Vol. 24 - Num. 95
Original Papers
Importance of the epidemiological investigation of a Salmonella outbreak in a school setting
M.ª del Mar López Matiaccia, Laura Moratilla Monzób, Miguel Ángel Zafra Anta
aServicio de Pediatría. Hospital Universitario de Fuenlabrada. Fuenlabrada. Madrid. España.
bServicio de Medicina Preventiva. Hospital Universitario de Fuenlabrada. Fuenlabrada. Madrid. España.
cPediatra. Grupo de Trabajo de Historia de la Asociación Española de Pediatría (AEP). Servicio de Pediatría. Hospital de Fuenlabrada. Fuenlabrada. Madrid. España.
dUnidad Técnica 9 del Área de Salud Pública. Consejería de Sanidad de la Comunidad de Madrid. Madrid. España.
Correspondence: MA Zafra. E-mail: miguelzafraanta@gmail.com
Reference of this article: López Matiacci MM, Moratilla Monzó L, Zafra Anta MA, García Marín N, Artero Segura RM, García Barba S. Importance of the epidemiological investigation of a Salmonella outbreak in a school setting . Rev Pediatr Aten Primaria. 2022;24:241-7.
Published in Internet: 04-10-2022 - Visits: 11385
Abstract
Introduction: we describe an outbreak of Salmonella gastroenteritis in an early childhood education centre and a neighbouring public school in a town in the south of the Community of Madrid (Spain) in October and November 2019. Objectives: to describe the epidemiological characteristics of an outbreak of salmonellosis, analyse the mechanism of transmission and underscore the importance of health reporting.
Methods: retrospective and prospective descriptive study of salmonellosis cases reported by different sources related to a school community. Analysis of variables in hospitalised patients. Epidemiological investigation and microbiological characterization.
Results: there were 38 reported cases (age range, 7 months-8 years; mean, 2.7 years). They were enrolled in 2 educational centres: 57.9% attended a nursery school and the rest were students of a neighbouring school who came to the nursery for lunch or recreation activities. Twelve were hospitalised (3 hospitals). There were no serious complications. The National Microbiology Centre identified Salmonella Typhimurium 4,5,12:i:-, a monophasic variant of S. enterica, in stool cultures. The inspection showed that food was not the source of transmission, but that there was a risk of faecal-oral was not alimentary; on the other hand, there was a risk of transmission through the faecal-oral route and fomites; the physical separation between different areas was suboptimal. Proposals for improvement were made. No more cases were reported thereafter.
Conclusions: the outbreak was not related to food, and its analysis allowed the implementation of measures to avoid secondary cases later on. Case reporting is considered of utmost importance to take appropriate public health measures.
Keywords
● Epidemic outbreak ● Gastroenteritis ● Non-foodborne ● Salmonella enteritidisINTRODUCTION
From an epidemiological surveillance perspective, an outbreak is defined as the detection of 2 or more cases of the same disease related to a given time, place and person, although the term can also be used to refer to catastrophic events or the emergence of a health problem in a territory previously free from it. The involvement of providers of the health care system, both public and private, is essential to produce the information required to do research and implement measures of control.1
The current regulatory framework of the Community of Madrid (Spain) calls for the mandatory and urgent reporting of any suspected outbreak. Epidemiological surveillance has been carried out in the Community of Madrid since 1996, in adherence to Decree 184/1996 of the Department of Health and Social Services, updating the conditions considered notifiable diseases (NDs) according to European Union regulations per Order SSI/445/2015. In adherence to this order, salmonellosis became a notifiable disease in 2015. As a ND, any new microbiologically confirmed cases of salmonellosis must be reported on a weekly basis.2
The most frequent and largest outbreaks of communicable diseases are those associated with foodborne or waterborne pathogens. Based on the most recent reports of the Community of Madrid, in 2017 there were 347 outbreaks amounting to a total of 4849 cases, of which 131 outbreaks were classified as foodborne outbreaks (2.01 outbreaks per 100 000 inhabitants) and 76 as non-foodborne acute gastroenteritis outbreaks (1.17 outbreaks per 100 000 inhabitants, with 2397 associated cases, 16 hospital admission, hospitalization rate of 0.67%, no deaths). In the subset of non-foodborne outbreaks, transmission occurred in the household in 17.1% of cases and in nursing homes, nurseries or schools in the rest (10 outbreaks, 320 cases). Cases were reported by the affected individuals or facilities (65.8%) and from the health care system (23.7%), with a higher incidence in the spring and autumn. The causative agent was identified in 38 of the 76 outbreaks (50% of outbreaks, with a higher proportion in household outbreaks), and norovirus and Salmonella were the most frequent pathogens (52.6% and 26.3%, respectively).
