Covid outbreak. After emerging from lockdown, what happened in our primary care consultations?
Yolanda Martín Peinadora, Mar Braza Claverb, Raquel Girón del Ríoa, Clara Torres Delafuea, Soledad Gallego Campilloa
aPediatra. CS Goya.
bMIR-Pediatría. Hospital Infantil Universitario Niño Jesús .
Correspondence: Y Martín. E-mail: yolmarpei@gmail.com
Reference of this article: Martín Peinador Y, Braza Claver M, Girón del Río R, Torres Delafue C, Gallego Campillo S. Covid outbreak. After emerging from lockdown, what happened in our primary care consultations? Rev Pediatr Aten Primaria. 2022;24:e53-e60.
Published in Internet: 12-04-2022 - Visits: 9917
Abstract
Introduction: on March 11, 2020, the World Health Organization (WHO) declared the outbreak caused by the novel coronavirus SARS-CoV-2 a pandemic. The rapid increase in cases forced governments and health authorities to take measures to contain the pandemic. After the first wave, when there was evidence of a decline in the number of cases, reopening started with progressive lifting of containment measures and ending the confinement of the population. Our objective was to analyse paediatric care delivery in our primary care centre at this point in the pandemic to determine the modalities of care delivery used (in-person/remote), the reasons for consultation in the total provided services and the degree of successful resolution of the reason for consultation.
Material and methods: prospective, observational and descriptive study of the patients managed by the paediatrics clinic of a primary care centre in the city of Madrid, Spain, in June 2020. We collected data from the paediatric primary care electronic health records system of Madrid.
Results: a total of 1321 patients were treated, 34% fewer compared to the same period the previous year. Forty-nine percent of consultations were managed in-person at the site and 51% remotely. Telephone consultations were the most frequent alternative to in-person visits. Of all the reasons for consultation, 20.7% were managed remotely.
Conclusion: in the wake of the public health emergency brought on by COVID-19, the remote care modality has become prevalent and grown as a means to resolve patient needs and presenting complaints in our paediatric primary care clinic. We believe that this care modality should be reinforced with digital tools so that it can supplement and coexist with the conventional model of in-person care delivery.
Keywords
● COVID-19 ● Pandemic ● Primary care ● Remote consultationINTRODUCTION
In December 2019, the public health authorities of the People’s Republic of China reported the detection of a cluster of cases of pneumonia of unknown aetiology. Early research evinced that it was cause by a new type of coronavirus that was eventually named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that was highly contagious. The disease it produced, known as coronavirus disease 2019 (COVID-19), had onset with respiratory symptoms similar to those caused by other common pathogens. Most cases were mild (80%), but a small percentage (of up to 5%) had a severe course, manifesting with respiratory distress syndrome, hypoxaemia, septic shock and possibly multiple organ failure, in some cases leading to death (1-3.5%). Most patients were aged between 30 and 79 years, with the disease affecting very few children, with paediatric cases accounting for 1% of the total reported.1 Three months later, more than 150 000 cases had been reported across the world, as well as nearly 6000 deaths, based on data from the European Centre for Disease Prevention and Control (ECDC).2
On March 11, 2020, the World Health Organization (WHO) declared this public health emergency a pandemic.3 The quick rise in cases, at the national and international level, compelled the adoption of immediate and potent measures to address the situation. On March 14, the Spanish government declared the state of alarm. The purpose was to establish a series of measures to protect the health and safety of the citizenry, contain the spread of the disease and reinforce the public health system.4 Restrictions were placed on free movement and leisure activities, which severely limited economic activity. Schools were closed and a large part of the population shifted to remote work, with the exception of essential workers.
In the early months of the pandemic, the segment of the population affected the most, based on data of the national epidemiological surveillance network (known as RENAVE),5 was the 50-59 years age group, and 55% of reported cases were in female patients. In the group of patients that required hospitalization, 55% were male and 21% were aged 70-79 years.6 Children were not as affected as adults, but were as likely to acquire the infection, which could be explained by the fact that most infections in the paediatric age group were mild or asymptomatic, so that in many cases they did not require medical attention.1,7,8 However, cases of severe disease associated with SARS-CoV-2 have also been described in children.9-11
The SARS-CoV-2 seroprevalence study conducted in Spain between April and May of 2020 (ENE-COVID)12 found a mean seroprevalence of 5%. The city of Madrid, where our study took place, had one of the highest, exceeding 10%. The seroprevalence in children aged less than 10 years was less than 3.1%.
