Vol. 16 - Num. 62
Original Papers
A Mental Health Prevention Program in Pediatric Primary Care: A pilot study
Irene Caro-Cañizaresa, L Rodríguez Blancoa, C Vidal Mariñoa, M Segura-Valverdea
aPsicóloga Interna Residente. Fundación Jiménez Díaz. Madrid. España.
Correspondence: I Caro-Cañizares. E-mail: icaroc@fjd.es
Reference of this article: Caro-Cañizares I, Rodríguez Blanco L, Vidal Mariño C, Segura-Valverde M. A Mental Health Prevention Program in Pediatric Primary Care: A pilot study. Rev Pediatr Aten Primaria. 2014;16:109-15.
Published in Internet: 27-06-2014 - Visits: 14966
Abstract
Introduction: childhood mental disorders are the most important non-organic reasons for consultation and the most common chronic conditions attended in Pediatric Primary Care. Early detection and intervention may prevent or ameliorate the development of these disorders and reduce healthcare burden in the long run.
Methods: we designed a parenting program for 16 parents or principal caregivers of 0-5-aged children. Participants were recruited from the Pediatric Primary Care services of the Ventura Rodriguez Health Center in Madrid. Participants were divided into two groups according to their children’s age. Our program was carried out in two sessions of one hour and a half combining theoretical contents and practical activities.
Results: in the first group, we obtained positive qualitative results regarding the usefulness of the addressed contents and the viability of the program. Quantitative data showed that 100% participants in the second group assessed the program as “Good” or “Very Good” and considered useful all the information provided in the program.
Conclusion: our results support the necessity of implementing prevention activities in the field of childhood mental health. It is also important to promote cooperation between Pediatric Primary Care and Mental Health services.
Keywords
● Childhood ● Mental health ● Parenting Program ● Primary preventionINTRODUCTION
In year 2010, paediatric care in primary care teams (PCTs) in centres of the autonomous community of Madrid (ACM) exceeded five million visits, with caseloads of 23 patients a day.1,2 The number of patients served by each paediatrician in a PCT of the ACM rose to 10933 in year 2010. Specifically, in the healthcare district known as Area 6 (west area of the ACM, to which the Ventura Rodríguez health care centre belongs), the ratio was the highest in this community, with 1294 patients cared for by each provider. This denotes an excess in demand and limits the time that can be devoted to each patient.
In their review about the evolution of child mental health services in primary care, Kelleher and Stevens4 showed that mental disorders of childhood were the most common chronic conditions for which services were sought in paediatrics. Similar data have been described in the Spanish population.5.
At a global level, it is estimated that the prevalence of mental disorders in children approximately ranges between 14% and 22%.6 More specifically, other authors have found high prevalence rates of mental health problems related to conduct disorders (between 3% and 7%),7 learning disorders (at least 5%),8 mood disorders (between 1% and 3% for depression, and between 3% and 7% for dysthymia)9 and anxiety disorders and phobias (between 1% and 16%).10
As various authors state,11-15 early detection and treatment of these problems facilitates a quick recovery. In this regard, the role of the PCT paediatrician could be crucial, as it is the referring provider for the parents, the professional that parents depend upon to manage the problems of their children.
In spite of this situation, PC centres in the ACM do not currently have mental health professionals on staff. However, for three years now, the educational curriculum for a specialist in clinical psychology (psychology resident intern [PIR]) has included a three-month-long rotation in PC. The activity they develop in relation to the child and adolescent population involves participation in PCT paediatrician and nurse visits, and participation and collaboration in health prevention and promotion programmes.16
Given the difficulties in the parent-child relationship observed in this context, the need to set up a parenting school to provide the main caregivers with the skills for the early detection and management of these problems was identified. This type of intervention is more established in other countries, where there are standardised programmes that have demonstrated their efficiency, such as the STAR Parenting Program in the United States, which focuses on increasing parents’ skills to manage the behaviour of children aged 1 through 5 years,17 or the programmes of the Centre for Parents and Child Support of London, which among other aspects attempt to improve parent-child interactions.18,19 The effectiveness of this type of early interventions in promoting the emotional and social wellbeing of children younger than five years was demonstrated in a recent meta-analysis study.20
The main purpose of the parenting school is to prevent the development of mental health problems in childhood and to alleviate the excessive caseload in paediatric consults. A pilot programme was implemented to work with the main caregivers of children aged 0 to 5 years who received paediatric care.
