Pneumomediastinum in paediatrics: experience in a tertiary hospital
Patricia Fernández Garcíaa, Cristina González Menchéna, José Tomás Ramos Amadora
aServicio de Pediatría. Hospital Universitario Clínico San Carlos. Madrid. España.
Correspondence: P Fernández . E-mail: pfernandezgarcia2@salud.madrid.org
Reference of this article: Fernández García P, González Menchén C, Ramos Amador JT. Pneumomediastinum in paediatrics: experience in a tertiary hospital. Rev Pediatr Aten Primaria. 2022;24:e37-e44.
Published in Internet: 20-01-2022 - Visits: 18713
Abstract
Introduction: pneumomediastinum is defined as the presence of air inside the mediastinum. It is infrequent beyond the neonatal period and typically occurs in male youth with a slender build.
Material and methods: we conducted a descriptive study of a case series with retrospective data collection in the 2009-2016 period and prospective collection in 2016-2019. We included all patients aged 6 months to 18 years given a diagnosis of pneumomediastinum in our hospital. The total sample included 8 patients, and we analysed epidemiological, clinical, diagnostic and therapeutic variables.
Results: 87% of the patients received a diagnosis of spontaneous pneumomediastinum, and there were predisposing factors in 37% of them, such as substance use, air travel, Valsalva manoeuvres or infection. The most frequent reason for seeking care was chest pain (75%), followed by dyspnoea (37%), palpitations and fever (12.5%). The most prevalent sign in the physical examination was subcutaneous emphysema (37%) followed by Hamman’s sign (12.5%). The diagnosis was based on the clinical manifestations and imaging features. All cases were confirmed by chest radiography and only 1 required CT for confirmation. None of the patients required respiratory support, and the average length of stay was approximately 2 days.
Conclusions: pneumomediastinum is usually a benign and self-limited condition. Despite its low incidence, it should be included in the differential diagnosis of chest pain due to its potential severity, as it can spread to subcutaneous, endothoracic, peritoneal or spinal tissue.
Keywords
● Chest pain ● Dyspnea ● Hamman ● Pneumomediastinum ● Young menINTRODUCTION
Spontaneous pneumomediastinum is an infrequent disease, usually benign and self-limiting, that generally happens in young and thin male individuals. Its actual incidence is unknown and difficult to quantify, as it can manifest in subclinical forms and many patients do not seek medical care for it. It is important, however, on account of its potential severity, as it can spread to the subcutaneous, endothoracic, peritoneal or intrathecal spaces, becoming a medical emergency.
There are potential predisposing factors, such as a history of pulmonary disease (asthma, cystic fibrosis or infection), Valsalva manoeuvres (cough, recurrent vomiting or physical exertion) or drug inhalation.
The typical clinical presentation is the triad of retrosternal chest pain, dyspnoea and subcutaneous emphysema. Chest pain is usually oppressive, intense, of abrupt onset and variable duration, worsening with deep inspiration and possibly radiating to the left upper extremity, neck and back. Hamman’s sign is very characteristic, but not commonly present, and consists of a crunching, rasping sound synchronous with the heart beat heard upon auscultation.1
The diagnosis is based on clinical manifestations and imaging features, mainly in the chest radiograph. Computed tomography (CT) is the gold standard but is only indicated if there is strong suspicion of pneumomediastinum in a patient with a normal chest radiograph, and an oesophagogram is only indicated if there is suspicion of oesophageal rupture.
The most frequent findings in the chest radiograph that allow diagnosis of pneumomediastinum are2-4:
- Ring around artery sign. In the lateral chest radiograph, presence of a circular radiolucency surrounding the right pulmonary artery and aortic root caused by mediastinal air.
- Continuous diaphragm sign. In the posteroanterior (PA) chest radiograph, the band of gas borders the upper portion of the diaphragm that is immediately inferior to the heart. Under normal conditions, the boundary between heart and diaphragm cannot be distinguished (cardiac silhouette), but in pneumomediastinum, due to the presence of air between the pericardium and diaphragm, both structures appear outlined.
- Visible pleura. In the PA chest radiograph, presence of a hyperlucent band parallel to the heart corresponding to the air separating the pleura and pericardium and outlined by a radiodense line corresponding to the separated pleura.
- Thymic sail sign, angel wing sign or spinnaker sign. In the PA chest radiograph, mediastinal air displaces the thymus to the upper portion of the image, so that it is separated from the cardiac silhouette. It is a typical sign of pneumomediastinum in neonates that usually results from cardiopulmonary resuscitation (CPR) manoeuvres or mechanical ventilation.