In this epidemiological context, our national health system had to adjust and respond to this public health emergency. The Spanish public health authorities, with the support of scientific societies and expert groups, published a variety of documents detailing the strategies for the management and followup of patients with COVID-19.13-15
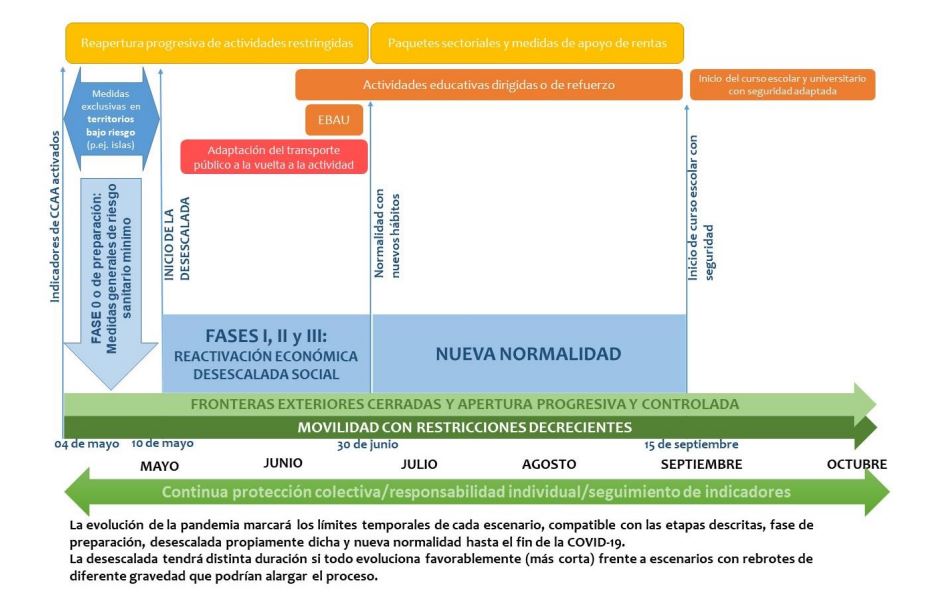
From May 2020, the number of cases and hospital occupancy rates, which had reached saturation, started to wane, with a visible flattening of the epidemic curve. The government started a stepwise reopening after imposing a strict lockdown toward the gradual recovery of what has been referred to as "the new normal"16 (Figure 1).
| Figure 1. Proposed timeline for the transition to the “new normal”. Ministry of Health of Spain |
|---|
 |

The reopening advanced gradually during June, when measures still needed to be applied to fight the pandemic and prevent a new spike in cases. These measures affected every segment of society and not only the health care field, changing lifestyle habits and interpersonal interaction patterns. In health care settings, there was a gradual return to normal activity, but it was still necessary to maintain safe care pathways, adhering to a series of standards established based on the experience had and the lessons learned (Table 1).
| Table 1. Reopening: Standards for health care delivery in primary care centres |
|---|
|

OBJECTIVES
The purpose of the study was to describe paediatric care delivery in our primary care centre in the early stages of reopening, chiefly aiming to establish how appointments were being implemented, the modalities of care offered (in person vs remote), the profile of patients that demanded and received care and the degree to which the reasons for consultation were addressed successfully.
