Vol. 21 - Num. 83
Original Papers
Is it possible to detect cases of bullying through the presence of psychosomatic problems?
Rosa M.ª Fuentes Chacóna, M.ª José Simón Saiza, Margarita Garrido Abejara, M.ª Dolores Serrano Parraa, M.ª José Díaz Valentína, Santiago Yubero Jiménezb
aFacultad de Enfermería. Universidad de Castilla-La Mancha. Cuenca. España.
bFacultad de Ciencias de la Educación y Humanidades. Universidad de Castilla-La Mancha. Cuenca. España.
Correspondence: RM Fuentes . E-mail: rosa.fuentes@uclm.es
Reference of this article: Fuentes Chacón RM, Simón Saiz MJ, Garrido Abejar M, Serrano Parra MD, Díaz Valentín MJ, Yubero Jiménez S. Is it possible to detect cases of bullying through the presence of psychosomatic problems? Rev Pediatr Aten Primaria. 2019;21:231-8.
Published in Internet: 01-08-2019 - Visits: 16587
Abstract
Introduction: the high prevalence of school bullying and its consequences make it a public health problem. Objective: to analyse the prevalence of school bullying and its association with psychosomatic problems in a population of adolescent students.
Materials and methods: we conducted a cross-sectional study in a representative sample of 844 students enrolled in 5 secondary education schools (SESs) in the city of Cuenca (Spain). The main assessment instruments were the social acceptance subscale of the KIDSCREEN-52 (bullying) and the PSP scale (psychosomatic problems).
Results: the prevalence of being subject to school bullying was 29.5%, with no differences based on age or sex. We found a higher frequency of psychosomatic problems in female and older adolescents. In students of both sexes, a higher frequency of these problems was associated with being bullied. The regression models built for each of the psychosomatic problems showed that, correcting for the influence of sex and age, being bullied is a predictor of psychosomatic problems and a poorer quality of life. The models that explained the largest percentages of the variance where those for the total score in the psychosomatic problem scale (21%), feelings of sadness (15%), headache (10%) and stomach ache (11%).
Conclusions: psychosomatic problems are frequent in adolescents, especially those who are victims of school bullying. Health care professionals, especially doctors and nurses, should strongly consider the possibility of bullying when an adolescent exhibits psychosomatic symptoms, especially sadness, headache or stomach ache, with no apparent organic cause.
Keywords
● Adolescent ● Bullying ● Health-related quality of life ● Psychosomatic problemsINTRODUCTION
School bullying is an intimidatory, aggressive and repetitive pattern of behaviour by a member in the peer group that manifests with behaviours such as physical or psychological abuse, harassment or isolation with the intent to hurt, bother, ridicule or undermine the self-esteem of the target.1,2 Despite the sociocultural differences that exist between countries, school bullying is an everyday phenomenon that manifests in multiple social contexts.3,4 There is wide variability in the prevalence reported in different studies. A study conducted in 40 countries in a sample of 202 056 adolescents found wide prevalence ranges, of 8.6% to 45.2% for male adolescents and 4.8% to 35.8% in female adolescents.3 The frequencies described in Spain have also varied widely, from the 10.7% reported by García Continente5 to the 23.7% reported by Analitis.6
This phenomenon affects children and adolescents, a vulnerable population, and threatens their development, wellbeing and health-related quality of life (HRQoL).7,8 The magnitude of this problem and its repercussions on health make it a phenomenon of international importance that commands the attention of researchers, parents, educators and health professionals.
Bullying in the school setting has specific characteristics, as it occurs in a restricted physical space and over a long period of time. In this context, violence between peers unfolds in the background and in many cases is not perceived by parents or educators,9 yet the literature suggests that being bullied has deleterious physical, psychological and social consequences in the lives of children and adolescents.1 Being a victim of school bullying is a predictor of physical, mental health and emotional problems12 and is associated with a poorer perceived quality of life.13 It is also reasonable to assume that being bullied also has an impact on academic performance.14
Psychosomatic symptoms may be a manifestation of emotional distress15 and an early indication of being bullied. Recent reviews with meta-analyses have shown that psychosomatic problems are frequent in adolescents that are victims of school bullying.16 However, despite the importance of this issue, few studies have analysed the association of school bullying and psychosomatic problems in Spain.
