Vol. 20 - Num. 77
Original Papers
Effectiveness of the Bicisalud programme in a group of schoolchildren with excess weight
Enrique Rodríguez-Salinas Péreza, José Ignacio Leguina Aranzamendib, María Rosalía Martín Canoc, David Bescos Delgadod, Gonzalo de las Casas Cámarae
aPediatra. CS Colmenar Viejo Norte. Colmenar Viejo. Madrid. España.
bCiencias Biológicas. Madrid. España.
cMédico de Familia. CS Canillejas. Madrid. España.
dTécnico de Animación de Actividades Físicas y Deportivas. Estudiante de Ciencias de la Actividad Física y el Deporte. Madrid. España.
eMedicina Preventiva y Salud Pública. Hospital Universitario Rey Juan Carlos. Móstoles. Madrid. España.
Correspondence: E Rodríguez-Salinas. E-mail: erodriguez-salinas@pap.es
Reference of this article: Rodríguez-Salinas Pérez E, Leguina Aranzamendi JI, Martín Cano MR, Bescos Delgado D, de las Casas Cámara G. Effectiveness of the Bicisalud programme in a group of schoolchildren with excess weight. Rev Pediatr Aten Primaria. 2018;20:53-63.
Published in Internet: 28-02-2018 - Visits: 24272
Abstract
Introduction: as we face the worrisome burden of disease resulting from the increase in sedentary habits and excess weight in children, multidisciplinary interventions are recommended to promote healthy dietary and physical activity habits in the entire family. The Bicisalud programme has been developed in accordance with these recommendations. The main objective of this article was to present the outcomes of this programme.
Methods: we conducted a quasi-experimental study where we analysed the variables at three time points: before, right after, and three months after the intervention. Between 2016 and 2017, a total of 47 children with overweight or obesity participated in a complex programme revolving around group bicycle rides in the countryside led by sports and health specialists. The programme also included educational activities on nutrition and exercising, among other topics. The primary outcome variable was physical fitness in its three main dimensions. The secondary outcome variables included anthropometric values, habits and physical self-perception.
Results: the programme achieved a statistically significant improvement in the three dimensions of physical fitness and in waist circumference in the assessment made immediately after completion of the programme. This effect was only sustained in the assessment after the three months of summer holidays in flexibility. The changes in the remaining variables were not statistically significant at any time point.
Conclusions: Bicisalud achieved a moderate but short-lived improvement in the primary outcome variables. There is evidence suggesting that longer programmes promoting the regular use of bicycles may be more effective in preventing and managing sedentary lifestyles, excess weight and their consequences.
Keywords
● Bicycling ● Childhood obesity ● Exercise ● Overweight ● Sedentary lifestyleINTRODUCTION
The growing burden of disease associated with excess weight in the paediatric population, along with the increase in sedentary lifestyles, may lead to the collapse of many health systems worldwide, in addition to producing significant suffering and costs in affected individuals.1,2
The extent of the burden of disease is due, on one hand, to the considerable prevalence of excess weight, of more than 40% in the pre-adolescent population of countries such as Spain3 and with significant variations based on geographical area and social variables,4,5 and, on the other hand, to the high morbidity and mortality resulting from the combination of obesity with sedentary habits, which is a risk factor for cardiovascular disease, metabolic syndrome, diabetes, orthopaedic, respiratory and psychological problems, and is also associated with a lower life expectancy.6-8 Obese children have a poor self-image and express feelings of inferiority and social rejection, and are at high risk of depression and anxiety. 9-11.
This problem is difficult to resolve once it has developed, and there is a clear correlation between overweight and obesity in childhood and in adulthood.7,12
The World Health Organization,1 health authorities and scientific associations have raised an alarm and proposed countless recommendations, guidelines, strategies and consensus documents for the treatment of what is by now considered a serious and significantly challenging epidemic.13-17 In Spain, the Strategy for Nutrition, Physical Activity and the Prevention of Obesity was launched 2005.18 Its aim is to raise awareness in the community of the problems associated with obesity and to promote every possible intervention that may contribute to the development of healthy dietary habits and regular physical activity, especially in children and youth.
