Vol. 19 - Num. 76
Original Papers
Prevalence of attention deficit disorder with hyperactivity in children from an urban area
Clara Tamiri Rodríguez Gonzáleza, M.ª Isabel González Marcosb, M.ª Luisa Arroba Basantac, Luisa Cabello Ballesterosd
aEstudiante de Medicina. Universidad Complutense de Madrid. Madrid. España.
bPediatra. CS Cerro del Aire. Majadahonda. Madrid. España.
cDepartamento de Salud Pública y Materno-Infantil. Universidad Complutense de Madrid. Pediatra. CS Pozuelo-Emisora. Pozuelo de Alarcón. Madrid. España.
dTécnico de Salud. Unidad Docente Multiprofesional de Atención Familiar y Comunitaria Noroeste. Madrid. España.
Reference of this article: Rodríguez González CT, González Marcos MI, Arroba Basanta ML, Cabello Ballesteros L. Prevalence of attention deficit disorder with hyperactivity in children from an urban area. Rev Pediatr Aten Primaria. 2017;19:311-20.
Published in Internet: 13-10-2017 - Visits: 35979
Abstract
Introduction: the primary objective was to assess the prevalence of attention deficit hyperactivity disorder in the paediatric population (ages 6-14 years) served by one primary care centre. The secondary objective was to describe the reasons for initial consultation, specialists that diagnosed and managed ADHD, the criteria used in diagnosis, the types of treatment and associated side effects, and the presence of comorbidities. We sought to determine whether the prevalence of ADHD in children was of approximately 5%, consistent with the reviewed literature.
Patients and methods: we conducted a cross-sectional descriptive study through the review, in collaboration with the paediatrician in charge of each patient, of the health records of children in the catchment area of the Cerro del Aire primary care centre of Majadahonda (Madrid, Spain) (4747 children).
Results: we identified 108 cases of attention deficit hyperactivity disorder (prevalence of 2.28%), 23.15% in girls and 76.85% in boys. The mean age at diagnosis was 7.89 years. Learning problems were the most frequent reason for consultation (39.82%). Paediatric neurologists diagnosed 48.15% of cases and managed 50% of them. In 64.8% of cases, the diagnosis was made based on the DSM-IV criteria combined with scales and a psychoeducational assessment. In 63.89% of patients, pharmacotherapy was used in combination with psychoeducational interventions. The most frequently used drug was methylphenidate (88.88%). Side effects were reported by 25.25%. There were comorbidities in 45.37% (learning disorders in 27.12%).
Conclusion: we found a low prevalence of ADHD, but the biases and limitations of the study must be taken into account. The establishment of a standardised protocol for the diagnosis and management of ADHD would be important to ensure accurate documentation and avoid under- or overdiagnosis. Twenty-eight percent of patients were followed up by primary care paediatricians.
Keywords
● Attention Deficit Hyperactivity Disorder ● Child ● Diagnosis ● Prevalence ● TherapeuticsINTRODUCTION
Attention deficit hyperactivity disorder (ADHD) is a chronic condition with onset in childhood. It has a neurobiological aetiology and results from a complex interaction of prenatal and/or postnatal genetic and environmental factors leading to abnormalities in dopamine transmission1 and characterised by a pervasive pattern of behaviour with features of hyperactivity, impulsivity and/or inattention.
These behaviours are more frequent and severe than would be expected for the age of the child, and the pattern leads to significant functional impairment in academic or work performance as well as everyday activities2 (social and family relationships).
In most cases, the impairment is pervasive and remains stable through time, and in a considerable number it persists into adulthood. However, the symptoms of ADHD are also found in the general population and manifest in a continuum (in which the limits of what is normal are set somewhat arbitrarily), so it could be said that they represent extremes of normal behaviour. Thus, dysfunction is not defined by the presence of a symptom in and of itself (inattention, hyperactivity, impulsivity), but by the intensity and frequency in which symptoms appear in relation to the developmental stage of the child and his or her context, and above all the impact they have on the daily functioning of the affected individual. To this we need to add that there are many other disorders or diseases, whether medical, psychiatric or behavioural, that may present with symptoms of ADHD. Thus, there is considerable controversy in the scientific community regarding the actual prevalence of this disorder.