- Naclerio V sign. In the PA chest radiograph, it appears as hypodense lines that form a shape resembling a V in the left lower and lateral margins of the mediastinum. The medial (vertical) limb of the V is produced by mediastinal air between the descending aorta and the left hemidiaphragm, while the lateral (horizontal) limb is produced gas between the parietal pleura and left hemidiaphragm. It is associated with pneumomediastinum secondary to oesophageal rupture.
- Pneumopericardium. In the PA chest radiograph, presence of a hyperlucent area running parallel to the heart, usually surrounding the entire cardiac silhouette, outlined by a radiodense band corresponding to the parietal pericardium.
- Subcutaneous emphysema. In the PA chest radiograph, air collection in the soft tissue of the chest wall.
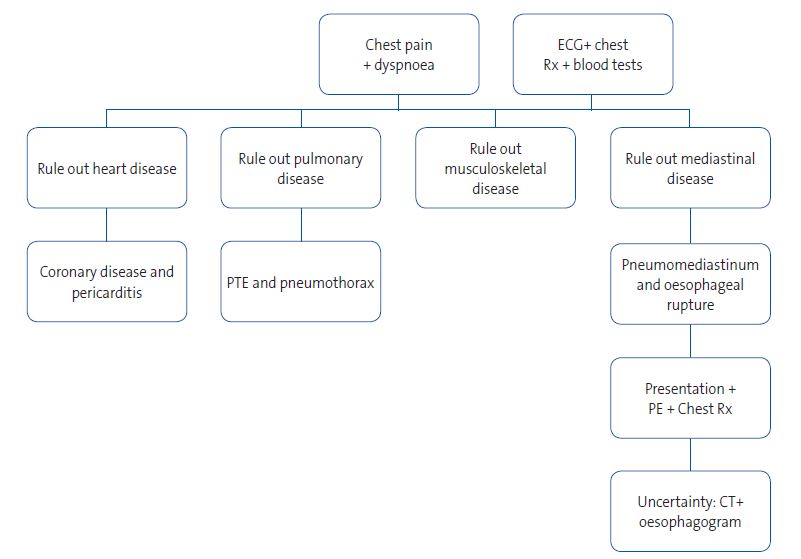
The differential diagnosis includes acute coronary syndrome, pneumothorax, pulmonary thromboembolism, pericarditis, spontaneous oesophageal perforation and rib fracture, among others (Figure 1).5
| Figure 1. Algorithm for differential diagnosis of acute chest pain |
|---|
 |

The treatment is symptomatic, with analgesia, oxygen therapy and rest and avoidance of situations that could promote barotrauma (Valsalva manoeuvres, diving or flying). The prognosis is generally good, with resolution in 2 to 15 days; complications and recurrence are rare. It does not usually require surgical treatment except in particular circumstances (such as pneumothorax, necrotising mediastinitis or underlying disease).
Our objective is to describe the characteristics of pneumomediastinum in the paediatric population and share our experience in the diagnosis and management of these patients.
MATERIAL AND METHODS
We conducted a descriptive study with retrospective data collection for cases between January 2009 and October 2016 followed by prospective inclusion of patients through September 1, 2019. We included every patient aged 6 months to 18 years given a diagnosis of pneumomediastinum in our hospital. We reviewed health records and analysed epidemiological, clinical, diagnostic and therapeutic variables with the statistical software IBM SPSS Statistics version 23. The series included a total of 8 patients.
Case 1
Male adolescent aged 16 years who presented to the emergency department with precordial pain with onset 4 hours prior. The pain was of moderate intensity (6-7/10), did not radiate and increased with deep inspiration. The patient had consumed a vegetarian diet for the past 9 months. As risk factors, the patient reported having consumed alcohol, tobacco and cannabis and experienced severe vomiting after their consumption in the 2 days preceding the emergency visit during a party in a rural resort. He reported that there was no history of cardiovascular disease in the family and no relevant personal medical or surgical history.
