Vol. 23 - Num. 92
Original Papers
Safety of extracurricular activities in times of pandemic by SARS-CoV-2. Prospective study in paediatric population
Ana Rodríguez Varelaa, Alicia Martínez Sebastiánb, Pedro Dongo Floresb, Carla A. Pérez Paretsc, Beatriz Mansilla Roigb
aServicio de Urgencias de Pediatría. Hospital Universitario Doctor Peset. Valencia. España.
bMIR-Pediatría. Servicio de Pediatría. Hospital Universitario Doctor Peset. Valencia. España.
cMIR-Pediatría. Servicio de Pediatría. Hospital Universitario Doctor Peset . Valencia. España.
Correspondence: A Rodríguez . E-mail: rodriguez_anaval@gva.es
Reference of this article: Rodríguez Varela A, Martínez Sebastián A, Dongo Flores P, Pérez Parets CA, Mansilla Roig B. Safety of extracurricular activities in times of pandemic by SARS-CoV-2. Prospective study in paediatric population. Rev Pediatr Aten Primaria. 2021;23:375-81.
Published in Internet: 15-11-2021 - Visits: 9145
Abstract
Introduction: the coronavirus disease 2019 pandemic has compelled the implementation of various measures to mitigate the impact of an inevitable increase in COVID-19 cases, such as the closure of schools. Upon their reopening, given that physical activity in childhood and adolescence is crucial for optimal development, we considered whether extracurricular athletic activities are safe in the COVID age.
Material and methods: we conducted a longitudinal, observational and descriptive study. We followed up 717 students and instructors from a municipal sports organization that participated in sports activities offered between September and December 2020. When a positive case was identified, the staff contacted the family, filling in the data collection form and monitoring the students.
Results: there was only 1 detected case SARS-CoV-2 infection among the 679 students and 38 adult instructors included in the study. It occurred in an adolescent aged 13 years that played basketball and acquired the infection from a family member and developed mild symptoms; both the boy and the peers in his consistent contact group were quarantined for 10 days without identification of additional cases.
Discussion: our results suggests that if athletic activities are carried out in controlled groups in optimised environments and adhering to health standards, sports facilities can be safe spaces for the paediatric population with a low SARS-CoV-2 transmission rate. We did not identify any outbreaks in the sample, having implemented the appropriate preventive measures and verified strict adherence by the students. Nevertheless, it is important to keep accurate records of current students for contact tracing and to guide the implementation of preventive measures, both general and specific to particular sports activities, with the aim of minimising risk.
Keywords
● Extracurricular ● Pediatrics ● Safety ● SARS-CoV-2 ● SportsINTRODUCTION
The emerging novel coronavirus (SARS-CoV-2) reached Spain as the first case was confirmed in German national on January 31, bringing a significant challenge to the country and signalling the arrival of a public health emergency of international concern.
On September 9, 2020, the date of the start of the study presented here, and based on data from the Ministry of Health and the General Directorate of Public Health of Spain, there were a total of 543 379 cases confirmed by polymerase chain reaction (PCR) or IgM antibody tests in the Spanish territory, of which 29 253 corresponded to the Valencian Community (as of 09/09), which ranked sixth in incidence among the autonomous communities of Spain following Madrid, Catalonia, Andalusia, the Basque Country and Castilla y Leon, with 537 cases requiring hospitalization, while Spain had the highest incidence in Europe second only to Russia.1
This led to the implementation of far-reaching preventive measures including promotion of social distancing, limits on the number of individuals allowed in gatherings, mask mandates and restrictions to the opening hours of non-essential businesses in different autonomous communities. The same preventive measures were promoted and reinforced at the beginning of the school year, which started on September 7 in the Valencian Community. To prevent the transmission and spread of the virus at school and during extracurricular and athletic activities, different measures have been implemented by facilities that work with children and youth, such as measurement of body temperature before the start of the activity, mandatory use of masks in recreational and sport spaces, limiting contacts through the creation of separate groups referred to as “bubbles”, increased ventilation in indoor spaces, closure of shared spaces like changing rooms and showers and frequent handwashing and use of hand sanitizers, among others, which have proven effective in the paediatric population as evinced in the study presented here.