Currently, ADHD is recognised as the most frequent neurobehavioural disorder in children and adolescents,1 with a high prevalence worldwide. In 2007, Polanczyk performed a meta-analysis of studies conducted in different countries applying the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV), and found that ADHD affects approximately 5% of schoolchildren.3 A later meta-analysis by the same author (2014) corroborated these findings.4
Many other studies have also reported high prevalences, with figures as high as 17%.5 This increase in prevalence, especially in the United States, raises the concern that this disorder may be overdiagnosed. Two studies recently conducted in Spain found prevalences of 4.7% and 6.6% applying the DSM-IV diagnostic criteria. Furthermore, a systematic review and meta-analysis of 14 studies comprising a total of 13 023 children and adolescents estimated an overall prevalence of 6.8% in Spain, with a predominance of the male sex.7-10
The variability in the estimates of the prevalence of ADHD is mostly due to the methodological characteristics of the studies. The observed increase in the number of ADHD cases managed in paediatric clinics can be explained by different factors2-11: 1) an increased awareness of the disorder on the part of health care professionals, with earlier detection and assessment; 2) an improvement in the information received by the parents of these children, and 3) overdiagnosis of ADHD in children that do not have the disorder due to the limitations of the available assessment tools.
At any rate, there has been no evidence in the past three decades suggesting an increase in the number of children that meet the diagnostic criteria for ADHD when the diagnosis is made through standardised procedures.3-6
This controversy and the heterogeneity of opinions pose challenges to the diagnosis of ADHD, so today there is still no conclusive diagnostic tool and the definitive diagnostic criteria are still under debate.11
Objectives
Our hypothesis was that the prevalence of this disorder in children aged 6 to 14 years in the caseload of the Cerro del Aire primary care centre (Majadahonda, Madrid, Spain) would be of approximately 5%, as reported in most of the reviewed literature.
The primary objective was to estimate the prevalence of ADHD in the paediatric population served by the Cerro del Aire primary care centre. As secondary objectives, we sought to describe the sociodemographic characteristics of children with an ADHD diagnosis, the reason for the initial consultation (school, behaviour or learning problems), the specialty of the providers that made the diagnosis and managed these patients (primary care paediatrician, paediatric neurologist or psychiatrist), the criteria used for diagnosis (DSM-IV, International Classification of Diseases, 9th edition [ICD-9], psychoeducational testing), the type of treatment prescribed (pharmacological and/or psychoeducational), the incidence of side effects from treatment, and the prevalence of comorbidities.
PATIENTS AND METHODS
We conducted a cross-sectional descriptive study through the review of the health records of paediatric patients. Geographical setting: urban area of intermediate-high socioeconomic level, Majadahonda (Madrid, Spain). Period under study: March 2016.
Population under study:
- Inclusion criteria: all children aged between 6 and 14 years included in the Paediatrics caseloads of the Cerro del Aire Primary Care Centre of Majadahonda (4747 children).
- Exclusion criteria: none.
Variables:
- Age: quantitative continuous.
- Sex: qualitative dichotomous (male or female).
- Presence of ADHD: qualitative dichotomous (yes or no). The presence of ADHD was defined as inclusion in the health record of any of the following diagnostic codes: P20, attention deficit; P21, hyperkinetic or hyperactive; P22, behaviour disorder in a child; P23, behaviour disorder in an adolescent; P24, learning disorders, academic underachievement or delays in learning.
- Type of ADHD: qualitative polychotomous (inattentive, hyperactive or combined).
- Reason for consultation: qualitative polychotomous (learning problem, hyperactivity, behaviour problem, learning and behaviour problems, all of the above or unknown).
- Family history: qualitative polychotomous (yes, no or not documented).
- Diagnosing specialist: qualitative polychotomous (paediatrician, paediatric neurologist, psychiatrist or a combination).
- Specialist in charge of followup: qualitative polychotomous (paediatrician, paediatric neurologist, psychiatrist or a combination).
- Diagnostic criteria: qualitative polychotomous (DSM-IV, ICD-9 or psychoeducational assessment).
- Age at diagnosis: quantitative continuous.
- Type of treatment: qualitative polychotomous (pharmacological, psychoeducational or both).
