Vol. 21 - Num. 82
Original Papers
How much do healthcare workers in the mother & child health area know about breastfeeding? A study of the 14 public hospitals in Castile & Leon
M.ª José González Veredaa, M.ª Rosario Bachiller Luqueb, Ana Dorado Díazc, Pilar Martín Pérezc, Tomás Maté Enríquezd, Virtudes Niño Martíne
aMatrona. CS Circular . Valladolid. España.
bPediatra. CS Pilarica Circular. Valladolid. España.
cTécnico en Estadística. Consejería de Sanidad. Valladolid. España.
dGerencia de Atención Primaria de Valladolid Este. Valladolid. España.
eEnfermera. CS La Victoria. Valladolid. España.
Correspondence: MJ González . E-mail: gonverma@gmail.com
Reference of this article: González Vereda MJ, Bachiller Luque MR, Dorado Díaz A, Martín Pérez P, Maté Enríquez T, Niño Martín V. How much do healthcare workers in the mother & child health area know about breastfeeding? A study of the 14 public hospitals in Castile & Leon. Rev Pediatr Aten Primaria. 2019;21:133-46.
Published in Internet: 06-06-2019 - Visits: 23825
Abstract
Introduction: breastfeeding is a priority objective in public health. Health care professionals involved in the delivery of hospital-based maternal and child health services need to have adequate knowledge of breastfeeding.
Material and methods: we conducted a cross-sectional descriptive study in January and February 2015 using the validated questionnaire ECola, which we adapted for administration to gynaecologists, midwives and nurses. To survey nursing assistant technicians (NATs), we adapted the questionnaire developed by Temboury Molina MC, modified by the authors. The study universe consisted of all health care professionals involved in the delivery of maternal and child health services in the 14 public hospitals of Castilla y León.
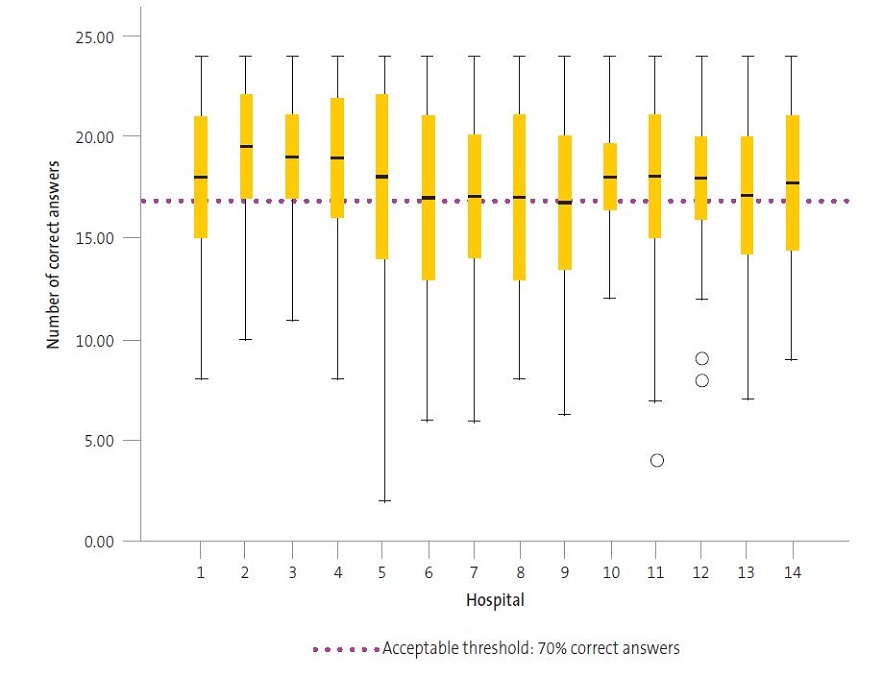
Results: we received a total of 724 questionnaires (61.0%). Having defined a threshold of 70% of correct answers (16.8 points) to define adequate knowledge, nurses had an adequate knowledge of breastfeeding (18.19) that was significantly better (p < 0.05) compared to physicians (17.01). Midwives had the highest mean score (20.03). Gynaecologists, with a mean score of 15.24 points, had a level of knowledge considered inadequate. Nurse assistants, with a mean score of 16.93 points, exhibited adequate knowledge but close to the lower limit. We found statistically significant differences in knowledge between the providers working in different hospitals. Overall, the level of knowledge of professionals working in maternal and child health in public hospitals in Castilla y Leon was adequate (17.54).
Conclusions: overall, the level of knowledge of health professionals involved in delivery of maternal and child health services was adequate. Some categories of professionals lacked knowledge in aspects that are essential to the adequate management of breastfeeding. We need to consider the need to include training in breastfeeding in educational curricula, especially those of gynaecologists and NATs.
Keywords
● Breastfeeding ● Knowledge ● Midwives ● Nurse ● Nurse assistant technicians ● PhysiciansINTRODUCTION
The Global Strategy on Infant and Young Child Feeding (GSIYCF) was developed by the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF), approved by the Board in 2002. It reinforced the importance of promoting and supporting exclusive breastfeeding in the first 6 months of life and maintenance of breastfeeding combined with a feasible diet of adequate, safe and appropriate complementary foods through age 2 years.1
Multiple studies conducted in Spain2-5 and other countries6-9 have described the factors associated with the prevalence of breastfeeding, and all of them have emphasised the important role of the health professionals that are in contact with the mother, both during pregnancy and after birth.