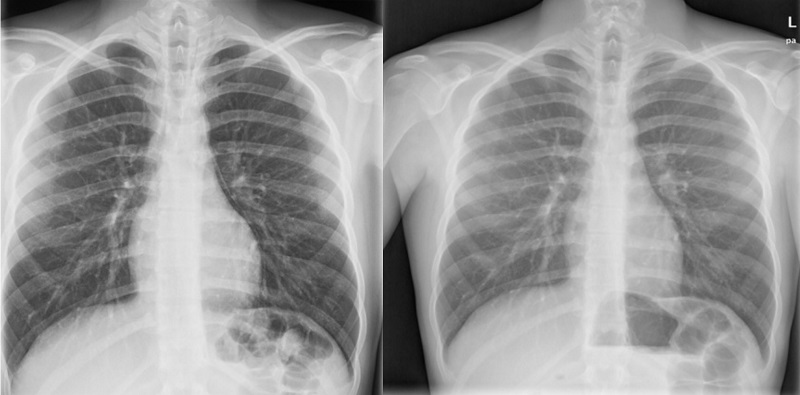
The vital signs and physical examination were normal, with the exception of a crepitations synchronous with the heartbeat upon auscultation (Hamman sign). The patient was evaluated with an electrocardiogram (ECG), chest radiograph, blood tests and a transthoracic echocardiogram. The ECG revealed a sinus rhythm of 68 bpm, a normal axis, the corrected QT interval of 0.38 and an early repolarization pattern. The chest radiograph revealed space between the parietal pleura and the pericardium at the left heart border (Figure 2). The complete blood count, chemistry panel, cardiac enzymes and coagulation tests were normal, echocardiogram with normal biventricular function, without chamber hypertrophy and no signs of cardiac tamponade.
| Figure 2. Case 1. Male adolescent aged 16 years who presented to the emergency department with precordial pain with onset 4 hours prior. Chest radiograph with separation of the parietal pleura from the pericardium in the left border of the heart (left image) and normal follow-up radiograph (right image) |
|---|
 |

The patient was hospitalized for 3 days and only required analgesia, with full resolution of symptoms and normal features in follow-up evaluations.
Case 2
Female adolescent aged 15 years that presented to the emergency department with sudden-onset central chest pain that radiated to the shoulder blades and associated with dyspnoea. She reported cold symptoms in the previous days, but no cough, Valsalva manoeuvres, substance use, menstruation at the time of the visit or vigorous physical activity. There was no relevant personal or family history of cardiovascular disease. In the physical examination, the vital signs were normal and there was no subcutaneous crepitation at the cervical level
The evaluation included blood gas analysis, an ECG and a chest radiograph. The results of blood gas analysis and the ECG were normal. The chest radiograph confirmed the presence of subcutaneous emphysema in the right cervical region and bilateral mediastinal gas with outlining of the left heart border.
The pain resolved within 24 hours with the prescribed analgesia and the patient was discharged in 2 days, after which she did not experience recurrences.
Case 3
Male adolescent aged 13 years who presented with oppressive chest pain and palpitations following an argument with his mother. He visited the emergency department and received an initial diagnosis of panic attack after performance of imaging and an ECG, but he returned to the emergency department 48 hours later after being told by telephone of a radiographic feature that had gone unnoticed before. The patient had no relevant personal or family history.
The physical examination was normal and the vital signs in the normal range. There were no abnormalities in the ECG, and the chest radiograph showed elongated shapes with air density in the superior mediastinum associated with the continuous diaphragm sign. The patient was managed at the outpatient level and the problem resolved fully and without recurrence.
Case 4
Male adolescent aged 16 years who presented to the emergency department with central chest pain with onset 10 hours prior after a flight from the United States to Spain. The pain worsened with inspiration and movement, but did not radiate. There were no vasovagal symptoms, previous infection or relevant personal medical or surgical history. The vital signs and the findings of the physical examination and ECG were perfectly normal. The radiographic features were compatible with pneumomediastinum and bilateral subcutaneous emphysema cervical bilateral.
The patient was admitted for 48 hours, with complete resolution of symptoms and without recurrence during the patient’s stay in Spain, after which we were unable to continue the followup.
Case 5
Male adolescent aged 13 years referred to the emergency department by his primary care paediatrician for evaluation of right cervical and central chest pain of 5 hours’ duration associated with dyspnoea and difficulty swallowing. The patient reported abrupt onset of pain that had worsened gradually, without radiation, and more severe in the cervical region. The patient denied having had any traumatic injury, infection, recent intake of fish or other symptoms. The personal history was unremarkable. There was no family history of heart disease, arrythmias, sudden death or hearing loss. The maternal grandparents died of acute myocardial infarction at age 49 and past age 60 years.
