Vol. 26 - Num. 102
Originales
Niveles de vitamina D en un área de baja radiación solar del norte de la península ibérica
Ferran Campillo i Lópeza, Laia Ferré Moraguesa, Diego Alberto Rincón Díaza, Emiliano Heras Martína, María Marlene Rojas de Millsa, Ernesto Segarra Garcíaa, Anton Foguet i Vidal a
aEquipo pediátrico territorial de la Garrotxa. Fundación Hospital de Olot y Comarcal de la Garrotxa. Olot. Gerona. España.
Correspondencia: F Campillo i López. Correo electrónico: fcampillo@hospiolot.cat
Cómo citar este artículo: Campillo i López F, Ferré Moragues L, Rincón Díaz DA, Heras Martín E, Rojas de Mills MM, Segarra García E, et al. Niveles de vitamina D en un área de baja radiación solar del norte de la península ibérica . Rev Pediatr Aten Primaria. 2024;26:137-45. https://doi.org/10.60147/2e098110
Publicado en Internet: 20-05-2024 - Número de visitas: 14772
Resumen
Introducción: el déficit de vitamina D es motivo de preocupación a nivel europeo, especialmente en latitudes más al norte del paralelo 40, y son varios los factores clínicos implicados. La mayor parte de los estudios de prevalencia en población pediátrica en España se han realizado para latitudes con alta exposición solar.
Materiales y métodos: estudio descriptivo transversal en dos periodos estacionales diferenciados (verano e invierno) en niños sanos de 2 a 14 años entre el 15 de julio de 2013 y el 15 abril de 2016, mediante recogida de datos y analítica sanguínea (calcidiol, calcio, fósforo) en un total de 603 niños residentes en la Garrotxa (Gerona) (latitud 42° N), una zona en Cataluña con baja radiación solar. Se calcularon prevalencias y una regresión multivariable para determinar la influencia de distintas variables clínicas.
Resultados: un 31,86% de los niños presentaban niveles de vitamina D inferiores a 20 ng/ml, aumentando al 52,87% en invierno. El grupo étnico, el fototipo o la estación del año justificaron el 53,2% de su variabilidad.
Conclusiones: los niños en áreas de baja radiación solar presentan una alta prevalencia de hipovitaminosis D, especialmente en invierno, en fototipo de pieles oscuras y en algunos grupos étnicos.
Palabras clave
● Etnicidad ● Hipovitaminosis D ● Pigmentación de la piel ● Radiación solar ● Vitamina DINTRODUCCIÓN
El déficit de vitamina D se ha convertido en un motivo de preocupación en los últimos años. Aunque existen distintos criterios según países y sociedades científicas, se ha establecido un consenso global para determinar que valores superiores a 20 ng/ml (50 nmol/l) indicarían un estado de suficiencia, entre 12-20 ng/ml se considera insuficiencia, y menos de 12 ng/ml, déficit1. En Europa el 40,4% de la población presentaría niveles séricos de vitamina D insuficientes, con mayores tasas durante el invierno2. Además del raquitismo y problemas de salud musculoesqueléticos relacionados con el metabolismo fosfocálcico, el déficit de vitamina D se ha asociado a varias enfermedades cardiovasculares, trastornos autoinmunes, enfermedades infecciosas y trastornos neurológicos3. La exposición solar limitada, especialmente en las regiones con latitudes más extremas (más de 40° N o S), el fototipo (a más melanina menos absorción de vitamina) o aspectos culturales pueden contribuir a niveles bajos de vitamina D4.