In this context, our objectives were to establish the prevalence of school bullying and analyse the association between being a victim of bullying and the presence of psychosomatic manifestations in adolescents enrolled in secondary education schools (SESs) in Cuenca, Spain.
MATERIALS AND METHODS
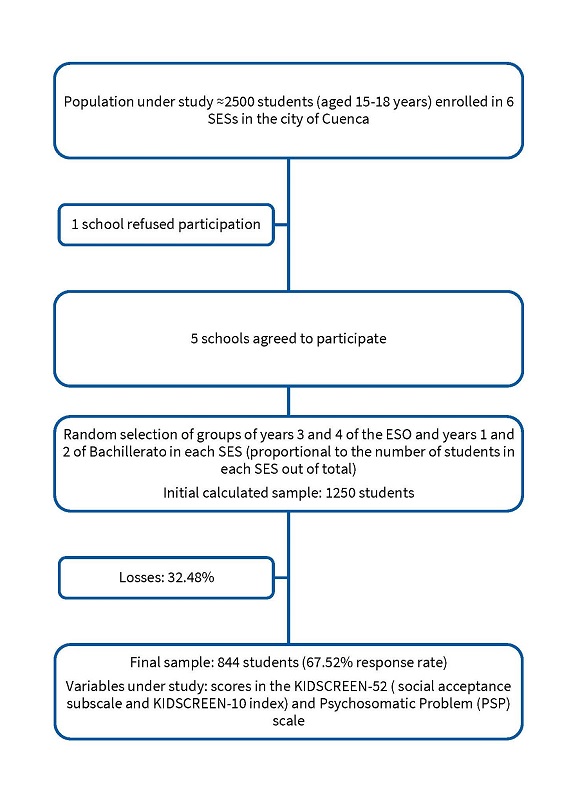
We conducted a cross-sectional multicentre observational and descriptive study in 5 public SESs in the city of Cuenca. The sample included adolescents aged 15 to 18 years enrolled in years 3 and 4 of compulsory secondary education (in Spanish, Educación Secundaria Obligatoria, or ESO) and years 1 and 2 of non-compulsory secondary education (in Spanish, bachillerato). For each academic year, we randomly selected groups of students from each school of a size proportional to the size of each SES relative to the total population to which we would administer the questionnaire (Figure 1). The inclusion criteria were to be a student of the academic years detailed above and informed consent for participation (given by parents in the case of minors and by the students themselves when they were of age). The total population was of 2500 students, and we calculated a minimum sample size of 526 (for a 99% confidence interval [CI] and e = 2%), although we included more students to make up for potential losses. The protocol was approved by the Peripheral Services of the Department of Education, Culture and Sports of Castilla-La Mancha.
| Figure 1. Sample selection process |
|---|
 |

Instruments
We collected data by means of a self-administered questionnaire that included items on sociodemographic variables like age or sex and the following standardised instruments:
- We evaluated psychosomatic manifestations by means of the Psychosomatic Problems scale (PSP),17 which assesses 8 common problems (headache, stomachache, lack of appetite, difficulty sleeping, feeling sad, feeling dizzy, feeling tense and difficulty concentrating) on a Likert scale. The scores of individual items are added to obtain a total score that ranges between 0 and 32, with higher values indicating more frequent symptoms. The scale has exhibited a fair internal consistency (Cronbach α = 0.76).
- We assessed school bullying using the social acceptance subscale of the KIDSCREEN-52 questionnaire on health-related quality of life,18 as has been done in similar studies.6 This subscale includes 3 items: “Have you been afraid of other girls and boys?”; “Have other girls and boys made fun of you?” and “Have other girls and boys bullied you?”. The score is calculated, as described by the authors of the original scale, using Rasch analysis, so that social acceptance/bullying scores are standardised with a mean of 50 and a standard deviation of 10.19 Higher scores indicate absence of bullying. The internal consistency of the scale was fair (Cronbach α = 0.77).
