Vol. 23 - Num. 89
Original Papers
Oral and dental manifestations of child abuse
Gonzalo Oliván Gonzalvoa, Alejandro Carlos de la Parte Sernab
aPediatra. Servicios de Pediatría y Adolescencia. Instituto Aragonés de Servicios Sociales. Gobierno de Aragón. Zaragoza. España.
bOdontólogo. Facultad de Ciencias de la Salud y del Deporte. Universidad de Zaragoza. Huesca. España.
Correspondence: G Oliván. E-mail: golivang@aragon.es
Reference of this article: Oliván Gonzalvo G, de la Parte Serna AC. Oral and dental manifestations of child abuse. Rev Pediatr Aten Primaria. 2021;23:15-23.
Published in Internet: 23-02-2021 - Visits: 32817
Abstract
Introduction: the objective of the study was to review the oral and dental manifestations of child abuse.
Material and methods: we performed a systematic review study following the PRISMA guidelines. We performed 2 searches using MeSH terms in the Medline/PubMed database for the period ranging from 1/1/2000 to 12/31/2019.
Results: the review included 26 articles, of which 65.4% were published in dental journals and 16% in paediatric journals. All oral and dental injuries caused by physical abuse raise suspicion, but none are pathognomonic. They must be distinguished from unintentional injuries, which are common in the paediatric population. To do so, the presence of physical signs considered strong warning signs must be assessed. All oral and dental diseases resulting from neglect are suggestive but not confirmatory of neglect. Therefore, it is necessary to assess whether there are factors considered necessary to diagnose dental neglect, such as other health problems arising from chronic neglect or other indicators of physical and/or sexual abuse. Oral infections by Neisseria gonorrhoeae or Treponema pallidum are pathognomonic for sexual abuse. All other oral injuries and diseases are considered suspicious or suggestive.
Conclusions: injuries and diseases resulting from child abuse or neglect frequently manifest the oral and intraoral regions. It is essential that paediatricians and dentists be aware of the problem, trained in its detection, and knowledgeable of when and how to document and notify suspected cases. These efforts, as well as the overall work of these professionals, will increase our ability to prevent and detect child maltreatment and to protect and care for children.
Keywords
● Abuse ● Child abuse ● Mouth diseases ● Neglect ● Sexual abuse ● Tooth injuriesINTRODUCTION
Child abuse is an important global public health problem that manifests in all ethnic, cultural and socioeconomic strata. This bane persists despite numerous awareness and education campaigns to alert the general population and health professionals in particular about its incidence, its red flags, the reporting systems and its sequelae.1
In the European Region of the World Health Organization (WHO), it is estimated that each year 22.9% of children aged less than 18 years suffers some form of physical abuse and 9.6% some form of sexual abuse. While these figures are large, it is well known that many cases of child abuse are not reported.2
Children can be subjected to multiple types of abuse and their consequences may manifest in the mouth and oral cavity, so that paediatricians and dentists may be the first clinicians to detect abuse. Thus, they must have the necessary knowledge to be able to identify these signs and address the situation appropriately. We ought to remember that all health providers are mandated to report all cases of suspected child abuse. Prepared health professionals that are aware of the problem are one of the pillars of child protection.3
The aim of our study was to review the evidence on the oral and dental signs of child abuse.