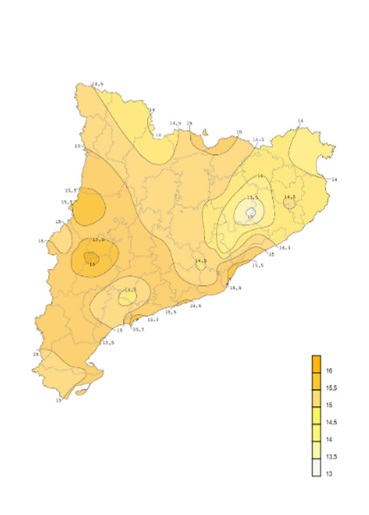
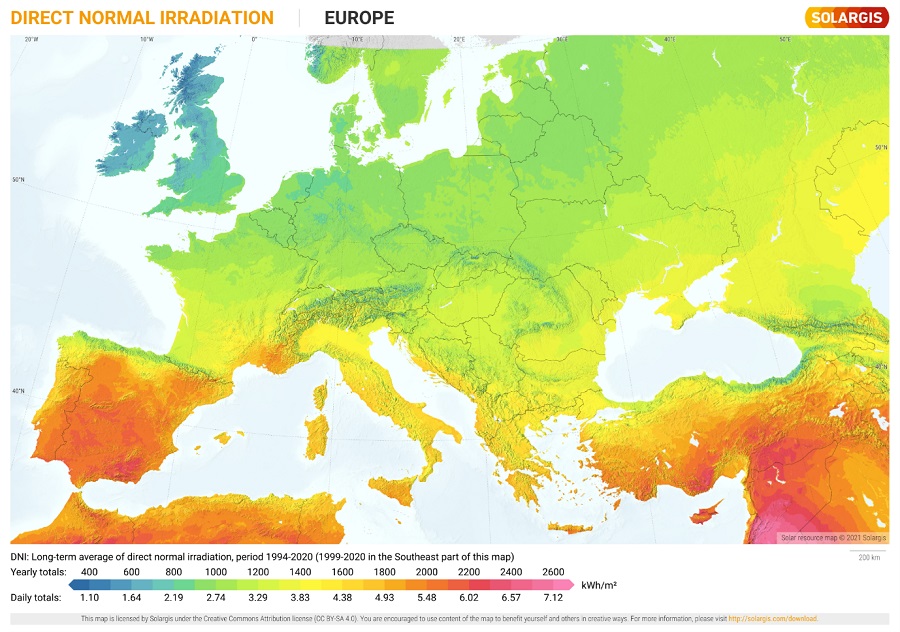
Cataluña está ubicada por encima del paralelo 40 N, y las comarcas más septentrionales se sitúan a 42° N. Los Prepirineos y Pirineos catalanes, junto con la mayor parte de las comarcas gerundenses y las zonas montañosas del Camp de Tarragona y las Terres de l'Ebre, son los territorios catalanes con menos radiación solar (Figura 1)5, similar a regiones españolas como Navarra, La Rioja o algunas provincias de Aragón, Castilla y León o Galicia, y otras áreas europeas, como el norte de Portugal, el sur de Francia, la zona central de Italia, Grecia o los países de los Balcanes (Figura 2).
| Figura 1. Mapa de radiación global diaria de Cataluña, media anual (MJ/m2) |
|---|
 |

| Figura 2. Mapa de radiación normal directa de Europa, media anual (kWh/m2) |
|---|
 |

La mayor parte de los estudios sobre prevalencia de hipovitaminosis D en nuestro entorno se han realizado en latitudes más meridionales con mayor radiación solar6. El objetivo de nuestro estudio es evaluar el estado de la vitamina D en una población pediátrica con una menor exposición solar y sus posibles predictores clínicos.
MATERIAL Y MÉTODOS
Se realizó un estudio descriptivo transversal en dos periodos estacionales diferenciados (verano e invierno) en niños sanos entre el 15 de julio de 2013 y el 15 abril de 2016. El área de muestreo fue la comarca de la Garrotxa, situada en una latitud 40° N en el Prepirineo gerundense. Participaron las cuatro Áreas Básicas de Salud de la comarca y el hospital comarcal de un equipo territorial de Pediatría, donde se analizaban las muestras de sangre con un método de inmunoanálisis quimioluminiscente de micropartículas para la determinación cuantitativa de 25-hidroxi vitamina D en suero y plasma humanos.