- We assessed quality of life by means of the KIDSCREEN-10 index, a summarised version of the KIDSCREEN-52. Higher scores are indicative of a better quality of life.
Data analysis
We processed and analysed the data using the Statistical Package for the Social Sciences (SPSS) version 23. We estimated the prevalence of school bullying applying the criteria used in similar studies,6 transforming the quantitative variable into a dichotomous variable, considering that participants with scores of less than 40 were victims of bullying and those with scores of more than 40 were not. We used the Student t test to compare the presence of psychosomatic symptoms and the HRQoL of victims and non-victims.
Lastly, we performed multivariate analysis (stepwise regression) setting as the dependent variable each of the psychosomatic problems, the PSP score, and HRQoL. The control variables (age and sex) were introduced in the first step, and the independent variable (victim of school bullying) in the second step, with the aim of comparing the amount of variance explained by the model (R2).
RESULTS
Of the 844 participants, 55.7% were female. The mean age of the sample was 16.3 ± 1 years.
We found a prevalence of exposure to school bullying of 29.5%, with no significant differences between the sexes (Table 1). When it came to psychosomatic manifestations, we found that girls scored significantly higher in the total scale (11 ± 4.6 compared to 7.7 ± 4.2 in boys) as well as each of the symptoms under analysis. In both sexes, the most frequent symptoms were difficulty concentrating (1.8 ± 0.9 in boys versus 1.9 ± 0.9 in girls), headache (0.9 ± 0.9 in boys versus 1.4 ± 0.9 in girls), feeling tense (1.1 ± 1.0 in boys versus 1.4 ± 1.0 in girls) and feeling sad (0.9 ± 0.9 in boys versus 1.4 ± 1.0 in girls). As for the HRQoL, boys scored significantly higher than girls (48.1 ± 6.7 versus 44.6 ± 7.2).
| Table 1. General characteristics of the sample by sex | |||||||
|---|---|---|---|---|---|---|---|
|
Mean ± SD |
Male Mean ± SD |
Female Mean ± SD |
p |
Age 15-16 years Mean ± SD |
Age 17-18 years Mean ± SD |
p | |
| Prevalence of school bullying | 29.5% | 29.9% | 29.1% | 0.801 | 28.9% | 30.3% | 0.704 |
| Psychosomatic Problem score | 9.5 ± 4.7 | 7.7 ± 4.2 | 11.0 ± 4.6 | 0.000 | 8.8 ± 4.7 | 10.5 ± 4.6 | 0.000 |
| Difficulty concentrating | 1.9 ± 0.9 | 1.8 ± 0.9 | 1.9 ± 0.9 | 0.006 | 1.7 ± 0.9 | 2.0 ± 0.9 | 0.000 |
| Difficulty sleeping | 1.1 ± 1.0 | 0.9 ± 1.0 | 1.2 ± 1.0 | 0.001 | 1.0 ± 1.0 | 1.2 ± 1.0 | 0.010 |
| Headache | 1.2 ± 0.9 | 0.9 ± 0.9 | 1.4 ± 0.9 | 0.000 | 1.1 ± 0.9 | 1.4 ± 0.9 | 0.000 |
| Stomach ache | 1.1 ± 0.9 | 0.8 ± 0.7 | 1.3 ± 0.9 | 0.000 | 1.0 ± 0.8 | 1.2 ± 0.9 | 0.004 |
| Feeling tense | 1.3 ± 1.0 | 1.1 ± 1.0 | 1.4 ± 1.0 | 0.000 | 1.2 ± 1.0 | 1.5 ± 1.0 | 0.000 |
| Poor appetite | 0.9 ± 0.9 | 0.6 ± 0.8 | 1.2 ± 1.0 | 0.000 | 0.9 ± 1.0 | 0.9 ± 0.9 | 0.322 |
| Feeling sad | 1.1 ± 1.0 | 0.9 ± 0.9 | 1.4 ± 1.0 | 0.000 | 1.0 ± 1.0 | 1.3 ± 1.0 | 0.001 |
| Feeling dizzy | 0.7 ± 0.8 | 0.4 ± 0.6 | 0.8 ± 0.9 | 0.000 | 0.6 ± 0.8 | 0.7 ± 0.8 | 0.003 |
| Social acceptance (bullying) | 46.9 ± 9.9 | 46.9 ± 9.4 | 47.0 ± 10.2 | 0.857 | 46.7 ± 9.7 | 47.2 ± 10.1 | 0.452 |