MATERIAL AND METHODS
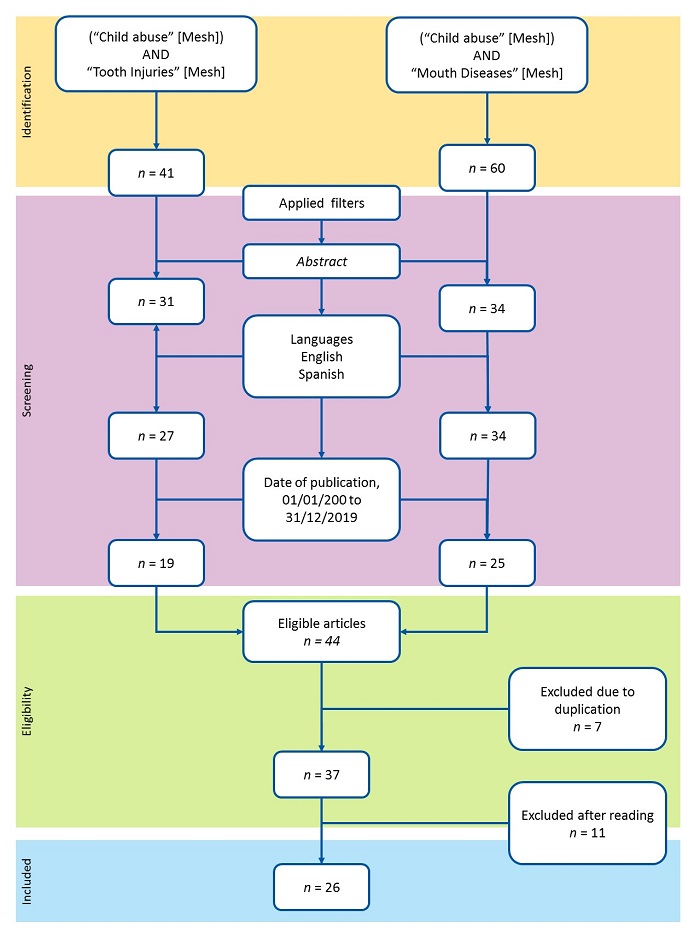
We conducted a systematic review following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).4 We performed 2 searches using MeSH (Medical Subject Headings) terms in the Medline/PubMed database for articles published between January 1, 2000 and December 31, 2019.
In search 1, we used the query ("Child Abuse"[MeSH]) AND "Tooth Injuries"[MeSH]. In search 2, we used the query ("Child Abuse"[MeSH]) AND "Mouth Diseases"[MeSH]. In both searches, we used the following filters: abstract (hasabstract[text]; languages (English[lang] OR Spanish[lang]); publication dates from 2000/01/01 to 2019/12/31 ("2000/01/01"[PDAT]:"2019/12/31"[PDAT]).
After the screening, we compared the articles identified in each search to exclude duplicates. After reading the abstracts of eligible articles, we excluded those that did not specifically address the topic of the review, and all remaining articles were included.
RESULTS
Figure 1 shows the flow chart of the literature search strategy and the inclusion of studies in the review. Search 1 yielded 41 articles before applying the filters. After applying the filters, we selected 19 articles. Search 2 yielded 60 articles before applying the filters. After the filters, 25 articles remained. When we compared the eligible articles obtained in the 2 searches, we excluded 7 that were duplicated, which left 37 articles. After reading the abstracts of these articles, we excluded 11 articles that did not specifically focus on the subject of the review. In the end, 26 articles were included in the review.
Table 1 presents the country of publication, type of article and specific field of the journal in which the 26 articles included in the review were published. We found that 38.5% (n = 10) of the articles were published in the United States. Those published in Spain amounted to 7.7% of the total (n = 2). When it came to the type of article, the most frequent types were case reports and reviews, with 6 articles in each of these categories. When it came to the specific field of the journal, 65.4% (n = 17) were published in dentistry journals and 16% (n = 4) in paediatrics journals.