METHODS
Population
Two group interventions were performed in the Ventura Rodríguez Healthcare Centre (Madrid, Spain). The first intervention took place in August 2010. This group comprised a total of six fathers, mothers, and caregivers of four children ages 2 to 5 years recruited from the paediatric office during July and August. Members received a phone reminder of the first group meeting a week prior. The second intervention took place in August 2011. This group consisted of ten fathers, mothers, or caregivers of a total of six babies 0 to 3 months who were recruited in the same manner as the first group (in-person communication at the Paediatrics office the previous month, and telephone reminder the week before the first group meeting).
Contents
The contents of the first group focused on conveying basic notions of parenting styles, identifying the styles characteristic of the caregivers and the styles with which they had been brought up, behaviour modification techniques, contingency management, and skills to set limits and manage temper tantrums.
The contents of the second group revolved around developing a bond and attaching with the child, the development of skills to adjust to the new situation, and learning the basics of parenting styles and behaviour modification to set limits in the future.
Both groups participated in two one-hour-and-a-half long sessions, which occurred weekly, facilitated by the psychology resident intern who was currently on rotation at the PC department, supervised by the paediatrician, and evaluated by an observer (nurse) to ensure adherence to the objectives. The sessions were divided into different sections depending on the subjects to cover, with theoretical presentations alternating with practical activities and group discussions.
Assessment
The purpose of the first group was to assess the possibility of implementing the program (demand for the service, availability of space to perform it, acceptance by other professionals, etc.), so structural assessment tools were not utilised. We recorded the overall impressions, expressed verbally, of the participants and of the rest of the staff in the centre.
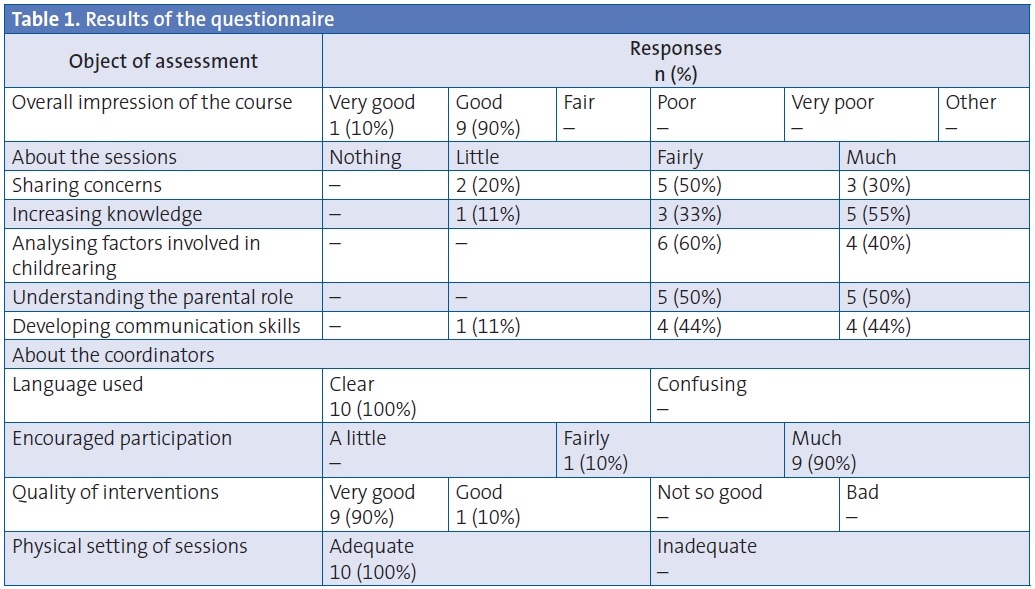
The purpose of the second group, following the first experience, was to assess the quality of the intervention and the satisfaction of the participants by means of a questionnaire of close- and open-ended questions that the fathers, mothers, and caregivers who attended the group filled out in the last session of the educational programme.
The questionnaire had ten close-ended questions on a Likert scale that assessed the overall impression of the course, the perceived improvement in the knowledge of aspects related to the contents of the sessions, appreciation of formal aspects pertaining to the professionals who facilitated the group, and assessment of the physical space in which the group sessions were held. It also included two open-ended questions about the perceived utility of the contents that the group had worked on.
An external observer was also present in the second group and evaluated the attendance, participation, and adherence to the planned contents.
RESULTS
In the first group, participants reported having favourable impressions of the programme. Parents stated that they had found the contents useful and the staff of the centre assessed the initiative favourably and believed it was viable to continue with the programme.