The success achieved in the paediatric population, attributable in large part to the actions just described, was facilitated by the particular characteristics of this collective, as children develop milder forms of disease when infected by coronaviruses, including SAR-CoV-2, as evinced by previous outbreaks, including the severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) epidemics, during which, as is the case now, few cases were reported in children compared to the adult population. Human-to-human transmission usually takes place through the airway (airborne droplets or aerosols, based on recent studies),2 although it can also be transmitted through fomites, such as toys or door knobs, a route that can be minimised through the use of the preventive measures usually implemented in settings where children carry out their activities under the close supervision of instructors.3 Infected children may be asymptomatic or develop fever, dry cough or fatigue; some patients have gastrointestinal symptoms, including abdominal discomfort or pain, nausea, vomiting or diarrhoea. Most have mild symptoms and good outcomes. Generally, children recover within 2 weeks from onset.3 When symptomatic, the proportion of children that transmit the virus is similar to the proportion observed in adults, which is why they cannot attend school or extracurricular activities and need to isolate at home until the infection resolves.4 Despite these measures, outbreaks can happen in schools and be difficult to detect due to the relative absence of symptoms in children.5,6 In our particular case, we did not detect any outbreaks in the sample after implementing the applicable measures in our students and ensuring excellent adherence to them.
We present the results of a study conducted in a sports organization in the Valencian Community, Spain, between September and December 2020, coinciding with the beginning of the academic year, in a sample of students aged 3 to 19 years that engaged in different extracurricular athletic activities under the aforementioned preventive measures, both indoors and outdoors, to determine whether these spaces can be safe for the paediatric population or, on the contrary, are milieus that facilitate transmission of the virus.
MATERIAL AND METHODS
Design: longitudinal observational descriptive study.
Sample: 717 members and instructors of a municipal sports organization (ACDSAB) located in San Antonio de Benagéber, Valencia, involved in any of the athletic activities offered between September and December of 2020.
Methodology: if the appointed COVID manager of the sports centre reported a case, the paediatrician that coordinated the study contacted the family to fill out the data collection form and follow up the student.
The data collection form was organised in 3 sections:
- General information: date case was notified, demographic characteristics of the case (age, sex), sports activity of the student, group the student belonged to, preventive measures implemented during activity.
- Clinical information: presenting symptoms and their duration, diagnostic method used to detect coronavirus (PCR, antigen or antibody test), comorbidities, hospital admission.
- Contact information/tracing: confirmed positive contacts and setting where positive contacts were identified (sports organization, family, school, other), quarantine duration, reinfection.
Contact tracing included household members and contacts in athletic activities and estimation of the date of transmission, with the purpose of assessing the traceability of SARS-CoV-2 infection.
We also assessed other factors, such as the experienced symptoms, their severity and duration, home isolation or hospital admission, and coinfection.
Statistical analysis: the statistical analysis was performed with the software SPSS® Statistics, version 19.0. We have summarised continuous quantitative data as mean and standard deviation, and categorical data as absolute frequency and percentage distributions.
Ethical considerations: before the start of the study, the principal investigator met with the management of the sports centre, which was open to collaboration throughout the project. The legal guardians received a form informing them of the study and requesting consent for participation of the minor, as did students aged more than 12 years, and signed informed consent was obtained prior to participation in the study. We assigned codes to the data for minors and their families safeguarded by the leaders of the project, guaranteeing the confidentiality and anonymity of the data as established by Organic Law 3/2018 on the protection of personal data of December 5. The project was reviewed and approved by the Clinical Research Ethics Committee of the Hospital Universitario Doctor Peset.
