Vol. 26 - Num. 102
Originales
La especialidad de Pediatría sigue teniendo interés para los residentes
Pedro J. Gorrotxategi Gorrotxategia, Concepción Sánchez Pinab, Carmen Villaizán Pérezc, M.ª Teresa Cenarro Guerrerod, M.ª Dolores Cantarero Vallejoe, Eva Suárez Vicentf, Marianna Mambié Meléndezg
aPediatra. CS Pasajes San Pedro. Pasajes. Guipúzcoa. España.
bPediatra. CS San Andrés. Madrid. España.
cPediatra. CS Toledo 4-Santa Bárbara. Toledo. España.
dPediatra. CS José Ramón Muñoz Fernández-Ruiseñores. Zaragoza. España.
ePediatra. CS Illescas . Illescas. Toledo. España.
fPediatra. CS. Burriana II. Burriana. Castellón. España.
gPediatra. CS Son Serra-La Vileta. Palma de Mallorca. España.
Correspondencia: PJ Gorrotxategi. Correo electrónico: pedro.gorrotxa@gmail.com
Cómo citar este artículo: Gorrotxategi Gorrotxategi PJ, Sánchez Pina C, Villaizán Pérez C, Cenarro Guerrero MT, Cantarero Vallejo MD, Suárez Vicent E, et al. La especialidad de Pediatría sigue teniendo interés para los residentes . Rev Pediatr Aten Primaria. 2024;26:147-54. https://doi.org/10.60147/a45613e8
Publicado en Internet: 13-06-2024 - Número de visitas: 15538
Resumen
Introducción: el objetivo de este trabajo es analizar el interés de los residentes que inician su formación por la especialidad de “Pediatría y sus áreas específicas” en función del retraso en la adjudicación de la última plaza en las pruebas selectivas.
Metodología: análisis de los datos obtenidos del registro del proceso de elección del MIR (médico interno residente) de los últimos nueve años, de las plazas de Pediatría en el sistema nacional de salud y del estudio sobre necesidades de especialistas 2021-2035.
Resultados: en los últimos nueve años ha habido un aumento del número de plazas de 392 a 501. Al haber más plazas, automáticamente se retrasa la adjudicación de la última plaza. De esa forma, el retraso ha sido del 49%, pero sin el aumento de plazas habría sido del 17%. El número de residentes que no pueden elegir Pediatría ─porque cuando llega su opción de elegir las plazas de Pediatría, estas se han agotado─ ha aumentado de 2703 a 3469, un 28%. Dado que el grado de abandonos es mínimo, habría habido la posibilidad de ofertar más plazas que se cubrirían de forma adecuada. Las ofertas de trabajo son un 65% en Atención Primaria y un 35% hospitalarias.
Conclusiones: la Pediatría sigue siendo una especialidad atractiva para los aspirantes a la formación MIR. En el caso de que aumentaran las plazas, habría más residentes que optarían por la especialidad de Pediatría. Dado que la salida profesional mayoritaria es la Atención Primaria, habría que reforzar este aspecto en la formación MIR.
Palabras clave
● Docencia ● MIR (médico interno residente) ● Pediatría de Atención PrimariaINTRODUCCIÓN
La difícil situación en la que se encuentra la Atención Primaria (AP) está haciendo que en la elección MIR (médico interno residente) de la especialidad de Medicina de Familia queden plazas sin ser cubiertas. Armando Martín-Zurro afirma: “La situación actual de la AP española se podría calificar como «preocupante». La sobrecarga asistencial, la falta de profesionales para cubrir sustituciones y lugares de trabajo de especial dificultad, el exceso de burocracia, la ausencia de perspectivas positivas de crecimiento personal y profesional, los problemas de conciliación o de sueldos bajos y la precariedad laboral son algunos ejemplos de las causas últimas del burnout, del llamado síndrome del profesional quemado, que se extiende como la pólvora en el seno de la AP”1. Podría ser que esa situación afectara también a la especialidad de Pediatría, en la que las mayores salidas profesionales se encuentran en AP y que ello dificultara la satisfacción de los residentes con las plazas de Pediatría.