- Methylphenidate formulation: qualitative polychotomous (Concerta®, Medikinet®, Rubifen®, Equasym® or more than one in sequence or in combination).
- Side effects: qualitative dichotomous (yes or no).
- Type of side effects: qualitative polychotomous (tics, changes in appetite, sleep disturbance, anxiety or cardiovascular disorder).
- Comorbidity: qualitative dichotomous (yes or no).
- Type of comorbidity: qualitative polychotomous (intellectual disability, autism spectrum disorder, anxiety, oppositional defiant disorder, learning disorder, oppositional defiant disorder combined with learning or other type of disorder).
Data collection method: to obtain a list of individuals of the population under study, we used the ConsultaWeb primary care electronic system. Later on, we reviewed each health record in collaboration with the paediatrician in charge of the patient.
RESULTS
The population served by the Cerro del Aire primary care centre included a total of 4747 children aged 6 to 14 years. Our review of their health records led to the identification of 108 children with a diagnosis of ADHD, corresponding to a prevalence of 2.28% (below the expected prevalence of 5% reported in most of the reviewed studies, P = .000), of who 23.15% were female and 76.85% male.
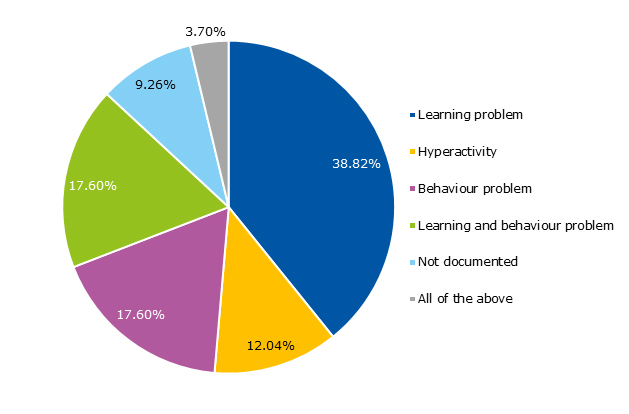
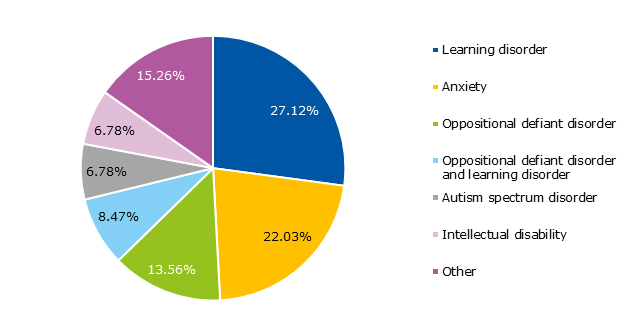
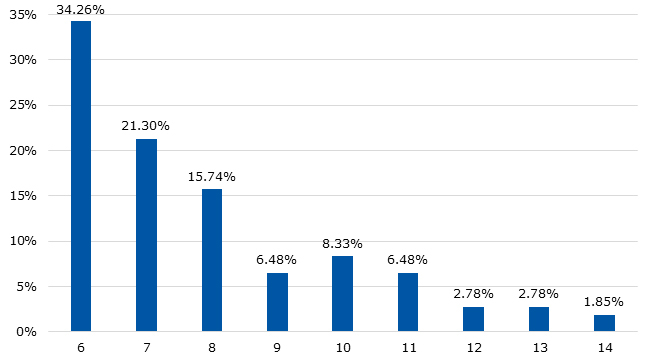
The mean age at the time of ADHD diagnosis was 7.89, and the mode was 6 years. Figure 1 shows the age frequency distribution. Figure 2 shows the distribution of patients with ADHD by reason for consultation.
| Figure 1. Prevalence of attention deficit hyperactivity disorder in the population under study, by age (percentage) |
|---|
 |

In regards to the family history, our data showed a clear predominance of patients in which records had no such documentation (80.56%). A family history of ADHD was documented in 18.52% of cases.
When it came to the type of ADHD diagnosed in the patients in our sample, there was a predominance of the combined type, which amounted to 49% of cases, and the following proportions: inattention in 34.26% and hyperactivity in 16.67%.