| Table 1. Country of publication, type of article and professional field of the journals that published the 26 articles included in the review | |||||
|---|---|---|---|---|---|
| Country of publication | n | Type of article | n | Professional journal | n |
| United States | 10 | Case report | 6 | Odontology | 17 |
| United Kingdom | 3 | Review | 6 | Paediatrics | 4 |
| Spain | 2 | Clinical practice guideline | 4 | Otorhinolaryngology | 3 |
| Canadá | 2 | Comparative study | 3 | Other specialities | 2 |
| Italy | 2 | Observational study | 3 | ||
| Portugal | 1 | Multicentre study | 2 | ||
| Switzerland | 1 | Case-control study | 1 | ||
| Sweden | 1 | Systematic review | 1 | ||
| Finland | 1 | ||||
| Brazil | 1 | ||||
| India | 1 | ||||
| China | 1 | ||||

Table 2 describes the oral and dental lesions observed in cases of physical abuse. All of them are suspicious, but none are pathognomonic. They must be differentiated from unintentional oral and dental injuries, which are relatively common in the paediatric age group. To do so, it is important to search for physical signs that are highly suspicious.5-19
| Table 2. Oral and dental lesions suggestive of physical abuse |
|---|
| Bruises and lacerations in lips, labial frenulum, gums, tongue, sublingual mucosa, soft or hard palate and oral mucosa caused by direct trauma or eating utensils used in force-feeding |
| Burns or blisters in the perioral region or oral cavity resulting from force-feeding of scalding liquids or foods |
| Bruises, scabbing or scarring in the lip corners caused by gagging of the child in an attempt to make them quiet |
| Dental fractures, dislocations o avulsions caused by direct trauma |
| Pulp necrosis (grey or pink decolouration of the tooth) caused by past repetitive trauma |
| Bite marks in the mouth caused by the child’s own teeth in the context of physical abuse |
| Bite marks caused by a human adult: ovoid or elliptical shape with an intercanine width > 3 cm, often with ecchymosis in the centre |
| Persistent, recurrent, multicoloured and unusual oral lesions that do not fit a specific clinical picture or disease and that are inflicted intentionally to seek medical care |
| Pharyngeal injuries inflicted intentionally to make the child cough or vomit blood or to create other symptoms requiring medical care |

Table 3 describes the oral and dental diseases found in cases of neglect in childcare and dental care. All of them are suggestive of neglect but none is pathognomonic. Therefore, it is important to assess for the presence of factors considered necessary to establish the diagnosis of dental neglect, whether there are other health problems resulting from chronic physical neglect in nutrition, hygiene, household safety or basic primary care, and whether there are other physical or behavioural signs physical or sexual abuse.5,6,12,13,16,20-25
| Table 3. Dental and oral health problems suggestive of neglect |
|---|
| Multiple untreated dental caries |
| Missing teeth |
| Recurrent gumboils |
| Granuloma and other periodontal diseases |
| Tooth discoloration |

Table 4 describes the oral diseases and lesions seen in cases of sexual abuse. Apart from the detection of sperm or semen in the perioral region or oral cavity, the only other finding that can be considered pathognomonic of sexual abuse are infection by Neisseria gonorrhoeae or Treponema pallidum. All other lesions and diseases are only suggestive or red flags of potential sexual abuse.6,12,16,17,26-30
| Table 4. Specific diseases and oral lesions suggestive or that raise suspicion of sexual abuse |
|---|
| Infection by Neisseria gonorrhoeae |
| Infection by Treponema pallidum (chancres associated with syphilis) |
| Infection by human papillomavirus, especially types 6, 11, 16 and 18 |
| Infection by Chlamydia trachomatis (lymphogranuloma venereum), types L1, L2 or L3 |
| Infection by herpes simplex virus, type 1 and especially type 2 |
| Petechiae, erythema and/on erosions in the oral cavity, particularly at the junction between the soft and hard palate, caused by forced oral sex |
| Bite marks inside the mouth caused by the child’s own teeth during sexual abuse |
| Bite marks caused by human adult: ovoid or elliptical shape with an intercanine width > 3 cm and often with central ecchymosis |

DISCUSSION
Out of the different types of child abuse, physical abuse, neglect and sexual abuse can cause lesions and diseases that manifest in or around the mouth and oral cavity in approximately 30% of cases.3,5,6,11,12 While the prevalence of oral and dental manifestations of child abuse is significant, there is a surprising scarcity of articles on the subject, especially in paediatric journals.
Oral lesions resulting from physical abuse are observed in 12% to 31% of children that experience this type of maltreatment, while intraoral lesions are observed much less frequently (2-11%), leading some researchers to suggest that these lesions frequently go unnoticed. Oral and intraoral lesions caused by physical abuse are more frequent in children aged less than 8 years, especially in infants and pre-schoolers, with no differences based on sex. Abused children that have oral or intraoral lesions are at increased risk of having additional undetected lesions resulting from abuse.5,10-12
The most frequently identified oral and intraoral lesions (46-95%) are bruises and cuts in the lips, labial frenulum, gums, tongue, sublingual mucosa, hard and soft palate and oral mucosa caused by direct trauma or eating utensils used in force-feeding and burns or blisters in the perioral region or oral cavity caused by force-feeding of hot foods or scalding liquids.5-19.