Hay reportajes periodísticos en los que se hace referencia a que el interés por la Pediatría es menor en los residentes, dando a entender que ha perdido atractivo esta especialidad. En uno de los artículos publicados, Los médicos con las mejores notas MIR ya no quieren ser pediatras: así se “desinfla” la especialidad2, se afirmaba que la especialidad se ha “desinflado” y atribuye ese problema a la realización de guardias: 'En las especialidades de primera llamada, como es el caso de Pediatría, las guardias se han convertido en trabajar a destajo las 24 horas seguidas”. Una pediatra consultada también hace referencia a las malas condiciones de trabajo: “Si los futuros residentes ven que los pediatras de AP están saturadísimos de trabajo y sus condiciones laborales no son buenas, no es de extrañar que se decanten por otra especialidad”; por último, en el mismo artículo antes citado, un representante de la Asociación Española de Pediatría de Atención Primaria (AEPap) expresaba una opinión totalmente contraria, afirmando que la Pediatría es una especialidad muy atractiva para el profesional porque estás en contacto con los pacientes, y concluía diciendo que 'la Pediatría no está de capa caída'.
Teniendo en cuenta estas diferentes visiones de los profesionales de la Pediatría, vamos a realizar un estudio para analizar, en primer lugar, si es real la disminución de la aceptación de la especialidad de Pediatría para los MIR y en qué medida se da ese retraso de la adjudicación de las plazas; y, en segundo lugar, las perspectivas laborales de la Pediatría como especialidad médica.
METODOLOGÍA
Se realiza el análisis de los datos de la adjudicación de la última plaza de Pediatría en los últimos 9 años. Para ello, nos basamos en el informe del Centro de Estudios del Sindicato Médico de Granada Distribución adjudicaciones de plazas MIR en 20233.
Se realiza el análisis del número de plazas de Pediatría en AP y hospitalaria en los últimos 10 años en base a los datos del Ministerio y el análisis de la situación de la Pediatría por medio del estudio sobre necesidades de especialistas 2021-2035.
En primer lugar, analizamos el proceso de elección de plazas MIR y nos hacemos las siguientes preguntas: ¿Se ha retrasado la adjudicación de las plazas de Pediatría en la convocatoria MIR?, ¿Qué factores influyen en que la elección se prolongue? y ¿Cuántos aspirantes a la especialización se quedan sin poder elegir plaza de Pediatría?
En segundo lugar, para analizar la situación de la Pediatría, nos preguntamos sobre aspectos relacionados con las salidas profesionales y con la Pediatría de Atención Primaria: ¿Cuáles son las salidas profesionales para los residentes de Pediatría? y ¿Está en peligro la Pediatría de Atención Primaria?
RESULTADOS
¿Se ha retrasado la adjudicación de las plazas de Pediatría en la convocatoria MIR?
A esta pregunta responden los datos del informe de elección MIR, del 9 de mayo de 2023, que ha recogido el Centro de Estudios del Sindicato Médico de Granada, titulado: Distribución adjudicaciones de plazas MIR en 20233. En dicho informe hay una relación de todas las plazas, cuál es la primera que se adjudica por especialidad y cuál es la última.
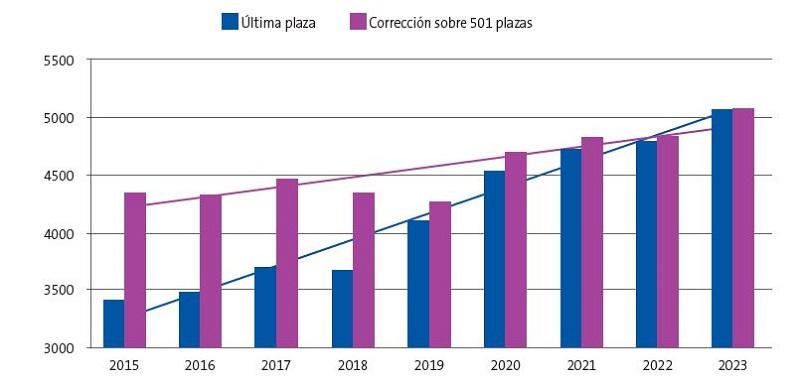
El informe ofrece estos datos de los últimos 9 años y en una primera visión parece que se ha retrasado mucho la adjudicación de las plazas: en 2015 la última plaza de Pediatría fue la 3399 y en 2023, la 5081, con lo que ha aumentado un 49%. Sin embargo, esto no es una situación real, porque en ese periodo el número de plazas aumentó de 392 a 501. Realizando la corrección en relación con la diferencia de plazas, el retraso en la adjudicación de las plazas ha sido de un 17%, como se puede ver en la Figura 1.
| Figura 1. Evolución de la última plaza en la que se asigna la especialidad de Pediatría |
|---|
 |

¿Qué factores influyen en que la elección se prolongue?