RESULTS
The study included 717 individuals (65% male) involved in the activities of the ACDSAB municipal sports organization in San Antonio de Benagéber, Valencia (Spain). Of this total, 679 were students that practiced sports, and 38 were adult instructors.
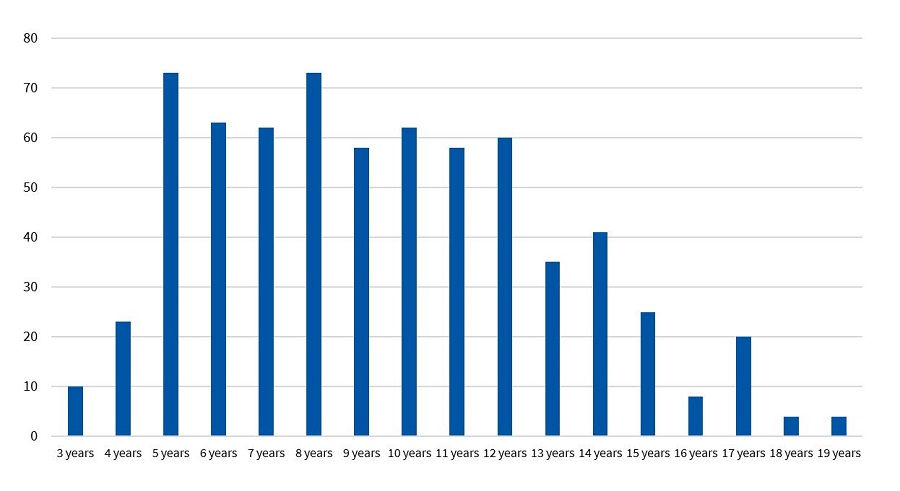
The students were aged 3 to 19 years, and their age distribution is shown in Fig. 1. Of all students, 15.8% were aged less than 5 years, and 29% more than 12 years. The mean age of the students was 9.4 years, and the median 9 years.
When it came to outdoor activities, 33% played soccer, 20% tennis; 17% basketball, 5,2% skating and 2.5% futsal; as for indoor activities, 13% practiced karate; 4.5% capoeira, 3.5% dance and 1.5% multidisciplinary sports.
In the four months of followup (September-December 2020), only 1 case of SARS-CoV-2 infection was detected in the sample. It corresponded to a boy aged 13 years that played basketball and was part of a consistent contact group (CCG) or bubble comprising his team. The source of infection was a relative, and the student developed cough and nasal discharge lasting 24 hours, and anosmia at 4 days from onset. The infection was detected through the rapid antigen test, and the student did not require hospital admission and was isolated for 10 days. The relevant personal history included extrinsic asthma with a favourable course that did not require chronic treatment.
Since the student was part of a CCG, his basketball teammates, who had trained with him 24 hours before the positive coronavirus test, were isolated. The student and his CCG were quarantined for 10 days, and since none of the teammates developed symptoms, performance of additional coronavirus detection tests was not necessary.
The rest of the basketball teams continued training as usual, and the affected group returned to normal activity after the preventive quarantine.
No positive cases were detected among the students practicing all other athletic activities requiring the implementation of preventive measures in peers, either because the criteria for close contact were not met or because the last contact with peers had occurred more than 72 hours prior to the onset of symptoms.
DISCUSSION
The positive case in 1 out of the total of 679 students and 38 instructors in the sample corresponded to an incidence of 1/717 (0.0014) in the 4-month period under study. This suggests that if athletic activities are carried out in “bubbles” under optimised conditions and in adherence with public health measures to contain the spread of the virus, it is possible to achieve a low rate of transmission even in situations in which social distance measures and the use of masks cannot be implemented optimally. Still, further research is required to confirm these results.
The only confirmed case occurred in an adolescent aged 13 years that practiced basketball exclusively. The lack of positive cases among his teammates suggests that the implemented measures were effective. The source of transmission was a relative (the grandfather and father of the student developed symptoms a few days before the patient, and the grandfather had a positive SARS-CoV-2 PCR test). Based on current data, it is likely that a substantial number of new cases are due to transmission within families and interpersonal contact between adults.
