Vol. 16 - Num. 61
Original Papers
Diagnosis and management of sinusitis: attitudes of the pediatricians
M.ª Rosa Albañil Ballesterosa, C Calvob, P Hernando Helgueroc, L Martínez Camposd, Begoña Domínguez Aurrecoecheae
aPediatra. CS Cuzco. Fuenlabrada. Madrid. España.
bServicio de Pediatría. Hospital Universitario Severo Ochoa. Leganés. Madrid. España.
cPediatra. CS Ramón y Cajal. Alcorcón. Madrid. España.
dUGC Pediatría. Hospital La Inmaculada. Almería. España.
ePediatra. Instituto de Investigación Sanitaria del Principado de Asturias (ISPA). Asturias. España.
Correspondence: MR Albañil. E-mail: mralba100@hotmail.com
Reference of this article: Albañil Ballesteros MR, Calvo C, Hernando Helguero P, Martínez Campos L, Domínguez Aurrecoechea B. Diagnosis and management of sinusitis: attitudes of the pediatricians. Rev Pediatr Aten Primaria. 2014;16:23-33.
Published in Internet: 14-04-2014 - Visits: 41604
Abstract
Introduction: sinusitis is a common condition whose approach in daily pediatric practice is not well known.
Methods: performing a national level cross-sectional study through a survey distributed "on line" to members of 2 pediatric societies, in March 2013.
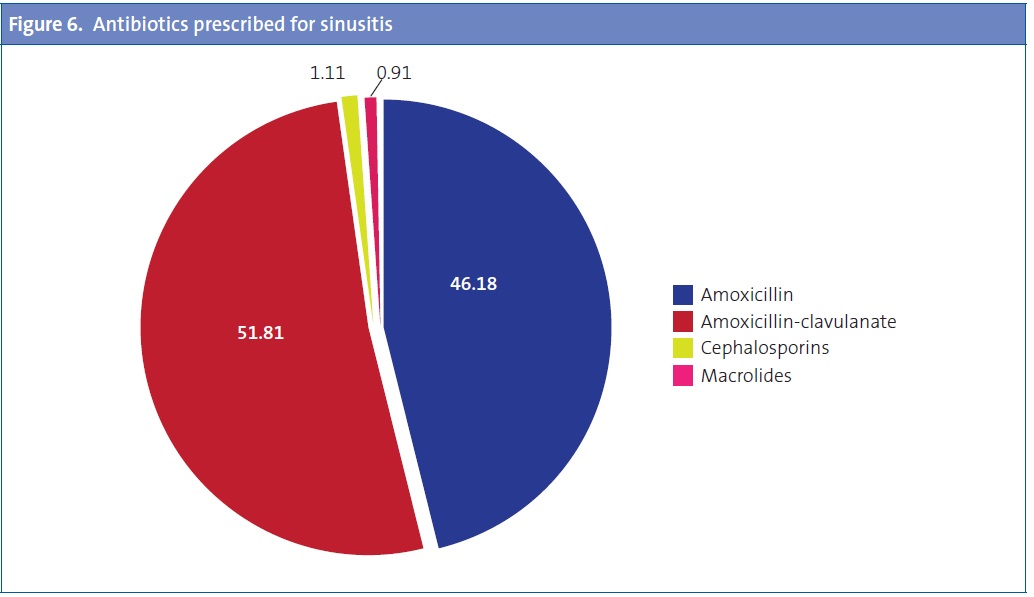
Results: 994 responses were obtained (78% of Primary Care). Most professionals estimated the frequency of sinusitis being about 1% of the visits. 76.6% reported exclusively diagnosis with clinical criteria, considering (92%) an association of symptoms including persistent / purulent rhinorrhea (89%), facial pain / headache (84%), prolonged or nocturnal cough and fever in the context of upper respiratory infection (URI) (54%). Between 19.7 and 33.4% of professionals (primary / specialist) would request radiographs. 90% reported using antibiotics with or without other adjunctive treatments, being amoxicillin-clavulanate (52%) the chosen antibiotic, followed by amoxicillin 46%.
81% of pediatricians diagnose URI in more than 30% of visits and in 85% of cases do not prescribe drug treatment. When the URI lasts more than 14 days, 70% of them decide to treat. The most widely used treatments are anti-inflammatory / analgesics (54.5%) and antibiotics (51.4%).
Conclusions: pediatricians' knowledge and clinical practice in URI and sinusitis indicate a high level of compliance with the most recent clinical practice guidelines, highlighting the limited use of antibiotics in the URI, the clinical diagnosis of sinusitis and the empirical choice of antibiotic.
Keywords
● Amoxicilin ● Amoxicilin-clavulanate ● Antibiotics ● Radiology ● Sinusitis ● Upper respiratory tract infectionINTRODUCTION
Sinusitis is defined as the inflammation of one or more of the paranasal sinuses1. Its aetiology is usually infectious and associated to viral respiratory conditions of the upper respiratory tract (URT) due to the continuity of the mucosa that lines the nasal cavity and the sinuses. Allergic conditions are the second leading cause. The American Academy of Pediatrics2 defined acute bacterial sinusitis as a bacterial infection of the paranasal sinuses lasting less than 30 days in which symptoms resolve completely.