In this article, we describe an outbreak of gastroenteritis caused by Salmonella associated with a childcare centre and a neighbouring public school located in a town in the south of the Community of Madrid (Spain) between September and November 2019.
Objectives: to describe the epidemiological characteristics of the outbreak, analyse the mechanism of transmission and demonstrate the importance of notifying outbreaks of salmonellosis to the public health authorities.
MATERIAL AND METHODS
We conducted a retrospective and prospective descriptive study through the analysis of cases of microbiologically confirmed salmonella infection in patients that visited the emergency department of the Hospital Universitario de Fuenlabrada (HUF) and associated with a school community. We collected data on the following variables: age, sex, attendance to childcare centre or school, use of food services in childcare centre (yes/no), date of onset, hospital admission (yes/no), length of stay (days), associated complications (dehydration, acidosis, hyponatraemia, other), administered treatment, results of microbiological testing (typing). We collected the information from patient health records and interviews with caregivers. We conducted interviews in the educational centres and with relatives of the patients, by telephone or at the bedside in hospital.
We generated a chart of the epidemic curve that shows the chronological association of the cases based on the date of onset. We also completed the dataset with data on the same variables collected from other cases reported to the public health authorities of the corresponding area, corresponding to patients managed at the primary care level and/or in other hospitals in the area.
RESULTS
The first patient admitted to our hospital, the index case in our study, was a boy aged 2 years admitted on October 24 who presented with symptoms of 12 hours' duration, including fever up to 38 °C, loose stools (with a frequency of 1 bowel movement per hour), 1 episode of vomiting and a history of several similar cases in the childcare centre he attended.
The outbreak was reported to the Department of Public Health on October 25 2019, following notification from the department of paediatrics to the department of preventive medicine of the HUF of the admission of 3 children (one aged 2 years and two aged 3 years) presenting with gastroenteritis. All had lunch in the childcare centre, although 2 of them attended the school across the street. At the time of the report, Salmonella enterica had been isolated from one of the stool cultures, while the results of the stool cultures for the other 2 patients were pending.
In total, 38 cases of salmonellosis associated with the school community were notified. They occurred in 19 girls and 19 boys aged 7 months to 8 years (mean: 2.71 years). Twenty-two (57.89%) were enrolled in a childcare centre, and 16 (42.1%) attended the public school across the street from it, but went to the childcare centre for food services (breakfast, lunch or afternoon snack) or recreational activities. There were no cases among the childcare centre staff (5 childcare workers and 1 cook) or the rest of the student body or staff of the public school.
There were 12 hospital admissions, distributed between the HUF (9 cases), the Hospital Universitario Fundación Alcorcón (2 cases) and the Hospital Universitario HM Puerta del Sur in Móstoles (1 case). The children resided in Humanes de Madrid and Moraleja de Enmedio. The reason for admission was dehydration, except in an infant aged 7 months admitted for fever and bulging fontanelle in the context of diarrhoea in household contacts. There were no serious complications or deaths.