Un factor importante en la prolongación de la adjudicación de las plazas es el número total de plazas de la especialidad.
Un ejemplo que podemos poner es el caso de Medicina Legal y Forense. Ha sido la quinta en terminar de adjudicar sus plazas. Pero solo se ofertaban 8 plazas, y la última adjudicada ha sido la que correspondía al número de orden 3231, mientras que Pediatría lo ha sido con el 5081. Por lo tanto, el número en el que se finaliza la adjudicación de plazas debe relacionarse con el número total de las mismas.
Volviendo a la adjudicación de plazas de Pediatría a lo largo de los años, si se reevalúan estos datos, con la hipótesis de que no hubiera aumentado el número de plazas y que se hubiera mantenido en las 392 que había en 2019, como vemos en la Figura 2, en lugar de finalizar la adjudicación de plazas en la 5081 habría finalizado en la 3975.
| Figura 2. Adjudicación de la última plaza en el caso de que no hubiera aumentado la oferta de plazas en el periodo 2015-2023 |
|---|
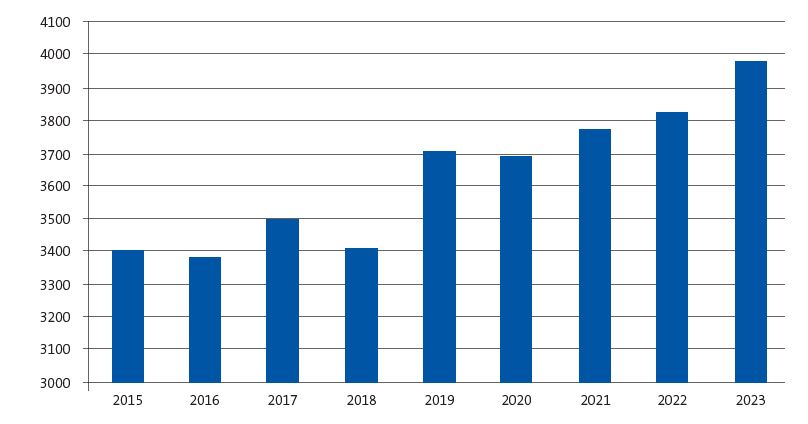 |

Se observa que el número se mantiene estable desde 2015 a 2018 y que hay un aumento a partir de 2019. Ese aumento se corresponde con un gran incremento de la oferta de plazas, un 11,1%, que ocurrió en 2019 cuando se pasó de 433 a 481 en la oferta de plazas de Pediatría.
¿Cuántos aspirantes a la especialización se quedan sin poder elegir plaza de Pediatría?
Si el número total de plazas MIR es 8550 y el número en el que se han agotado las plazas de Pediatría es 5081, quiere decir que 3469 aspirantes no pueden elegir Pediatría porque se ha acabado. No quiere decir que todos esos hubieran deseado realizar la especialidad de Pediatría, que no es así, pero no han tenido la opción. Y ¿este número ha disminuido o ha aumentado en los últimos años?
Siguiendo la evolución de las plazas MIR, vemos que hay un 28% más de residentes que no pueden optar a las plazas de Pediatría. En 2015 había 2703 residentes que si deseaban elegir una plaza de Pediatría no podían porque cuando ellos optaban ya se habían acabado y en 2023 ese número ha aumentado a 3469.
¿Cuáles son las salidas profesionales para los residentes de Pediatría?