In the last two years, several Clinical Practice Guidelines have been published with diagnosis and treatment recommendations1,3-5, but there are few studies6-8 allowing the evaluation of the knowledge and attitudes of health professionals, which may be due to the variability of diagnostic criteria and the lack of an objective and easy to do diagnostic test.
Recently, a Consensus Document on the aetiology, diagnosis, and treatment of sinusitis has been developed, with the collaboration of the Sociedad Española de Infectología Pediátrica (Spanish Society of Paediatric Infectology, SEIP), the Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics, AEPap), the Sociedad Española de Pediatría Extrahospitalaria y Atención Primaria (Spanish Society of Out-of-Hospital and Primary Care Paediatrics, SEPEAP) and the Sociedad de Otorrinolaringología (Society of Otorhinolaryngology, SEORL PCF)9, some of whose conclusions were presented at the Congreso Nacional de la Asociación Española de Pediatría (National Congress of the Spanish Association of Paediatrics, AEP). We thought that it would be of interest to learn about the clinical practice of Spanish paediatricians in regards to this disease prior to the diffusion of the Consensus.
MATERIALS AND METHODS
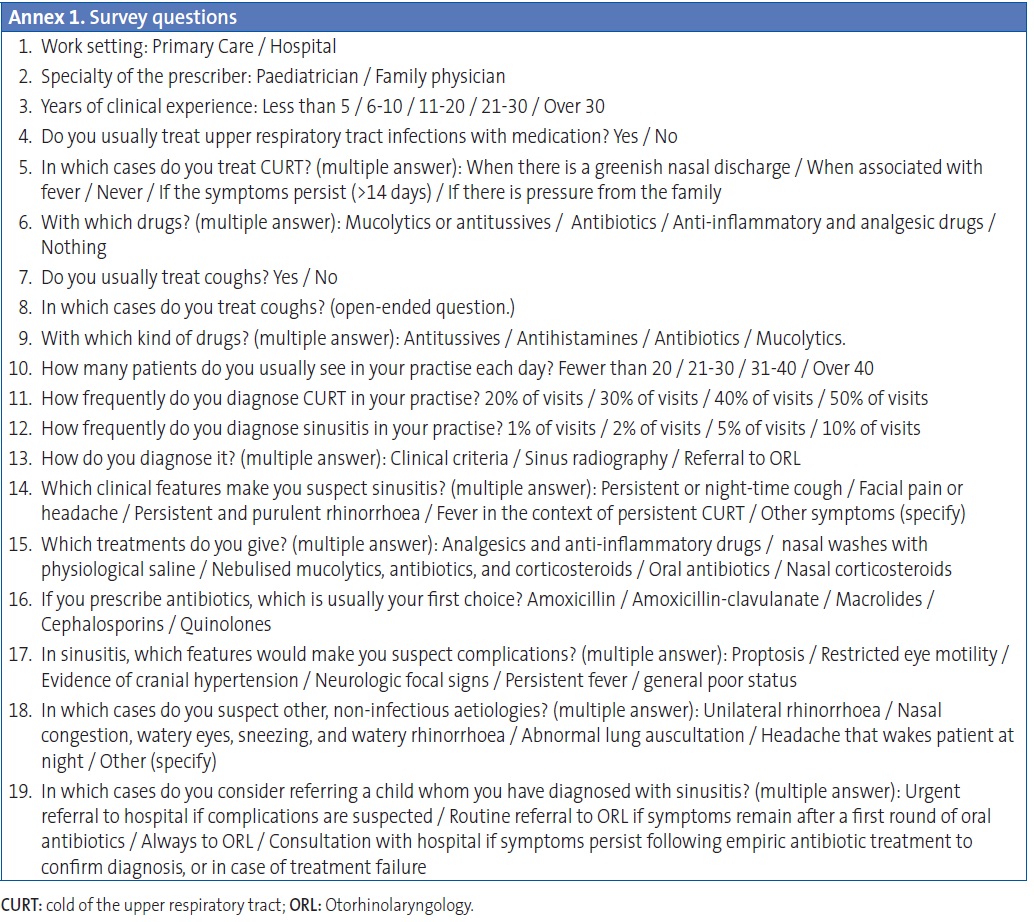
We performed a nationwide cross-sectional multicentre study by means of an online questionnaire designed for this purpose, which was addressed to paediatricians and distributed by email to all members of the two paediatric societies (AEP and AEPap) and through the mailing list of the PEDIAP. We designed the questionnaire using Google Docs®. Its questions (Annex 1) are geared to explore the knowledge and attitudes of Spanish paediatricians in relation to colds involving the upper respiratory tract (their frequency, symptoms, and treatment) and sinusitis (its frequency, symptoms, diagnosis, treatment, and complications). Some questions were single-answer, most were multiple-answer, and one was open-ended. The preliminary information of the questionnaire specified that only professionals who provide care for sinusitis in their regular practise should respond to it. We also gathered data for the following variables: work setting, specialty, years of experience, and number of patients seen per day. Participation was anonymous and voluntary.