MATERIAL AND METHODS
We conducted a retrospective, observational and descriptive study based on the health records of patients managed in the department of paediatrics of the Goya primary care centre (Madrid, Spain) in June 2020. This facility is located in the centre of the city. It serves a catchment population of 59 289 inhabitants, including 6545 children aged 0 to 14 years and 11 months (Table 2).
| Table 2. Data on the consultations managed by the Goya primary care centre (Madrid, Spain) | |||
|---|---|---|---|
| Paediatric age group | Paediatricians on staff | Type of consultation | |
| 0-2 years | 1176 | 2 paediatricians in morning shift | Paediatrician 1: COVID-related Paediatrician 2: not COVID-related |
| 3-6 years | 1736 | ||
| 7-13 years | 3195 | 2 paediatricians in afternoon shift | Paediatrician 1: COVID-related Paediatrician 2: not COVID-related |
| 14 years | 438 | ||
| Total | 6545 | 4 paediatricians | |

The inclusion criteria were: age ≤14 years, having received services from the centre, either in person or by telephone, in the period under study. Patients that had scheduled appointments but did not attend were included in the analysis of demographic characteristics but excluded from the rest of the analyses.
We collected demographic data on age and sex for all patients that sought health care services. Subsequently, we collected data on health care services that were initially scheduled and the care that was actually delivered by health care providers.
After excluding patients that did not attend the clinic or answer the scheduled phone call (a minimum of 2 attempts were made), we classified the reasons for consultation codified as numbers to facilitate the subsequent analysis (Table 3). We also collected data on activities carried out at the centre, such as the fulfilment of the routine vaccination schedule, performance of diagnostic tests, performance of polymerase chain reaction (PCR) tests for detection of coronavirus or referral to hospital-based care. We divided other diseases into the following categories: gastrointestinal, ear-nose-throat (ENT), genitourinary, ophthalmologic, neurologic, psychiatric, dental and miscellaneous.
| Table 3. Results. Categories of reasons for consultation that were managed (and their frequency) | |||||
|---|---|---|---|---|---|
| Category | n | Telephone | In-person | Electronic mail | |
| 1 | Suspected COVID-19 (PCR, 28.6%) | 175 | 111 (63.4%) | 64 (36.6%) | |
| 2 | Asthma and allergy | 72 | 48 (66.7%) | 24 (33.3%) | |
| 3 | Dermatology | 164 | 83 (50.6%) | 75 (45.7%) | 6 (3.7%) |
| 4 | Infant and child care | 60 | 42 (70%) | 18 (30%) | |
| 5 | Social problem | 14 | 11 (78.6%) | 3 (21.4%) | |
| 6 | HCP (vaccination, 47.24%) | 297 | 9 (3%) | 288 (97%) | |
| 7 | Administrative | 158 | 95 (60.1%) | 60 (38%) | 3 (1.9%) |
| 8 | Test results | 42 | 37 (88.1%) | 5 (11.9%) | |
| 9 | Other diseases | 286 | 151 (52.8%) | 135 (47.2%) | |

We retrieved the necessary data from the primary care electronic health records database of Madrid. We used an Excel Microsoft Office spreadsheet to organise the data. Later, the data were exported to the XLSTAT2020 statistical software for analysis. We conducted a descriptive analysis of the variables. For quantitative variables, we summarised the data with measures of central tendency (median and range, as the mean and standard deviation would have been affected substantially by outliers, except in the description of the total number of patients). We summarised qualitative data as absolute frequencies and percentages.
RESULTS
In the period under study, the primary care centre provided services to 1321 patients. Of this total, 640 were female (48.5%) and 681 male (51.5%). The median age was 4 years (range, 3 days-15 years).
There were no salient differences in visit volume during the month, with a mean of 60 patients managed each day between the 4 paediatricians. If we compare this to the mean volume in the same period in 2019, there was a 34% decrease.
Of the total appointments, 49% (648) were in-person and 51% (582) remote. Of all in-person visits, 268 corresponded to Healthy Child Programme (HCP) visits, and 380 to other medical concerns. When it came to remote consultations, 571 were conducted by telephone and 11 by electronic mail. There were 73 patients that did not answer the phone. Of all telephone appointments, 461 (80.7%) had been requested by the patient and 110 (19.3%) were suggested by the provider.
As concerns the agreement between the type of appointment scheduled (in person/telephone/electronic mail) and the type of appointment that actually took place, the initial plan was maintained most frequently in the case of telephone appointments, with an agreement of 63.6%, followed by HCP visits (60%), while planned in-person visits were ultimately conducted in person in only 47.6% of cases.