The last time the adolescent trained with his team before testing positive for SARS-CoV-2 was 24 hours before obtaining the result, which meant that all members of the CCG were close contacts and required isolation for 10 days per the established public health regulations. During this 10-day period, none of the peers developed symptoms, so none underwent a PCR test, and all returned to their usual athletic activities after the quarantine. It is worth noting that none of the 38 staff tested positive, either.
In relation to the analysis of athletic activities, the general guidelines issued by the Department of Health of the Valencian Community included,7 in addition to general prevention measures, specific measures to implement in the context of extracurricular activities to make them as safe as possible. Some of them highlighted the duty of parents or guardians to check the health status of the child or adolescent before attending the activity, the importance of avoiding crowding on arriving or departing the facilities, the need to ensure adequate ventilation for indoor physical activity and avoid the use of changing rooms and showers, and the need to disinfect sports equipment and the facility. It also stated the need to keep accurate records of current students to allow efficient contact tracing if a positive case were detected. The guidelines also stated the importance of social distancing and limiting physical activities requiring direct contact between students, encouraging individual training routines during most of the activity time even in the case of contact sports. In sports that involve close contact precluding maintenance of an interpersonal distance of at least 1.5 m with a high level of intensity that could make it difficult to train or compete while wearing a mask,8,9 students were organised in CCGs. The students inside each CCG could socialise and play without needing to adhere strictly to the minimum interpersonal distance or wearing a mask. Such groups can include a maximum of 20 students (exceptionally expanded to 25) and their aim is to optimise contact tracing and management of positive cases while allowing interactions that may be unavoidable in the performance of school activities. Academic and non-academic staff that are not part of the CCG but interacts with it should wear masks and maintain the minimum interpersonal distance.10
When it came to the only detected case, the practice of basketball entailed certain particularities, as, while unfolding out of doors, the sport involves regular direct physical contact between players and of all players with the balls used during training and games that cannot be disinfected after each contact. The fact that the virus was not transmitted to any of the peers of the infected adolescent that partook in the extracurricular activity and the lack of positive SARS-CoV-2 cases related to contact during sports practice indicates that the commitment of the staff and, above all, the parents, students and instructors to adhere to the established preventive measures was key, reducing the probability of transmission.
The fact that the rate of transmission was not higher in indoor activities compared to outdoor activities shows that the conclusions also apply to the former, which a priori carry a higher risk (contact sports in indoor spaces), and that it is possible to maintain both physical education classes and extracurricular athletic activities including a variety of sports and some in which interpersonal distance measures are more difficult to implement, as opposed to reducing the range of outdoor athletic activities and sports offered to students.
Lastly, since there was no difference in the rate of transmission in children versus adolescents of different ages, it appears that extracurricular athletic activities can continue in every age group, including younger children, despite the difficulty of ensuring optimal adherence to social distancing measures in young children and that children under 6 years are exempt from wearing a mask.
It ought to be emphasised that this is the case only as long as these activities are carried out under supervision with the strictest possible adherence to general evidence-based health prevention measures introduced to contain the spread of the virus.11 We consider this essential, since physical activity is key during childhood and adolescence for optimal development, decreasing the incidence of prevalent diseases such as obesity, preventing sedentary habits and promoting the development of social skills and values like responsibility and team work. We believe that a broader range of options can improve adherence. However, further research is required to confirm these results, which is very important to guide the practice of extracurricular athletic activities in schools.
Among the limitations of the study, we ought to highlight that at least 1 student tested positive to SARS-CoV-2 and, since the public health authorities determined that the criteria of close contact with peers had not been met in the context of athletic activities (the test was positive more than 48 hours after the last time the student had practiced sports with his teammates) the club was not informed of this positive result and none of the peers that had contact with him were isolated, although we should also note that, in adherence with the established measures, no student with symptoms suggestive of SARS-CoV-2 infection or asked to isolate due to a history of exposure to a positive case attended the extracurricular athletic activities.
