Vol. 14 - Num. 55
Original Papers
Who goes with patients to the pediatrician? The accompanying personof pediatric patients in primary care
Andrea Lacasa Maseria, Sonia Lacasa Maserib, Juana M.ª Ledesma Albarránc
aMIR segundo año. MIR-Pediatría. Málaga. España.
bMIR-Pediatría. Servicio de Pediatría del Hospital Regional Universitario Carlos Haya. Málaga. España.
cPediatra. CS Delicias. Málaga. España.
Correspondence: A Lacasa. E-mail: andrealacasa@gmail.com
Reference of this article: Lacasa Maseri A, Lacasa Maseri S, Ledesma Albarrán JM. Who goes with patients to the pediatrician? The accompanying personof pediatric patients in primary care. Rev Pediatr Aten Primaria. 2012;14:217-24.
Published in Internet: 01-10-2012 - Visits: 17701
Abstract
Introduction: today, cultural changes may have changed the usual pattern of the mother as the accompanying person in the pediatric office.
Objetives: descriptive analysis of the current situation in the pediatrics office.
Material and methods: Las Delicias Health Center (health district of Malaga). Selected sample of 250 patients between the periods 1-15 July and 15-30 September, 2011.
Results: in most cases (54.8%), the mother stands as the main accompanying person, appearing both parents in the consultation in 16.4% of cases. The figure of the grandparents is of special significance when the mother is an active worker. Most consultations were on-demand by appointment (82.4%), for acute symptoms, with symptoms lasting less than 3 days in most cases (59.2%).
Discussion: the mother is presented as the main accompanying person in most cases. The father or grandparents will be present in front of social-cultural factors, mainly active employment status of the mother.
Keywords
● Clinical interview ● Pediatric consultation ● Primary careINTRODUCTION
The clinical interview is an essential competence (the basis of the visit) of the Primary Care paediatrician, so communication is a crucial element in the doctor-patient relationship1. Healthcare services and their outcomes depend on how the professional and the service-seeker communicate, since productive communication is a key element toward the recovery of health2. The doctor-patient relationship is different in the field of paediatrics than in other medical specialties, since other individuals besides the child are involved in it. In this field, the accompanying adult that comes to the paediatrician’s office becomes a key player in establishing an appropriate doctor-patient relationship3.4.
Traditionally, it was customary for the mother to accompany her child to the clinic, since from a socio-cultural standpoint she was considered the person in charge of the children. Furthermore, many families perceive the management of healthcare issues as one of the responsibilities of the mother, regardless of whether or not she works outside the home5. Several studies have confirmed that most of the time the children are accompanied by their mothers to the paediatrician’s office, in over 90% of cases, followed by grandmothers, aunts, and sisters6.
We are all aware that socio-cultural shifts have been happening in our environment for about two decades leading to the incorporation of women into the workforce; a shift that has intensified in recent years given the delicate financial situation of many families. This fact may have modified the traditional schema of the mother as the main accompanying adult in the paediatric clinic, and may need to be taken into account if we are to develop an approach to healthcare that works well.
The entry of women into the workforce has brought on one of the deepest social changes of this century. This calls for the configuration of a system which takes into account the newly emerged social relationships and allows a new way for men and women to cooperate and compromise, so that they can attain an equitable division of responsibilities in their professional and personal lives. The need to reconcile work and family has been broached in the European Union and other countries as one that is unequivocally tied to the new social reality. This poses a complex and difficult challenge that must be addressed not only through important legislative reforms (Organic Law 3/2007 dated 22 March for the effective equality of men and women), but also through the promotion of additional services to the public within a broader framework of family policy. The aforementioned law introduces legislative changes in the work environment so workers can participate in family life, taking a new step toward equal opportunity for men and women. At the same time, it makes it easier for men to share the care of their children from the very moment of their birth or their incorporation in the family7.
The objective of the present study is to perform a descriptive analysis of the current situation in the paediatric office in order to learn what the profile and characteristics of the main accompanying adult are.
MATERIALS AND METHODS
We did an observational descriptive cross-sectional study on a sample of the population served by a paediatric office in the Healthcare Centre of Las Delicias (Málaga City health district, Spain), analysing all the visits that took place from 8:30 to 15:00 pm Monday through Friday during the period under study (July 1-15 and September 15-30 2011).
We calculated the sample size for an expected proportion of 5%, a precision of 5%, and a 95% confidence interval, which resulted in n = 203. For practical purposes, aiming to facilitate the distribution of patients in relation to the school holidays, we chose a final sample size of 250 patients (125 patients in July and 125 patients in September).