The survey was distributed in March 2013. At the time, the number of AEP members was 9036, of whom 6215 were Primary Care (PC) paediatricians. The number of members of the AEPap was 3287, most of whom worked in PC. The members of the AEPap can also be members of the AEP. The target population addressed by the survey were the 6215 PC paediatricians, as well as a small percentage of hospital-based paediatricians who provide care for sinusitis cases in their clinical practice. There are probably fewer than 7000 in total. Using other survey-based studies in our environment as a reference10, we deemed that the sample size needed to be able to estimate the attitudes of paediatricians in regards to URTI and sinusitis with less than 5% error, a 50% level of heterogeneity, and a 95% confidence interval (95% CI), assuming the target population of paediatricians was 7000, was of 365 responses.
Since the study did not include any patient data and the responses were anonymous and voluntary, we did not think it necessary to seek approval by an Ethics Board. The authors of the study have been the only individuals with access to the results, which were gathered exclusively for their statistical use.
RESULTS
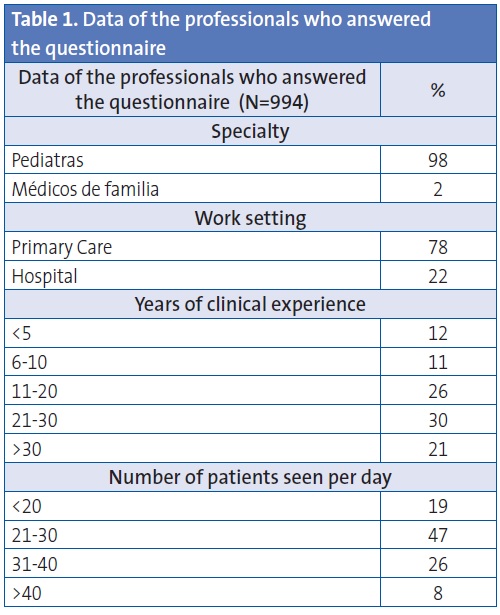