CONCLUSION
Based on our findings, the practice of sports can be safe in controlled groups, optimised environments and adhering to preventive measures, without significant differences between outdoor and well-ventilated indoor spaces, in the local paediatric population, in which we found a low rate of transmission of SARS-CoV-2.
We did not identify any outbreaks in our sample, having implemented the applicable preventive measures and verified strict adherence in the children.
Nevertheless, it is important to keep an accurate register of current students so that, should a case be detected, contract tracing can be performed efficiently and general and specific prevention measures for athletic activities can be reinforced in order to minimise risk.
CONFLICT OF INTERESTS
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
CCG: consistent contact group · MERS: Middle East respiratory syndrome · PCR: polymerase chain reaction · SARS: severe acute respiratory syndrome.
ACKNOWLEDGMENTS
We thank the entire staff and management of the ACDSAB municipal sports organization of San Antonio de Benagéber (Valencia, Spain) and the students and their families for their participation in the study.
REFERENCES
- Actualización n.º 203. Enfermedad por el coronavirus (COVID-19) (datos consolidados a las 14:00 horas del 09.09.2020). In: Ministerio de Sanidad [online] [accessed 11/11/2021]. Available at www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_203_COVID-19.pdf
- Paules CI, Marston HD, Fauci AS. Coronavirus infections ‒ More than just the common cold. JAMA. 2020;323:707-8.
- Cao Q, Chen YC, Chen CL, Chiu CH. SARS-CoV-2 infection in children: Transmission dynamics and clinical characteristics. J Formos Med Assoc. 2020;119:670-3.
- COVID-19 in children and the role of school settings in COVID-19 transmisión – Draft Technical Report - 31 July 2020. European Centre for Disease Prevention and Control; 2020.
- Panovska-Griffiths J, Kerr CC, Stuart RM, Mistry D, Klein DJ, Viner RM, et al. Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: a modelling study. Lancet Child Adolesc Health. 2020;4:817-27.
- Medeiros GCBS, Nunes ACF, Azevedo KPM, de Oliveira Segundo VH, Santos GM, Mata ÁNS, et al. The Control and Prevention of COVID-19 Transmission in Children: A Protocol for Systematic Review and Meta-analysis. Medicine (Baltimore). 2020;99:e21393.
- Protocol de mesures de Prevenció i Higiene Sanitària en les Activitats Extraescolars. In: GVA; Conselleria de Sanitat Universal i Salut Pública [online] [accessed 11/11/2021]. Available at https://coronavirus.san.gva.es/documents/469630/873868/Protocolo+Actividades+Extraescolares+Cas.pdf/b445f8c4-dfa4-f650-802f-2876a5d7e948?t=1634302727152
- Davis BA, Tsen LC. Wearing an N95 Respiratory Mask: An Unintended Exercise Benefit? Anesthesiology. 2020;133:684-6.
- Pifarre F, Dulanto D, Grazioli G, de Yzaguirre I, Maura I. COVID-19 and masks in sports. Apunts Sports Med. 2020;55:143-5.
- Actualización del protocolo de protección y prevención frente a la transmisión y contagio del sars-cov-2 para centros educativos que impartan enseñanzas no universitarias en el curso 2020-21. In: GVA; Conselleria d’Educació Cultura i Sport [online] [accessed 11/11/2021]. Available at https://ceice.gva.es/documents/161634256/174782899/Protocolo/927f90ba-7d23-4559-b8bc-9d3ef95898a8
- Chen P, Mao l, Nassis GP, Harmer P, Ainsworth BE, Li F. Returning Chinese school-aged children and adolescents to physical activity in the wake of COVID-19: actions and precautions. J Sport Health Sci. 2020;9:322-4.