Obesity continues to be one of the most challenging problems in everyday clinical practice. There is evidence that interdisciplinary interventions for treatment of obesity in children and adolescents with the collaborative and coordinated involvement of professionals from different fields (psychologists, fitness and sports professionals, nutritionists, physicians) are more effective than interventions based on a single approach.19-23
The current clinical practice guidelines for the management of child and adolescent obesity recommend the development of community-based programmes to promote healthy lifestyles, a healthy diet, and the practice of physical activity.13,15-17
One of the most significant challenges that arises is the lack of adherence to treatment and prevention programmes. This is related to the difficulty in gaining the motivation necessary to change lifestyle habits.21,24
When it comes to fostering the habit of exercising in children, it is essential to make physical activity fun. Many aspects of outdoor bicycle riding may further this goal. In addition to its association with exercise, bicycles have always been desirable toys for children. It promotes autonomy in everyday travelling and environmental awareness, as it does not cause pollution.25
Studies on the effects of bicycle riding interventions on cardiovascular health and the prevention and treatment of excess weight and the associated comorbidities have focused on the daily commute to work in adults or to school in children.26-36 There is solid evidence that programmes that promote daily bicycle riding offer benefits that far outweigh the risks.37-44
On the foundation of the recommendations of the guidelines and strategies mentioned above, we developed a multidisciplinary programme called Bicisalud (“Bikehealth”) based on group bicycle rides through nature combined with practical workshops on how to develop healthy lifestyles. The aim of our study was to assess the impact of this programme on the physical skills and body composition of schoolchildren with excess weight, as well as on their physical self-perception and their dietary and exercising habits.
MATERIALS AND METHODS
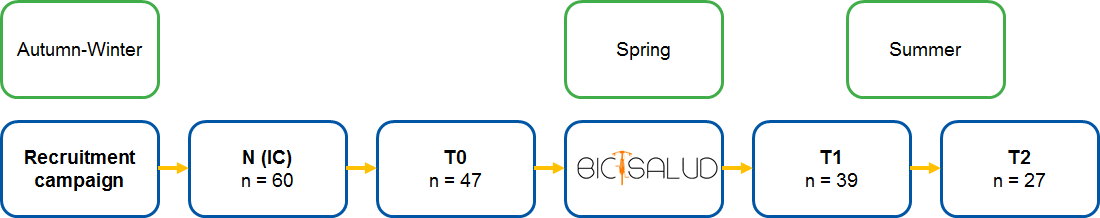
We conducted a quasi-experimental study with assessment of outcome variables pre and post intervention (Fig. 1). The study took place between summer 2015 and summer 2017 in Colmenar Viejo, a town with 48 000 inhabitants north of Madrid in an area with an extensive network of country roads and a low volume of motor vehicle traffic, which allows their use for both agricultural use and recreational exercise on foot or on bicycle. The first summer, before starting the programme, we contacted local and regional health care institutions to make the project known and to obtain the approval of the competent ethics committee.
| Figure 1. Flow chart of the project (2015-17) |
|---|
 |

Sample: the inclusion criteria for the programme were: age 8 to 14 years, body mass index (BMI) at or above the 90th percentile based on the growth tables of the 1988 study by Hernández et al., knowing how to ride a bicycle, and parental authorization through signing of an informed consent form. The exclusion criteria were: chronic or subacute underlying disease where physical activity is contraindicated, concurrent participation in other fitness programmes, or current pharmacological or surgical treatment for obesity.
Since gathering a group of volunteers proved difficult, we implemented an intensive informational campaign in the fall-winter season: in the primary care centres of the area; in the community, with the support of the authorities, by hanging posters and distributing flyers printed by the city council in mailboxes (5000 flyers and 80 posters) (Fig. 2); in the local press and radio stations; in pharmacies, recreational centres, and in schools, visiting the classrooms and using that opportunity to provide education on healthy lifestyle habits to more than 2400 students over the two seasons. Based on the available resources and taking into account potential losses to followup, we decided that we needed to have a group of 45 participants.
| Figure 2. Sample of the poster printed by the City Council of Colmenar Viejo |
|---|
 |

Outcome variables
Primary outcome: physical fitness in its three main aspects, aerobic endurance, strength and flexibility, assessed based on the Eurofit battery of tests.45 Participants were assessed at three time points: T0, T1 and T2 (Fig. 1) in the sports grounds of a local high school by the same observers, a paediatrician and 3 sports technicians, who were blinded to the results obtained by participants in previous assessments.
After a short warm-up, the flexibility of the trunk and hamstrings was assessed with the classic sit and reach test, the explosive leg power with the broad jump test, and aerobic fitness or endurance with the Course Navette test. Flexibility was measured with a testing box (flexometer); participants were allowed three attempts and the best result was recorded. The strength test was performed with the aid of a measuring tape and three attempts were also allowed, recording the best result. In the endurance test, four cones and measuring tape were used to demarcate a 20 m course and 1 computer to run the test protocol, recording the number of back-and-forth cycles completed by the participant and dividing it by 2.
Secondary outcome variables: BMI; waist circumference; self-concept; dietary and physical activity habits.