We obtained 994 responses. Paediatricians accounted for 98% of respondents (the remaining 2% were general practitioners or family physicians), 78% of whom worked in a PC setting. Out of all respondents, 77% had more than 10 years of experience, and half of those more than 20. Almost 50% were seeing between 20 and 30 patients each day, and 73% saw between 20 and 40 patients (Table 1).
Upper respiratory tract infection (URTI)
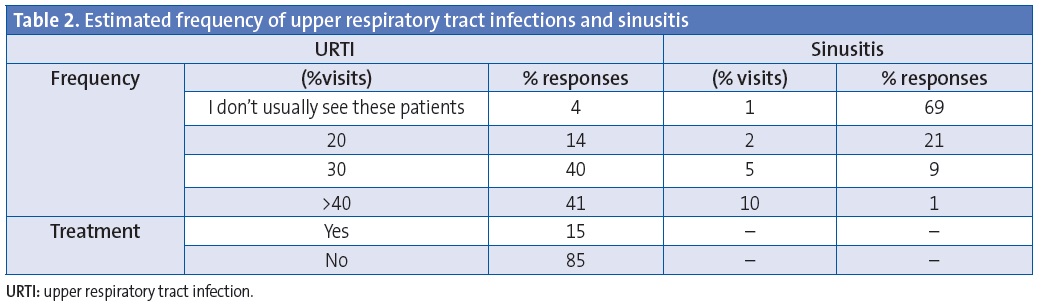
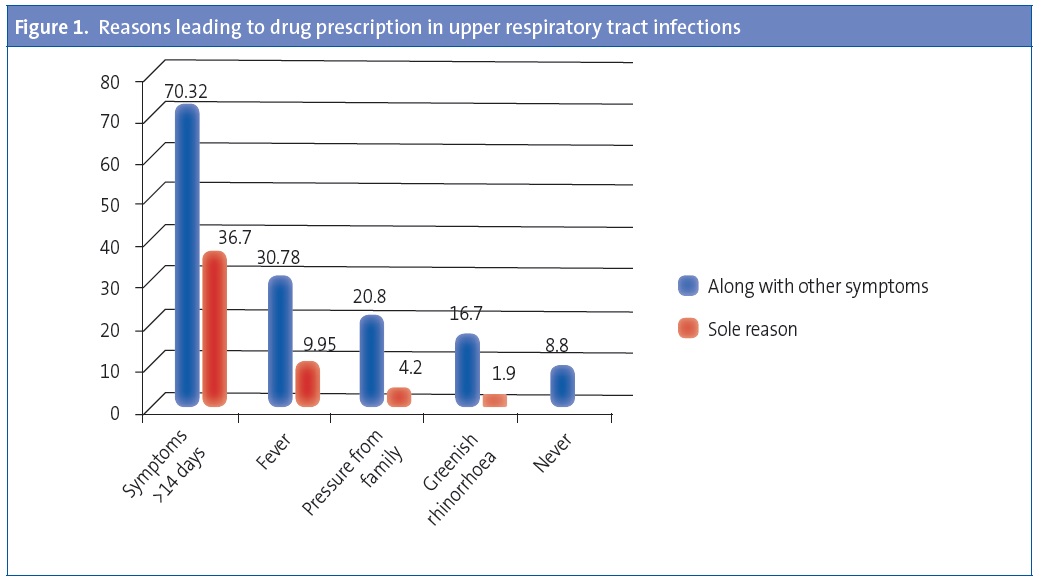
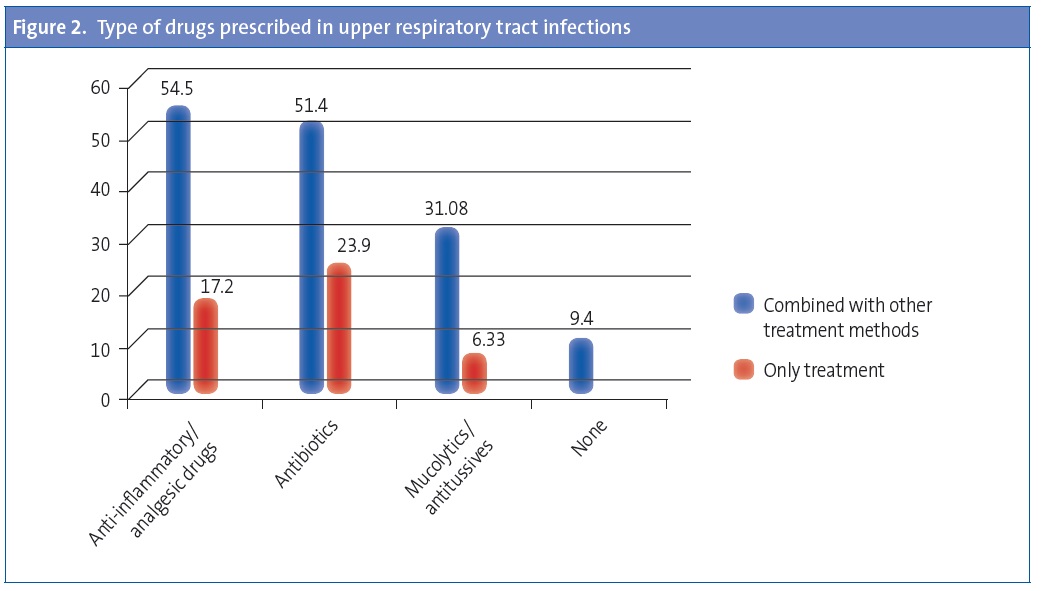
Of all paediatricians, 81% reported diagnosing URTI in over 30% of the visits, and the majority (85%) did not prescribe medication for this condition (Table 2). However, when the cold symptoms lasted more than 14 days, with or without associated symptoms, up to 70% of paediatricians chose to treat the illness (Figure 1). The most frequently used treatments were anti-inflammatory or analgesic drugs, alone or in combination with other medication, by 54.5% of physicians, followed by antimicrobials alone or in combination with other medication, used by 24% and 51% of respondents, respectively (Figure 2).
Sinusitis
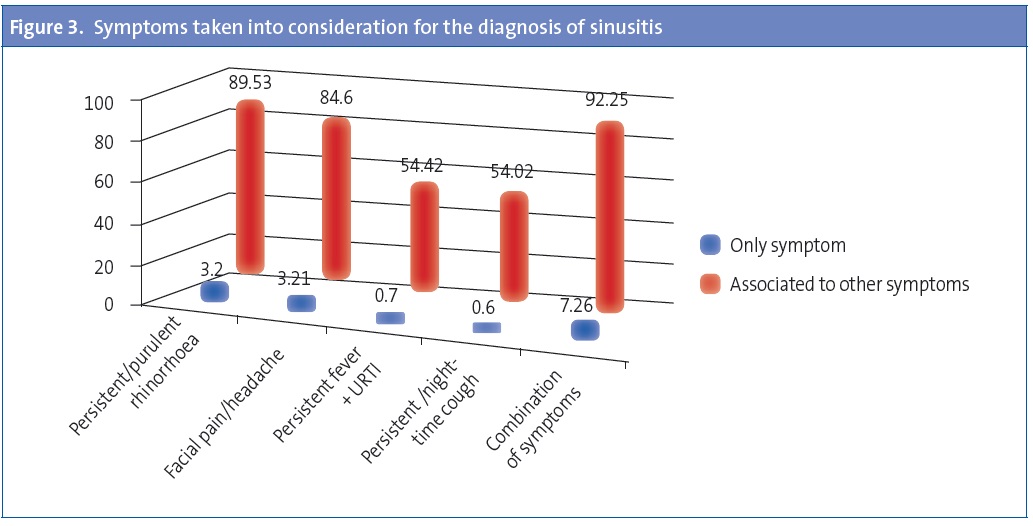
A majority of paediatricians, 69%, diagnosed sinusitis in 1% of the visits (Table 2). Over 92% of them did it based on a combination of symptoms, of which the most frequently considered for diagnosis were persistent or purulent rhinorrhoea (89.5%) and facial pain/headache (84.6%). Persistent or night-time cough and fever in the context of URTI are taken into account by 54% of paediatricians (Figure 3).