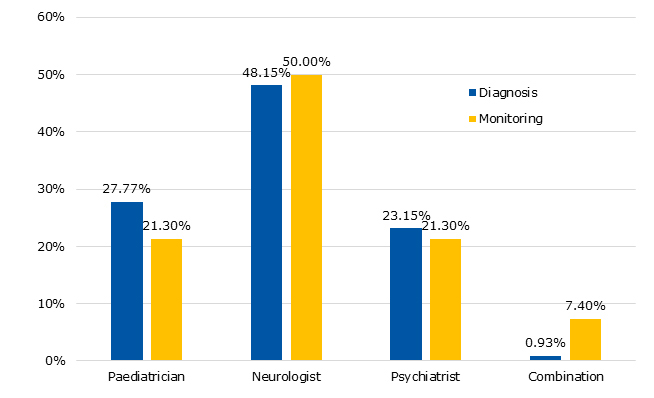
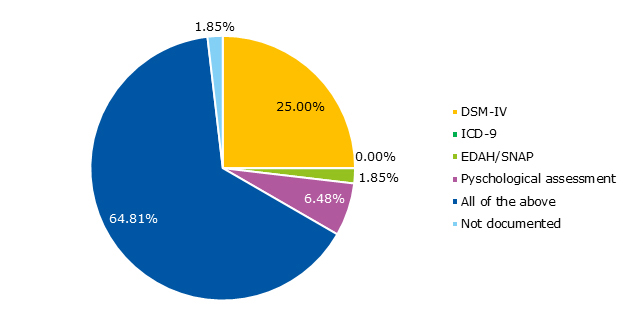
The data regarding the specialists that diagnosed and managed the disorder are shown in Figure 3. Figure 4 summarises the data on the criteria used to diagnose ADHD.
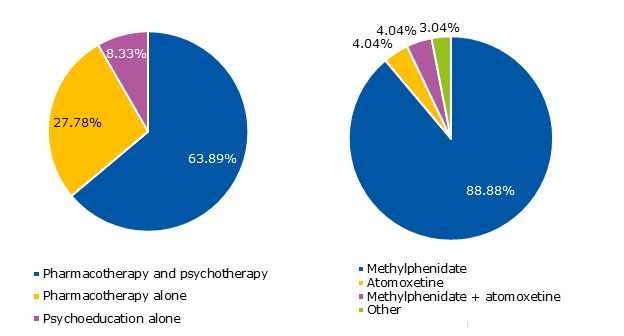
The management of patients could involve pharmacotherapy or other types of treatment, which are reflected in Figure 5, along with the different drugs used. Figure 6 shows the distribution of the different methylphenidate formulations used. Of the patients who received pharmacological treatment, 25.25% experienced side effects, including changes in appetite (40%), sleep disturbances (24%), tics (20%), anxiety (12%) and cardiovascular effects (4%).
| Figure 6. Methylphenidate formulations used in patients with attention deficit hyperactivity disorder |
|---|
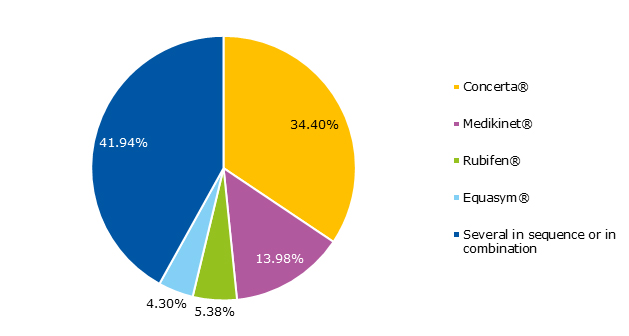 |

Figure 7 shows the presence and absence of comorbidities. We found the following disorders in the patients that had comorbidities: learning disorders (27.12%), anxiety (22%), oppositional defiant disorder (15.56%), oppositional defiant disorder with learning disorder (8.47%), autism spectrum disorder (6.78%), intellectual disability (6.78%) and other (15%).