Another 2 observers in the primary care centre, physicians who were also blinded to the results of previous tests, carried out measurements at the three time points (T0, T1 and T2), of weight and height with the participants wearing light clothing and barefoot, and of the waist circumference with the tape at the level of the umbilicus, using the same tools every time: scale, stadiometer and flexible measuring tape accurate to 100 g, 1 mm and 5 mm, respectively.
We calculated BMIs, their percentiles and their distance from the mean in standard deviations (z-scores) with the virtual calculator of the EndocrinoPed website.46 We assessed psychological and behavioural variables by means of a brief self-perception questionnaire (Cuestionario de Autoconcepto Abreviado [CAF])47 and the Kreceplus battery of tests on diet and sedentary habits.48
Independent variable
The independent variable was the implementation of the multicomponent group education programme known as Bicisalud. It included physical activity and interactive education on healthy nutrition and environmental variables.
The physical activity selected for the programme was cycling. Participants had to wear a helmet and a reflective vest during the rides, as well as adhere to traffic rules. We managed to obtain up to 9 donated bicycles to lend to participants that did not own any. The programme consisted of group bicycle rides through the countryside of increasing difficulty, outside school hours, in periods of 12 weeks, and with a total of 24 sessions per season (Table 1). Participants were divided into 2 groups by age, level of fitness and bicycle riding skills. The group comprised of younger or less fit participants went on shorter and easier rides (6-8 km) compared to the group with older or more skilled participants (10-12 km). Both groups were led and supported by at least 2 physical education or health care professionals. Relatives or other local volunteers also participated in nearly every ride.
| Table 1. Summary of the progression of the bicycle riding activities in the Bicisalud programme | ||||
|---|---|---|---|---|
| Week | Sessions/week | Duration (min) | Terrain | Difficulty |
| 1-3 | 1 | 60 | Easy, flat | Light |
| 4-6 | 2 | 60 | Variable | Moderate |
| 7-9 | 3 | 90 | Challenging | Vigorous |
| 10-12 | 3 | 90 | Difficult | Vigorous |

In order to reinforce the educational nature of the programme, there were visits to different natural sites and relevant institutions in the community, such as the Dehesa de Navalvillar, with its archaeological remains and diversity of birds, the animal shelter, the day care centre for individuals with disabilities or the Casa Museo de la Villa. There were also three informational workshops held at the primary care centre on the subjects of nutrition, shopping for healthy foods, and risks and benefits of bicycle riding which the families were also asked to attend. The workshop on nutrition was led by a nutritionist, a biologist, a family physician and four nurses. It was divided into two simultaneous sessions, one for children and the other for their families. The workshop on healthy food shopping was led by a paediatrician and included a visit to the fruit, vegetables and fish stands of a nearby market. The workshop on bicycle riding was taught by the technicians that led the rides. A phone messaging group was created to facilitate participation and organise outings or report relevant issues.
After each outing to the countryside, the group shared a healthy afternoon snack consisting of seasonal fruit.
Statistical analysis
We performed a univariate descriptive analysis of the sample. We have summarised quantitative variables with measures of central tendency (mean or median) and of dispersion (standard deviation or interquartile range). After verifying the normality of their distributions, we compared the means of quantitative variables at the three time points by repeated measures ANOVA (testing the assumption of homogeneity of variance), and compared the three pairs of time points by means of the Student t test for paired samples with the Bonferroni correction, defining statistical significance as a p-value of less than 0.016. We performed all the analyses with the statistical software SPSS® version 18.
RESULTS
Of the 60 applicants (26 in 2016 and 34 in 2017) for who we obtained informed consent for participation in Bicisalud, 47 met the inclusion criteria (25 + 22) and, after measurement of the primary and secondary outcome variables at baseline (T0), started the programme of activities that run through two springs with a flexible calendar of outings and workshops that were scheduled as the programme advanced. The mean age at initiation of the programme was 11.2 years (SD, 1.52); 57.45% of participants were male, and 42.55% female. The median number of events that participants attended was 16 (interquartile range: 11-19).