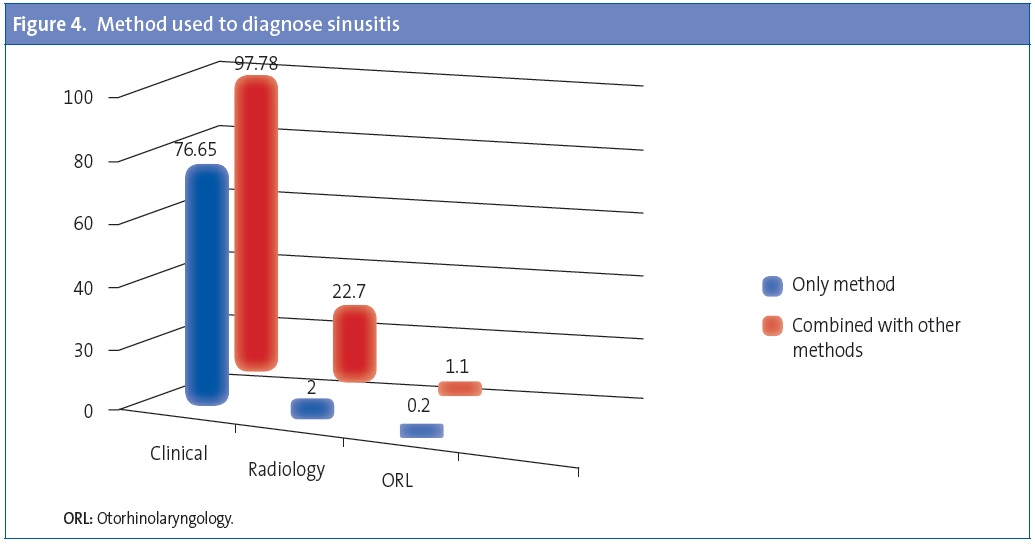
Of all respondents, 76.6% (79.71% of PC paediatricians and 65.58% of paediatric specialists) reported diagnosing on the basis of clinical criteria alone, while radiology, alone or in combination with other resources, was used by 22.7% (19.76% of PC paediatricians vs. 33.48% of paediatric specialists). One percent reported referring patients to Otorhinolaryngology (ORL) (Figure 4).
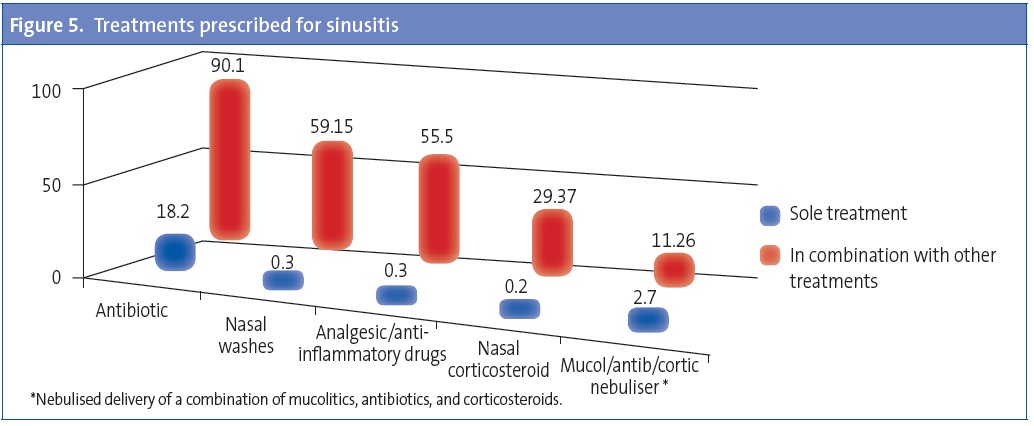
As for treatment, 78.26% of respondents would prescribe two or more drugs. Antibiotics, alone or in combination with other drugs, would be used by 90% (18% would use it as the only treatment) (Figure 5), with amoxicillin-clavulanate being the most frequently used treatment (52%), followed by amoxicillin, used by 46% of respondents (Figure 6). The choice of amoxicillin is more frequent among PC paediatricians (50.57%) than among paediatric specialists (30.23%), while amoxicillin-clavulanate is more frequently chosen by specialists (68.37%) than by PC paediatricians (47.24%). Other prescribed treatments include nasal irrigation with saline solution (59%), anti-inflammatory/analgesic drugs (55.5%), and nasal corticosteroids (29%). Nebulised medication is recommended by 11% (Figure 5).
The respondents reported suspecting complications when there is persistent fever and poor general status (92.75%), altered ocular motility (79.47%), proptosis (79.37%), focal neurologic signs (72.54%), and evidence of intracranial hypertension (61.46%).
They made urgent referrals to the hospital if complications were suspected (70.72%) or did routine referrals to ORL (34.40) or the hospital (29.27%) in case of therapeutic failure. Only 0.5% referred every case to ORL.
The symptoms reported as being suggestive of non-infectious aetiology were unilateral rhinorrhoea (81.2%), nasal congestion, watery eyes, sneezing, and watery rhinorrhoea (75%), headache that wakes the patient at night (71.8%) and abnormal pulmonary auscultation (51.7%).