The families were informed that the data was going to be collected, and all patients participated in the study voluntarily after the legal representative of the patient had given consent in writing. The following data were collected at each visit: age of the child and parents, who was accompanying the child (mother, father, both parents, grandparents, etc.), the type of visit (scheduled routine visit, scheduled appointment by demand, unscheduled appointment by demand), type of acute pathology (and duration of symptoms in days) or chronic pathology, school period (holiday or term), and the education level and employment status of the father and the mother.
For the statistical analysis, we did numerical summaries for quantitative variables and percentages for qualitative variables. We used a 95% confidence interval (95% CI). When it came to variable comparison, we performed Student’s T-test to compare means, and Pearson’s chi-squared test to compare percentages. The data were analysed using the SPSS® 15.0 application for Windows®.
RESULTS
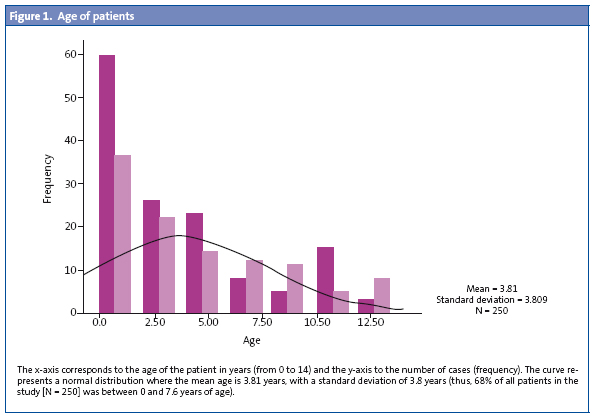
We studied 250 visits (125 from July 1st through 15th, and 125 from September 15th through 30th) in which 55% of the patients were boys and 45% girls, with ages ranging from 1 month to 14 years (the average age was three years) (Fig. 1).
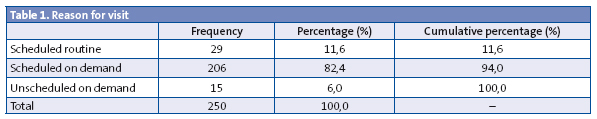
Out of all visits, 206 were appointments scheduled on demand (82.4%), 29 (11.6%) were routine visits scheduled in accordance with the PSI (Programa de Salud Infantil), the healthy child programme, and lastly 25 were unscheduled appointments on demand (6%) (Table 1).
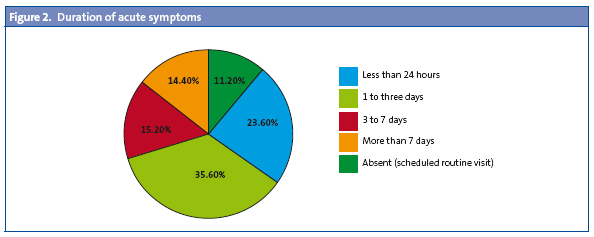
In 13.6% of the cases there had been a previous visit for the same reason. In 88.4% of the visits (221 patients) services were sought due to an acute pathology, with symptoms that had been present for one to three days in 35.6% of the cases (89 patients), for less than 24 hours in 23.6% (59 patients), from three to seven days in 15.2% (38 patients) and with symptoms lasting over seven days in the remaining cases (Fig. 2). As we mentioned above, 50% of the visits took place during the school holidays, and the remaining 50% during the school term.
When it came to the accompanying adult, on average the child was accompanied by one adult (95% CI), who was the mother only in 54.8% of the cases (137 visits), the father only in 8% (20 visits), and with both parents accompanying the child in 16.4% of the cases (41 visits). Children were accompanied by grandparents in 10% of the cases (25 visits), and in 8% of the cases (20 visits) the accompanying adults consisted in one parent and a grandmother. In 21% of the visits the child was accompanied by another person (aunt or uncle, older sibling, etc.), independently of the presence or not of the mother, the father, or the grandparents.
If we look at the data on the parents, and at the mother figure in particular, the average age was of 36 years (95% CI: 41 to 31); 63.2% (158 cases) were employed at the time of the clinical interview, and when it came to the education level, 28.8% (72 cases) had finished elementary school, 44.4% (111 cases) have finished high school, and 26.8% (67 cases) had college-level studies. As for the father, the average age was 38 years (95% CI: 45 to 31); 80.4% (201 cases) were actively employed at the time of the clinical interview, and in terms of their level of education, 28.8% (72 cases) had finished elementary school, 46.8% (117 cases) had graduated from high school, 20.4% (51 cases) had college-level studies, and 4% (10 cases) had no formal education.