The first and possibly most important step to promote breastfeeding is to improve the knowledge and attitudes of health care providers. They must be able to help mothers initiate breastfeeding and address the questions and concerns that arise during breastfeeding.10 The education of parents before and after birth seems to be another essential factor for successful breastfeeding.11
Every instance in which breastfeeding is dropped due to lack of training of health professionals constitutes a failure of the health care system. To date, there were no validated tools for the assessment of knowledge about breastfeeding in Spain. The rigorous work of Gómez Fernández-Vegue and Menéndez Orenga has produced a valuable instrument that allows us to evaluate knowledge and skills in breastfeeding.12 A questionnaire was developed in the context of the Baby Friendly Hospital Initiative (BFHI) to assess the knowledge and training needs of health care professionals on the subject of breastfeeding13 and disseminated in mid-2015, but we do not have any current data on its use in Spanish hospitals.
The current situation of breastfeeding in Castilla y Leon is that 82.7% of mothers initiate exclusive breastfeeding, but only 27.1% (95% confidence interval [95 CI]: 21.8 to 39.9) maintain it through 6 months post birth.14 There are no published data for Castilla y Leon about the knowledge of health professionals regarding breastfeeding.
MATERIALS AND METHODS
Study design: we conducted a descriptive cross-sectional study in January and February 2015.
Study universe: health care professionals of any type (paediatricians, gynaecologists, midwives, nurses, nurse assistant technicians [NATs]) involved in the delivery of maternal and child health services in the 14 hospitals of the Regional Public Health Administration of the Autonomous Community of Castilla y Leon (SACYL): 1187 health care providers. We chose to survey the entire population to obtain data from every hospital.
Methods: we used two questionnaires as measurement tools:
Questionnaire 1: questionnaire on the Knowledge of Breastfeeding (Encuesta sobre Conocimientos en Lactancia Materna, ECola),12 validated for use in paediatricians and medical intern-residents (MIR) in the area of paediatrics. In collaboration with the authors of the original questionnaire, we adapted it to make it applicable to gynaecologists, midwives and nursing staff. We obtained the permission of the authors to do so, and the final version used in the study included 42 items.
Items 1 to 8 collect data about the health provider. The questionnaire has been validated, and it includes 24 items whose answers can be rated (items 9 to 33 excluding item 30, which we could not rate, as it was an open-ended question). We gave correct answers 1 point. A total score of 24 points thus corresponded to 100% correct answers. The questionnaire also included items whose answers could not be scored (items 34 to 42), which addressed the attitudes of health professionals toward breastfeeding, which we did not analyse in this study.
The questionnaire explored basic knowledge and skills in breastfeeding: physiology of breastfeeding, public health, problems in the first few days, late problems, assessment of intake during feeds, maternal factors and attitudes.
Questionnaire 2: this questionnaire was developed by Temboury Molina in 200310 to assess the knowledge of paediatrics MIRs in Spain on the management of breastfeeding. Since it is simple and it explores the knowledge areas that we considered important, we used it to survey NATs after making minor adjustments. The final questionnaire comprised 29 items. Items 1 to 4 explored sociodemographic characteristics. Items 5 to 28 received a score of 1 point if answered correctly. We did not score item 29 because it was an open-ended question.
We assessed basic knowledge areas about breastfeeding: advantages of breastfeeding, risks of artificial feeding, mechanisms of lactation and sucking, skills to adequately manage breastfeeding initiation and maintenance, assessment of feeds, management of difficulties, and hospital regulations regarding breastfeeding.
Study protocol: we reached out to health professionals through a letter sent from the Directorate General of Public Health to the administrators, medical directors, directors of nursing and supervisors of maternal and child health services in all hospitals of Castilla y Leon. We also contacted the Asociación Castellanoleonesa de Matronas (Midwife Association of Castilla y Leon, ASCALEMA) to appoint a study coordinator in each hospital. Questionnaires were administered in paper form and completed during team meetings or patient care conferences, at which point respondents also signed their informed consent to participation.
We performed the analysis using the software package IBM SPSS Statistics version 22.0.0.0.
RESULTS
Sociodemographic data
The distribution of respondents to questionnaire 1 by professional category was: 13.3% neonatologists, 18.6% gynaecologists, 24.8% midwives, 19.7% nurses employed in the maternity ward, 19.5% nurses in the neonatal ward. Most respondents were female (87.1%), and the median age was 43.6 years (±10.6), 62.5% had children and 59.2% had experience breastfeeding.
In questionnaire 2, the distribution of respondents that were NATs was predominantly female (95.8%), with a mean age of 53.1 years (±7.5), 78.8% had children, most of them 2 children (61.1%).
Some respondents did not complete some of the questions in the sociodemographic section (Table 1).
| Table 1. Sociodemographic data | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Absolute frequency(n) | Sex | Type of employment | Professional experience | Experience breastfeeding(self or partner) | Age | ||||||||||
| Female | Male | Permanent | Temporary | Per diem | <10 years | ≥10 years | No | Yes | Mena | Standard deviation | Minimum | Median | Maximum | ||
| n | n | n | n | n | n | n | n | n | |||||||
| Professional category | Neonatologist | 50 | 18 | 41 | 14 | 13 | 25 | 43 | 31 | 36 | 40.98 | 9.65 | 27 | 39 | 64 |
| Gynaecologist | 63 | 32 | 58 | 17 | 20 | 32 | 63 | 38 | 56 | 43.33 | 11.18 | 26 | 42 | 65 | |
| Midwife | 122 | 5 | 85 | 10 | 32 | 46 | 80 | 51 | 74 | 42.74 | 10.53 | 24 | 41 | 64 | |
| Maternity nurse | 99 | 2 | 69 | 13 | 18 | 17 | 83 | 35 | 60 | 44.59 | 10.93 | 27 | 45 | 62 | |
| Neonatal nurse | 96 | 2 | 70 | 15 | 13 | 15 | 84 | 24 | 70 | 46.69 | 10.25 | 21 | 48 | 64 | |
| NATs | 203 | 4 | 0 | 0 | 0 | 84 | 87 | 0 | 0 | 53.15 | 7.54 | 25 | 55 | 63 | |
| Total | 633 | 63 | 323 | 69 | 96 | 219 | 440 | 179 | 296 | 46.46 | 10.75 | 21 | 48 | 65 | |

Response rate
We received a total of 724 responses (corresponding to 61.0% of all eligible health providers in Castilla y Leon). Questionnaire 1 was completed by 512 professionals (response rate of 60.5%) and questionnaire 2 by 212 (response rate of 62.2%) (Table 2).