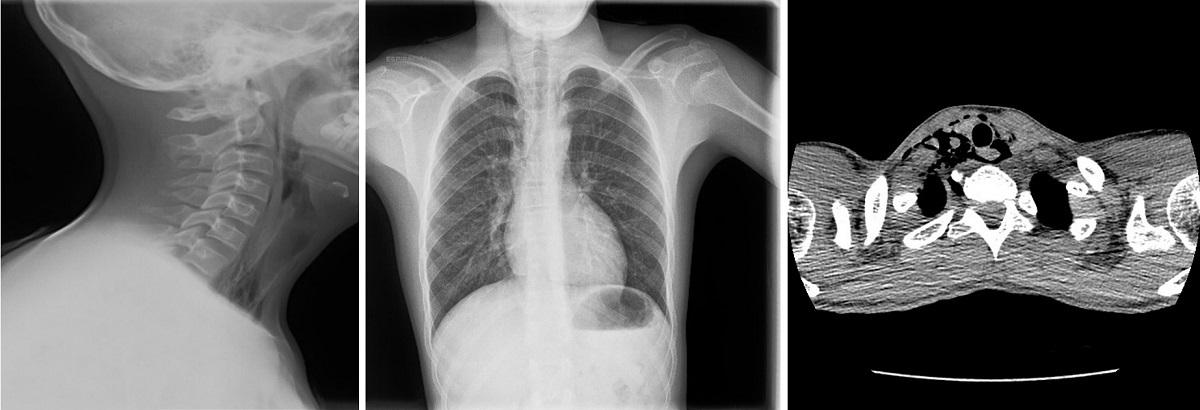
The vital signs were in the normal range. There was subcutaneous emphysema in the right submandibular area. The rest of the physical examination was normal. In the soft-tissue neck and chest radiographs, there were hyperlucent areas in the right superior mediastinum associated with the continuous diaphragm sign and subcutaneous emphysema in the right side of the neck. A neck and chest CT scan revealed anterior, medial and posterior pneumomediastinum extending cranially into the soft tissues surrounding the trachea and oesophagus toward the right carotid sheath and the right retropharyngeal space (Figure 3). The findings of the ECG, flexible fibreoptic laryngoscopy examination and blood tests were normal. The patient remained in hospital for 3 days under continuous vital sign monitoring and did not require active treatment at any point. He was evaluated in the paediatric cardiology and paediatric pulmonology departments, and there were no significant findings or events and no recurrences.
| Figure 3. Case 5. Male adolescent aged 13 years referred to the emergency department by his primary care paediatrician for evaluation of right cervical and central chest pain of 5 hours’ duration associated with dyspnoea and difficulty swallowing. Soft-tissue neck and chest radiographs with hyperlucent areas in the right superior mediastinum, continuous diaphragm sign and subcutaneous emphysema in the right side of the neck. Neck and chest CT scan revealed anterior, medial and posterior pneumomediastinum extending cranially into the soft tissues surrounding the trachea and oesophagus toward the right carotid sheath and the right retropharyngeal space |
|---|
 |

Case 6
Female adolescent aged 15 years that presented to the emergency department with severe epigastric pain (7/10) of 24 hours’ duration associated with nausea in the absence of vomiting, diarrhoea or fever. She reported weekly episodes of epigastric pain in the last month. There were no other symptoms. As for the personal history, the patient was born in Santo Domingo and had resided in Spain for one month. She carried a gastrostomy tube that had been placed 3 months prior due to distal oesophageal stenosis secondary to deliberate caustic ingestion. She had no relevant cardiovascular history.
The findings of the physical examination were: vital signs in the normal range, gastrostomy tube carrier, epigastric pain upon deep palpation, with no signs of peritoneal irritation; the rest of the examination was normal.
The patient was admitted for evaluation and treatment. She underwent serial endoscopic balloon oesophageal-pyloric dilations, developing pneumomediastinum with mild mediastinitis as a complication of one of these procedures. The diagnosis was made by chest radiograph, which was indicated on account of onset of fever 24 hours after performance of an upper endoscopy (Figure 4). The illness resolved with intravenous antibiotherapy, and the patient did not require respiratory support, haemodynamic support or drainage. The follow-up evaluations were normal, and there was no recurrence.
| Figure 4. Case 6. Female adolescent aged 15 years that presented to the emergency department with severe epigastric pain of 24 hours’ duration associated with nausea without vomiting, diarrhoea or fever. The diagnosis was made by chest radiograph, which was indicated on account of onset of fever 24 hours after performance of an upper endoscopy |
|---|
 |

The pneumomediastinum resolved completely within 5 days, but the patient remained hospitalised for 45 days for management of the underlying disease.