Los criterios de inclusión fueron niños y niñas sanos de la Garrotxa, de entre 2 a 14 años que no cumplieran ningún criterio de exclusión de los siguientes: asma moderada o grave (se aceptaba la episódica ocasional), insuficiencia renal o hepática, trastornos del aparato digestivo que causen malabsorción, fibrosis quística, enfermedades endocrinas y metabólicas, enfermedades cutáneas que requieran uso prolongado de corticoides, inmunosupresión (por enfermedad o por tratamiento), pacientes que sigan dieta vegana, pacientes en tratamiento con vitamina D3 y pacientes con obesidad (índice de masa corporal [IMC] >p97).
Previo consentimiento informado, se registraron de forma anónima la edad, el sexo, el fototipo (según escala de Fitzpatrick), el peso, la talla y el IMC. Mediante análisis bioquímico se obtuvieron las variables del calcio, fósforo y el calcidiol o 25-hidroxi vitamina D, que fue la variable principal a estudiar.
Los datos descriptivos se expresaron en número y porcentaje para las variables categóricas y como mínimo, máximo, promedio y desviación estándar para las variables cuantitativas. La normalidad de las variables cuantitativas se comprobó mediante el test de Shapiro-Wilk. Para comparar las variables cuantitativas entre los diferentes grupos del estudio se utilizaron el test ANOVA o el test no paramétrico de Kruskal-Wallis, dependiendo de si se cumplían los criterios de normalidad. Para comparar las variables categóricas, el test de la ji-cuadrado de Pearson o el test exacto de Fischer de forma apropiada. Se calcularon los coeficientes de correlación entre vitamina D y otras variables. Para evaluar el peso de las variables clínicas sobre la variabilidad de la vitamina D se realizó una regresión múltiple, adecuando las variables categóricas con el método de codificación one-hot en el que se crea una nueva variable binaria por cada categoría. El nivel de significación estadística se fijó en valores p <0,05.
Las variables se introdujeron en una base de datos Microsoft Access® y se exportaron al software de acceso abierto PSPP versión 1.2.0-g0fb4db para su análisis estadístico. Paralelamente, se utilizó Julius.ai, una herramienta de inteligencia artificial basada en el modelo GPT-3 de OpenAI para la preparación de los datos, análisis estadístico y tareas de interpretación.
El estudio fue evaluado y aprobado por el Comité Ético de Investigación Clínica del Hospital Universitario de Girona Josep Trueta (AC 89-13).
RESULTADOS
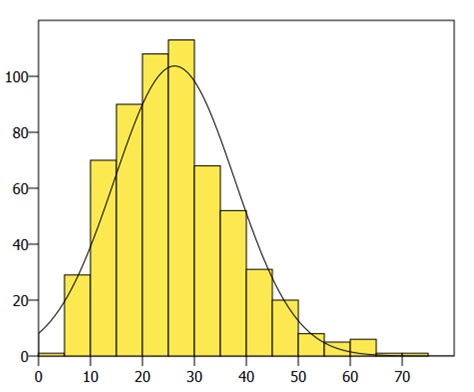
Se reclutaron a un total de 603 niños con las características que se pueden consultar en las Tablas 1 y 2. La concentración de los niveles de vitamina D presentó una distribución normal (Figura 3). Un 68,33% mostraba valores superiores a 20 ng/ml (suficiencia), un 22,38% entre 12 y 20 ng/ml (insuficiencia) y un 9,29% inferiores a 12 ng/ml (deficiencia). En los dos periodos de estudio no hubo diferencias estadísticamente significativas en las características de las muestras, excepto los valores medios de vitamina D entre verano (29,40 ng/ml) e invierno (19,05 ng/ml). En verano la prevalencia de suficiencia, insuficiencia y deficiencia fue de 82,73%, 15,59% y 1,67%, respectivamente, mientras que en invierno fue de 47,13%, 31,97% y 20,90%. Los niveles medios variaron según el fototipo de piel (Tabla 3), con una diferencia estadísticamente significativa (valor p 0,008) entre los niños de pieles claras (fototipo 1-3) (30,24 ng/ml) y los de pieles oscuras (fototipo 4-6) (19,74 ng/ml), y también con diferencias según el grupo étnico (Tabla 4). Los coeficientes de correlación entre las diferentes variables y los niveles de vitamina D pueden consultarse en la Tabla 5. La regresión multivariable con las variables clínicas (edad, sexo, peso, talla, IMC, grupo étnico, fototipo, estación) resultó en un coeficiente de determinación (R2) de 0,532, que implicaría que el 53,2% de la variabilidad de los parámetros de vitamina D podría deberse a estas variables clínicas. De todas ellas, solo el fototipo, el grupo étnico y la estación del año fueron predictores estadísticamente significativos. El coeficiente de correlación entre el fototipo y el grupo étnico fue alto, de 0,876225, por lo que, y para descartar un fenómeno de multicolinealidad, se crearon dos modelos en los que se incluía solo una de las dos variables. El modelo basado en el grupo étnico presentaba un R2 de 0,529, mientras que el modelo del fototipo el R2 fue de 0,448.