A total of 17 patients sought care in the HUF and underwent collection of stool samples for culture that turned out positive for Salmonella. They presented with similar manifestations: fever, diarrhoea, malaise, abdominal and general pain, vomiting. Table 1 summarises the characteristics of the cases that resulted in hospital admission.
| Table 1. Main characteristics of the 9 cases of acute gastroenteritis that required admission to the Hospital Universitario de Fuenlabrada | ||||||||
|---|---|---|---|---|---|---|---|---|
| Case | Age in years or months | Sex | Length of stay | Dehydration | Compensated metabolic acidosis | Mild hyponatraemia | Other | Antibiotherapy |
| 1 | 2.4 y | Male | 6 | Yes | Yes | Yes | No | No |
| 2 | 3.1 y | Male | 6 | Yes | Yes | No |
ITU by Enterococcus faecalis Mild prerenal failure |
Yes; fot ITU |
| 3 | 3.6 y | Male | 2 | Yes | No | Yes | No | No |
| 4 | 2.1 y | Female | 4 | Yes | No | Yes | No | No |
| 5 | 2.1 y | Female | 2 | Yes | No | No |
Stool not collected Hypoglycaemia |
No |
| 6 | 20 m | Female | 8 | Yes | No | Yes | Upper airway infection | Ceftriaxone (5-day fever) |
| 7 | 23 m | Female | 6 | Yes | Yes | Yes | Bronchitis | No |
| 8 | 7 m | Male | 3 | No | No | No |
Fever Bulging fontanelle (normal LP) |
No |
| 9 | 22 m | Female | 5 | Yes | No | No | No | No |

Additional diagnostic tests were performed depending on the clinical presentation. They included a capillary blood gas analysis, complete blood count and blood chemistry panel in every case, and additional tests depending on the clinical manifestations. All hospitalised patients received intravenous fluids. The mean length of stay was 4.67 days.
A girl aged 15 months presented with primary immune thrombocytopenia (PIT) 8 days after the onset of symptoms of gastroenteritis due to Salmonella. The onset consisted in a recurrence of fever and development of petechiae, thrombocytopenia with a platelet count of 5000, mild anaemia and leucocytosis and metamyelocytes-possible blasts, so the patient was transferred to the tertiary care referral hospital, where she stayed for 2 days to undergo diagnosis and receive immunoglobulin therapy.
All stools samples were processed and cultures done in the hospital laboratory that yielded positive results for Salmonella were submitted to the Centro Nacional de Microbiología (Instituto de Salud Carlos III) for characterisation, and were identified as Salmonella enterica, monophasic typhimurium variant 4.5,12:i:-. Genotyping was not performed.
One stool culture evinced coinfection by Salmonella and Citrobacter braakii (Enterobacteriaceae family). The presence of viruses in stools was assessed with a polymerase chain reaction (PCR) panel that included adenovirus 40/41, astrovirus, norovirus, rotavirus and sapovirus. All samples tested negative for viruses.
The same day the outbreak was notified, Technical Unit 9 (TU9) of the Department of Health started active epidemiological surveillance, sending the epidemiologist and food hygiene technicians of the TU9 to the childcare centre to inspect the facilities and collect retain samples of the foods consumed in the days preceding the emergence of cases, as foodborne transmission was initially suspected. In the same visit, the team recommended intensifying hygiene and disinfection measures. Neither Salmonella nor other pathogens were isolated from the samples of the foods consumed in the childcare centre on October 21 and 22.
In a second inspection conducted on November 6, the team identified a risk of cross-contamination due to the performance of diaper changes, preparation of bottles and handling of meal items in the same space without optimal separation. In addition, there was inadequate control of the access of children (especially older ones) to the toilet, and the available space was not proportionate to the number of meals that were prepared and served. A new round of cleaning and disinfection was ordered, in addition to resolution of the identified deficiencies, to prevent new cases. There were no more cases after that date.