Unintentional oral and dental injuries are relatively frequent in the paediatric population and must be differentiated from injuries resulting from abuse.11 No oral or intraoral lesion is pathognomonic of physical abuse, so the presence of physical manifestations that raise suspicion of potential abuse needs to be assessed: lesions whose extension, depth, location, distribution or pattern/type are incompatible with the age or developmental capabilities of the child; lesions that are inconsistent with the history given the provider; lesions in different stages of healing or scarring; frequent and recurrent lesions in children aged less than 6 years; lesions in infants aged less than 9 months or that cannot move independently yet.6,11,12,16-19
Lesions in the mouth cavity caused by physical abuse in the context of Munchausen syndrome by proxy (faking disease or injury on another) are rare, but this syndrome must be taken into account given the dire consequences that it may have on the child. Usually, the children are aged less than 5 years and the lesions are usually inflicted by the mother voluntarily, intentionally, knowingly in planned and recurrent episodes. The perpetrator is motivated by a psychological need to assume the role of being ill through the child. The purpose of these actions are to seek health care to start a diagnosis and treatment process. This behaviour does not yield any economic or social benefit, but rather the psychological “reward” of being in contact with health care staff and receiving the sympathy, solidarity and compassion extended to the caregivers of a “poor ill child”.6
Dental neglect is defined as the wilful failure of parent or guardian to seek and follow through with treatment necessary to ensure a level of oral health essential for adequate function and freedom from pain and infection.6
Failure of parents or guardians to seek or provide adequate dental care may be due to factors such as isolation of the household, lack of money, difficulties with transport, ignorance or not perceiving the value of dental care.22-24 Therefore, a series of factors are considered necessary to establish the presence of dental neglect: the child being harmed or at risk of harm from lack of dental care; the recommended dental care offering significant benefits to the child; the expected benefit of dental care significantly outweighing any potential adverse effects, so that it would be logical for parents to choose providing care over withholding it; parents or guardians understanding the information given by the provider on the problems of the child and having access to adequate dental care. In addition, oral and dental problems and diseases resulting from dental neglect are usually accompanied by other health problem associated with chronic physical neglect in nutrition, hygiene, household safety or primary care health services (vaccinations, healthy-child checkups, etc). These features are also frequently associated with other physical or behavioural signs of physical or sexual abuse. Therefore, these problems are frequently detected by dentists once the child has entered the child protection system and is referred to a dental provider for treatment.6,12,16,21-25
Although the oral cavity is a frequent site of sexual abuse in children, visible oral lesions and diseases are infrequent and difficult to detect. The only features that can be considered pathognomonic of sexual abuse are oral infections by Neisseria gonorrhoeae or Treponema pallidum. All other suspicious lesions or diseases are suggestive of sexual abuse, but not sufficient for diagnosis.6,12,16,17,22,26-30.
Oral infection by Neisseria gonorrhoeae in sexually abused children is infrequent before puberty, while in adolescents, the observed frequency is of up to 12%. It manifests with multiple ulcers associated with intensely red mucosal surfaces covered by a whitish pseudomembrane. It usually manifests in the form of pharyngitis, but it may also manifest as tonsillitis, gingivitis, stomatitis or glossitis. It is usually asymptomatic but in some cases may cause itching or a burning feeling or be painful.6,26
Oral infection by Treponema pallidum is extremely rare. It manifests with a painless, indurated and hard necrotic ulcer with raised edges that lasts 3 to 6 weeks, usually manifesting in the tonsil region and associated with ipsilateral lymphadenopathy, and less frequently in the pharynx or other regions of the oral cavity or perioral region.26
The incidence in children of infection by human papillomavirus as a sexually transmitted disease has been increasing in recent decades. The most frequently involved serotypes are 6 and 11, followed with a much lower frequency by serotypes 16 and 18. The positive predictive value of this infection for potential sexual abuse is 36% for children aged 4-8 years and 70% for children aged more than 8 years. The incubation period after exposure ranges from 1 to 20 months, lasting a mean of 2-3 months. It manifests with condyloma acuminatum, verrucae vulgaris or squamous papilloma, usually painless, in the perioral area or any mucosal surface of the oral cavity or pharynx.26-30.
