegue6 in medical residents in paediatrics published in 2019 showed improvement, as the mean score in the questionnaire was 21.15 ± 4.67 points (with a range of 3-26 points and a median of 23 points). It also demonstrated that the knowledge of residents was greater in IHAN hospitals compared to other hospitals.
In a study conducted in Canada13 with the aim of assessing the knowledge, beliefs and attitudes of paediatricians, family physicians and final-year paediatric and final-year family medicine residents, the correct knowledge score of physicians was under 70%, while it was above 70% in paediatrics residents The mean correct knowledge score was 67.8 % in paediatricians, 64.3 % in family physicians, 72.7 % in final-year paediatrics residents and 66.8 % in family medicine residents. In our study, family physicians had slightly lower scores (60.4%), while paediatrics residents overall, final-year residents in particular and attending paediatricians achieved the best scores (77.4% in residents, 74.3% in final-year residents and 84.6% in attending paediatricians).
In a study conducted in 14 public hospitals in the region of Castilla y Leon in 201910 that focused on neonatologists, gynaecologists, midwives, nurses and nurse aids, two thirds in the professional categories that had professional contact with mothers initiating BF did not have a level of knowledge defined as good or acceptable (only neonatologists and midwives exceeded 70% of correct answers). In our study, comparing scores by specialities, only midwives, attending paediatricians and paediatrics medical residents had more than 70% of correct answers.
Few studies on the subject have been conducted at the PC level in Spain; specifically, in 2001 a study was conducted in health care professionals practicing in a health care zone in the Valencian Community.17 In that study, 36% of respondents believed that newborns had to be trained to feed on a regular schedule and were against feeding on demand, compared to 21.3% of PC professionals and none of the residents in our study. In the past study, 20% of health care professionals continued to believe that breast milk could be of poor quality and 80% that the maternal diet has an impact on the quality of the milk; in our study, all residents believed that breast milk continued to be of high quality in the second year of life and 23.4% of PC professionals believed that the nutrient content decreased after the first year. Only 15.8% of the residents believed that the maternal diet had an effect on the quality of breast milk. Also, 29% of respondents in the past study believed that pacifiers and plastic nipples soothed the baby and facilitated BF, compared to 10.5% in our study. In the past, 28% recommended washing with soap and water for nipple care, compared to 10.6% in our study. Also, 18% of clinicians in the past study would have offered a dextrose solution or water between feedings if the baby cried, while none of the respondents in our study would.
Our study evinced a lack of knowledge, especially as regards the composition of human milk and the physiology of lactation. For example, only 10.5% of residents knew that the foremilk was the milk produced at the beginning of a feeding, only 10.5% correctly answered that milk production increased with the frequency and effectiveness of BF, and 26.3% believed that the first feeding should occur 3 hours after the birth.
When it came to PC professionals, the salient findings were that 31.9% were unaware that formula feeding is associated with an increase in morbidity and mortality, 40.4% did not know what foremilk was, 25.5% would not place healthy newborns on their mothers with skin to skin contact immediately after birth without carrying out some type of intervention first, 27.7% would not be able to identify a newborn that needs to be awakened for every feeding after 15 hours post birth as being at risk, and 34% did not know about the International Code of Marketing of Breast-milk Substitutes. In addition, 21.3% believed that BF should not be offered on demand, and 23.4% believed that the quality of breast milk is not good in the second year of life.
Respondents that had received training on BF had slightly better scores than those who had not (mean score of 20.54 points vs. 18.65 points). We ought to highlight that more than half of respondents (57.5%) was fairly or totally prepared to diagnose and offer solutions to specific BF problems.
Despite the efforts made in recent years, much remains to be done to further improve the training of medical residents and, most importantly, PC providers in the management of BF; there are still significant areas of improvement, especially as regards the International Code of Marketing of Breast-milk Substitutes and the risks associated with formula feeding.
While it is undeniable that individual effort is important, the funding and offering of trainings and activities related to BF also need to increase to make improvements possible, as does the support of institutions, scientific societies and health care authorities.
The training of health care professionals is essential for improving BF initiation and maintenance rates.
Questionnaires can identify gaps in knowledge that can be addressed with training.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
AEP: Asociación Española de Pediatría (Spanish Association of Pediatrics) · BF: breastfeeding · EBF: exclusive breastfeeding · EcoLa: Encuesta de Conocimientos en Lactancia (Breastfeeding Knowledge Survey) · IHAN: Iniciativa para la Humanización de la Asistencia al Nacimiento y la Lactancia (Initiative for the Humanization of Childbirth and Breastfeeding Services)· PC: primary care · WHO: World Health Organization.