| Tabla 1. Análisis de frecuencias de la muestra | |||
|---|---|---|---|
| n | % | ||
| Sexo | Femenino | 281 | 46,6 |
| Masculino | 322 | 53,4 | |
| Estacionalidad | Verano | 359 | 59,5 |
| Invierno | 244 | 40,5 | |
| Etnia | Blanco/caucásico | 306 | 50,7 |
| Blanco/sudamericano | 42 | 7,0 | |
| Árabe | 63 | 10,4 | |
| Asiático/indio | 73 | 12,1 | |
| Sudeste asiático/China | 14 | 2,3 | |
| Gitana | 2 | 0,3 | |
| Negro/africano | 103 | 17,1 | |
| Fototipo | 1 | 13 | 2,2 |
| 2 | 130 | 21,6 | |
| 3 | 228 | 37,8 | |
| 4 | 98 | 16,3 | |
| 5 | 33 | 5,5 | |
| 6 | 101 | 16,7 | |

| Tabla 2. Análisis descriptivo de rangos y medias | ||||
|---|---|---|---|---|
| Mínimo | Máximo | Media | Desviación estándar | |
| Edad (años) | 2 | 14 | 7,95 | 3,48 |
| Pesos (kg) | 9,1 | 80 | 28,74 | 13,21 |
| Talla (cm) | 82 | 182 | 126,85 | 22,41 |
| Índice de masa corporal | 12,08 | 28 | 16,78 | 2,54 |
| Calcio (mg/dL) | 8,4 | 12,3 | 9,76 | 0,38 |
| Fósforo (mg/dL) | 3,1 | 7,0 | 5,04 | 0,55 |
| Vitamina D (ng/ml) | 3,5 | 70,8 | 26,19 | 11,59 |

| Tabla 3. Niveles de vitamina D según fototipo | |||
|---|---|---|---|
| Fototipo | Media (ng/mL) | n | Desviación estándar |
| 1 | 30,43 | 13 | 10,99 |
| 2 | 30,54 | 130 | 10,51 |
| 3 | 30,06 | 228 | 11,20 |
| 4 | 22,96 | 98 | 11,68 |
| 5 | 20,25 | 33 | 5,84 |
| 6 | 16,44 | 101 | 6,75 |

| Tabla 4. Niveles de vitamina D según grupo étnico | |||
|---|---|---|---|
| Grupo étnico | Media (ng/mL) | n | Desviación estándar |
| Blanco/caucásico | 32,68 | 306 | 10,93 |
| Blanco/sudamericano | 26,01 | 42 | 6,65 |
| Árabe | 20,45 | 63 | 6,83 |
| Asiático/indio | 17,98 | 73 | 8,40 |
| Sudeste asiático/China | 25,20 | 14 | 6,90 |
| Gitana | 25,40 | 2 | 0,42 |
| Negro/africano | 16,50 | 103 | 6,64 |

| Tabla 5. Coeficientes de correlación con la vitamina D | ||
|---|---|---|
| Correlación | Valor p | |
| Edad | 0,105402 | 0,00989987* |
| Grupo étnico | -0,545708 | <0,0001* |
| Fototipo | -0,37943 | <0,0001* |
| Peso | 0,0652751 | 0,110802 |
| Talla | 0,085449 | 0,0367056* |
| Índice de masa corporal | 0,00530901 | 0,896918 |
| Calcio | 0,131348 | 0,00128538* |
| Fósforo | -0,103725 | 0,0111477* |
|
*Valor p <0,05 |
||

DISCUSIÓN
De forma global, el 31,86% de los niños y adolescentes previamente sanos de la Garrotxa mostró niveles insuficientes de vitamina D (<20 ng/ml). En un estudio multicéntrico español que incluía a niños de 8 a 13 años de diferentes latitudes (A Coruña, Barcelona, Madrid, Sevilla y Valencia) la prevalencia global fue del 35%7.