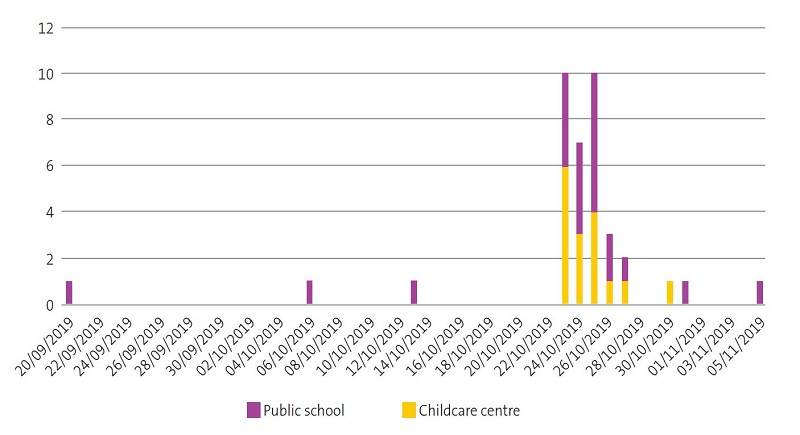
As regards the epidemiological study, 81.6% of cases (31 out of 38) had onset between October 23 and 27. There had been 3 isolated cases in the second fortnight of September and the first fortnight of October (which was known a posteriori upon reviewing other notifications of isolated cases of salmonellosis reported from primary care) (Fig. 1). There were 6 associated cases in 3 sibling pairs, some of which were secondary cases in which infection was transmitted in the household. In fact, some of the parents said they had experienced gastrointestinal symptoms and diarrhoea for which they had not sought medical care.
DISCUSSION
Salmonella infection is most commonly associated with the ingestion of eggs, fowl products and dairy products, but many other foods (including contaminated powdered infant formula3), the faecal-oral route (contact with hands or fomites) and contact with pets,4 including turtles, reptiles or even parrots,5 among others, are also sources of infection.6
In cases of Salmonella infection, risk factors for complications or severe disease must be taken into account7:
- Immunosuppressed status, including due to HIV infection, systemic immunosuppressive steroid therapy, depressed phagocytic function, haemoglobinopathy, chronic granulomatous disease.
- Extreme ages: newborns (risk of meningitis) and the elderly. Antibiotherapy should also be considered in infants under 3 months with salmonellosis. Adults aged more than 50 years are at risk, especially those with known endovascular disease or atherosclerosis, due to the risk of aortitis if bacteraemia develops.
- Malaria, histoplasmosis. Antibiotherapy the previous month.
- Abnormal gastrointestinal function. Use of antacids.
A possible association of PIT with a preceding infection has been described in children aged 1 to 6 years (a proposed mechanism is an abnormal autoimmune response triggered by viral illness or infection of other aetiology).8
Of the total cases of salmonellosis notified in Spain in 2016 in which a serotype was identified,9 3.8% were caused by the monophasic variant of S. typhimurium (126 cases). Cases were more frequently caused by S. typhimurium (1953 cases; 58.7%) and S. enteritidis (1110; 33.4%).
The notification of outbreaks is mandatory. The suspicion can arise from different sources. In our study, cases were notified from the HUF (15), the school (9), the Hospital Severo Ochoa (5), primary care facilities (4), the families themselves (4) and the childcare centre (1).
Thus, the investigation of an outbreak can start from the clinical suspicion of health care professionals and physicians, but also from schools, food or hospitality services, parents or even city councils. It then falls to microbiology laboratory and clinicians to report the clustering of cases to the department of preventive medicine of the hospital, which in turn notifies the Department of Public Health Services, the Rapid Public Health Alert Service or even the Epidemiology Department of the Department of Health of Madrid.1
Neither the epidemiological interviews nor the inspections carried out in our study succeeded in clearly identifying the source of the outbreak; but a food-borne origin was ruled out within reason. A turtle tank was initially suspected as the source of the outbreak, but it was later verified that there were no animals in within the premises. Previous isolated cases were identified, and the acme of the outbreak peaked on October 24, as can be seen in Figure 1. Only one of the stool cultures for the 38 known cases turned out negative, and Salmonella was identified in the rest. The submission of all the isolated strains to the Centro Nacional de Microbiología allowed the full characterization of Salmonella and evinced a direct association with the sporadic cases reported before October 23 and the clustering of cases in the days that followed, as all isolates were of the same serotype.
School staff also underwent collection of stool samples for culture, with negative results for enteric pathogens.
Some possible contributing factors were the lack of adequate control of children’s access to the toilet (the space that served as the classroom and canteen was open to the washing and toilet area, without intervening doors, allowing access and playing in both) and the lack of proportion between the size of the available space and the number of meals prepared and served. All these factors may have contributed to the development of the outbreak through one or more mechanisms of transmission, chiefly person-to-person through the contamination of surfaces and via the faecal-oral route.