Fig. 1 shows the sample at each time point (T0, T1, T2), illustrating the losses to followup. Table 2 provides a descriptive summary of the variables under study. The purpose of this table is merely to document the impact of the losses to followup, as the corresponding data had to be removed from the analyses presented in Tables 3 and 4.
| Table 2. Results (mean [SD]) of the measurements of the different variables at the three time points | |||
|---|---|---|---|
| T0 (n = 47) | T1 (n = 39) | T2 (n = 27) | |
| AE | 9.65 (4.25) | 12.95 (5.20) | 10.87 (4.67) |
| FL | 18.02 (7.01) | 19.77 (8.43) | 21.04 (8.01) |
| ES | 121.37 (21.7) | 129.21(21.76) | 126.65 (19.92) |
| BMI | 25.15 (2.58) | 24.60 (2.72) | 25.45 (3.2) |
| BMI-z | 2.38 (0.75) | 2.12 (0.83) | 2.34 (1.0) |
| WC | 86.96 (8.23) | 84.71 (8.24) | 88.46 (10.7) |
| KN | 6.89 (1.86) | 7 (1.92) | 6.04 (2.36) |
| KA | 5.83 (2.09) | 5.9 (2.16) | 5.59 (2.22) |
| SP | 28.02 (4.02) | 29.67 (4.50) | 28.81 (4.65) |

| Table 3. Results (mean [SD]) of the measurements of the different variables at the three time points | ||||
|---|---|---|---|---|
| T0 | T1 | T2 |
P* |
|
| Variables | M (SD) | M (SD) | M (SD) | |
| AE n = 26 | 10.4 (5.1) | 13.7 (5.6) | 10.8 (4.7) | .003 |
| FL n = 26 | 19.1 (7.2) | 20.6 (8.7) | 21.0 (8.0) | .012 |
| ES n = 26 | 122.9 (18.8) | 129.2 (23.1) | 126.7 (19.9) | .014 |
| SP n = 27 | 28.0 (4.3) | 29.9 (4.5) | 28.8 (4.7) | .103 |
| Weight n = 27 | 55.1 (11.3) | 55.6 (11.7) | 58.5 (12.4) | <.0001 |
| Height n = 27 | 147 (9.4) | 149.5 (9.5) | 150.8 (9.2) | <.0001 |
| BMI n = 27 | 24.9 (2.7) | 24.6 (2.9) | 25.5 (3.2) | <.0001 |
| BMI-z n = 27 | 2.3 (0.8) | 2.1 (0.9) | 2.34 (1.0) | .002 |
| WC n = 27 | 87.2 (8.9) | 84.9(9.0) | 88.5 (10.7) | <.0001 |
| KN n = 27 | 6.6 (1.8) | 7.0 (1.7) | 6.0 (2.4) | .036 |
| KA n = 27 | 5.5 (2.4) | 5.7 (2.4) | 5.6 (2.2) | .81 |

| Table 4. Results (DM [SD]) of the measurements of the different variables at the three time points | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| T1-T0 | T2-T1 | T2-T0 | |||||||
| Variables | DM (SD) | 95 CI | P* | DM (SD) | 95 CI | P* | DM (SD) | 95 CI | P* |
| AE n = 26 | 3.3 (4.5) | 1.5 to 5.1 | .001 | -2.8 (4.7) | -4.7 to 0.92 | .005 | 0.44 (4.5) | -1.4 to 2.3 | .622 |
| FL n = 26 | 1.5 (2.9) | 0.3 to 2.7 | .015 | 0.4 (2.7) | -0.7 to 1.5 | .43 | 1.9 (3.1) | 0.7 to 3.2 | .004 |
| ES n = 26 | 6.3 (9.7) | 2.2 to 10.3 | .004 | -2.5 (11.3) | -7.1 to 2.0 | .264 | 3.7 (9.9) | -0.25 to 7.7 | .065 |
| SP n = 27 | 1.9 (4.3) | 0.2 to 3.6 | .032 | -1.1 (5.3) | -3.2 to 0.9 | .287 | 0.8 (4.7) | -1.1 to 2.6 | .399 |
| Weight n = 27 | 0.5 (2.4) | -0.4 to 1.5 | .257 | 2.9 (1.7) | 2.3 to 3.6 | .001 | 3.5 (2.9) | 2.3 to 4.7 | .001 |
| Height n = 27 | 1.6 (0.7) | 1.3 to 1.9 | .001 | 1.4 (1.3) | 0.9 to 1.9 | .001 | 2.9 (1.3) | 2.4 to 3.5 | .001 |
| BMI n = 27 | -0.3 (1.1) | -0.7 to 0.2 | .185 | 0.8 (0.8) | 0.5 to 1.2 | .001 | 0.5 (1.3) | 0.04 to 1.0 | .036 |
| BMI-z n = 27 | -0.2 (0.4) | -0.36 to 0.04 | .019 | 0.20 (0.30) | 0.09 to 0.32 | .001 | 0.01 (0.5) | -0.17 to 0.18 | .947 |
| WC n = 27 | -2.2 (4.4) | -3.9 to 0.5 | .013 | 3.5 (3.7) | 2.0 to 4.9 | .001 | 1.2 (4.5) | -0.5 to 3.0 | .164 |
| KN n = 27 | 0.4 (1.8) | -0.32 to 1.06 | .284 | -0.92 (1.7) | -1.6 to 0.25 | .009 | -0.55 (2.0) | -1.3 to 0.22 | .154 |
| KA n = 27 | 0.22 (1.8) | -0.48 to 0.93 | .523 | -0.11 (1.9) | -0.88 to 0.66 | .77 | 0.11 (1.6) | -0.53 to 0.75 | .725 |

These tables present the results of the statistical analysis of the subset of participants that completed the programme, that is, the 27 children (44.5% male and 55.5% female) assessed at all 3 time points, although one of the girls missed one fitness assessment.