| Table 2. Differences in participation by professional (medical/nursing) category | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Absolute frequency | Sex | Type of employment | Professional experience | Experience breastfeeding (self or partner) | Age | |||||||||||
| Female | Male | p-value, physicians vs nurses | Permanent | Temporary | Contract | p-value, physicians vs nurses | < 10 years | ≥ 10 years | p-value, physicians vs nurses | No | Yes | p-value, physicians vs nurses | Mean | p-value, physicians vs nurses | ||
| n | n | n | n | n | n | n | n | n | ||||||||
| Profession | Physicians | 113 | 50 | p = 0.0000 | 99 | 31 | 33 | p = 0.0866 | 57 | 106 | p = 0.227 | 69 | 92 | p = 0.110 | 42.36 | p = 0.045 |
| Nurses | 317 | 9 | 224 | 38 | 63 | 78 | 247 | 110 | 204 | 44.46 | ||||||
| NATs | 203 | 4 | 0 | 0 | 0 | 84 | 87 | 0 | 0 | 53.15 | ||||||
| Total | 633 | 63 | 323 | 69 | 96 | 219 | 440 | 179 | 296 | 46.46 | ||||||

We found statistically significant differences based on sex and age; physicians that responded were younger, and there was a predominance of the female sex.
We did not find statistically significant differences in participation based on type of employment, personal experience with breastfeeding, or years of professional experience.
Variation in participation in the different public hospitals of Castilla y Leon
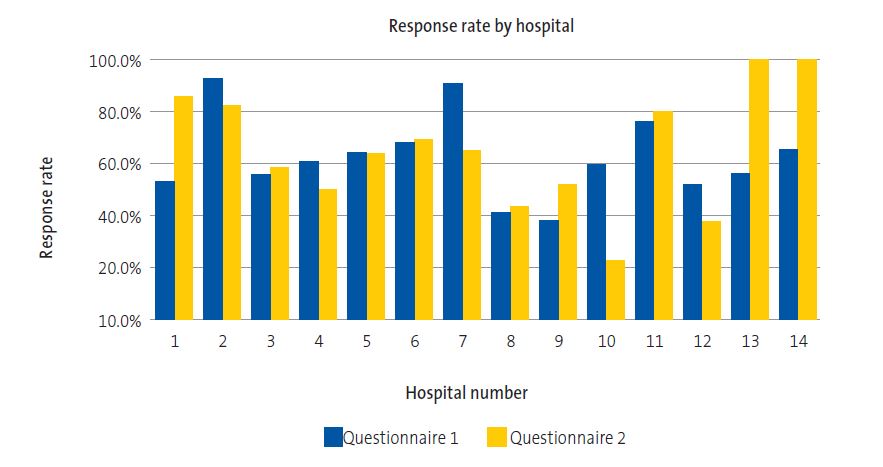
We found significant differences (p < 0.05) between hospitals in the response rate. In most hospitals (9/14), between 50% and 70% of the health care staff in women’s and children’s services participated in the survey (Figure 1).
Analysis of questionnaire items
The results can be found in Tables 3 and 4.
| Table 3. Percentage of professionals that answered correctly by professional category | |||||||
|---|---|---|---|---|---|---|---|
| Correct answer | Overall | Neonatologists | Gynaecologists | Midwives | Maternity nurses | Neonatology nurses | |
| Questionnaire 1. First section | |||||||
| 9. A blood glucose test should be performed in all breastfed full term newborns in the first 24-48 h of life, even in the absence of symptoms | False | 92.1% | 98.5% | 78.9% | 98.4% | 96.0% | 89.0% |
| 10. In case of mastitis, breastfeeding should be suspended temporarily | False | 88.8% | 92.6% | 89.5% | 93.7% | 88.1% | 84.0% |
| 11. Mothers should be advised to feed infants each breast for 15 minutes every 2-3 hours | False | 77.3% | 88.2% | 64.2% | 96.9% | 76.2% | 64.0% |
| 12. Exclusive formula feeding carries an increased risk of morbidity and mortality | True | 55.9% | 67.6% | 44.2% | 64.6% | 51.5% | 52.0% |
| 13. Most infants delivered by caesarean section will require supplementation with formula in the first hours of life | False | 79.9% | 88.2% | 74.7% | 96.1% | 75.2% | 66.0% |
| 14. In case a breastfed infant has problems breastfeeding and requires supplementation (with human milk or formula), administration with a bottle is generally against, especially in the first weeks of life | True | 67.2% | 80.9% | 47.4% | 80.3% | 64.4% | 65.0% |
| 15. In breastfed infants, frequent feeds decrease the risk of requiring phototherapy | True | 74.1% | 79.4% | 67.4% | 74.0% | 81.2% | 69.0% |
| 16. In healthy newborns, before the first feed in the delivery room, the newborn should be weighted and placed in a radiant crib to obtain the Apgar score and deliver adequate eye prophylaxis | False | 67.0% | 85.3% | 53.7% | 91.3% | 54.5% | 51.0% |
| 17. 17. In very preterm newborns (<32 weeks) the preferred food is maternal milk (fortified as needed), and the second best option is banked human milk, with administration of preterm formula used only as a last resort | True | 89.0% | 100% | 83.2% | 92.1% | 85.1% | 90.0% |
| 18. In the maternity ward, after 15 hours post birth, a full term newborn with normal weight that needs to be awakened to be breastfed in every feed is considered an infant at risk | False | 76.4% | 79.4% | 82.1% | 79.5% | 69.3% | 72.0% |
| Questionnaire 1. Second section | |||||||