The importance of early notification, the standardization of the response and the coordination between the involved institutions or care levels, in addition to parents and caregivers, are essential to the adequate implementation of prevention and control measures when an outbreak is suspected.1 Knowing the epidemiological and microbiological characteristics of the disease is also crucial to be able to implement preventive measures and reduce the incidence.
This study had two chief limitations: first, that the origin of the outbreak could not be identified, although it was known that transmission occurred through person-to-person contact and fomites, and second, that we may have underestimated the number of cases, missing those with mild presentations or for which patients did not seek care.
CONCLUSION
The outbreak was not foodborne, but emerged and spread through other routes. The relevance of an exhaustive epidemiological investigation and the potential benefits of educating the general population on food safety should not be underestimated. The analysis of the outbreak allowed the implementation of measures to prevent future cases. All health care professionals share the responsibility to report cases of notifiable diseases. Studies like the one we present here underscore the importance of reporting outbreaks to implement more effective interventions.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
PREVIOUS PRESENTATION
Partial results of this study were presented as an oral communication at the XXIV Meeting of the Sociedad de Pediatría de Madrid y Castilla-La Mancha, October 22-23, 2021, Guadalajara, Spain.
ABBREVIATIONS
HIV: human immunodeficiency virus · HUF: Hospital Universitario de Fuenlabrada · PIT: primary immune thrombocytopenia · TU9: Technical Unit 9 of the Public Health Section.
REFERENCES
- Dirección General de Salud Pública. Subdirección General de Epidemiología. Brotes Epidémicos en la Comunidad de Madrid, año 2017 [online] [accessed 16/06/2020]. Available at comunidad.madrid/sites/default/files/doc/sanidad/epid/brotes_epidemicos_2017.pdf
- Centro Nacional de Epidemiología. Instituto de Salud Carlos III. Red Nacional de Vigilancia Epidemiológica. Protocolos de la Red Nacional de Vigilancia Epidemiológica. Madrid, 2015 [online] [accessed 16/06/2020]. Available at www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/PROTOCOLOS/PROTOCOLOS%20EN%20BLOQUE/PROTOCOLOS_RENAVE-ciber.pdf
- Andreu Román MM, Allué Tango M, Berbel Hernández D, Andrés García I. Brote por Salmonella serovar Poona en una guardería. Rev Pediatr Aten Primaria. 2016;18:35-43.
- Marin C, Vega S, Marco-Jiménez F. Tiny turtles purchased at pet stores are a potential high risk for salmonella human infection in the Valencian Region, Eastern Spain. Vector Borne Zoonotic Dis. 2016;16:455-60.
- Olmedo Lucerón C, Pérez Meixeira A, Abad Sanz I, Cid Deleyto V, Herrera León S, Gutiérrez Ruiz l. An outbreak of Salmonella typhimurium associated with playground sand in a preschool setting-Madrid, Spain, September-October 2016. MMWR. 2017;66:256-57.
- Hohmann EL. Non typhoidal Salmonella: Microbiology and epidemiology. In: UpToDate. 2019 [online] Available at www.uptodate.com/contents/nontyphoidal-salmonella-microbiology-and-epidemiology
- Hohmann M EL. Non typhoidal Salmonella: Gastroeintestinal infection and carriage. In: UpToDate. 2019 [online] Available at www.uptodate.com/contents/nontyphoidal-salmonella-gastrointestinal-infection-and-carriage
- D'Orazio JA, Neely J, Farhoudi N. ITP in children: pathophysiology and current treatment approaches. J Pediatr Hematol Oncol. 2013;35:1-13.
- Centro Nacional de Epidemiología. CIBER Epidemiología y Salud Pública (CIBERESP). Instituto de Salud Carlos III. Madrid, 2018. Resultados de la vigilancia epidemiológica de las enfermedades transmisibles. Informe anual 2016 [online] [accessed 16/06/2020]. Available at http://gesdoc.isciii.es/gesdoccontroller?action=download&id=25/01/2019-d8ee271b6f