With the exception of the physical self-perception and Kreceplus-physical activity scores, we found differences in the means of all other variables at some point.
When we compared the moment when the intervention had just ended (T1) with baseline (T0), we found increases in strength, aerobic endurance, flexibility and height, and a decrease in waist circumference. However, when we compared the time point at 3 months post intervention (T2) with the end of the intervention (T1), we found decreases in aerobic endurance and the Kreceplus-Nutrition score, as well as increases in weight, BMI (and BMI z-score) and waist circumference; the height also continued to increase. The changes observed between the T0 baseline time point and T2 were increases in flexibility, weight and height.
In short, implementation of the programme was associated with a significant and rapid improvement in the primary endpoint (physical fitness), which was not sustained through the three months of the summer holidays except for flexibility, which remained improved in most of participants. The changes found in other variables were not statistically significant.
During the two periods of scheduled activities (three months/participant), there were only a few falls and minor accidents, and none of them resulted in significant injury or changes in participation.
We ought to mention that the development of the Bicisalud programme provides an example of an interactive intervention with very positive aspects—albeit not measurable ones—involving the collaboration of primary care settings, elementary and secondary schools, sports organizations, paediatric participants and their families, recreational counsellors and cultural, social and environmental groups in the context of what has been come to be known as social health promotion networks.49
This experience has led to the allocation of funds in the town council budget for the implementation of a new Bicisalud programme in the next season, which this time will be open to all schoolchildren regardless of their BMI.
DISCUSSION
Bicisalud succeeded in improving the physical fitness of participating children, fulfilling its primary objective, although these gains were short-lived. The effect of the programme disappeared in the followup assessment performed after the summer holidays, except for flexibility, which continued to be significantly better compared to baseline.
When we asked participants about the activities they had engaged in during summer and specifically about bicycle riding or other types of exercising, most replied that they had for the most part remained inactive during summer and that they had only used their bicycle occasionally.
This is consistent with the considerable increase of sedentary habits worldwide, which is one of the key aetiological factors in the growing epidemic of excess weight and its deleterious consequences.50-52 It is clear that children are being entertained at increasingly early ages with activities such as hypnotically watching the smartphones of their parents, until they get one of their own, also increasingly early. This is why the Bicisalud programme, while having other components, focuses on the promotion of active and fun leisure activities involving bicycle riding with peers of similar characteristics.
The decreases achieved in some of the secondary outcome variables, such as the BMI, which may be the most socially desirable goal, were not statistically significant and were not sustained through the summer holidays. On the other hand, along the same lines, there was a statistically significant improvement in waist circumference, which is also an indicator of excess body fat, even if it had returned to baseline during the relatively inactive summer. Other authors have reported similar difficulties in pursuing these goals with interventions of broader scope.21,23,28,51,53
We also found moderate improvements in physical self-perception that did remain after summer, although the differences were not significant at any point. Low self-esteem is an important associated problem in children with overweight or obesity, which is both cause and effect of them, and while improving it was only a secondary objective in our programme, we would have wanted to find a more consistent improvement in this variable.9-11
The areas where Bicisalud achieved the least favourable results were dietary and physical activity habits, assessed by the validated and well-known Kreceplus questionnaires.19,21,24,48 A possible explanation of the ineffectiveness of the programme on these areas could be that achieving even small changes in lifestyle habits requires more intensive and longer-lasting interventions through various channels of communication, especially when the change requires the involvement of the entire family. We also need to take into account social pressure factors that facilitate sedentary leisure activities and deplorable dietary habits.54
The recruitment of participants was one of the main barriers to the success of the Bicisalud project. It is not easy for children with excess weight to take the initiative of enrolling and thus acknowledge their problem openly in the community. Due to this difficulty, we had to conduct the study over two different periods to achieve the necessary sample size. On the other hand, the efforts required to overcome this challenge resulted in increased cohesion and enthusiasm in the group of children and collaborators.
Despite the fun and adventurous nature of each ride and the variety of the activities and the people involved, which helped add interest to the programme, there were significant losses to followup that may have affected the final results.