La estación del año modifica significativamente la prevalencia de hipovitaminosis, aumentando en invierno, con un 52,87% de la muestra con niveles inferiores a 20 ng/ml, y disminuyendo en verano, afectando solo al 17,27%. En Navarra (42° N), con un tamaño muestral y latitudes similares, se observó también que la hipovitaminosis afectaba al 62,6% en invierno y al 20,0% en verano8; en Asturias (42-43° N), algo más al norte, al 71,8% y al 34,5%9, respectivamente. En cambio, en estudios con latitudes más en el sur (y con muestras más pequeñas) mostraron prevalencias más bajas: en Madrid (40° N), el 51% presentaba valores inferiores 20 ng/ml en invierno10; en Zaragoza (41° N), el 29,2%, y en verano un 25%11; en Cádiz (36° N) en invierno la prevalencia de hipovitaminosis era del 45,2%12, y en Córdoba (37° N) en invierno no se detectó13. Esta relación entre hipovitaminosis D y la estación del año, pero también la latitud, se ha observado en cohortes europeas, con una menor prevalencia en la cuenca mediterránea14-16.
Existe una correlación positiva de la concentración de vitamina D con la edad. Esto coincide con estudios realizados en áreas con mayor exposición solar: recién nacidos sanos de Mallorca (60,8% con niveles insuficientes)17, prematuros de Tarragona (50,0% con niveles insuficientes)18, lactantes sanos de 1 a 6 meses (8,4% con niveles inferiores a 10 ng/ml)19 o menores de 2 años ingresados (24,3% con niveles insuficientes)20 de Valencia. También parece existir una correlación entre los niveles maternos de vitamina D y en sangre de cordón21.
Por lo que respecta al IMC, debemos considerar que la muestra del estudio excluía la obesidad. Esto podría haber limitado la capacidad de detectar esa relación negativa que otros estudios han observado12.
En la Garrotxa ha habido un aumento de población de origen extranjero en los últimos años (3,48% en 2000 frente al 13,38% en 2016), un fenómeno que se ha observado con cifras similares al resto de Cataluña (13,60%)22. En un estudio de Salt (Gerona), con un porcentaje de niños de familias migradas más alto que la media catalana (72% no caucásicos)23 observaron diferencias estadísticamente significativas de los niveles de vitamina D según el grupo étnico.
El modelo matemático basado en datos clínicos pudo predecir el 53,2% de la variabilidad de los niveles de vitamina D, donde el fototipo de piel, el grupo étnico y la estación del año fueron los predictores más importantes. A pesar del solapamiento esperable entre grupo étnico y fototipo, cada variable cubre aspectos distintos. De hecho, el grupo étnico aporta más datos a la variabilidad. Este fenómeno puede explicarse por factores culturales o religiosos, como el tiempo dentro de espacios cerrados, ropa que cubra mayor superficie corporal20 o hábitos alimenticios.
Sin embargo, la variabilidad restante podría deberse a otros factores que no se han incorporado al modelo. En estudios de metanálisis se ha observado que las personas expuestas al humo del tabaco presentan niveles de vitamina D sensiblemente inferiores a los no expuestos24. Se estima que alrededor del 80-90% de la fuente de vitamina D es la exposición solar, pero el resto podría deberse a factores dietéticos, principalmente el pescado, las setas y, en menor medida, algunos lácteos enriquecidos25. El porcentaje de tiempo que los niños pasan al aire libre es primordial también para alcanzar estas horas de exposición solar15. Los niños y adolescentes que viven en barrios con más zonas verdes presentan niveles más altos de vitamina D26. El cambio climático también es un motivo de preocupación para los efectos indeseables de una exposición solar más intensa, a la vez que puede inducir comportamientos de pasar más tiempo en espacios cerrados o el uso de protectores solares27.