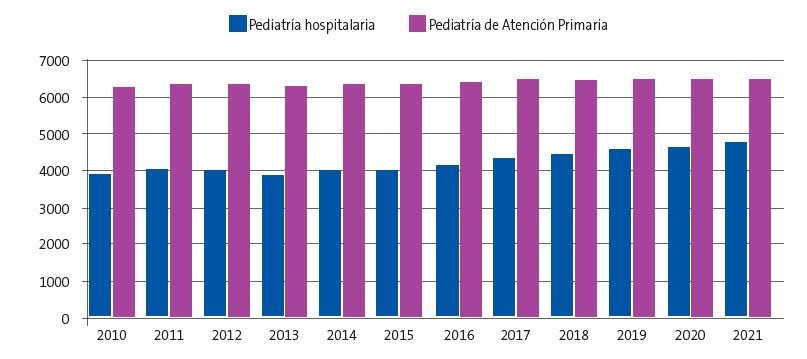
Los residentes que optan a la especialización de Pediatría son conscientes de que la salida laboral más posible para ellos es la Pediatría de AP. Según los datos del Ministerio del 2021, el número de pediatras en atención hospitalaria y en AP es de 47524 y 64745, respectivamente. Es decir, el 42% de las plazas son hospitalarias y el 58% de AP. Y eso que en los últimos 10 años ha aumentado en mayor proporción el número de plazas hospitalarias, ya que en 2010 había un 38% de plazas hospitalarias y un 62% de plazas de AP, como se puede ver en la Figura 3.
| Figura 3. Número de plazas de Pediatría hospitalaria y de Pediatría de Atención Primaria en el periodo 2010-2021 según el sistema de información del Ministerio de Sanidad |
|---|
 |

Otro aspecto a tener en cuenta, para analizar las futuras salidas profesionales, es la edad media de los profesionales de Pediatría de AP y Pediatría hospitalaria, que es muy diferente. Según el Informe Oferta-Necesidad de Especialistas Médicos 2021-20356, la estructura etaria difiere significativamente entre ambos, siendo más elevada en AP. Los pediatras en AP son mayores: un 52,8% tienen 50 años o más, mientras que ese porcentaje es casi la mitad, 27,6%, para los pediatras adscritos a la red de hospitales. Mientras que uno de cada 5 pediatras de la red de AP cumplirá la edad de jubilación en el próximo lustro, solo el 11% de los que trabajan en la red de hospitales están en esa edad de prejubilación (Figura 4).
| Figura 4. Porcentaje de mayores de 50 años y mayores de 60 años en función de la actividad de Pediatría de Atención Primaria u hospitalaria |
|---|
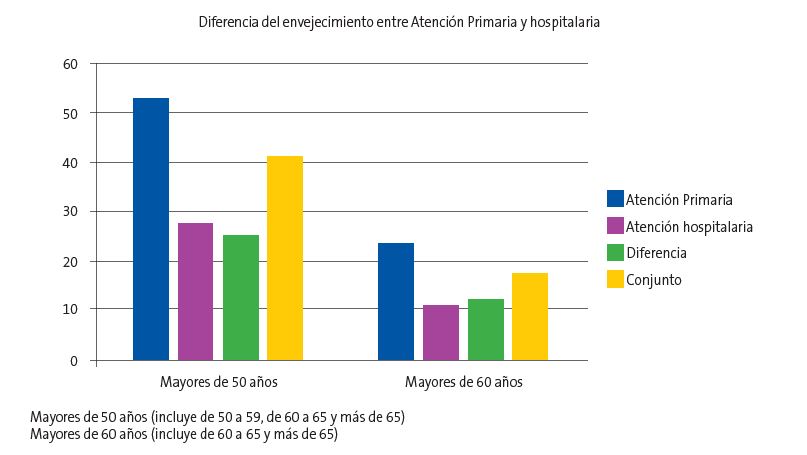 |

Si sumamos a los datos actuales de profesionales que hay en este momento, que se van a jubilar en los próximos quince años el 52,8% en AP y el 27,6% en hospital, se obtiene que hay necesidad de 9872 pediatras para PAP y 6063 para Pediatría hospitalaria. Eso quiere decir que las ofertas de trabajo en AP son el 62% y un 38% en Pediatría hospitalaria.
Otro dato del mismo informe es que la Pediatría, siendo la segunda especialidad que más plazas de formación oferta anualmente, es la que menos recirculación o abandono sufre durante la formación especializada. Casi la totalidad de los residentes que se inician en la Pediatría finalizan la especialidad, lo que indica que es satisfactoria para ellos.