| KIDSCREEN-10 index | 46.1 ± 7.2 | 48.1 ± 6.7 | 44.6 ± 7.2 | 0.000 | 46.7 ± 7.2 | 45.4 ± 7.1 | 0.008 |

The results of the analysis of the association between being a victim of school bullying and the presence of psychosomatic symptoms can be found in Table 2, and show that being a victim of bullying is significantly associated with obtaining higher scores for all the psychosomatic problems under analysis and a poorer perceived quality of life. However, we found differences in these results when we stratified the analysis by sex. In male victims, we found an association with headache, stomach ache, feeling tense, lack of appetite, feeling sad and feeling dizzy, while in female victims we found an association with difficulty concentrating, difficulty sleeping, headache, feeling tense, feeling sad and feeling dizzy.
| Table 2. Association between psychosomatic problems and being bullied. Differences based on sex | |||||||
|---|---|---|---|---|---|---|---|
| Male | Female | Total | |||||
| (Mean ± SD) | p | (Mean ± SD) | p | (Mean ± SD) | p | ||
| Psychosomatic score | Victims | 9.3 ± 4.4 | 0.000 | 13.0 ± 4.5 | 0.000 | 11.3 ± 4.8 | 0.000 |
| Non-victims | 7.1 ± 4 | 10.2 ± 4.5 | 8.8 ± 4.5 | ||||
| Difficulty concentrating | Victims | 1.9 ± 1 | 0.113 | 2.2 ± 0.9 | 0.000 | 2.1 ± 0.9 | 0.000 |
| Non-victims | 1.7 ± 0.9 | 1.8 ± 0.8 | 1.8 ± 0.9 | ||||
| Difficulty sleeping | Victims | 1.1 ± 1 | 0.126 | 1.4 ± 1 | 0.015 | 1.2 ± 1 | 0.005 |
| Non-victims | 0.9 ± 1 | 1.1 ± 1 | 1.0 ± 1 | ||||
| Headache | Victims | 1.2 ± 0.9 | 0.003 | 1.6 ± 1 | 0.004 | 1.4 ± 1 | 0.000 |
| Non-victims | 0.9 ± 0.8 | 1.4 ± 0.9 | 1.1 ± 0.9 | ||||
| Stomach ache | Victims | 0.9 ± 0.7 | 0.034 | 1.4 ± 0.8 | 0.055 | 1.2 ± 0.8 | 0.008 |
| Non-victims | 0.7 ± 0.7 | 1.2 ± 0.9 | 1.0 ± 0.9 | ||||
| Feeling tense | Victims | 1.5 ± 1 | 0.000 | 1.7 ± 1 | 0.000 | 1.6 ± 1 | 0.000 |
| Non-victims | 1.0 ± 1 | 1.3 ± 1 | 1.2 ± 1 | ||||
| Poor appetite | Victims | 0.7 ± 0.8 | 0.032 | 1.3 ± 0.9 | 0.059 | 1.0 ± 0.9 | 0.010 |
| Non-victim | 0.5 ± 0.8 | 1.1 ± 1 | 0.8 ± 0.9 | ||||
| Feeling sad | Victims | 1.2 ± 0.9 | 0.000 | 1.9 ± 1 | 0.000 | 1.62 ± 1 | 0.000 |
| Non-victim | 0.7 ± 0.8 | 1.2 ± 0.9 | 1.0 ± 0.9 | ||||
| Feeling dizzy | Victims | 0.6 ± 0.7 | 0.005 | 1.0 ± 0.9 | 0.002 | 0.8 ± 0.9 | 0.000 |
| Non-victim | 0.4 ± 0.6 | 0.7 ± 0.8 | 0.62 ± 0.8 | ||||
| Quality of life-10 index | Victims | 45.2 ± 6.1 | 0.000 | 41.5 ± 5.5 | 0.000 | 43.1 ± 6.1 | 0.000 |
| Non-victim | 48.3 ± 6.6 | 45.9 ± 7.5 | 47.3 ± 7.3 | ||||

With the aim of assessing the impact of being bullied on dependent variables (overall perceived HRQoL, total PSP score and score in each of the psychosomatic problems), we developed different stepwise linear regression models, controlling for sex and age in all. The results revealed that, save for the lack of appetite, all other psychosomatic variables were significantly associated with being bullied. The models that explained the largest amount of variance were those developed for the following dependent variables: total PSP score (21%), global HRQoL score (15%), feeling sad (15%), headache (10%) and stomach ache (11%).