Case 7
Male adolescent aged 16 years transferred to our hospital with a diagnosis of pneumomediastinum with subcutaneous emphysema. The patient reported retrosternal pain that worsened with deep inspiration with onset 24 hours prior. The patient had no cough, cold symptoms, asthma, previous episodes of choking or Valsalva manoeuvres. He was transferred from a private hospital to our hospital, as his insurance policy did not cover performance of additional diagnostic tests or therapeutic trials. He had a history of spontaneous pneumothorax at birth.
The vital signs were normal. There was subcutaneous emphysema in the right supraclavicular region. The patient had a marfanoid phenotype with pectus excavatum. The chest radiograph revealed pneumomediastinum, with a visible pleura and supraclavicular subcutaneous emphysema.
The patient was admitted for 24 hours, and a follow-up visit was scheduled for 48 hours post discharge, which he did not attend. There was no subsequent followup, as the patient had been in Spain on vacation.
Case 8
Male adolescent aged 17 years who presented to the emergency room with cough producing a greenish phlegm of several days’ duration associated with dyspnoea in the past 24 hours. The patient felt he had a temperature but had not measured it with a thermometer. No other symptoms reported. He had a history of hay fever.
The vital signs were in the normal range. The lung sounds were compatible with bronchospasm. The findings of the chest radiograph indicated the presence of pneumomediastinum and right supraclavicular emphysema.
The patient was admitted for 24 hours, during which he did not require respiratory or haemodynamic support. There were no abnormal findings in subsequent follow-up evaluations.
RESULTS
We identified 8 patients for the 2009-2019 period under study. Of this total, 6 were male and 2 female, and the median age was 15.5 years (range: 12-18 years). Eighty-seven percent of the patients (n = 7) received a diagnosis of spontaneous pneumomediastinum, and 12.5% (n = 1) of traumatic pneumomediastinum secondary to performance of upper endoscopy. In the spontaneous pneumomediastinum group, predisposing factors were identified in 37% of patients, including substance use, a recent flight, Valsalva manoeuvres and infection. None of the patients had asthma or smoked, and none had a relevant personal or family history of cardiovascular disease.
Chest pain was the most frequent reason for seeking care, reported by 75% of the patients (n = 6), present in 71% (n = 5) of patients with spontaneous pneumomediastinum and in the sole patient with pneumomediastinum secondary to trauma. The second most frequent symptom was dyspnoea, present in 37% of patients (n = 3), followed by palpitations (12.5%; n = 1) and fever (12.5%; n = 1/8). The fever was secondary to mediastinitis secondary to iatrogenic oesophageal rupture. All patients sought care within 24 horas of the onset of symptoms.
In the physical examination, the most prevalent sign was subcutaneous emphysema, detected in 37% of the cases (n = 3), followed by the sign of Hamman (12.5%; n = 1).
The diagnosis was based on the clinical manifestations and imaging features. All cases were confirmed by chest radiography, with visualization of mediastinal gas associated with subcutaneous emphysema in 75% of patients (n = 6). An ECG was performed in 62.5% of patients (n = 5), with no abnormal findings in any. A confirmatory CT scan was performed in 12.5% of patients (n = 1). None required performance of an oesophagogram.
Eighty-seven percent of the patients required admission. All were managed with rest and analgesia. During the stay, they remained stable without need of respiratory or haemodynamic support. None needed admission to the intensive care unit (ICU) or surgery.
The mean length of stay was 2.1 days (range: 1-5). The median duration of followup was 3 years (range: 2 months to 10 years). After discharge, all patients had favourable outcomes, with no complications or recurrences observed during the followup.
DISCUSSION
Pneumomediastinum is an infrequent disease that accounts for 1 in 10 000 to 40 000 emergency visits, with an incidence of 1/22 800 in our hospital. As for the age at which it develops, there are 2 incidence peaks: early childhood, due to respiratory infections, and adolescence, with a higher frequency in male adolescents with a slender build.6,7 We ought to highlight the increase in frequency in neonates due to the use of mechanical ventilation and CPR manoeuvres in the ICU.8-10 In our sample, the lack of documentation of cases of neonatal pneumomediastinum and the probably low frequency of visits emergency departments for pneumomediastinum resulted in a small number of cases in the analysis.