DISCUSSION
The symptoms of ADHD have a considerable impact on development and interfere with the social, emotional and cognitive functioning of affected individuals, causing significant morbidity and impairment not only in them, but also in their peers and family.2
The high prevalence reported by some studies, reaching as high as 17%, should raise concern and alert us to the possibility of overdiagnosis.11 However, the prevalence found in our study was of 2.28%, which is below the expected mean based on the data of the most recent meta-analyses. Underdiagnosis would seem a more likely problem our centre.
We ought to highlight that the most important way to avoid over- or underdiagnosis of these disorders is to be knowledgeable and make better use of the various diagnostic tools available, keeping in mind that the DSM-IV criteria and scales for the assessment of ADHD (Conners and EDAH) are solely based on pre-established categorical criteria. These are supplementary tools that are not diagnostic by themselves, and therefore should never replace clinical observation in diagnosis. In our study, we found that the diagnosis had been made using a combination of criteria in 64.81% of the patients, and that the DSM-IV criteria were used most frequently, in 25% of cases.
On the other hand, we should also underscore that it is important to know not only the diagnostic criteria, but also the criteria for exclusion, as the differential diagnosis of suspected ADHD is broad and heterogeneous and includes multiple neurologic, paediatric and psychosocial entities. The diagnosis must also be made with a rigorous approach and by a multidisciplinary team. The data of our study shows that only 0.93% of children were diagnosed by a multidisciplinary team, with the diagnosis made most often by a paediatric neurologist (48.15%). The percentage of children managed by several specialists was 7.4%, and in this subset, too, paediatric neurologists were also the specialists that most frequently managed the followup of these patients, in 50% of cases.
In our study, the most prevalent type of ADHD was the combined type, which amounted to 49.07% of the patients and was more frequent in boys (50.6% of the total). Conversely, the inattentive type was the one diagnosed most frequently in girls (in 64% of the total). These data were similar to those reported in various other publications.12,13
The treatment of ADHD should be multimodal with the coordinated involvement of parents, teachers, therapists and physicians. It should be conducted in a health care setting and employ evidence-based interventions recommended in clinical practice guidelines and individualised for each patient (adapted to the age and needs of the patient, and his or her context). Pharmacological treatment aims to control the core symptoms (inattention, hyperactivity and impulsivity) while psychological and psychoeducational interventions address the behavioural and learning problems resulting from those symptoms.14 In our study, 63.89% of the children were managed with a combination of pharmacological and psychoeducational treatment.
The following drugs are approved in Spain for treatment of ADHD in children and adolescents: stimulant drugs (methylphenidate and lisdexamfetamine) and non-stimulant drugs (atomoxetine).15 The side effects of these drugs are usually mild and temporary. In this study, 88.88% of the children were being treated with one of the methylphenidate formulations, and 25.25% of them experienced side effects.
According to published data, up to 67% of children with ADHD has at least one other psychiatric or neurodevelopmental disorder, unlike children without ADHD, of who only 11% have them. Furthermore, many children with ADHD have multiple comorbidities.16 In our study, 45.37% of children had at least one comorbidity, and the most frequent comorbidities were learning disorders (27.12%).
CONCLUSIONS
The observed prevalence was lower than that described in other studies, but we need to take into account the potential biases at play in this study, such as the intermediate-to-high socioeconomic level of the geographical area under study, which may entail that a percentage of children, while having a diagnosis in their health records, may not visit or be managed by professionals in the public health system. Furthermore, the electronic primary care database, AP-Madrid®, does not have a specific diagnostic code for this disorder. Clinicians entered diagnoses based on the reason for initial consultation, and these diagnoses were not subsequently adjusted.
Since there is no protocol for the diagnosis and followup of this disorder in primary care, its documentation is widely variable, which hinders data collection.
The majority of children in our study were diagnosed and managed by paediatric neurologists, which probably was due to the population under study and the private infrastructures available in this geographical area, combined with the low availability of public mental health services. Still, the percentage of children diagnosed and managed by primary care paediatricians was not small (approximately 28%), which is a relevant finding, as there are not enough paediatric neurologists or even child and adolescent psychiatrists in Spain to manage the existing volume of patients with ADHD.