SUPPLEMENTARY INFORMATION
Appendix 1. Questionnaire adapted for medical residents, developed by the Committee on Breastfeeding of the AEP.
Appendix 2. Questionnaire on the knowledge of breastfeeding (ECola).
Appendix 3. Checklist of correct items in a feeding observation.
Appendix 4. Correct answers of residents in paediatrics to the adapted questionnaire.
Appendix 5. Correct answers of primary care providers to the ECoLa questionnaire.
REFERENCES
- La duración óptima de la lactancia materna exclusiva: resultados de una revisión sistemática de la OMS. In: World Health Organization (WHO), Geneva (2001) [online] [accessed 16/11/2022]. Available at www.who.int/es/news-room/fact-sheets/detail/infant-and-young-child-feeding
- Alves da Cunha AJ, Madeiro Leite ÁJ, Saraiva de Almeida I. The pediatrician’s role in the first thousand days of the child: the pursuit of healthy nutrition and development. J Pediatr (Rio J). 2015;91:S44-51.
- Traebert J, Lunardelli SE, Martins LGT, Santos KD, Nunes RD, Lunardelli AN, et al. Methodological description and preliminary results of a cohort study on the influence of the first 1.000 days of life on the children’s future health. An Acad Bras Cienc. 2018;90:3105-14.
- Moreno Villares JM, Collado MC, Larqué E, Leis Trabazo R, Saenz de Pipaón M, Moreno Aznar LA. Los primeros 1000 días: una oportunidad para reducir la carga de las enfermedades no transmisibles. Nutr Hosp. 2019;36:218-32.
- Gómez Fernández-Vegue M, Menéndez Orenga M. Validación de un cuestionario sobre conocimientos y habilidades en lactancia materna. An Pediatr (Barc). 2015;83:387-96.
- Gómez Fernández-Vegue M, Menéndez Orenga M. Encuesta nacional sobre conocimientos de lactancia materna de los residentes de pediatría en España. Rev Esp Salud Pública. 2019;93:e201908060.
- Encuesta Nacional de Salud 2017. In: Portal Estadístico del SNS. Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid; 2017 [online] [accessed 16/11/2022]. Available at www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm
- Pallás Alonso CR, Soriano Faura J, Colomer Revuelta J, Cortés Rico O, Esparza Olcina MJ, Galbe Sánchez-Ventura J, et al. Apoyo a la lactancia materna en Atención Primaria. Rev Pediatr Aten Primaria. 2019;21:191-201.
- Temboury Molina MC. Informe sobre el conocimiento de los residentes de pediatría en el manejo de la lactancia materna. An Pediatr (Barc). 2003;58:263-7.
- González Vereda MJ, Bachiller Luque MR, Dorado Díaz A, Martín Pérez P, Maté Enríquez T, Niño Martín V. ¿Cuánto saben de lactancia los sanitarios del área materno-infantil? Estudio de los 14 hospitales públicos de Castilla y León. Rev Pediatr Aten Primaria. 2019;21:133-46.
- De Jesus PC, De Oliveira MI, Fonseca SC. Impact of health profesional training in breastfeeding on their knowledge, skills, and hospital practices: a systematic review. J Pediatr (Rio J). 2016;92:436-50.
- Schanler RJ, O’Connor KG, Lawrence RA. Pediatricians’ practices, attitudes regarding breastfeeding promotion. Pediatrics. 1999;103:e35.
- Pound CM, Williams K, Grenon R, Aglipay M, Plint AC. Breastfeeding knowledge, confidence, beliefs, and attitudes of Canadian physicians. J Hum Lact. 2014;30:298-309.
- Freed GL, Clark SJ, Lohr JA, Sorenson JR. Pediatrician involvement in breast-feeding promotion: a national study of residents and practitioners. Pediatrics. 1995;96 3 Pt 1:490-4.
- Freed GL, Clark SJ, Sorenson J, Lohr JA, Cefalo R, Curtis P. National assessment of physicians’ breast-feeding knowledge, attitudes, training, and experience. JAMA. 1995;273:472-6.
- Freed GL, Clark SJ, Curtis P, Sorenson JR. Breast-feeding education and practice in family medicine. J Fam Pract. 1995;40:263-9.
- Palomares Gimeno MJ, Labordena Barceló G, Sanantorio Valdearcos F, Agramunt Soler G, Nácher Fernández A, Palau Fuster G. Opiniones y conocimientos básicos sore lactancia materna en el personal sanitario. Rev Pediatr Aten Primaria.2001;3:393-402.