DISCUSSION
We present the results of a nationwide survey conducted mainly among PC paediatricians, which showed that in cases of protracted cold symptoms lasting over 14 days, 70% of paediatricians prescribed pharmacological treatment. Sinusitis was suspected in about 1% of all visits, and 76.6% of sinusitis cases were diagnosed on the basis of clinical criteria alone. Antibiotics were prescribed in nearly 90% of the cases, alone or in combination with other therapies. The most frequently used antibiotic agent was amoxicillin-clavulanate. Although there were some deviations, these data showed a great degree of adherence to the most recent Clinical Practise Guidelines.1,3,4,9
It is hard to know the prevalence of sinusitis for various reasons. As for the definition of the illness, according to the International Classification of Primary Care (ICPC) (included in the software used in many autonomous communities) it consists of “purulent nasal/post-nasal discharge, or previous medically treated episodes of sinusitis, plus tenderness over one/more sinuses, or deep-seated aching facial pain aggravated by dependency of head, or opacity on transillumination; or imaging evidence of sinusitis; or pus obtained from the sinus”. This definition is in clear contrast with the most recent recommendations for the diagnosis and use of complimentary tests and incorporated to a large extent in everyday clinical practise. The second challenge is the lack of proper documentation in medical records, as sometimes symptoms are documented, such as rhinorrhoea, persistent rhinorrhoea, or persistent cough, as opposed to processes, or else an early diagnosis, such as acute respiratory infection, remains unchanged even when the course of the disease shows that there is a different entity at work. We thought it would be interesting to open the survey on the management of sinusitis with data pertaining to URTIs, as both processes are closely related and in most cases the symptoms can correspond to either, so that they can only be differentiated by duration and severity criteria.
It is estimated that children have between 6 and 8 viral infections of the upper respiratory tract a year, of which 5% to 13%2 can be complicated by a bacterial superinfection of the paranasal sinuses. Thus, sinusitis was reported in 6.5% of URTIs in healthy children one to ten years of age11 and in 8% of children 6 to 35 months of age, with the peak incidence (10%) occurring in the second year of life12. In the United States, yearly rates of about 11 to 14 visits per 1000 children under 18 years of age have been reported, with 13 for the 0-5 age group, 9 for the 6 to 11 year group, and 15 for children ages 12 to 17 years.7 The reported rate in Europe ranges from 2 to 18 visits for every 1000 in children ages 0 to 17 years, with a lower incidence in the younger ages5. According to the data of the survey, most paediatricians (90%) see 10-20 cases of sinusitis for each 1000 visits (69% saw 10 cases), a figure that is quite consistent with those mentioned above and with the figure reported in a morbidity study conducted in PC paediatric offices in Asturias, which reported a diagnosis of sinusitis in 2.1% of the episodes of respiratory disease, which themselves amounted to 44.8% of all documented visits.13
At present, the recommendation for the diagnosis of sinusitis in all the Clinical Practise Guidelines1,3-5 and the recently published Spanish Consensus Document9 is that it must be made on the basis of clinical criteria in any of these three patterns: cold symptoms lasting over 10 days without improvement, symptoms that worsen after 6-7 days after having started to improve, or symptoms with an unusually severe onset with fever and purulent rhinorrhoea lasting more than 3-4 days. The key symptoms that are taken into account to diagnose sinusitis are rhinorrhoea and cough for the first pattern, and rhinorrhoea, cough, and the resurgence of fever for the second. These are also the symptoms, grouped into various combinations, reported in our survey: the most frequent ones were persistent/purulent rhinorrhoea (89%) and facial pain/headache (84%). Very few paediatricians (7.7%) mentioned a single symptom as a basis for a suspected diagnosis of sinusitis. In this regard, we should note that while headache could be the only symptom in some patients (sphenoiditis), both headache and facial pain in isolation of any other symptoms are not usually indicative of sinusitis.14 In another study done by means of an online survey of United States paediatricians, which we cannot use to make an exact comparison with our data because the possible answers had different categories, the clinical feature most frequently considered important was persistent duration of symptoms, as reported by 93% of the paediatricians, followed by purulent rhinorrhoea for 55%, nasal congestion for 43%, and headache and night-time cough for 32% and 29%, respectively.6 Among paediatricians 95% reported they were less likely to make the diagnosis if the symptoms were improving. The issue of improvement, or the absence thereof, is considered very important by the Guidelines when it comes to diagnosing a bacterial infection.4
According to our survey, only 22% of paediatricians would do a radiological study for the purposes of diagnosis, which would be more frequent in specialists than in PC doctors, in accordance with the recommendation of not doing radiological studies in uncomplicated, non-severe, non-recurrent sinusitis or in patients without underlying disease15 currently included in all Clinical Practise Guidelines1,3-5 and the Spanish Consensus Document,9 and which contrasts with the aforementioned United States study, in which over half the paediatricians surveyed reported requesting, at least occasionally, a computerised tomography scan (58%) or a radiography of the sinus (40%), and 70% reported requesting one of these two radiology tests, to aid in the diagnosis of non-severe sinusitis.6
In our survey, paediatricians reported prescribing antibiotics in 90% of the cases, in 18% as the sole treatment, a figure consistent with those previously published (82% and 92%) in the context of PC and hospital emergency services,7,16 with data collected from medical records (82%)7 and online surveying, in which 95% reported treatment with antibiotics either frequently or very frequently.6