In the second group, the results of the Likert scale (Table 1) were the following: 100% (n=10) of participants evaluated the group as “good” or “very good”. When it came to specific sessions, 80% of participants believed that the group had helped them to express their concerns about their children “fairly” or “much”; 88% of participants considered that the sessions had helped them increase their knowledge “fairly” or “much”; 100% stated that they had helped them analyse the factors involved in childrearing “fairly” or “much”; 100% reported that their understanding of the role of the parent as educator had grown “fairly” or “much”; and 88% answered “fairly” or “much” to whether they had acquired skills to communicate with their children.
When it came to the open-ended questions, 100% of participants considered that all the information was useful, and that the most useful contents were the information pertaining to baby massage, parenting styles, and the factors involved in childrearing, as well as the practical examples and the discussion of concerns.
The data gathered by the external observer (a paediatric nurse of the centre) showed the following: when it came to attendance and participation, out of the 10 recruited participants, all showed up to the first session, and 9 to the second. All of them participated actively asking at least one question or making at least one comment during the sessions. As for adherence to the programme, the four subject blocks were taught as planned (time-wise and in terms of the contents covered).
DISCUSSION
As we have mentioned, paediatric offices can be overburdened not only with visits regarding medical matters, but also with visits for mental health or behavioural problems, which constitute the most common non-organic reason for visits.21. Under these circumstances, it is essential that the healthcare centre can respond to the parents’ requirements. As some authors have pointed,22 creating spaces for reflection can be beneficial in minimising the suffering of children and their closest relatives. Providing the main caregivers with correct information and training may prevent the development of problems, working as a preventive strategy, and helping detect problems early, keeping them from getting worse or becoming chronic, and ultimately alleviating the high caseloads in paediatric services.
Past studies have revealed the difficulty experienced by paediatric departments to identify and treat mental health disorders.23. Although many limitations have been overcome in recent years, increasing the frequency of the diagnosis and treatment of mental disorders in paediatric care,4 there is still work to be done in this area, as the management of some of these cases can be challenging.4
The development of a parenting school has been a useful tool in this regard. The experiences were well received by caregivers and healthcare staff alike, and the results make it worth considering the possibility of developing a long-term project. Still, we need to keep in mind the limitations of this study. First of all, it is a cross-sectional pilot study of limited duration, so it does not allow us to know the mid- and long-term effects of the intervention. No baseline assessment was available, so we could not objectively quantify the degree of improvement. Secondly, the sample size limits the generalisability of the results. And third of all, this is a descriptive study with no control group, with the limited capacity for reaching conclusions characteristic of such designs.
Despite these limitations, the fact that all participants found the experience satisfactory suggests that we could observe sufficiently good results in a larger sample. On the other hand, the limitations of having done a descriptive study could be compensated by its greater ecological validity.
Furthermore, we currently plan on conducting a study with longer duration and a larger sample allowing for the objective assessment of the results using a pretest-posttest design, and with a longitudinal long-term follow up to assess the impact of the intervention in decreasing the number of paediatric visits compared to a control group. Such data would allow us to support the need of a permanent link between PC and mental health, as opposed to one restricted to three months a year.
In our opinion, these interventions are a health prevention and promotion activity that benefits both caregivers and their children, and that could lead to a decreased burden on the healthcare system and decreased healthcare costs in the long term. Thus, we believe it is essential that we develop preventive programs within PC, such as the parenting school, and generally promote a greater integration and collaboration of PC and mental health services.
CONFLICTS OF INTEREST
The authors declare having had no conflicts of interest in relation to the preparation and publication of this study.
ACRONYMS: ACM: Autonomous Community of Madrid • PC: primary care • PCTs: Primary Care teams • PIR: psychology resident intern.
BIBLIOGRAPHY
- Servicio Madrileño de Salud. Memoria 2012 [on line] [consulted on 01/05/2013]. Available in http://goo.gl/d00KWX
- Servicio Madrileño de Salud. Memoria 2011 [on line] [consulted on 01/05/2013]. Available in http://goo.gl/R94JN6
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Ratios: población por profesional. 2012 [on line] [consulted on 01/05/2013]. Available in http://pestadistico.inteligenciadegestion.msssi.es
- Kelleher KJ, Stevens J. Evolution of child mental health services in primary care. Academic Pediatr. 2009;9:7-14.
- Morán Sánchez I, Navarro-Mateu F, Robles Sánchez F, Concepción Salesa A. Validez del diagnóstico clínico del trastorno por déficit de atención con hiperactividad en las derivaciones de pediatría a la consulta de psiquiatría infantil. Aten Primaria. 2008;40:29-33.