| 19. Starting at 12 months, the nutrient content of human milk decreases compared to the first year of lactation | False | 69.8% | 66.2% | 66.3% | 74.0% | 71.3% | 72.0% |
| 20. If a lactating mother becomes pregnant, weaning is recommended due to an increased risk of miscarriage | False | 91.2% | 94.1% | 86.3% | 96.9% | 89.1% | 92.0% |
| 21. If a breastfed baby in good general health shows poor weight gain as the sole health problem, the first step is to supplement feeds with formula followed by re-evaluation | False | 72.4% | 82.4% | 53.7% | 86.6% | 69.3% | 70.0% |
| 22. From the first week of life, the 2 most reliable signs to assess milk intake are weight gain and urine output. | True | 95.3% | 95.6% | 95.8% | 94.5% | 98.0% | 95.0% |
| 23. Starting at 6 months, the number of feeds should be reduced to 2-3 a day, supplemented with complementary foods | False | 66.4% | 73.5% | 43.2% | 79.5% | 70.3% | 67.0% |
| 24. Kangaroo care should be available to all haemodynamically-stable preterm newborns regardless of gestational age, as it helps regulate body temperature, promotes breastfeeding and attachment and reduces the risk of infection | True | 94.7% | 95.6% | 90.5% | 95.3% | 96.0% | 98.0% |
| 25. The foremilk at the beginning of each feed is thinner | True | 67.4% | 69.1% | 53.7%< | 79.5% | 67.3% | 65.0% |
| 26. The drawing below represents correct latching
|
False | 75.1% | 69.1% | 70.5% | 79.5% | 71.3% | 84.0% |
| Questionnaire 1. Third section | |||||||
| 27. What are the current breastfeeding recommendation of the WHO? | Exclusive BF through 6 months and BF complemented with other foods through age 2 years or more, as the mother and child wish | 84.8% | 85.3% | 75.8% | 92.9% | 81.2% | 87.0% |
| 28. Which of the following actions is most important for a breastfeeding mother to do if she has cracked nipples? | Assess milk intake | 60.5% | 75.0% | 46.3% | 81.9% | 48.5% | 48.0% |
| 29. Two parents bring their 17-day-old baby to the emergency department due to crying. The baby is exclusively breastfed and everything was fine until present, but parents report that for the past 24 h the baby cries and wants to nurse very often, sometimes every 30-60 minutes. The baby is soothed at the breast and suckles vigorously. The infant is not ill-appearing, the weight gain is adequate and the physical examination is normal, but the mother feels that the infant is still hungry after feeds. How would you diagnose and treat this case? | Growth spurt. Observation of a feed, recommendation of feeding on demand and regular check-ups by paediatrician | 52.7% | 54.4% | 45.3% | 69.3% | 43.6% | 45.0% |
| Questionnaire 1. Fourth section | |||||||
| 30. Not evaluated | |||||||
| 31. What would you tell a pregnant woman that tells you during an appointment that she is considering formula feeding? | I would ask her to elaborate on the subject to understand her rationale and source of information and, with a respectful attitude, would encourage her to reconsider | 83.2% | 94.1% | 60.0% | 88.2% | 87.1% | 88.0% |
| 32. What do you think about newborn formula samples being given out for free to mothers in health care facilities? | This practice is in violation of the code for the marketing of breast milk substitutes | 40.4% | 48.5% | 12.6% | 59.8% | 40.6% | 33.0% |
| 33. A lactating mother has sought a consultation because she needs to start treatment with adalimumab for Crohn’s disease. Her gastroenterologist advised her to wean her 8-month-old baby because this treatment is important. Where can you check whether this drug is compatible or contraindicated for breastfeeding? | In a website I know | 48.4% | 83.8% | 38.9% | 58.3% | 31.7% | 4.0% |
| Questionnaire 1. Fifth section | |||||||
| 34. You are in the maternity ward and a nurse is worried about breastfeeding in a newborn, she thinks something is amiss and would like you to go observe a feed | I’ve done feed observations many times and feel capable of diagnosing the most common breastfeeding problems and offering solutions | 68.4% | 70.6% | 36.8% | 78.7% | 78.2% | 81.0% |