ETHICAL AND LEGAL CONSIDERATIONS
We did not include any personally identifiable information of participants in the databases used for the study. We thus adhered to international directives on the protection of personal data as well as current Spanish law (Organic 15/1999 of 13/12/99 on the Protection of Personal Data, BOE 298 from 14/12/99). We upheld patient autonomy rights in the context of human research (Law 41/2002 of November 14, regulating patient autonomy and rights and obligations of information and clinical documentation). The researchers in charge guaranteed the security of the databases, which will not be used for any purpose other than the one noted in the section on specific objectives.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation with the preparation and publication of this article.
ABBREVIATIONS
ADHD: attention deficit hyperactivity disorder · DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, 4th edition · ICD-9: International Classification of Diseases, 9th edition.
ACKNOWLEDGMENTS
First of all, we thank the Paediatrics team of the Cerro del Aire Primary Care Centre, Carmen Ramos Ramos, Rosa Duque Ortega, Susana Domínguez García-Cano, Cristina Fresno Calle, Nieves Lobato Gómez and María Isabel González Marcos for their collaboration in the collection of data pertaining to their patients. We thank Luisa Cabello Ballesteros, health technician of the Dirección Asistencial Noroeste (Northeast Area Health Care Directorate) for her continuous availability and help during the study. Also, Antonio Martínez de Coca, for his patience, his help with this project, and his support through the last 3 years of study. And last of all, my parents… for giving me life.
REFERENCES
- Grupo de trabajo de la Guía de Práctica Clínica sobre el Trastorno por Déficit de Atención con Hiperactividad (TDAH) en niños y adolescentes. Guía de Práctica Clínica sobre el Trastorno por Déficit de Atención con Hiperactividad (TDAH) en Niños y Adolescentes. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad, Política Social e Igualdad. Agència d´Informació, Avaluació i Qualitat (AIAQS) de Cataluña; 2010. Clinical Practice Guidelines, SNS: AATRM No 2007/18. Available at www.guiasalud.es/GPC/GPC_477_TDAH_AIAQS_compl.pdf
- Cardo E, Servera M. Trastorno por déficit de atención/hiperactividad: estado de la cuestión y futuras líneas de investigación. Rev Neurol. 2008;46:365-72.
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942-8.
- Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43:434-42.
- Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490-9.
- Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135:e994-e1001.
- Catalá-López F, Peiró S, Ridao M, Sanfélix-Gimeno G, Gènova-Maleras R, Catalá MA. Prevalence of attention deficit hyperactivity disorder among children and adolescents in Spain: a systematic review and meta-analysis of epidemiological studies. BMC Psychiatry. 2012;12:168.
- Pérez Payá A, Lizondo Escuder A, García López C, Silgo Gauche E. Déficit de atención con hiperactividad. Perspectiva desde Atención Primaria. Rev Pediatr Aten Primaria. 2012;14:225-9.
- Rodríguez Molinero L, López JA, Garrido M, Sacristán AM, Martínez MT. Estudio psicométrico-clínico de prevalencia y comorbilidad del trastorno por déficit de atención con hiperactividad en Castilla y León (España). Rev Pediatr Aten Primaria. 2009;11:251-70.
- Cardo E, Servera M, Llobera J. Estimation of the prevalence of attention deficit hyperactivity disorder among the standard population on the island of Majorca. Rev Neurol. 2007;44:10-4.
- García Peñas JJ. Domínguez Carral J ¿Existe un sobrediagnóstico del trastorno de déficit de atención e hiperactividad (TDAH)? Evid Pediatr. 2012;8:51.
- Clinical Guideline. Attention deficit hyperactivity disorder. En: National Institute for Health and Clinical Excellence (NICE) [online] [accessed 09/10/2017]. Available at www.nice.org.uk/CG072.2008
- Subcommittee on Attention-Deficit/Hyperactivity Disorder; Steering Committee on Quality Improvement and Management, Wolraich M, Brown L, Brown RT, DuPaul G, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007-22.
- Hidalgo Vicario MI. Situación en España del trastorno por déficit de atención e hiperactividad. Editorial. Pediatr Integral. 2014;18:595-7.
- Soutullo C, Álvarez-Gómez MJ. Bases para la elección del tratamiento farmacológico en el trastorno por déficit de atención/hiperactividad. Rev Neurol. 2013;56:S119-29.
- Larson K, Russ SA, Kahn RS, Halfon N. Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics. 2011;127:462-70.