Antibiotic prescription for the treatment of sinusitis is a generalised yet controversial practise, as sinusitis is a self-limiting disease with high rates of spontaneous resolution.17 There are few studies comparing the results of placebo and antibiotic administration.11,18-20 Furthermore, these studies include a small number of cases and the inclusion criteria, that is, the definition of a case, as well as criteria for improvement and/or resolution, and the type and dosage of antibiotic used, are not consistent. There are two meta-analytical studies, one of which concludes that antibiotic treatment at the studied doses does not show benefits in children with acute sinusitis,21 while the second concludes that the efficacy of antibiotic treatment, with an odds ratio of 2 (95% CI 1.16 to 3.47) is not supported by strong evidence, and that the diagnostic and inclusion criteria need to improve.22
As for which antibiotic agent is used, the literature describes a significant percentage of inappropriate prescription in 42% of ambulatory visits8 and in 22% of hospital paediatric emergency services16. While the Guidelines recommend amoxicillin or amoxicillin-clavulanate as first-line treatment and discourage or condone with strong reservations and in very specific cases the use of macrolides,9 these drugs are used in up to 18% of cases, a figure that is not justified given the rates of penicillin allergy. We should note that in contrast to these published data, the intention to prescribe reported in our survey adheres to the recommendations almost completely, as it corresponds to amoxicillin and amoxicillin-clavulanate, with minimal prescription of cephalosporins and macrolides, and no prescription of quinolones. These figures are similar to those obtained in the United States survey.6 It could be that the use of amoxicillin-clavulanate exceeds the recommendations, at least in relation to the Spanish Consensus Document.9
The higher frequency of radiological examination requests and of the use of amoxicillin-clavulanate reported by paediatric specialists could be associated to the care, at this level, of patients with poor progression in whom a first course of treatment has failed, or patients with suspected complications.
When it came to adjuvant therapies, the most used would be, along with anti-inflammatory and analgesic drugs, physiological saline solution for nasal washes (60%) and nasal corticosteroids (30%), which are the treatments that seem to have demonstrated a certain efficacy in the recent literature.23,24 We should also note that the respondents demonstrated competent knowledge of both the symptoms suggestive of complications, a circumstance that would determine urgent referral to the hospital, and the symptoms that suggest a non-infectious aetiology.
It is interesting to note the influence that the opinion of parents has in the diagnostic and therapeutic decisions of paediatricians. This was manifested both in our survey, where 4% admitted to treating URTIs with drugs as a result of family pressure, and in the United States survey, in which 13% agreed that they were more likely to diagnose sinusitis if they thought parents expected the diagnosis, and 16% that they were more likely to treat it with an antibiotic if they thought parents expected this kind of therapy.6
This study has some limitations. Firstly, this is a survey, that is, it does not reflect the reality of clinical practise but theoretical opinions about it, with answers that involve the subjective assessment of the provider of his practise; the questions do not address specific clinical scenarios, but are questions about clinical practise in general terms. Second of all, the number of responses we obtained was relatively high, but we cannot be certain that our sample represents the overall population of Spanish paediatricians. In Spain there has been a very recent experience, the ABES study10, where they obtained 1214 responses and with a broader population, as it was addressed to all Spanish paediatricians, of any specialty, members of the AEP, over 9000 at the time, while our survey was only addressed to providers that cared for patients with these conditions. Considering that of the 9036 paediatricians member of the AEP 6215 are PC paediatricians, the level of care at which most cases of this pathology are treated, the proportion of responses is greater than the one achieved in the ABES study.10 The study may be biased due to its characteristics and to the fact that the paediatricians that responded may be professionals used to sharing experiences and opinions with other colleagues, so they have joined mailing lists, and could have a greater motivation not only to answer the questionnaire but also to keep their knowledge updated.
In short, we can conclude that the survey addressed to Spanish paediatricians about hteir knowledge and clinical management of two conditions, URTI and sinusitis, suggests a high degree of adherence to the most recent Clinical Practise Guidelines and to the Spanish Consensus Document published later on, underscoring the scarce use of prescribed antibiotics in URTIs, the diagnosis based on clinical criteria and not radiology of sinusitis, and the antibiotics chosen to treat the latter. Nevertheless, we believe that the recent publication of the Consensus could contribute even more to the appropriate diagnosis and treatment of patients with sinusitis in clinical practise, something that could and should be studied in the near future.
ACKNOWLEDGMENTS
We would like to thank the Boards of the AEP and the AEPap, for facilitating the distribution of the survey among their members, and all colleagues that chose to participate.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ACRONYMS: AEP: Asociación Española de Pediatría (Spanish Association of Paediatrics) • AEPap: Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics) • PC: Primary Care • 95% CI: 95% confidence interval• URTI: upper respiratory tract infection • ORL: otorhinolaryngology. • HCC: Health Care Centre.