| 35. Do you think it is appropriate for mothers to breastfeed in public? | Yes | 88.1% | 91.2% | 74.7% | 92.9% | 93.1% | 90.0% |
| 36. Not evaluated | |||||||
| 37. Have you received any specific training on breastfeeding within your education programme or in the time you have been working in the maternity ward? | Yes | 57.2% | 57.4% | 12.6% | 88.2% | 59.4% | 61.0% |
| How many trainings? Mean (SD) | Average | 2-3 workshops | 1.7 (1.0) | 1.7 (0.7) | 2.6 (1.8) | 2.6 (1.9) | 2.5 (2.2) |
| What was the duration of these trainings? Mean (SD) | Average | Duration > 40 h< | 13.8 (15.4) | 8.0 (6.4) | 52.4 (77.5) | 44.7 (53.5) | 55.4 (98.2) |
| 38. What is the most important source of knowledge for breastfeeding? (multiple possible answers) | Highest proportion | 54.5% books/articles | 69.1% books/articles | 34.7% Co-workers | 70.1% Trainings | 56.4% Trainings | 55.0% Trainings |
| 39. Do you think training is required to diagnose and manage specific problems in breastfeeding? | Highest proportion: yes | 88.7% | 94.1% | 73.7% | 96.1% | 91.1% | 88.0% |
| 39.A. Why? (multiple possible answers) | Highest proportion Because it is part of my job |
84.6% | 89.1%< | 72.9% | 87.7% | 83.7% | 87.5% |
| 41. On a scale of 1 (not at all) to 5 (totally), rate how prepared you feel to diagnose and manage specific problems in breastfeeding | Mean | 3.33 (±0.93) | 3.6 SD (0.7) | 2.8 SD (1.1) | 3.5 SD (0.8) | 3.4 SD (0.9) | 3.4 SD (0.9) |

| Table 4. Percent distribution of answers for each item given by nurse assistant technicians | |||
|---|---|---|---|
| True | False | Did not answer | |
| 5. Breast milk is the best food for newborns as long as the mother is not malnourished | 83.5% | 15.6% | 0.9% |
| 6. In the second year of life, the quality of breast milk is very low | 16.0% | 80.2% | 3.9% |
| 7. Breastfeeding should be discontinued if the mother is taking any medication | 5.7% | 90.1% | 4.2% |
| 8. When breastfed infants cry due to hunger, breastfeeding should be supplemented with bottle feeding | 52.8% | 43.4% | 3.8% |
| 16. The first feed should take place right after birth | 90.6% | 7.5% | 1.9% |
| 17. Administration of normal saline with dextrose is needed to prevent hypoglycaemia in newborns | 16.5% | 81.6% | 1.9% |
| 18. Breastfeeding frequently reduces the risk of jaundice | 59.0% | 38.7% | 2.4% |
| 19. Many newborns need to be bottle-fed the first few days until the mother’s breast milk “comes in” | 54.2% | 43.9% | 1.9% |
| 20. Babies should be breastfed on demand | 96.2% | 2.8% | 0.9% |
| 21. Pacifiers interfere with and hinder breastfeeding | 60.4% | 37.3% | 2.4% |
| 22. Newborns should stay with their mothers day and night | 81.6% | 17.0% | 1.4% |
| 23. The first feed should take place in the first 3 hours post birth | 26.9% | 71.2% | 1.9% |
| 24. Breastfeeding should be discontinued if the mother develops mastitis | 24.1% | 73.6% | 2.4% |
| 25. The breasts should be washed before and after each feed | 53.8% | 44.8% | 1.4% |
| 26. Breastfeeding is contraindicated if the mother is hepatitis B-positive | 38.2% | 54.2% | 7.5% |
| 27. If the baby has diarrhoea, breastfeeding should be discontinued for a few days | 6.1% | 92.5% | 1.4% |
| 28. Breastfeeding should not be recommended for twins | 3.8% | 95.8% | 0.5% |

Level of knowledge by professional category
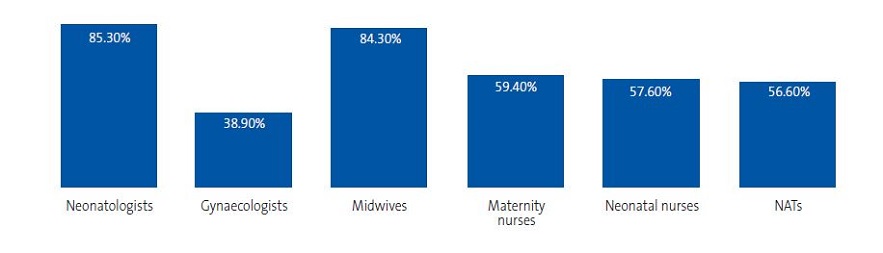
To analyse the level of knowledge, we set a minimum of 70% of correct answers (16.8 points) to define adequate knowledge. We based this threshold on the recommendations of the authors of the questionnaires,12 who categorised scores as: <50% very poor, 50%-70% inadequate, 70%-85% adequate, > 85% excellent. A study in Canada also set a threshold of 70% to define adequate knowlege.18 Neonatologists, midwives, nursing professionals in the maternity ward and NATs exhibited adequate knowledge. Gynaecologists did not achieve the recommended minimum number of correct answers (Tables 5 and 6, Figure 2).