In conclusion:
- Bicisalud is an innovative and promising programme with a specific structure to address the serious problem of inactivity and excess weight in the preadolescent population.
- It has achieved good short-term outcomes in physical fitness, although only its effects on flexibility were sustained in the medium term.
- It would be interesting to replicate the study with larger samples and attempting to increase motivation to minimise dropouts during the study period, which may have interfered with the hypothesised scenario of minimal losses.
- A key aspect for designing more effective studies in the future is to extend the duration of the intervention and, above all, to succeed in making the use of the bicycle or other active means of transport an everyday habit in the lives of schoolchildren, their families, and the members of their communities.
APPENDICES
We have added three appendices that are available in the webpage of the journal:
- Acknowledgments (Appendix 1).
- Table with structured literature summaries (Appendix 2).
- Photo album (Appendix 3).
CONFLICTS OF INTEREST
The authors are habitual bicycle users, riding regularly for commuting and exercising.
ABBREVIATIONS
BMI: body mass index • CAF: brief self-perception questionnaire • SD: standard deviation.
FUNDING
AMPap Grant for Research in Paediatrics and Primary Care. Town Council of Colmenar Viejo. Own funding.
REFERENCES
- Estrategia mundial sobre régimen alimentario, actividad física y salud. Sobrepeso y obesidad infantiles. In: World Health Organization [online] [accessed 27/02/2018]. Available at www.who.int/dietphysicalactivity/childhood/es/
- Ding D, Lawson KD, Kolbe-Alexander TL, Finkelstein EA, Katzmarzyk PT, van Mechelen W, et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet. 2016;388:1311-24.
- Estudio ALADINO 2015: Estudio de Vigilancia del Crecimiento, Alimentación, Actividad Física, Desarrollo Infantil y Obesidad en España 2015. In: Agencia Española de Consumo, Seguridad Alimentaria y Nutrición. Ministerio de Sanidad, Servicios Sociales e Igualdad [online] [accessed 27/02/2018]. Available at http://www.aecosan.msssi.gob.es/AECOSAN/docs/documentos/nutricion/observatorio/Estudio_ALADINO_2015.pdf
- Sánchez Echenique M. Aspectos epidemiológicos de la obesidad infantil. Rev Pediatr Aten Primaria Supl. 2012;21:S9-14.
- Ninatanta Ortiz JA, Núñez Zambrano LA, García Flores SA, Romaní Romaní F. Factores asociados a sobrepeso y obesidad en estudiantes de educación secundaria. Rev Pediatr Aten Primaria. 2017;19:209-21.
- Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329-37.
- Steinberger J, Moran A, Hong CP, Jacobs DR,Jr, Sinaiko AR. Adiposity in childhood predicts obesity and insulin resistance in young adulthood. J Pediatr. 2001;138:469-73.
- Paffenbarger RS Jr, Kampert JB, Lee IM, Hyde RT, Leung RW, Wing AL. Changes in physical activity and other lifeway patterns influencing longevity. Med Sci Sports Exerc. 1994;26:857-65.
- Erermis S, Cetin N, Tamar M, Bukusoglu N, Akdeniz F, Goksen D. Is obesity a risk factor for psychopathology among adolescents? Pediatr Int. 2004;46:296-301.
- D’Autume C, Musher-Eizenman D, Marinier E, Viarme F, Frelut ML, Isnard P. Eating behaviors and emotional symptoms in childhood obesity: a cross-sectional exploratory study using self-report questionnaires in 63 children and adolescents. Arch Pediatr. 2012;19:803-10.
- Ortega MA, Muros JJ, Palomares J, Martín JA, Cepero M. Influencia del índice de masa corporal en la autoestima de niños y niñas de 12-14 años. An Pediatr (Barc). 2015;83:311-7.
- Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;331:929.
- Grupo de trabajo de la Guía de Práctica Clínica sobre la Prevención y el Tratamiento de la Obesidad Infantojuvenil. Centro Cochrane Iberoamericano (coordinator). Guía de Práctica Clínica sobre la Prevención y el Tratamiento de la Obesidad Infantojuvenil [summary]. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad y Política Social. Agència d´Avaluació de Tecnologia i Recerca Mèdiques; 2009. Guías de Práctica Clínica en el SNS: AATRM N. 2007/25. Available at http://www.guiasalud.es/GPC/GPC_452_obes_infantojuv_AATRM_compl.pdf
- Waters E, de Silva-Sanigorski A, Burford BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;3:CD001871.
- Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E, et al. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ. 2007;176:S1-13.