When we analysed the reasons for consultation (Table 3), we found most of the appointments were for services in the framework of the HCP (23.4% of the total). The second most frequent type were appointments for patients that reported symptoms compatible with the features of SARS-CoV-2 described in the literature (13.8%): fever, cough and/or respiratory distress, headache, sore throat, diarrhoea, myalgia, cutaneous lesions and, less frequently, loss of smell and taste. In this group, a PCR test was performed for diagnosis in 28.6% of cases. The next most frequent presenting complaint category was dermatologic (12.9%), followed by consultations for asthma or allergic disease (5.7%). The consultations for administrative issues amounted to 158, or 12.5% of the total. The consultations for diseases other than COVID-19, in decreasing order of frequency, concerned gastrointestinal, ENT, genitourinary, ophthalmologic, neurologic and psychiatric/mental health disorders and traumatic injury.
Sixty-nine patients were referred to hospital (5.2% of managed patients). In this group, the specialities that patients were referred to most frequently were ophthalmology (40.6%), dermatology (10.1%) and psychiatry (8.7%). Only 1 patient was referred directly to the emergency department, an infant with dehydration in the context of gastroenteritis.
DISCUSSION
The COVID-19 pandemic arrived unexpectedly. The health care authorities of Spain issued recommendations regarding access to health care facilities with the aim of ensuring the safety of both patients and health professionals in care delivery. At the same time, care needed to continue to be provided for other diseases and needs in the population.
During the lockdown, the volume of paediatric visits decreased substantially at the primary care level, as families were confined home, schools were closed and there was widespread fear of contagion. Most primary care centres remained open, establishing triage systems to manage access to the facilities to separate the care pathways of patients with possible SARS-CoV-9 infection and of other patients. Routine appointments were maintained for the care of young infants and to maintain the routine primary vaccination schedule. There was a drastic change in the way care was delivered, seeking telehealth options to provide alternatives in response to the restrictions to in-person care imposed by the COVID-19 pandemic.
Through the month of June, during the reopening, primary care services were meant to resume their normal activity, but measures still needed to be implemented to contain the pandemic and prevent a new rise in cases. The analysis of the activity of our centre during that month revealed that we had managed 34% fewer paediatric visits compared to the same period the year before. On-site activity was gradually resumed with a balance of in-person appointments (49%) and remote consultations (51%). In the analysis of the agreement between the type of appointment scheduled and the type of appointment that actually happened, we found that agreement was lowest, at 47%, for scheduled in-person visits, which can be explained by the fact that telephone calls were made ahead of in-person visits that appeared in the schedule and the reason for consultation was resolved by telephone or electronic mail.
In-person visits were divided into those that provided routine preventive care in the framework of the HCP (42%) and visits for other reasons (58%). Telephonic consultations were the most frequent alternative to in-person visits. Of the former, 19% were proposed by the provider, either to change the type of appointment initially scheduled or for followup of patients. Electronic mail consultations were least frequent, and conducted using the email address of the centre. The content of the messages were mainly images, in addition to submission of documents, reports and test results. These vehicles of consultation, which before the pandemic were rarely used, became a cornerstone of care delivery and were found to be effective and positively perceived by families and health professionals, allowing the development of rapport and a rapid response.
In the analysis of the reasons for consultation, we found that the bulk corresponded to HCP services. Particular efforts were made to review vaccination schedule and reach out to catch up with the administration of vaccines that were missed in the preceding period, as the data at the time evinced a clear decrease in vaccination coverage in the early months of the pandemic. 17,18
As regards consultations related with possible COVID, which were second in frequency, we ought to note that in the first wave of the pandemic, when community-based transmission was at play, diagnostic tests to detect acute infection were not available for the general population without risk factors at the primary care level. In the period under study, the protocols restricted indication of these tests to patients in who SARS-CoV-2 infection was strongly suspected.19 These posed a challenge, as many infections in paediatric patients share a constellation of symptoms with COVID-19, thereby complicating diagnosis. Epidemiological and clinical severity criteria were applied.20 At the time, the only test available was the PCR test for detection of SARS-CoV-2 in a nasopharyngeal secretion sample. The proportion of patients in which PCR was performed, of 28.8%, may seem low, but it is justified because in many cases the reported symptoms at the time of scheduling were not consistent with the symptoms reported in the actual in-person assessment or had resolved by the time of the visit, or a different diagnosis was given that better fit the presentation after the assessment, all of it combined with an epidemiological context in which the number of cases was declining, and therefore so was the probability of transmission.