| Table 5. Percent of professionals (NATs) that answered each question | ||
|---|---|---|
| % answers | ||
| 9. Have you ever heard of “baby-friendly hospitals”? | No | 36.3% |
| Yes | 61.8% | |
| Did not answer | 1.9% | |
| 10. Until what age is exclusive breastfeeding recommended at present? | 1 month | 0.0% |
| 2 months | 0.0% | |
| 3 months | 4.7% | |
| 4 months | 2.8% | |
| 5 months | 4.7% | |
| 6 months | 86.3% | |
| Did not answer | 1.4% | |
| 11. What should a normal newborn receive in addition to breast milk? | Nothing | 87.7% |
| Water | 4.2% | |
| 5% dextrose solution | 2.4% | |
| Formula | 4.7% | |
| Did not answer | 0.9% | |
| 12. What is the scientific meaning of the milk commonly known as “foremilk”? | Colostrum | 16.5% |
| Milk released at the beginning of each feed | 26.4% | |
| Milk of low nutritional value | 31.6% | |
| None of the above | 23.1% | |
| Does not answer | 2.4% | |
| 13. The amount of milk a woman can produce depends on: (you can check more than one) | Fluid intake | 42.0% |
| Breast size | 0.9% | |
| Frequency and vigour of feeds | 85.4% | |
| Emotional state | 49.1% | |
| 14. Mark which of these institutional practices is most effective in promoting breastfeeding in the maternity ward | Analgesia during delivery | 0.5% |
| Allow the mother to rest at night (remove the baby) | 2.8% | |
| Placing the baby at the breast in the first hour of life | 88.7% | |
| Placing baby at the breast every 3 hours during the night | 5.7% | |
| Stimulation of sucking with a pacifier | 0.9% | |
| Does not answer | 1.4% | |
| 15. Mark the most widely available and effective resource for nipple care | Moisturising creams | 1.4% |
| Alcohol and glycerine | 1.9% | |
| Correct latch-on | 77.4% | |
| Vigorous brushing | 0.0% | |
| Soap and water | 16.5% | |
| Does not answer | 2.8% | |

| Table 6. Overall score in each health professional category | |||||||
|---|---|---|---|---|---|---|---|
| Number of correct answers | |||||||
| Mean | Standard deviation | Median | 25th percentile | 75th percentile | Interquartile range | ||
| Professional category | Neonatologist | 19.47 | 3.92 | 20.00 | 18 | 22 | 4 |
| Gynaecologist | 15.24 | 4.62 | 15.00 | 12 | 19 | 7 | |
| Midwife | 20.03 | 3.58 | 21.00 | 19 | 23 | 4 | |
| Maternity nurse | 17.07 | 4.21 | 18.00 | 15 | 20 | 5 | |
| Neonatal nurse | 16.97 | 4.21 | 17.00 | 14 | 20 | 6 | |
| NAT | 16.93 | 3.70 | 17.00 | 15 | 20 | 5 | |

As can be seen in Table 7, we found a statistically significant difference in the number of correct answers between medical and nursing professionals (p = 0.01).
| Table 7. Total score for each health provider category | |||||||
|---|---|---|---|---|---|---|---|
| Number of correct answers | |||||||
| Mean | Standard deviation | Minimum | Median | Maximum | p-value | ||
| Profession | Physicians | 17.01 | 4.81 | 2.00 | 18.00 | 24.00 | 0.01 |
| Nurses | 18.19 | 4.23 | 7.00 | 19.00 | 24.00 | ||
| NATs | 16.93 | 3.70 | 4.00 | 17.00 | 24.00 | ||
| Total | 17.54 | 4.26 | 2.00 | 18.00 | 24.00 | ||

We found differences between professionals working in different hospitals (p = 0,033), with significant differences in the number of correct answers between hospital 7 and hospital 2, hospital 9 and hospital 2, and others) (Figura 3).
DISCUSSION
Given that we conducted a survey of breastfeeding knowledge addressed to all professionals employed in maternal and child health services in public hospitals of the SACYL based on the information of the database of this public health system, obtained a high response rate (60.9%), and the administered the survey in paper form and within the framework of clinical team meetings, we expect that our findings provide an accurate perspective regarding the knowledge of health providers on this subject.
In our review of the literature, we did not find a similar study conducted in Spain in the previous literature surveying different types of professionals or the entire collective of professionals involved in maternal and child care in all the public hospitals of an autonomous region. We did find studies involving specific types of professionals (resident physicians in paediatrics,10 paediatricians and residents in paediatrics,12 family physicians in Tenerife15 and various health providers in a single health district in the Valencian Community,16 but found no studies comparing the different categories of health professionals.
In the state of Sonora (Mexico),17 which has a very different health care system compared to ours, a similar study was conducted using an adaptation of the questionnaire developed by Temboury that also included residents in paediatrics and gynaecology.10 The questionnaire was administered by students of nutrition with random selection of a sample of physicians and nurses (327 responses). This study also concluded that the knowledge of breastfeeding of health professionals was inadequate, although the authors found that residents in paediatrics achieved better scores, which could be explained by previous training in educational workshops and conferences.
The study conducted in Canada to assess the knowledge, beliefs and attitudes of paediatricians, family physicians and final-year residents in paediatrics and family medicine18 found a score below 70% (the threshold for correct knowledge) in physicians, while the score of residents in paediatrics exceeded 70%.
To improve breastfeeding outcomes and offer solutions to the problems reported by mothers, it is important to evaluate the baseline level of knowledge. In pursuit of the same objectives and after we had started our study, the BFHI in Spain in 2015 published a document “Monitorización de la formación en atención a la lactancia materna mediante encuestas a profesionales” (Monitoring of training in the management of breastfeeding by surveying health professionals)13 proposing a tool for monitoring levels of training and educational needs and recommending a yearly survey of health professionals and the sample sizes to be obtained in different hospitals based on the number of beds. This proposal of the BFHI has not yet led to published results.
Our findings have highlighted different aspects for consideration. More than 80% of midwives and neonatologists had an “adequate” level of knowledge, but only 39% of gynaecologists reached this threshold, and no more than 40% of professionals in the remaining categories reached it either. Therefore, in two-thirds of the professional categories that are in contact with mothers that initiate breastfeeding, a substantial proportion of providers do not have knowledge at a level considered “adequate” in our study.
Our study revealed a lack of training in breastfeeding protocols and skills in the inpatient setting in NATs, who are professionals that carry out important tasks in this area. They were not aware of the significant impact of the introduction of bottles (items 8 and 19), challenges breastfeeding and the use of pacifiers (item 21), the importance of early skin-to-skin contact and the first feed (item 23) and did not recognised as erroneous something as basic as the need to wash the breasts before and after breastfeeding (item 25, 44.8%). Nearly half of these providers failed to reach the threshold for a level of knowledge defined as adequate.
Overall, our findings call for a reflection on the need to invest in training in breastfeeding across all involved categories of health professionals, especially gynaecologists, whose close involvement in the management of mothers at the time of breastfeeding initiation is of utmost importance. The level of knowledge in this collective of professionals was lowest of all.