It is important to consider potential predisposing factors in the case of spontaneous pneumomediastinum (pulmonary disease, Valsalva manoeuvres or exposure to toxic substances), and iatrogenesis (endoscopy, mechanical ventilation) in the case of traumatic pneumomediastinum.11-13 In our case series, we identified these factors in 4 patients: Valsalva manoeuvres, air travel, consumption of toxic substances and history of upper endoscopy.
We found a predominance of male adolescents, none of whom experienced recurrence, and when it came to the clinical manifestations, the most frequent one was chest pain, followed by dyspnoea, palpitations and fever. All of the above was consistent with the previous medical literature.
Usually, the diagnosis can be made based on the clinical presentation and the findings of chest radiography. However, a CT scan may be necessary if there is strong suspicion despite normal radiographic features, or an oesophagogram, if oesophageal rupture is suspected. In our study, a CT scan was only performed in 1 patient to rule out underlying lung disease, and the oesophagogram was not necessary in any case.
The initial management is conservative, and chest drainage is only required in the case of massive or tension pneumomediastinum. In our experience, conservative management sufficed, without need of respiratory support and with spontaneous resolution of the pneumomediastinum in 2 to 3 days. Some hospitals use oxygen therapy to promote gas reabsorption, although this is not necessary if the patient maintains adequate oxygenation.
Pneumomediastinum is a usually benign and self-limiting disease, but one that must be included in the differential diagnosis of acute chest pain on account of its potential severity.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose in relation to the preparation and publication of this article.
ABBREVIATIONS
CPR: cardiopulmonary resuscitation · CT: computed tomography · ECG: electrocardiogram · ICU: intensive care unit · PA: posteroanterior.
REFERENCES
- Álvarez C, Jadue A, Rojas F, Cerda C, Ramírez M, Cornejo C. Neumomediastino espontáneo (síndrome de Hamman): Una enfermedad benigna mal diagnosticada. Rev Med Chile. 2009;137:1045-50.
- Alishlash AS, Janahi IA. Spontaneous pneumomediastinum in children and adolescents. In: UpToDate [online] [accessed 13/01/2022]. Available at www.uptodate.com/contents/spontaneous-pneumomediastinum-in-children-and-adolescents
- Godoy l, Morilla l, Iramain V, Pavlicich V. Presentación en la Emergencia de un niño con neumomediastino espontáneo. Pediatría (Asunción). 2011;38:49-52.
- Cottani M. Signo de la V de Naclerio. Rev Arg Radiol. 2012;76:263.
- Valdovinos Mahave MC, Melendo Gimeno J, Ruiz Valero F, Juan Belloc S. Niño de dos años con dificultad respiratoria aguda. An Esp Pediatr. 1998;49:641-2.
- Díez R. Neumomediastino espontáneo con neumopericardio. FML Rev Med Fam AP. 2016;20:5.
- Guasch Arriaga I, StaitieGali AM, Quintero Rivera JC, López de Castro P. Neumomediastino espontáneo y secundario no traumático: signos radiológicos. ¿Cómo distinguirlos? SERAM. 2014;S-1148.
- Gerazounis M, Athanassiadi A, Kalantzi N, Moustardas M. Spontaneous pneumomediastinum: a rare benign entity. J Thorac Cardiovasc Surg. 2003;126:774-6.
- Crespo Marcos D, Iglesias Fernández C, Márquez de la Plata l, Panadero Carlavilla E. Neumomediastino espontáneo idiopático: a propósito de un caso. Anales Pediatr (Barc). 2006;64:100-8.
- Navarro E. Álbum de signos radiológicos. Tesis doctoral. In: Universidad de Málaga [online] [accessed 13/01/2021]. Available at www-rayos.medicina.uma.es/Rmf/Tesis/Tesis_Doctoral_Eugenio_Navarro.pdf
- Carzolio Trujillo HA, Navarro Tova F, Padilla Gómez Cl, Hernández Martínez IA. Blunt chest trauma with pneumomediastinum and pneumoperitoneum secondary to Macklin effect. Case report. Cir Cir. 2016;84:409-14.
- De la Mata-Martín M, Galán MJ, Gallego J. Pneumomediastinum and pneumothorax during emergency tracheotomy under spontaneous ventilation: Macklin metes Mueller? Rev Esp Anestesiol Reanim. 2016;63:231-4.
- Santos Montón C, Moreno Flores A, Llorens Salvador R. Síndrome de fuga aérea pulmonar neonatal: factores de riesgo y patrones radiológicos. Rev Esp Pediatr. 2014;70:205-8.