Oral infection by serotypes L1, L2 or L3 of Chlamydia trachomatis in sexually abused children is infrequent before puberty, with the frequency increasing to up to 14% in adolescence. It manifests with an ulcer in the oral cavity or pharynx that can be very painful and that resolves without treatment. Two to six weeks, the patient develops a painful inflammation of the lymph nodes that are near the original lesion.6,26
Oral infection by herpes simplex virus manifests as gingival exanthema, oral bleeding and clusters of small fluid-filled vesicles that appear throughout the oral mucosa, including the tongue, palate and perioral skin that progress to pustules. These vesicles and pustules can rupture, giving rise to very painful ulcers 1-5 mm in diameter that tend to coalesce, with scalloped borders and surrounded by redness. The most frequent serotypes are 1 and above all 2.26
In suspected cases of abuse or neglect, oral and dental lesions and diseases must be documented in writing along with any other behavioural signs of abuse exhibited by the minor or the parents/guardians. The provider must take pictures of the lesions and, in case of suspected sexual abuse, collect samples of the oral mucosa and tongue with a sterile cotton swab, allowed to dry in room air and stored appropriately for future analysis in the laboratory. The precision in the diagnosis of sexually transmitted infections of the oral cavity increases if samples are collected within 24 of exposure in prepubertal children and within 72 hours in adolescents. This documentation can be useful in the legal procedures for child protection, and also to assess the response to treatment.6,12,16,19,22
Paediatricians and dentists are legally obligated to report any case of confirmed or suspected child abuse to welfare services, child protection services or the youth justice system. However, there are still barriers that keep a significant proportion of these health professionals from reporting. The main barriers to the detection and notification of cases are insufficient training on the subject, fear of having wrong suspicions, the potential impact on their clinical practice, fear of the consequences reporting may have on the minor, not knowing what documentation and procedures are necessary, and fear of having to do a statement in legal proceedings.5,6,11,12,16,19,22
CONCLUSIONS
Lesions and diseases resulting from child abuse and neglect frequently manifest in the mouth and oral cavity. It is essential that paediatricians and dentists be aware of the issue, be trained on how to detect them, know when and how to document suspicious clinical features and how to report suspected abuse or neglect. These efforts, as well as the overall work of these professionals, will increase our ability to prevent and detect child maltreatment and to protect and care for children.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report in relation to the preparation and publication of this article.
ABBREVIATIONS
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-analyses · WHO: World Health Organization.
REFERENCES
- World Health Organization. Child Maltreatment. In: World Health Organization [online] [accessed 17/02/2021]. Available at: http://apps.who.int/violence-info/child-maltreatment
- World Health Organization. Violence against children: tackling hidden abuse. In: World Health Organization [online] [accessed 17/02/2021]. Available at: http://www.euro.who.int/en/health-topics/disease-prevention/violence-and-injuries/news/news/2020/01/violence-against-children-tackling-hidden-abuse
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Protocolo básico de intervención contra el maltrato infantil en el ámbito familiar. In: Secretaría de Estado de Servicios Sociales e Igualdad [online] [accessed 17/02/2021]. Available at: http://www.observatoriodelainfancia.mscbs.gob.es/productos/pdf/MaltratoInfantil_accesible.pdf
- Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
- Vidal HG, Caldas IM, Coelho Júnior LGTM, Souza EHA, Carvalho MVD, Soriano EP, et al. Orofacial injuries in children and adolescents (2009-2013): a 5-year study in Porto, Portugal. Braz Dent J. 2018;29:316-20.
- Fisher-Owens SA, Lukefahr JL, Tate AR, American Academy of Pediatric Dentistry, Council on Clinical Affairs, Council on Scientific Affairs, et al. Oral and Dental Aspects of Child Abuse and Neglect. Pediatrics. 2017;140:e20171487.
- Mehra M, Chiesa AE, Sirotnak AP. Two cases of sublingual hematoma as a manifestation of child abuse. Ear Nose Throat J. 2015;94:494-6.
- Wolter NE, Cushing SL, Das-Purkayastha PK, Papsin BC. Non-accidental caustic ear injury: two cases of profound cochleo-vestibular loss and facial nerve injury. Int J Pediatr Otorhinolaryngol. 2012;76:145-8.