Based on the answers to items 19, 21, 23, and 25 in questionnaire 1, we could state that despite the campaigns that have been implemented, the importance of exclusive breastfeeding through age 6 months and maintenance of breastfeeding combined with complementary foods through age 2 continues to be underestimated. There also seems to be a lack of awareness of the need to support mothers in addressing any challenges that may arise during this period.
Our findings confirm the frequent ignorance of the code on the marketing of breast milk substitutes and the tools that could help integrate breastfeeding in everyday clinical practice, such as the website e-lactancia.org and other digital applications, both of which have a direct impact on the prevalence of breastfeeding.
All professionals involved in maternal and child health services in hospitals in Castilla y Leon recognised their lack of specific training in breastfeeding, and nearly 90% considered this training important to be able to diagnose and successfully manage specific problems in breastfeeding, which they considered areas within the scope of their profession (item 39).
When we reviewed the official educational curricula for the degree in Medicine of the Universidad de Valladolid19,20 and for different medical specialties, we found that medicine students are only educated on the physiology of lactation and that the educational curriculum for the MIR residency in gynaecology did not include specific training on the physiology of lactation, although it did specify the need to train residents on breastfeeding-related problems in the postpartum period.21 The published official educational curriculum for NATs does not include any contents related to breastfeeding.22
The learning objectives of the official educational curricula published for paediatricians,23 nursing professionals,24-27 midwives28 and paediatric nurses29 include training in breastfeeding, although with a varying depth. Our findings show that there is a clear correlation between knowledge and the previous training of professionals, and highlight the need to improve the knowledge, skills and competencies in different types of health providers. There ought to be an emphasis on offering specific training in breastfeeding to those professionals that do not receive any during their formal education, such as gynaecologists and NATs.
Based on our findings, the knowledge of breastfeeding of the health care staff providing women’s and children’s services in Castilla y Leon in 2015 was lacking in aspects that are essential for the adequate management of breastfeeding: health providers lacked basic knowledge and skills with an impact on breastfeeding, made recommendations that did not promote breastfeeding (delaying the first feed, fixed feeding schedules, use of bottles and pacifiers), and when difficulties arose simply recommended discontinuation of breastfeeding, disregarding the wishes of the mother and the wellbeing of the infant. Having defined a score of 16.8 points (70% correct answers) as the threshold for adequate “knowledge”, we found that neonatologists, midwives and nurses and NATs employed in maternity or neonatal wards reached this threshold, while gynaecologists exhibited “inadequate” knowledge.
Breastfeeding is not a subject relevant solely to nursing professionals or those who have “an interest in the subject”, on the contrary, due to its importance for the promotion of public health, it is the duty of politicians and health care administrators to develop adequate educational strategies for inclusion in the curricula of the different health professions and joint training programmes for delivery in the maternal and child health units of all hospitals addressed to all the professionals involved in the care of women and infants (neonatologists, gynaecologists, midwives, nurses and NATs). In short, improving the prevalence of breastfeeding in the autonomous region of Castilla y Leon will require an investment on specific training in breastfeeding.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
ASCALEMA: Asociación Castellanoleonesa de Matronas · BFHI: Baby-Friendly Hospital Initiative · ECola: Encuesta sobre Conocimientos en Lactancia Materna · GSIYCF: Global Strategy for Infant and Young Child Feeding · NAT: nurse assistant technician · SACYL: Gerencia Regional de Salud de la Comunidad Autónoma de Castilla y León · UNICEF: United Nations Children's Fund · WHO: World Health Organization · 95 CI: 95% confidence interval.
ACKNOWLEDGMENTS
We would like to thank everyone who has contributed to this project with their work and support.
REFERENCES
- Aguayo Maldonado J, Cañedo Argüelles CA, Arena Ansótegui J, Canduela Martínez V, Flores Antón B, Gómez Papí A, et al. BFHI Calidad en la asistencia profesional al nacimiento y la lactancia. Informes, estudios e investigación 2011. Madrid: Ministerio de Sanidad, Política Social e Igualdad; 2011.
- Estévez-González M, Martell Cebrián D, Medina Santana R, García Villanueva E, Saavedra Santana P. Factores relacionados con el abandono de la lactancia materna. Anal Esp Pediatr. 2002;56:144- 51.
- Barriuso Lapresa LM, Sánchez-Valverde Visus F, Romero Ibarra C, Vitoria Comerzana JC. Epidemiología de la lactancia materna en el centro-norte de España. An Esp Pediatr 1999; 50: 237-243.
- Aguayo Maldonado J, Pasadas del Amo S, Ramírez Troyano A, Rello Yubero C, Martínez Rodríguez MT, Bonal Pitz P. La lactancia materna en Andalucía: resultados del estudio de prevalencia de la lactancia materna en Andalucía y los factores asociados a su duración en el primer año de vida. Seville: Junta de Andalucía, Consejería de Salud; 2005.
- Hernández-Aguilar M, Muñoz-Guillén A, Lasarte-Velillas JJ, García-Vera C, Díaz-Marijuan C, Martín-Calama J. La lactancia materna en la Comunidad Valenciana: Análisis multivariante de una encuesta a 6400 lactantes. Rev Pediatr Aten Primaria. 2004;6:19-37.
- Gartner LM, Morton J, Lawrence RA, Naylor AJ, O’Hare D, Schanler RJ, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496-506.
- Merewood A, Mehta SD, Chamberlain LB, Philipp BL, Bauchner H. Breastfeeding rates in US baby-friendly hospitals: results of a national survey. Pediatrics. 2005;116:628-34.
- Zakarija-Grković I, Burmaz T. Effectiveness of the UNICEF/WHO 20-hour course in improving health professionals’ knowledge, practices, and attitudes to breastfeeding: a before/after study of 5 maternity facilities in Croatia. Croat Med J.2010;51:396-405.