DISCUSIÓN
Los argumentos que utilizan los residentes a la hora de elegir o no una especialidad están basados en la imagen que de la misma ofrecen los profesionales que la practican o de la que muestran otros residentes. Por lo tanto, analizaremos las opiniones realizadas por estos. Inicialmente, ofreceremos opiniones personales de residentes y posteriormente estudios que recogen opiniones colectivas de los mismos.
En cuanto a opiniones personales, tenemos la de la coordinadora del Grupo MIR de la Asociación Española de Pediatría (AEP) que como problema de la Atención Primaria refiere que las posibilidades de investigación son escasas. Decía: “Una vez conoces el funcionamiento y empiezas a trabajar, te enamoras de la labor principal de los pediatras, la prevención, el diagnóstico y tratamiento de la enfermedad en el niño y adolescente. En cuanto al día a día, varía según cada profesional, hay pediatras trabajando exclusivamente en el hospital, mientras que otros se centran en la AP, por lo que el trabajo de unos y otros es completamente diferente. Precisamente, en esta última área, tan sobrecargada y falta de recursos, la carga asistencial es tan grande que es muy difícil sacar tiempo a lo largo de la jornada laboral para poder dedicárselo a la investigación”7.
Una residente de primer año del Hospital Severo Ochoa de Leganés, a la pregunta: “¿Barajas la posibilidad de trabajar en un centro de salud?”, su respuesta fue: “A priori no me lo planteo. Por mi forma de ser me gusta más la actividad en el hospital; ahora que soy joven y tengo ganas, me apetece vivir el ritmo del hospital y sus guardias. Sin embargo, sí que pienso que el centro de salud me puede servir de escapatoria para un futuro. Quizás después de años trabajados, cuando tenga mi familia formada, quiera un ritmo de vida más «tranquilo» y eso me lo puede proporcionar el centro de salud, poder dejar de hacer guardias cuando el cuerpo me lo pida y dedicarme a la revisión del niño sano. También me gusta la investigación, que es una pieza clave del profesional médico. Estar actualizado, motivar y fomentar la investigación es fundamental para seguir avanzando en la medicina. De no ser por la investigación no tendríamos todos los avances que existen actualmente”8.
Vemos que, como la anterior residente, opina que tiene más vida el hospital y en él se puede investigar.
Una imagen muy diferente expresa un residente de Pediatría de cuarto año del Hospital Materno-Infantil de Málaga, que dice: “Mi entusiasmo por la AP es quizá porque supone una atención integral al paciente, al mismo tiempo que te hace partícipe de su crecimiento y desarrollo, ya que permite una continuidad tanto en el niño «sano» como en aquel que presenta alguna patología y es posible seguir el rumbo de los niños de tu cupo, conociendo sus características personales y familiares. Se genera más confianza en la relación médico-paciente y una mayor implicación de ambos. El pediatra del centro de salud suele ser el primer filtro ante cualquier enfermedad, lo que suscita en él un sentimiento de utilidad y responsabilidad. Es, por otro lado, un educador de padres, tratando de inculcarles hábitos y procedimientos que repercutan favorablemente en la salud de sus hijos. Se crea un cierto vínculo con familiares y cuidadores que favorece el aprendizaje mutuo. La AP es como una gran ensalada variada y muy rica, que cada día trae distintos ingredientes. Aunque los elementos de la base sean comunes, las posibilidades de innovación son numerosas. Los pediatras de AP deben sentirse orgullosos de la labor que realizan cada día, siendo conscientes del papel tan relevante que ocupan en nuestra sociedad y del enorme bien que hacen a millones de familias que les confían a su bien más preciado, sus hijos”9. Y continúa: “Durante mis primeros años en el hospital, la AP pasaba prácticamente desapercibida. Eso sí, me parecía extraño que la duración de la rotación por AP fuese tan corta en relación con la gran proporción de residentes de Pediatría que posteriormente acaban trabajando en un centro de salud. Desde fuera y para algunos (menos mal que no para la mayoría), esta sección parece monótona, aburrida e, incluso, hablan de ella con un cierto matiz despectivo. No obstante, esta visión está sesgada y manipulada. Hay que salir y ver la luz por uno mismo, no hacer caso a lo que nos dicen; abrir la mente y vislumbrar con nuestros propios ojos otro mundo distinto”. Vemos que este residente “entusiasmado por la AP” cita dos claves importantes, el escaso tiempo de rotación por Atención Primaria y el concepto despectivo que tiene la Atención Primaria en algunos ámbitos de la Pediatría.