- McIntosh N, Mok JY, Margerison A, Armstrong L, Mathews A, Robertson AK, et al. The epidemiology of oro-nasal haemorrhage and suffocation in infants admitted to hospital in Scotland over 10 years. Arch Dis Child. 2010;95:810-6.
- Cavalcanti AL. Prevalence and characteristics of injuries to the head and orofacial region in physically abused children and adolescents--a retrospective study in a city of the Northeast of Brazil. Dent Traumatol. 2010;26:149-53.
- Maguire S, Hunter B, Hunter L, Sibert JR, Mann M, Kemp AM, et al. Diagnosing abuse: a systematic review of torn frenum and other intra-oral injuries. Arch Dis Child. 2007;92:1113-7.
- Harris JC, Sidebotham PD, Welbury RR. Safeguarding children in dental practice. Dent Update. 2007;34:508-10, 513-4, 517.
- Subramanian EM, Subhagya B, Muthu MS, Sivakumar N. Neglected child with substance abuse leading to child abuse: a case report. J Indian Soc Pedod Prev Dent. 2005;23:92-5.
- Stricker T, Lips U, Sennhauser FH. Oral bleeding: Child abuse alert. J Paediatr Child Health. 2002;38:528-9.
- Lee LY, Ilan J, Mulvey T. Human biting of children and oral manifestations of abuse: a case report and literature review. ASDC J Dent Child. 2002;69:92-5, 14.
- Serrano García MI, Tolosa Benedicto E, Forner Navarro L. Oral lesions due to child abuse. Identification of the problem and role of the professional. Med Oral. 2001;6:276-89.
- Fenton SJ, Bouquot JE, Unkel JH. Orofacial considerations for pediatric, adult, and elderly victims of abuse. Emerg Med Clin North Am. 2000;18:601-17.
- Haug RH, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:126-34.
- Rupp RP. The dentist’s role in reporting suspected child abuse and neglect. Gen Dent. 2000;48:340-2.
- Kvist T, Zedrén-Sunemo J, Graca E, Dahllöf G. Is treatment under general anaesthesia associated with dental neglect and dental disability among caries active preschool children? Eur Arch Paediatr Dent. 2014;15:327-32.
- Scorca A, Santoro V, De Donno A, Grattagliano I, Tafuri S, Introna F. Early childhood caries (ECC) and neglect in childcare: analysis of an Italian sample. Clin Ter. 2013;164:e365-71.
- Rayman S, Dincer E, Almas K. Child abuse: concerns for oral health practitioners. N Y State Dent J. 2013;79:30-4.
- Montecchi PP, Di Trani M, Sarzi Amadè D, Bufacchi C, Montecchi F, Polimeni A. The dentist's role in recognizing childhood abuses: study on the dental health of children victims of abuse and witnesses to violence. Eur J Paediatr Dent. 2009;10:185-7.
- Valencia-Rojas N, Lawrence HP, Goodman D. Prevalence of early childhood caries in a population of children with history of maltreatment. J Public Health Dent. 2008;68:94-101.
- Mezzich AC, Bretz WA, Day BS, Corby PM, Kirisci L, Swaney M, et al. Child neglect and oral health problems in offspring of substance-abusing fathers. Am J Addict. 2007;16:397-402.
- Fernández-López C, Morales-Angulo C. Otorhinolaryngology manifestations secondary to oral sex. Acta Otorrinolaringol Esp. 2017;68:169-80.
- Sinclair KA, Woods CR, Kirse DJ, Sinal SH. Anogenital and respiratory tract human papillomavirus infections among children: age, gender, and potential transmission through sexual abuse. Pediatrics. 2005;116:815-2.
- Kui LL, Xiu HZ, Ning LY. Condyloma acuminatum and human papilloma virus infection in the oral mucosa of children. Pediatr Dent. 2003;25:149-53.
- Babich SB, Haber SD, Caviedes EY, Teplitsky P. Condylomata acuminata in a boy. J Am Dent Assoc. 2003;134:331-4.
- Syrjänen S, Puranen M. Human papillomavirus infections in children: the potential role of maternal transmission. Crit Rev Oral Biol Med. 2000;11:259-74.