- National Clinical Guideline Centre. Obesity: identification, assessment and management of overweight and obesity in children, young people and adults. London: National Institute for Health and Care Excellence (NICE); 2014.
- August GP, Caprio S, Fennoy I, Freemark M, Kaufman FR, Lustig RH, et al. Prevention and treatment of pediatric obesity: an endocrine society clinical practice guideline based on expert opinion. J Clin Endocrinol Metab. 2008;93:4576-99.
- Estrategia para la Nutrición, Actividad Física y Prevención de la Obesidad (NAOS). In: Agencia Española de Consumo, Seguridad Alimentaria y Nutrición. Ministerio de Sanidad, Servicios Sociales e Igualdad [online] [accessed 27/02/2018]. Available at http://www.aecosan.msssi.gob.es/AECOSAN/web/nutricion/seccion/estrategia_naos.htm
- Gussinyer S, Garcia-Reyna NI, Carrascosa A, Gussinyer M, Yeste D, Clemente M, et al. Cambios antropométricos, dietéticos y psicológicos tras la aplicación del programa “niños en movimiento” en la obesidad infantil. Med Clin (Barc). 2008;131:245-9.
- Serra-Paya N, Ensenyat A, Blanco A. Intervención multidisciplinar y no competitiva en el ámbito de la salud pública para el tratamiento del sedentarismo, el sobrepeso y la obesidad infantil: Programa NEREU. Educación Física y Deportes. 2014;117:7-22.
- Rajmil L, Bel J, Clofent R, Cabezas C, Castell C, Espallargues M. Intervenciones clínicas en sobrepeso y obesidad: revisión sistemática de la literatura 2009-2014. An Pediatr (Barc). 2017;86:197-212.
- Fundación Thao. Programa Thao-salud infantil [online] [accessed 27/02/2018]. Available at https://programathao.com/que-es/
- Pérez Solís D, Díaz Martín JJ, Álvarez Caro F, Suárez Tomás I, Suárez Menéndez E, Riaño Galán I. Efectividad de una intervención escolar contra la obesidad. An Pediatr (Barc). 2015;83:19-25.
- Gorrotxategi Gorrotxategi P, Leizaola Olarreaga L, Solorzano Sánchez C, García Conde G, Aguirre Sorondo B, Totoricaguena Imaz A, et al. Protocolo del estudio: abordaje del sobrepeso en Atención Primaria. Papel de la entrevista motivacional. Rev Pediatr Aten Primaria. 2014;16:e199-e207.
- Rissel CE, New C, Wen LM, Merom D, Bauman AE, Garrard J. The effectiveness of community-based cycling promotion: findings from the Cycling Connecting Communities project in Sydney, Australia. Int J Behav Nutr Phys Act. 2010;7:8.
- Grøntved A, Koivula RW, Johansson I, Wennberg P, Østergaard L, Hallmans G, et al. Bicycling to work and primordial prevention of cardiovascular risk: a cohort study among Swedish men and women. J Am Heart Assoc. 2016;5:1-12.
- Chillón P, Villén-Contreras R, Pulido-Martos M, Ruiz JR. Desplazamiento activo al colegio, salud positiva y estrés en niños españoles. SPORT TK. 2017;6:117-24.
- Rosenberg DE, Sallis JF, Conway TL, Cain KL, McKenzie TL. Active transportation to school over 2 years in relation to weight status and physical activity. Obesity (Silver Spring). 2006;14:1771-6.
- Macridis S, García Bengoechea E. Adoption of safe routes to school in Canadian and the United States contexts: best practices and recommendations. J Sch Health. 2015;85:558-66.
- De Nazelle A, Nieuwenhuijsen MJ, Antó JM, Brauer M, Briggs D, Braun-Fahrlander C, et al. Improving health through policies that promote active travel: a review of evidence to support integrated health impact assessment. Environ Int. 2011;37:766-77.
- Ostergaard L, Børrestad LA, Tarp J, Andersen LB. Bicycling to school improves the cardiometabolic risk factor profile: a randomised controlled trial. BMJ Open. 2012;2.pii:e001307.
- Østergaard L, Grøntved A, Børrestad LA, Froberg K, Gravesen M, Andersen LB. Cycling to school is associated with lower BMI and lower odds of being overweight or obese in a large population-based study of danish adolescents. J Phys Act Health. 2012;9:617-25.
- Villa-González E, Ruiz JR, Ward DS, Chillón P. Effectiveness of an active commuting school-based intervention at 6-month follow-up. Eur J Public Health. 2016;26:272-6.
- Lu W, McKyer EL, Lee C, Ory MG, Goodson P, Wang S. Children’s active commuting to school: an interplay of self-efficacy, social economic disadvantage, and environmental characteristics. Int J Behav Nutr Phys Act. 2015;12:29.