Aside from COVID-19, the most frequent presenting complaints were dermatologic problems and asthma and allergy-related complaints (it is important to remember that the study was conducted in the month of June). However, the burden of asthma and allergy was lower compared to previous seasons. Clearly, the confinement and the preventive measures implemented in the pandemic (handwashing, masks) had an effect.
When it came to referrals to hospital, a total of 5.2% of the patients were referred, chiefly to outpatient ophthalmology, dermatology and psychiatry clinics, with the latter speciality accounting for 8.7% of referrals. When we reviewed a study conducted in our centre in 2008 to compare the pattern of referrals to hospital-based care,21 we found that the 2 most frequent specialities were the same, but that the third most frequent at the time had been the trauma clinic, while psychiatry was included in a miscellaneous group that included the specialities to which patients were referred least frequently. Although time has passed since, and the awareness and management of mental health problems has grown at the primary care level, we did notice a substantial increase in the months of the pandemic in the frequency of consultation for anxiety disorders, sleep problems, behavioural changes and disruptions to everyday life, especially in children with existing diagnosis of attention-deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and eating disorders.
Table 3, where we analyse the reasons for consultation and present the implemented model of care delivery, shows that electronic mail was used for consultations regarding dermatological complaints and for administrative tasks. Most consultations regarding infant and child care, social problems, administrative issues and for reporting of test results were managed remotely. Overall, these consultations amounted to 274, or 20.7% of the total. We think this is an important finding, and believe that the care pathways established in our centre and the scheduling of health care professionals should be adapted to include this modality of care delivery to maximise efficiency and resolution of the need leading to consultation.
The pandemic caused by SARS-CoV-2 has changed the way we live and deliver services at the primary care level. With the aim of establishing safe and efficient care pathways, facilities managed the health care demands of the population directly, assessing from first contact the reason for consultation and the potential severity. This results in targeted care delivery from first contact, an approach that we consider desirable not only for COVID-19 but for any instance of health care demand. To implement it, health care facilities needed to adapt both at the physical and organizational levels, especially primary care centres, to which access has been traditionally unrestricted and unlimited.
Triaging patients based on the reason for consultation, redefining professional goals and redesigning schedules to make them flexible and adaptable are some of the strategies that have been implemented and that should be maintained, as they have demonstrated their relevance for the improved management of the health care demands of our catchment population. In-person visits are essential in our interaction with patients and families, but they can and should coexist with remote care.
Every crisis is an opportunity for change. The health care system in general and the primary care system in particular have reallocated their resources to meet the challenge brought by the COVID-19 pandemic. Our article offers a modest but real contribution in this regard, as remote care became prevalent and could be used to successfully address the reason for consultation. We believe that further advances must be made in this field, incorporating remote tools to help health care professionals meet the needs of our population and achieve improvements allowing the provision of reliable and sustainable primary care fitting the current times.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose. The study did not receive any funding.
ABBREVIATIONS
ADHD: attention-deficit hyperactivity disorder · ASD: autism spectrum disorder · ECDC: European Centre for Disease Prevention and Control · ENT: ear, nose, throat · HCP: Healthy Child Programme · PC: primary care · PCR: polymerase chain reaction · RENAVE: Red Nacional de Vigilancia Epidemiológica (National Epidemiological Surveillance Network) · WHO: World Health Organization.
REFERENCES
- Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China. JAMA. 2020;323:1239-42.