DISCUSSION
Our study shows that being bullied is a predictor of psychosomatic symptoms in adolescent students aged 15 to 18 years. Our data also suggest that being bullied also has an impact on HRQoL. The effect of bullying is particularly strong and manifest most frequently manifesting in symptoms like sadness and impairment in HRQoL.
We found a prevalence of being subject to bullying of 29.5%, with no significant differences based on sex or age group. The scientific literature exhibits a wide variability in the reported prevalence3,5,6 that can be attributed both to the differences in methodology between studies and to the fact that adolescents do not always acknowledge that they are being bullied. Instruments that use the term bullying find lower frequencies, whereas those that assess observed school bullying (behaviours identified as bullying), as the one used in our study, find higher frequencies.20 We also ought to highlight that most bullying behaviours are kept secret and are downplayed or trivialised as normal among adolescents rather than considered acts of real violence.21 This situation may lead to condoning of abusive behaviours and the perception that these behaviours are acceptable means to resolve conflicts and fulfil wants.22 The disparity of the existing data reflects the complexity of this phenomenon but does not detract from its importance, evincing the need to develop accurate and reliable tools for its assessment that neither overestimate nor underestimate this problem.
School bullying does not always produce visible harm, especially in the most frequent forms of abuse (psychological and social). However, as the literature evinces, it may have a severely negative impact on the health, socio-emotional development and academic performance of adolescents, causing problems that may persist and have repercussions in adult life.23,24 One of the most likely early repercussions that can be detected in victims is an increase in stress and social anxiety, which may manifest in the form of different psychosomatic problems, signs that the adolescents may be experiencing a stressful situation in everyday life.
Thus, the presence of psychosomatic problems may be a manifestation of bullying and can be a red flag to detect a phenomenon that in many cases remains hidden and is not recognised in the household, school or health care settings.
In our study, we found that adolescents that were victims of bullying scored higher in all the psychosomatic problems analysed as well as the total PSP score, confirming the results of similar studies.11,25 Based on our results, the psychosomatic problem most strongly associated with being bullied is sadness. Being subject to school bullying is a strong predictor of symptoms of depression26 and, as other studies have shown, the presence of these symptoms in victims of bullying can cause health problems in the long, medium and short term.23 Bullying can cause very significant scars, and in some cases, the underestimation or trivialization of this problem is a source of intense distress to bullied adolescents, a pain that may lead the adolescent to engage in self-injurious behaviours that could have irreparable consequences, including death.27
As we have already mentioned, school bullying can have a negative impact on the mental health of the individual victim, but as the study conducted by Modin in 2015 shows, it can also affect the overall atmosphere of the school, thus becoming an environmental threat.28 In classrooms where bullying is frequent, non-victims can perceive a potential risk of becoming a target of bullying in the future, which may cause them increased stress; thus, students in classrooms with greater numbers of victims of bullying exhibit more psychosomatic problems.29 This suggests that bullying between peers affects both the targets of bullying and their classmates.