- Cattaneo A, Buzzetti R. Effect on rates of breast feeding of training for the baby friendly hospital initiative. BMJ. 2001;323:1358-62.
- Temboury Molina MC. Informe sobre el conocimiento de los residentes de Pediatría en el manejo de la lactancia materna. An Pediatr (Barc). 2003;58:263-7.
- Hernández Aguilar MT, Aguayo Maldonado J. La lactancia materna. Cómo promover y apoyar la lactancia materna en la práctica pediátrica. Recomendaciones del Comité de Lactancia de la AEP. An Pediatr (Barc). 2005;63:340-56.
- Gómez Fernández-Vegue M, Menéndez Orenga M. Validación de un cuestionario sobre conocimientos y habilidades en lactancia materna. An Pediatr (Barc). 2015;83:387-96.
- Monitorización de la formación en atención a la lactancia mediante encuestas a profesionales. In: UNICEF – Google Search. Available at https://bit.ly/2Roca9k
- Sacristán Martín AM, Lozano Alonso JE, Gil Costa M, Vega Alonso AT, Red Centinela Sanitaria de Castilla y León. Situación actual y factores que condicionan la lactancia materna en Castilla y León. Rev Pediatr Aten Primaria. 2011;13:33-46.
- Monge Zamorano, M, Garrido Martín, M. Conocimientos de los residentes de medicina de familia de Tenerife sobre la lactancia materna. BSCP Can Ped. 2007;31:7-1.
- Palomares Jimeno MJ, Labordena Barceló C, Sanantonio Valdearcos F, Agramunt Soler G, Nácher Fernández A, Palau Fuster G. Opiniones y conocimientos básicos sobre lactancia materna en el personal sanitario. Rev Pediatr Aten Primaria. 2001;3:393-402.
- Valenzuela H, Gabriel J, Trujillo EA, Lares AAO, Sánchez GAM, Hernández GÁ. Saberes de médicos y enfermeras de un hospital, acerca de las bondades de la lactancia. Rev Mex Pediatr. 2014;81:56-60.
- Pound CM, Williams K, Grenon R, Aglipay M, Plint AC. Breastfeeding knowledge, confidence, beliefs, and attitudes of Canadian physicians. J Hum Lact. 2014;30:298-309.
- Guía docente de la asignatura Obstetricia y Ginecología. In: Universidad de Valladolid [online] [accessed 24/05/2019]. Available at https://alojamientos.uva.es/guia_docente/uploads/2017/478/46294/1/Documento.pdf
- Guía docente de la asignatura Pediatría. In: Universidad de Valladolid [online] [accessed 24/05/2019]. Available at https://alojamientos.uva.es/guia_docente/uploads/2017/478/46306/1/Documento.pdf
- Ministerio de Sanidad y Política Social. Orden SAS/1350/2009, de 6 de mayo, por la que se aprueba y publica el programa formativo de la especialidad de Obstetricia y Ginecología. In: Boletín Oficial del Estado [online] [accessed 24/05/2019]. Available at http://www.boe.es/buscar/doc.php?id=BOE-A-2009-8882
- Ministerio de Educación y Ciencia. Real Decreto 558/1995, de 7 de abril, por el que se establece el currículo del ciclo formativo de grado medio correspondiente al título de Técnico en Cuidados Auxiliares de Enfermería. In: Boletín Oficial del Estado [online] [accessed 24/05/2019]. Available at https://www.boe.es/buscar/doc.php?id=BOE-A-1995-13592
- Ministerio de Sanidad y Consumo. ORDEN SCO/3148/2006, de 20 de septiembre, por la que se aprueba y publica el programa formativo de la especialidad de Pediatría y sus Áreas Específicas. In: Boletín Oficial del Estado [online] [accessed 24/05/2019]. Available at https://boe.vlex.es/vid/formativo-Pediatría-especificas-23787972
- Proyecto docente de Enfermería en la Infancia y Adolescencia. Campus Soria. In: Universidad de Valladolid [online] [accessed 24/05/2019]. Available at https://alojamientos.uva.es/guia_docente/uploads/2017/476/46227/1/Documento.pdf
- Proyecto docente de Enfermería en la Infancia y Adolescencia. Campus Valladolid. In: Universidad de Valladolid [online] [accessed 24/05/2019]. Available at https://alojamientos.uva.es/guia_docente/uploads/2017/475/46182/1/Documento.pdf
- Proyecto docente de la asignatura Enfermería en salud sexual y reproductiva. Campus de Soria. In: Universidad de Valladolid [online] [accessed 24/05/2019]. Available at https://alojamientos.uva.es/guia_docente/uploads/2017/476/46229/1/Documento.pdf
- Proyecto docente de la asignatura Enfermería en salud sexual y reproductiva. Campus Valladolid. In: Universidad de Valladolid [online] [accessed 24/05/2019]. Available at https://alojamientos.uva.es/guia_docente/uploads/2017/475/46184/1/Documento.pdf
- Ministerio de Sanidad y Política Social. Orden SAS/1349/2009, de 6 de mayo, por la que se aprueba y publica el programa formativo de la especialidad de Enfermería Obstétrico-Ginecológica (Matrona)… In: Boletín Oficial del Estado [online] [accessed 24/05/2019]. Available at https://www.boe.es/diario_boe/txt.php?id=BOE-A-2009-8881
- Ministerio de Sanidad y Política Social. Orden SAS/1730/2010, de 17 de junio, por la que se aprueba y publica el programa formativo de la especialidad de Enfermería Pediátrica. In: Boletín Oficial del Estado [online] [accessed 24/05/2019]. Available at https://www.boe.es/diario_boe/txt.php?id=BOE-A-2010-10365