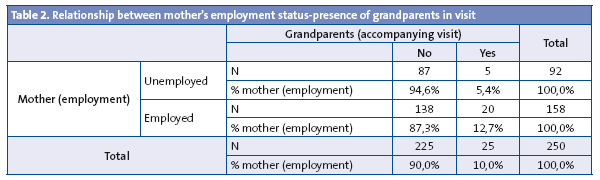
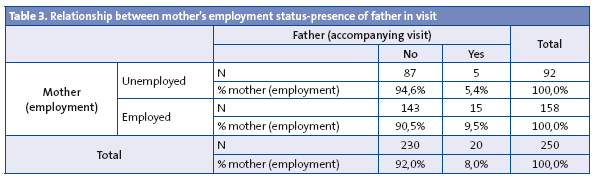
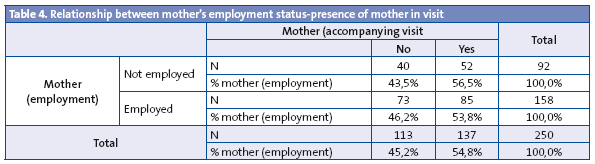
When we take into account the employment status of the mother in the bivariate analysis, we can observe considerable differences: when the mother is actively employed, we see that the grandparents come to the visit in 12.7% of the cases, compared to 5.4% (p = 0.06) (Table 2), and the father in 9.5% of the cases compared to 5.4% of the cases (Table 3); however, when it came to the mother herself accompanying the child, her being actively employed or not did not make a difference in frequency (56.5 compared to 53.8%) (Table 4).
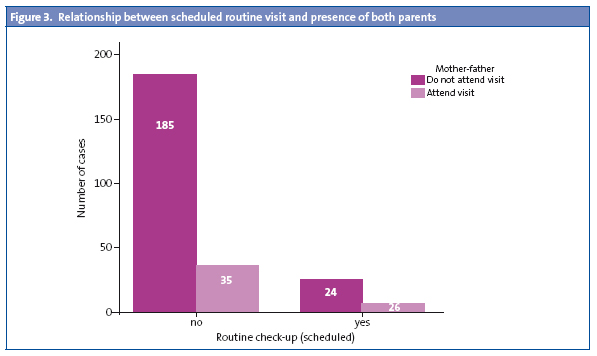
We observed no differences in the presence or absence of the father in relation to his level of education. In terms of the type of visit to the office (whether it was a scheduled routine visit or an appointment on demand) we observed the following: the mother attended the visit with practically the same frequency whether the visit was a scheduled routine one or not (63 versus 53%); as for the father, we observed that he tended to come more often to scheduled routine visits (20%) than to appointments on demand (15%) (Fig. 3).
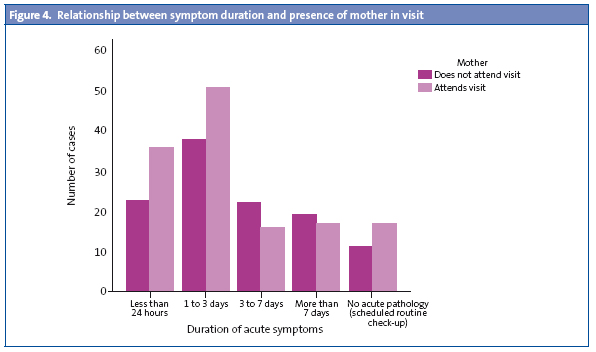
Looking at the duration of the symptoms, we see that the mother tends to accompany the child more often when the symptoms have lasted less than 24 hours (61% compared to 39%) and between one and three days (57% versus 42%) (Fig. 4). When it came to the number of people accompanying the child, the data did not show variations in relation to the visit taking place during the school holidays as opposed to the school term.
DISCUSSION
The paediatric visit is based on the relationship established between the physician, the child, and the adult that accompanies the latter, an adult who, generally speaking, tends to be a parent, and more specifically the mother. In this context, the adult that accompanies the child to the paediatric visit must be able to meet certain necessary requirements to be able to establish an appropriate relationship with the healthcare professional: handling the patient, providing the information needed to make a diagnosis, and participating in the care of the child on a regular basis3.
As for the results of our study, we found that the child was accompanied to the visit in 100% of the cases, with the mother being the most frequent accompanying adult, followed by both parents together, and lastly by the grandparents. The father also was the accompanying adult in a considerable percentage of cases, a fact that seems to be associated to the mother’s active employment status, although in our study the level of education of the father did not seem to influence whether he came to the visit or not. The employment status of the mother had a significant influence on the presence or absence of the grandparents in the paediatric visit, with employment having the effect of doubling their presence. Last of all, the type of visit had no effect on the presence of the mother as the accompanying adult, since the mother attended whether the visit was on demand or a scheduled routine visit. When the symptoms had lasted for fewer than three days, the mother was the accompanying adult in practically 100% of the cases.
While women are playing an increasingly relevant role in today’s society, in most cases they continue to be the main caregiver of the children, and thus the most frequent accompanying adult in the paediatric office. Taking into account the socio-cultural changes that have occurred in recent years, and based on the results obtained in our study, the father is gaining relevance in the role of main caregiver to the children and in accompanying them to healthcare visits.