We ought to highlight some limitations of the study in regard to the interpretations of its results. While it seems reasonable to assume a causal relationship between being the target of bullying and developing psychosomatic problems, we need to take into account that the data cannot provide information about the causal direction of the observed associations due to the cross-sectional design of the study, and therefore, do not allow us to conclude whether being bullied leads to an increase in health problems or whether adolescents with health problems are more likely to be bullied. The performance of longitudinal studies could clarify these questions in the future, although there are studies that already suggest that this may be a two-way relationship.30
CONCLUSIONS
The findings of our study may have important implications for health care professionals. A careful assessment of health should include an assessment of psychosomatic problems as manifestations of emotional distress,15 as these are a warning sign of potential exposure to school bullying.
When it comes to school bullying, the school community (students, teachers and parents) plays the most important role; nevertheless, primary care health professionals also play an significant role due to their previous acquaintance with adolescents and their family environment.31 Although the effects of intimidation are rarely obvious and adolescents rarely verbalize that they are being subject to intimidation, paediatricians and nurses in primary care clinics can identify bullying situations, counsel families, treat victims and advocate for implementation of bullying prevention programmes in the school setting.22 In this sense, it is important for health providers, especially paediatricians and nurses, to seriously consider the possibility of a patient being a victim of bullying when an adolescent exhibits several psychosomatic problems without an organic cause, especially those associated with a depressed mood.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
CI: confidence interval · ESO: Educación Secundaria Obligatoria (Compulsory Secondary Education) · HRQoL: health-related quality of life · SES: secondary education school.
REFERENCES
- Olweus D. School bullying: development and some important challenges. An Rev Clin Psychol. 2013;9:751-80.
- Armero Pedreira P, Bernardino Cuesta B, Bonet de Luna C. Acoso escolar. Rev Pediatr Aten Primaria. 2011;13:661-70.
- Craig W, Harel-Fisch Y, Fogel-Grinvald H, Dostaler S, Simons-morton B, Molcho M, et al. A cross-national profile of bullying and victimization among adolescents in 40 countries. Int J Public Heal. 2009;54:216-24.
- Romera EM, Rey R, Ortega R. Prevalencia y aspectos diferenciales relativos al género del fenómeno bullying en países pobres. Psicothema. 2011;23:624-9.
- García Continente X, Pérez Giménez A, Manel Nebot A. Factores relacionados con el acoso escolar (bullying) en los adolescentes de Barcelona. Gac Sanit. 2010;24:103-8.
- Analitis F, Velderman MK, Ravens-Sieberer U, Detmar S, Erhart M, Herdman M, et al. Being Bullied: Associated Factors in Children and Adolescents 8 to 18 Years Old in 11 European Countries. Pediatrics. 2009;123:569-77.
- Chester KL, Spencer NH, Whiting L, Brooks FM. Association between experiencing relational bullying and adolescent health-related quality of life. J Sch Health. 2017;87:865-72.
- Hellfeldt K, Gill PE, Johansson B. Longitudinal analysis of links between bullying victimization and psychosomatic maladjustment in swedish schoolchildren. J Sch Violence. 2016;17:1-13.
- Informe del Defensor del Pueblo. Violencia escolar: el maltrato entre iguales en la Educación Secundaria Obligatoria 1999-2006. In: Defensor del Pueblo [online] [accessed on 30/07/2019]. Available at www.defensordelpueblo.es/informe-monografico/violencia-escolar-el-maltrato-entre-iguales-en-la-educacion-secundaria-obligatoria-1999-2006-nuevo-estudio-y-actualizacion-del-informe-2000-2007/
- Nielsen MB, Hetland J, Matthiesen SB, Einarsen S. Longitudinal relationships between workplace bullying and psychological distress. Scand J Work Environ Health. 2012;38:38-46.
- Gini G, Pozzoli T. Association between bullying and psychosomatic problems: a meta-analysis. Pediatrics. 2009;123:1059-65.
- Bond L, Carlin JB, Thomas L, Rubin K, Patton G. Does bullying cause emotional problems? A prospective study of young teenagers. BMJ. 2001;323:480-4.
- Hidalgo-Rasmussen C, Molina T, Molina R, Sepúlveda R, Martínez V, Montaño R, et al. Bullying y calidad de vida relacionada con la salud en adolescentes escolares chilenos. Rev Med Chi. 2015;143:716-23.