En cuanto al segundo aspecto, la recogida de opiniones de grupos de residentes, vamos a mostrar dos ejemplos.
En 2009 se realizó una encuesta a 61 residentes asistentes al XIV Curso de Formación Continuada para Residentes de Cuarto Año de la Especialidad de Pediatría a Nivel Nacional10, con las limitaciones de ser una encuesta realizada a un grupo restringido, cuya representatividad del conjunto de los residentes no podemos establecer, sus respuestas fueron las siguientes: la mayoría (90%) de los residentes considera la figura del tutor de residentes como importante; sin embargo, la valoración de sus tutores de formación MIR osciló ampliamente entre 0 y 10, con una mediana de 6; el 35% de los tutores recibió una puntuación inferior a 5. Todos consideran positiva la rotación por AP, si bien en la mayoría de las respuestas (70%) el tiempo de rotación se limitaría a 2 o 3 meses. Por último, hay que mencionar que, al finalizar el MIR, 2 de cada 3 residentes ya tenían confirmado un puesto de trabajo, mayoritariamente en hospitales (80% de los que tenían confirmado el puesto de trabajo).
En la AEPap se ha realizado en 2017 una encuesta a la que respondieron 117 residentes, el 7% del total de residentes de España y, según esos resultados, un 98% opina que es necesaria la rotación por AP. Un 75% piensa que trabajarán en AP, un 43% lo desea y a un 55% no le importaría a pesar de no ser su primera opción. El 51% considera que el tiempo de rotación adecuado sería cuatro meses y tan solo un 11% considera adecuado rotar menos de tres meses11. En esta encuesta, realizada 8 años después de la del curso de residentes de la AEP, vemos cómo aumenta el tiempo que los residentes creen que es necesario rotar por AP y cómo aumenta la opción de la AP en sus valoraciones como futuro profesional.
Este aumento de las rotaciones de los residentes de Pediatría por AP ha sido recogido por el Marco Estratégico para la Atención Primaria12. Igualmente, desde la AEPap: “Proponemos que se flexibilice la duración de las rotaciones de los pediatras en formación para que puedan adquirir los conocimientos básicos necesarios para el pediatra generalista en áreas como Psiquiatría infantil, Dermatología y Ortopedia, entre otros”. Los pediatras de AP esperan que los próximos años se modifique el “hospitalocentrismo” en la formación de médicos residentes de una especialidad con gran necesidad de profesionales con consultas cerca de las familias, con consultas cerca de los recién nacidos, lactantes, niños, niñas y adolescentes. La AEPap, junto con el resto de las sociedades científicas pediátricas, está dispuesta a buscar soluciones conjuntas con las administraciones sanitarias con el fin de conseguir la mejora de la adecuación de la formación a las salidas laborales de los residentes en el sistema nacional de salud13.
CONCLUSIONES
A modo de conclusión se podría decir:
- La Pediatría sigue siendo una especialidad atractiva para los aspirantes al MIR.
- El hecho de que el número de adjudicación de la última plaza se retrase está, en parte, mediatizado por el aumento de oferta de plazas, ya que, quitando ese factor, el retraso en los últimos 9 años solo ha sido del 17%.
- Si se aumentara el número de las plazas de Pediatría ofertadas, podría haber más médicos que optaran por la especialidad de Pediatría.
- Los residentes que comienzan Pediatría tienen una de las tasas de abandono de la especialidad más baja, lo que indica que su formación les satisface.
- Está cambiando, positivamente, la valoración de los residentes de la Atención Primaria como salida profesional de la especialidad de Pediatría y, dado que las salidas son mayoritarias en Atención Primaria, habría que reforzar esa formación dentro del aprendizaje MIR.
- Desde las asociaciones pediátricas tenemos que dar mensajes más positivos de nuestra especialidad para que sea atractiva para los futuros residentes.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo. Este trabajo no ha contado con financiación.