- Marsh E, Graham S. Clasificación y Tratamiento de la Psicopatología Infantil. In: Caballo V, Simón M (eds.). Manual de Psicopatología Clínica Infantil y del Adolescente. Trastornos Generales. Madrid: Ediciones Pirámide; 2006. p. 29-56.
- Servera M, Bornas X, Moreno I. Hiperactividad Infantil: conceptualización, evaluación y tratamiento. In: Caballo V, Simón M (eds.). Manual de Psicopatología Clínica Infantil y del Adolescente. Trastornos Generales. Madrid: Ediciones Pirámide; 2006. p. 401-33.
- Sadock B, Sadock V. Kaplan & Sadock's concise textbook of child and adolescent psychiatry. Philadelphia: Lippincott Williams & Wilkins; 2009.
- Del Barrio V. El niño deprimido. Barcelona: Ediciones Ariel; 2007.
- Méndez F, Olivares J, Bermejo R. Características clínicas y tratamiento de los miedos, fobias y ansiedades. In: Caballo V, Simón M (eds.). Manual de Psicopatología Clínica Infantil y del Adolescente. Trastornos Generales. Madrid: Editorial Pirámide; 2006. p. 59-92.
- Butter E, Mulick JA, Metz B. Eight case reports of learning recovery in children with pervasive developmental disorders after early intervention. Behavioral Interventions. 2006;21:227-43.
- Cioni G, D'acunto G, Guzzetta A. Perinatal brain damage in children: neuroplasticity, early intervention, and molecular mechanisms of recovery. Prog Brain Res. 2011;189:139-54.
- Fowler DG, Hodgekins J, Arena K, Turner R, Lower R, Wheeler K, et al. Early detection and psychosocial intervention for young people who are at risk of developing long term socially disabling severe mental illness: Should we give equal priority to functional recovery and complex emotional dysfunction as to psychotic symptoms? Clin Neuropsy. 2010;7:63-71.
- Peris A, Bonizzoli M, Iozzelli D, Migliaccio ML, Zagli G, Bacchereti A, et al. Early intra-intensive care unit psychological intervention promotes recovery from post traumatic stress disorders, anxiety and depression symptoms in critically ill patients. Crit Care. 2011;15:R41.
- Shanahan T, Barr R. Reading recovery: An independent evaluation of the effects of an early instructional intervention for at-risk learners. Read Res Quart. 1995;30:958-96.
- Programa formativo de la especialidad en Psicología Clínica. Orden SAS/1620/2009 del 02 de junio de 2009. BOE N.º146; 2009 [en línea]. Available in www.msssi.gob.es/profesionales/formacion/docs/Psicologia_C.pdf
- Fox RA, Fox DA, Anderson RC. Measuring the effectiveness of the star parenting program with parents of young children. Psychol Rep. 1991;68:35-40.
- Barlow J, Davis H, McIntosh E, Jarrett P, Mockford C, Stewart-Brown S. Role of home visiting in improvin parenting and healthin families at risk of abuse and neglect results of a multicentre randomised controlled trial and economic evaluation. Arch Dis Child. 2007;92:229-33.
- Puura K, Davis H, Cox A, Tsiantis J, Tamminen T, Ispanovic-Radojkovic V, et al. The european early promotion project: description of the service and evaluation study. Int J Ment Health Prom. 2005;7:17-31.
- McMillan SA, Barnes J, Barlow J. Primary study evidence on effectiveness of interventions (home, early education, child care) in promoting social and emotional wellbeing of vulnerable children under 5. London, U.K.: National Institute for Clinical Excellence; 2012 [en línea]. Available in http://goo.gl/9ljyCw
- Rodríguez Hernández PJ. Trastornos del comportamiento. Pediatr Integral. 2008;12:949-58.
- Bonet de Luna C, Fernández García M, Chamón Parra M. Depresión, ansiedad y separación en la infancia. Aspectos prácticos para pediatras ocupados. Rev Pediatr Aten Primaria. 2011;13:471-89.
- Lavigne JV, Binns HJ, Kaufer K. Behavioural and emotional problems among preschool children in pediatric primary care: prevalence and pediatricians' recognition. Pediatrics. 1993;91:649-55.
- Kelleher KJ, McInerny TK, Gardner WP. Increasing identification of psychosocial problems: 1979-1996. Pediatrics. 2000;105:1313-21.