- Lubans DR, Boreham CA, Kelly P, Foster CE. The relationship between active travel to school and health-related fitness in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. 2011;8:5.
- Andersen LB, Lawlor DA, Cooper AR, Froberg K, Anderssen SA. Physical fitness in relation to transport to school in adolescents: the Danish youth and sports study. Scand J Med Sci Sports. 2009;19:406-11.
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40.
- Embree TE, Romanow NT, Djerboua MS, Morgunov NJ, Bourdeaux JJ, Hagel BE. Risk factors for bicycling injuries in children and adolescents: a systematic review. Pediatrics. 2016;138.pii:e20160282.
- Johan de Hartog J, Boogaard H, Nijland H, Hoek G. Do the health benefits of cycling outweigh the risks? Environ Health Perspect. 2010;118:1109-16.
- Sánchez Ruiz-Cabello, FJ. Prevención en la actividad física y el deporte. Recomendación. In: PrevInfad/PAPPS [online] [updated 04/08/2007; accessed 27/02/2018]. Available at http://previnfad.aepap.org/recomendacion/deporte-rec
- Rasmussen MG, Grøntved A, Blond K, Overvad K, Tjønneland A, Jensen MK, et al. Associations between recreational and commuter cycling, changes in cycling, and type 2 diabetes risk: a cohort study of Danish men and women. PLoS Med. 2016;13:e1002076.
- Oja P, Titze S, Bauman A, de Geus B, Krenn P, Reger-Nash B, et al. Health benefits of cycling: a systematic review. Scand J Med Sci Sports. 2011;21:496-509.
- Dudas RA, Crocetti M. Association of bicycling and childhood overweight status. Ambul Pediatr. 2008;8:392-5.
- Yang L, Sahlqvist S, McMinn A, Griffin SJ, Ogilvie D. Interventions to promote cycling: systematic review. BMJ. 2010;341:c5293.
- Council of Europe. Committee for the Development of Sport. EUROFIT. Test Europeo de Aptitud Física. MEC. Madrid: CSD; 1992.
- EndocrinoPED. Antropometría. In: Web PEDiatrica [online] [accessed 27/02/2018]. Available at www.webpediatrica.com/endocrinoped/antropometria.php
- Rodríguez-Fernández A, Axpe I, Goñi A. Propiedades psicométricas de una versión abreviada del Cuestionario de Autoconcepto Físico (CAF). Actas Esp Psiquiatr. 2015;43:125-32.
- Serra Majem L, Aranceta Bartrina J, Rivas Barba L, Sangil Monroy M, Pérez Rodrigo C. Crecimiento y desarrollo: dimensión alimentaria y nutricional. In: Serra Majem L, Aranceta Bartrina J, Rivas Barba L (eds.) Crecimiento y desarrollo. Estudio en Kid-Kreceplus. Barcelona: Masson; 2003. p. 45-55.
- Implementación Local de la Estrategia de Promoción de la Salud y Prevención en el SNS. In: Ministerio de Sanidad, Servicios Sociales e Igualdad [online] [accessed 27/02/2018]. Available at www.msssi.gob.es/profesionales/saludPublica/prevPromocion/Estrategia/Implementacion_Local.htm
- Montil M, Barriopedro MI, Oliván J. El sedentarismo en la infancia. Los niveles de actividad física en niños/as de la comunidad autónoma de Madrid. Educación Física y Deportes. 2005;82:5-11.
- Ruiz JR, Rizzo NS, Hurtig-Wennlöf A, Ortega FB, Wärnberg J, Sjöström M. Relations of total physical activity and intensity to fitness and fatness in children: the European Youth Heart Study. Am J Clin Nutr. 2006;84:299-303.
- Wafa SW, Aziz NN, Shahril MR, Halib H, Rahim M, Janssen X. Measuring the daily activity of lying down, sitting, standing and stepping of obese children using the ActivPALTM activity monitor. J Trop Pediatr. 2017;63:98-103.
- Martínez Vizcaíno V, Salcedo Aguilar F, Franquelo Gutiérrez R, Solera Martínez M, Sánchez López M, Serrano Martínez S, et al. Assessment of an after-school physical activity program to prevent obesity among 9- to 10-year-old children: a cluster randomized trial. Int J Obes (Lond). 2008;32:12-22.
- Casabona Monterde C. Sobrepeso y obesidad infantil: no tiramos la toalla. In: AEPap (ed.). Curso de Actualización Pediatría 2017. Madrid: Lúa Ediciones 3.0; 2017. p. 39-52.