RESPONSABILIDAD DE LOS AUTORES
Todos los autores han contribuido de forma equivalente en la elaboración del manuscrito publicado.
ABREVIATURAS
AEP: Asociación Española de Pediatría · AEPap: Asociación Española de Pediatría de Atención Primaria · AP: Atención Primaria · MIR: médico interno residente.
BIBLIOGRAFÍA
- Martín-Zurro A. Situación actual de la Atención Primaria y Comunitaria en España. ENE. 2022;16(3):2-3
- García Santos P. Los médicos con las mejores notas MIR ya no quieren ser pediatras: así se 'desinfla' la especialidad. En: El Español [en línea] [consultado el 10/06/2024]. Disponible en www.elespanol.com/ciencia/salud/20230425/medicos-mejores-mir-no-pediatras-desinfla-especialidad/758674299_0.html
- Centro de Estudios del Sindicato Médico de Granada. Distribución adjudicaciones de plazas MIR en 2023 (9 mayo 2023) [en línea] [consultado el 10/06/2024]. Disponible en https://simeg.org/wp/wp-content/uploads/2023/05/Informe-MIR-2023.pdf
- Portal Estadístico. Sistema de Información de Atención Especializada (SIAE) [en línea] [consultado el 10/06/2024]. Disponible en https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/C/siae/siae/hospitales/personal-y-formacion/areas-profesionales-y-especialidades
- Portal Estadístico. Sistema de Información de Atención Primaria (SIAP) [en línea] [consultado el 10/06/2024]. Disponible en https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/C/sistema-de-informacion-de-atencion-primaria-siap/profesionales/equipos-de-atencion-primaria-eap
- Necesidades de Médicos Especialistas [en línea] [consultado el 10/06/2024]. Disponible en www.sanidad.gob.es/areas/profesionesSanitarias/profesiones/necesidadEspecialistas/docs/2022Estudio_Oferta_Necesidad_Especialistas_Medicos_2021_2035V3.pdf
- Uhrig A. Pediatría, una especialidad “preciosa” en la que los pacientes sacan una carcajada cada día. En: ConSalud.es; 2022 [en línea] [consultado el 10/06/2024]. Disponible en www.consalud.es/especial-mir/pediatria-especialidad-preciosa-pacientes-sacan-carcajada_113168_102.html
- Maldonado G. Los primeros días de una R1 en el hospital: “Quiero aprender, crecer y convertirme en la figura del médico que idealizo”. En: iSanidad.com; 2023 [en línea] [consultado el 10/06/2024]. Disponible en https://isanidad.com/250505/los-primeros-dias-de-una-r1-en-el-hospital-quiero-aprender-crecer-convertirme-figura-medico-idealizo/
- López García R. El residente de Pediatría: entusiasmo por la Atención Primaria. Rev Pediatr Aten Primaria. Supl. 2012;(21):71-6.
- González de Dios J, Polanco Allue I, Díaz Vázquez CA. De las facultades de Medicina a la residencia de Pediatría, pasando por el examen de médico interno residente: ¿algo debe cambiar? Resultados de una encuesta en residentes de Pediatría de cuarto año. An Pediatr (Barc). 2009;70(5):467-76. https://doi.org/10.1016/j.anpedi.2009.02.009
- Goez Sanz C, Álvarez Casaño M, Castillo Campos l, Gorrotxategi Gorrotxategi PJ, Villaizán Pérez C. ¿Qué opinan los residentes de Pediatría de la rotación por Atención Primaria? Rev Pediatr Aten Primaria. 2021;23:e181-e184.
- Marco Estratégico para la Atención Primaria y Comunitaria. Ministerio de Sanidad, Consumo y Bienestar Social. Madrid. 2019 [en línea] [consultado el 10/06/2024]. Disponible en www.sanidad.gob.es/areas/calidadAsistencial/estrategias/atencionPrimaria/docs/Marco_Estrategico_APS_25Abril_2019.pdf
- MIR 2022: los pediatras de Atención Primaria proponen más formación en los centros de salud para aumentar la capacidad docente y sortear el déficit de profesionales [en línea] [consultado el 10/06/2024]. Disponible en www.aepap.org/sites/default/files/noticia/archivos-adjuntos/np_mir_pediatria_ap.pdf