- European Centre for Disease Prevention and Control. An agency of the European Union. In: EDCD [online] [accessed 21/03/2022] Available at www.ecdc.europa.eu/en/covid-19-pandemic
- World Health Organization. Brote de enfermedad por coronavirus COVID-19). In: WHO [online] [accessed 21/03/2022] Available at www.who.int/es/emergencies/diseases/novel-coronavirus-2019
- Real Decreto 463/2020, de 14 de marzo. Declaración Estado alarma. In: Boletín Oficial del Estado [online] [accessed 21/03/2022] Available at www.boe.es/buscar/doc.php?id=BOE-A-2020-3692
- Red Nacional de Vigilancia Epidemiológica (RENAVE). In: Centro Nacional de Epidemiología [online] [accessed 21/03/2022] Available at https://cnecovid.isciii.es/
- Centro de Coordinación de Alertas y Emergencias Sanitarias. Información Científica-Técnica. Enfermedad por coronavirus, COVID-19. In: Ministerio de Sanidad [online] [accessed 21/03/2022] Available at www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/ITCoronavirus.pdf
- Mehta NS, Mytton OT, Mullins EWS, Fowler TA, Falconer CL, Murhpy OB, et al. SARS-CoV-2 (COVID-19): What Do We Know About Children? A Systematic Review. Clin Infect Dis. 2020; 71: 2469–79.
- Medeiros GC, Nunes AC, Azevedo KP, Segundo VH, Santos GM, Mata AN, et al. The Control and Prevention of COVID-19 Transmission In Children: A Protocol For Systematic Review And Meta-Analysis. Medicine 2020;99:e21393.
- Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF, et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med. 2020;383:334-46.
- García A, Antón J, Martínez-Pajares JD, Giralt G, Gómez B, Tagarro A et al. Documento español de consenso sobre diagnóstico, estabilización y tratamiento del síndrome inflamatorio multisistémico pediátrico vinculado a SARS-CoV-2 (SIM-PedS). An Pediatr. 2021; 94: 116.e1-e11.
- Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, Perlini S, et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review. JAMA Pediatr. 2020;174:882-9.
- Pollán M, Pérez-Gómez B, Pastor-Barriuso R, Oteo J, Hernán MA, Pérez-Olmeda M, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396:535-44.
- Ministerio de Sanidad. Información por nuevo coronavirus, COVID-19. In: Ministerio de Sanidad, Consumo y Bienestar Social [online] [accessed 21/03/2022] Available at www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/home.htm
- Comunicados COVID-19. Normativa y notas de prensa. Repositorio histórico de informes diarios de datos 2020. In: Comunidad de Madrid [online] [accessed 21/03/2022] Available at www.comunidad.madrid/servicios/salud/comunicados-covid-19-normativa-notas-prensa
- Comunidad de Madrid. Coronavirus. In: Comunidad de Madrid [online] [accessed 21/03/2022] Available at www.comunidad.madrid/servicios/salud/coronavirus
- Plan para la transición hacia una nueva normalidad. In: Ministerio de Sanidad [online] [accessed 21/03/2022] Available at www.lamoncloa.gob.es/consejodeministros/resumenes/Documents/2020/PlanTransicionNuevaNormalidad.pdf
- Moraga FA, Fernández M, Grande AM, Martínez LI, Moreno D, Pérez JJ. Recuperando las coberturas vacunales perdidas en la pandemia COVID-19. Vacunas. 2020;21:129-35.
- Comité Asesor de Vacunas de la AEP. Objetivo: Recuperar las vacunaciones perdidas por la pandemia de COVID-19. In: Vacunas AEP [online] [accessed 21/03/2022] Available at https://vacunasaep.org/profesionales/noticias/vacunaciones-demoradas-COVID-19-recuperacion
- Documento Técnico. Manejo en Atención primaria y domiciliaria del COVID-19. In: Ministerio de Sanidad AEP [online] [accessed 21/03/2022] Available at www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Manejo_primaria.pdf
- Documento de manejo clínico del paciente pediátrico y pacientes de riesgo con infección por SARS-CoV-2. In: Asociación Española de Pediatría [online] [accessed 21/03/2022] Available at www.aeped.es/noticias/documento-manejo-clinico-paciente-pediatrico-y-pacientes-riesgo-con-infeccion-por-sars-cov2
- Martín Y, Caruana l, Gallego MS, Ruiz S. Derivaciones a especializada desde una consulta de pediatría de atención primaria. Comunicación oral, 57 Congreso de la Asociación Española de Pediatría. An Pediatr. 2008;68:1-378.