We must address the task of making the paediatric office easily accessible to both parents, as it is yet another factor that plays in the reconciliation of work and family life. The reconciliation of work, family and personal life is a strategy that facilitates the fulfilment of the effective equality of men and women. Its purpose is to achieve a new organisation of the social and economic system where men and women can make the different facets of their lives compatible: work, family, leisure, and personal time. Therefore, the reconciliation of family, work, and personal life contributes to building a society based on the quality of life of its people, that offers the same opportunities to men and women so they can develop in every aspect of their lives, advance professionally, attend to their familial responsibilities, and be able to enjoy their family and personal time. For these goals to be achieved, the reconciliation of work, family, and personal life requires that certain challenges be met:
- The development of social resources and structures that allow serving and caring for dependent persons (children, the elderly, the sick, and disabled individuals).
- The reorganisation of work spaces and schedules.
- The implementation of measures in workplaces that allow employed individuals to develop in the different facets of their lives.
- The modification of the traditional roles of men and women in relation to their involvement in family, home, and workforce.
Thus, there needs to be a social shift that introduces new models of organisation, and it necessitates the participation of all social agents from a position of shared responsibility8.
A professional relationship with patients and families based on the active participation of the former in decision making leads to satisfaction and better clinical outcomes, since it increases efficacy in the identification and resolution of medical problems, as well as treatment compliance. It is the duty of both the paediatrician and the entire healthcare team to foster communication skills that facilitate the establishment of an optimal clinical relationship between the paediatrician, the child, and his parents, who at present are the main accompanying adults9.
The clinical relationship with the patient and his caregivers plays a decisive role in the outcome of all activities associated to healthcare. The clinical interview is considered an essential piece in the doctor-patient relationship. The goals of the clinical interview in paediatric care are:
- Learning the reason why the patient and his family are coming to the doctor’s office.
- Prescribing a treatment or recommending a course of action.
- Establishing a satisfactory healthcare relationship with the parents and the child10.
The ability to learn and understand why a patient and his parents come seeking help and advice, and to agree on a course of action with them, demands technical skills from the paediatrician, but also communication skills. Treating a patient and his parents does not consist solely of diagnosing a disease and prescribing an evidence-based treatment. There are biological, psychological, and social components to health and disease, and this is why it is critical that the physician establishes a connection with every aspect of the person from the outset11.
CONFLICT OF INTERESTS
The authors declare that they have no conflict of interest in regard to the preparation and publication of this article.
ACRONYMS: 95% CI: 95% confidence interval
BIBLIOGRAPHY
- López García-Ramos L, López Martín D, Berbel Jiménez FJ, Pérez de Colosía Civantos M, Pedregal González M. Influencia del acompañante en la negociación y la duración de la consulta en atención primaria. Aten Primaria. 2009;41(3):147-51.
- Castillo Barrera J, Schwartz Calero P, Pardo Álvarez J, Ortega Carpio A, Aguilar Valadez C, Pedregal González M. El acompañante en la entrevista clínica: frecuencia y técnicas utilizadas. Medicina de Familia (And). 2003;2:136-8.
- Domínguez Aurrecoechea B, Alonso Lorenzo J. Acompañantes de los niños a la consulta de pediatría: ¿algo está cambiando? Aten Primaria. 1998;22(1):444-9.
- Quiroz R. La consulta pediátrica. Rev Perú Pediatr. 2007;60:65-6.
- Caroli PL, Navia MJ. Presencia del padre en la consulta pediátrica. Arch Arg Pediatr. 2006;104:325-7.
- Santiago B. El 90 por ciento de los acompañantes de los niños enfermos son sus madres. En: Repercusiones biopsicosociales y educacionales en la hospitalización infantil. Santiago de Compostela: Fundación María José Jove; 2011.
- Ley Orgáncia 3/2007, de 22 de marzo, para la igualdad efectiva de mujeres y hombres. BOE número 71 de 23/3/2007; p. 12611-12645.
- Ministerio de Igualdad. Conciliación de la vida laboral, familiar y personal. Madrid: Ministerio de Igualdad; 2010.
- Arroba Basanta ML, Dago R, Manzarbeitia P. Entrevista clínica en Pediatría: teoría y práctica. Rev Pediatr Aten Primaria. 2010;12(Supl 19):263-70.
- Arroba Basanta ML, Dago R. Relación clínica y comunicación asistencial en pediatría. Primera parte. ¿Disfrutamos del encuentro clinic con nuestros pacientes? Form Act Pediatr Aten Prim. 2008;1(1):27-33.
- Arroba Basanta ML, Dago R. Relación clínica y comunicación asistencial en pediatría. Segunda parte. La exploración. Form Act Pediatr Aten Prim. 2008;1(2):88-94.