BIBLIOGRAPHY
- Callén Blecua M, Garmendia Iglesias MA. Sinusitis. El Pediatra de Atención Primaria y la sinusitis. Protocolos del GVR (publicación P-GVR-7) [on line] [consulted on 31/07/2013]. Available in http://aepap.org/grupos/grupo-de-viasrespiratorias
- American Academy of Pediatrics. Clinical Practice Guideline: Management of Sinusitis. Pediatrics. 2001;108:798-808.
- Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, et al. Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54:e72-e112.
- Wald E, Applegate K, Bordley C, Darrow D, Glode M, Marcy S, et al. Clinical Practice Guideline for the Diagnosis and Management of Acute Bacterial Sinusitis in Children Aged 1 to 18 Years Pediatrics. 2013;132:e262-e280.
- Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinology. 2012;50 (Supl 23):1-298.
- McQuillan L, Crane LA, Kempe A. Diagnosis and management of acute sinusitis by pediatricians. Pediatrics. 2009;123:e193-8.
- Shapiro D, Gonzales R, Cabana M, Hersh A. National Trends in visit Rates and Antibiotic Prescribing for children With Acute Sinusitis. Pediatrics. 2011;127:28-34.
- Cox E, Saluja S. Criteria-Based Diagnosis and Antibiotic Overuse for Upper Respiratory Infections. Ambulatory Pediatr. 2008;8:250-4.
- Martínez Campos L, Albañil Ballesteros R, de la Flor Bru J, Piñeiro Pérez R, Cervera J, Baquero Artigao F, et al. Documento de consenso sobre etiología, diagnóstico y tratamiento de la sinusitis. Rev Pediatr Aten Primaria. 2013;15:203-18.
- Piñeiro Pérez R, Calvo Rey C, Medina Claros AF, Bravo Acuña J, Cabrera García L, Fernández-Llamazares CM, et al. Uso empírico de antibióticos en niños en España. Resultados de una Encuesta Pediátrica Nacional 2012 (Estudio ABES). An Pediatr (Barc). 2013;79:32-41.
- Wald E, Nash D, Eickhoff J. Effectiviness of amoxicillin/clavulanate potassium in the treatment of acute bacterial sinusitis in chidren. Pediatrics. 2009;124:9-15.
- Revai K, Dobbs LA, Nair S, Patel JA, Grady JJ, Chonmaitree T. Incidence of acute otitis media and sinusitis complicating upper respiratory tract infection: the effect of age. Pediatrics. 2007;119:e1408-e1412.
- Domínguez Aurrecoechea B, Martín Rodríguez D, García Mozo R. Morbilidad en Pediatría de Atención Primaria en Asturias. Rev Pediatr Aten Primaria. 2006;8:21-37.
- National Institute for Health and Clinical Excellence. Clinical Knowledge Summaries. Sinusitis. Additional information [on line] [consulted on 26/06/2013]. Available in http://cks.nice.org.uk/sinusitis#!diagnosissub
- American College of Radiology. ACR Appropiateness Criteria sinusitis Children. Última revisión 2012 [on line] [consulted on 26/06/2013]. Available in www.acr.org/~/media/485AEEC108E941C6B5551A8D21017EED.pdf
- Ochoa C, Inglada L, Eiros JM, Solís G, Vallano A, Guerra L. Appropriateness of antibiotic prescriptions in community-acquired acute pediatric respiratory infections in Spanish emergency rooms. Pediatr Infect Dis J. 2001;20:751-8.
- Acute Bacterial Sinusitis Guideline Team, Cincinnatti Children’s Hospital Medical Center: Evidence-Based Care Guideline for medical management of Acute Bacterial Sinusitis in children 1 through 17 years of age [on line]. Available in www.cincinnatichildrens.org/workarea/linkit.aspx?linkidentifier=id&itemid=87964&libid=87652
- Wald ER, Chiponis D, Ledesma-Medina J. Comparative effectiveness of amoxicillin and amoxicillin-clavulanate potassium in acute paranasal sinus infections in children: a double-blind, placebo-controlled trial. Pediatrics. 1986;77:795-800.
- Garbutt JM, Goldstein M, Gellman E, Shannon W, Littenberg B. A randomized, placebo-controlled trial of antimicrobial treatment for children with clinically diagnosed acute sinusitis. Pediatrics. 2001;107:619-5.
- Kristo A, Uhari M, Luotonen J, Ilkko E, Koivunen P, Alho OP. Cefuroxime axetil versus placebo for children with acute respiratory infection and imaging evidence of sinusitis: a randomized, controlled trial. Acta Paediatr. 2005;94:1208-13.
- Guarch Ibáñez B, Buñuel Álvarez JC, López Bermejo A, Mayol Canals L. El papel de la antibioterapia en la sinusitis aguda: revisión sistemática y metaanálisis. An Pediatr (Barc). 2011;74:154-60.
- Cronin MJ, Khan S, Saeed S. The role of antibiotics in the treatment of acute rhinosinusitis in children: a systematic review. Arch Dis Child. 2013;98:299-303.
- Kassel JC, King D, Spurling GK. Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst Rev. 2010;3:CD00682.
- Zalmanovici A, Yaphe J. Intranasal steroids for acute sinusitis. Cochrane Database Syst Rev. 2011;4:CD005149.