- Penning SL, Bhagwanjee A, Govender K. Bullying boys: the traumatic effects of bullying in male adolescent learners. J Child Adolesc Ment Heal. 2010;22:131-43.
- Fuentes Chacón RM, Simón Saiz MJ, Garrido Abejar M, Serrano Parra MD, Larrañaga Rubio ME, Yubero Jiménez S. Síntomas psicosomáticos como expresión del deterioro de la calidad de vida relacionada con la salud en adolescentes. Aten Primaria. 2017;50:493-9.
- Gini G, Pozzoli T. Bullied children and psychosomatic problems: a meta-analysis. Pediatrics. 2013;132:720-9.
- Hagquist C. Psychometric properties of the PsychoSomatic Problems scale: A Rasch analysis on adolescent data. Soc Indic Res. 2008;86:511-23.
- Rajmil L, Alonso J, Berra S, Ravens-Sieberer U, Gosch A, Simeoni MC, et al. Use of a children questionnaire of health-related quality of life (KIDSCREEN) as a measure of needs for health care services. J Adolesc Health. 2006;38:511-8.
- Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Power M, et al. The KIDSCREEN-52 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Value Heal. 2008;11:645-58.
- Sánchez-Queija I, García-Moya I, Moreno C. Trend analysis of bullying victimization prevalence in spanish adolescent youth at school. J Sch Health. 2017;87:457-64.
- Oñate A, Piñuel I. Informe Cisneros X. Acoso y violencia escolar en España. In: Bienestar y protección infantil [online] [accessed on 30/07/2019]. Available at www.bienestaryproteccioninfantil.es/fuentes1.asp?sec=27&subs=281&cod=2356&page=
- Buitrago Ramírez F, Ciurana Misol R, Chocrón Bentata L, Fernández Alonso M del C, García Campayo J, Montón Franco C, et al. Recomendaciones para la prevención de los trastornos de la salud mental en Atención Primaria. Aten Primaria. 2016;48:77-97.
- Sigurdson JF, Undheim AM, Wallander JL, Lydersen S, Sund AM. The long-term effects of being bullied or a bully in adolescence on externalizing and internalizing mental health problems in adulthood. Child Adolesc Psychiatry Ment Health. 2015;9:42.
- Vivolo-Kantor A, Martell B, Holland K, Westby R. A systematic review and contenct analysis of bullying and cyber-bullying measurement strategies. Aggress Violent Behav. 2014;19:423-34.
- Fekkes M, Pijpers F, Verloove-Vanhorick S. Bullying behavior and associations with psychosomatic complaints and depression in victims. J Pediatr. 2004;144:17-22.
- Pham TB, Adesman A. Increased risk of sadness and suicidality among victims of bullying experiencing additional threats to physical safety. Int J Adolesc Med Health. 2017;1:1-9.
- Kelly EV, Newton NC, Stapinski LA, Slade T, Barrett EL, Conrod PJ, et al. Suicidality, internalizing problems and externalizing problems among adolescent bullies, victims and bully-victims. Prev Med. 2015;73:100-5.
- Modin B, Låftman SB, Östberg V. Bullying in context: an analysis of psychosomatic complaints among adolescents in Stockholm. J Sch Violence. 2015;14:382-404.
- Laftman SB, Modin B. Peer victimization among classmates—associations with students’ internalizing problems, self-esteem, and life satisfaction. Int J Environ Res Public Health. 2017;14. pii: E1218.
- Fekkes M, Pijpers F, Fredriks A, Vogels T, Verloove-Vanhorick S. Do bullied children get ill, or do ill children get bullied? a prospective cohort study on the relationship between bullying and health-related symptoms. Pediatrics. 2006;117:1568-74.
- Galardi Andonegui M, Ugarte Líbano R. Maltrato entre iguales (bullying) en la escuela. ¿Cuál es el papel de los pediatras de Atención Primaria? Rev Pediatr Aten Primaria. 2005;7:11-9.