La necesidad o no de suplementar con vitamina D exógena fuera del periodo de lactancia sigue siendo un motivo de debate28. El haber recibido suplementación durante el primer año de vida parece contribuir a unos niveles óptimos posteriormente11. Tener identificadas variables clínicas como predictores de un posible déficit de vitamina D pueden ser útiles para establecer estrategias para tratar su déficit. Actividades al aire libre y en contacto con la naturaleza, con una mirada ambiental y sociocultural, con especial atención en invierno, que trabajen también para eliminar el humo ambiental del tabaco en el hogar, podrían convertirse en primordiales a la hora de abordar el tratamiento y la prevención de la hipovitaminosis D en estas latitudes.
CONCLUSIONES
La prevalencia de hipovitaminosis D en esta área con menor radiación solar fue mayor que en los estudios realizados en latitudes más meridionales de la península ibérica. La etnia, el fototipo y la estación del año son variables clínicas relevantes para establecer estrategias que mejoren los niveles de vitamina D.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo. El presente trabajo no ha recibido ningún tipo de financiación.
RESPONSABILIDAD DE LOS AUTORES
Contribución de los autores: búsqueda bibliográfica, análisis de datos, redacción y revisión final (FLC), búsqueda bibliográfica, redacción y revisión final (LFM), concepción y diseño del estudio, recogida de datos, revisión final (DARD), recogida de datos y revisión final (EHM, MMRM y ESG), concepción y diseño del estudio, revisión final (AFV).
ABREVIATURAS
· IMC: índice de masa corporal · N: norte · S: sur.
BIBLIOGRAFÍA
- Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, et al. Global Consensus Recommendations on Prevention and Management of Nutritional Rickets. J Clin Endocrinol Metab. 2016;101:394-415. https://doi.org/10.1210/jc.2015-2175
- Cashman KD, Dowling KG, Škrabáková Z, González Gross M, Valtueña J, Henauw SD, et al. Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr. 2016;103:1033-44. https://doi.org/10.3945/ajcn.115.120873
- Holick MF. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017;18:153-65. https://doi.org/10.1007/s11154-017-9424-1
- Misra M, Pacaud D, Petryk A, Ferrez Collett-Solberg P, Kappy M. Deficiencia de vitamina D en los niños y su tratamiento: revisión del conocimiento y las recomendaciones actuales. Pediatrics. 2008;66:86-106. https://doi.org/10.1542/peds.2007-1894
- Sancho Ávila JM, Riesco Martín J, Jiménez Alonso C, Sánchez de Cos Escuin MC, Montero Cadalso J, López Bartolomé M. Atlas de Radiación Solar en España utilizando datos del SAF de Clima de EUMETSAT. 2012 [en línea] [consultado el 09/05/2024]. Disponible en https://www.aemet.es/documentos/es/serviciosclimaticos/datosclimatologicos/atlas_radiacion_solar/atlas_de_radiacion_24042012.pdf
- Domenech Vallejo A. Situación de los niveles de vitamina D en la edad pediátrica y adolescencia en España. Universitat de les Illes Balears; 2022 [en línea] [consultado el 09/05/2024]. Disponible en https://dspace.uib.es/xmlui/handle/11201/160112
- De Piero Belmonte A, Rodríguez Rodríguez E, González Rodríguez LG, Ortega Anta RM, López Sobaler AM. Vitamina D sérica y factores de riesgo metabólico en un grupo de escolares españoles. Nutr Hosp. 2015;31:1154-62. https://dx.doi.org/10.3305/nh.2015.31.3.8447
- Durá Travé T, Gallinas Victoriano F, Chueca Guindulain MJ, Berrade Zubiri S, Moreno Gónzalez P, Malumbres Chacón M. Prevalencia de hipovitaminosis D y factores asociados en la edad infantojuvenil. Aten Primaria. 2018;50:422-9. https://doi.org/10.1016/j.aprim.2017.06.003
- Rodríguez Dehli AC, Riaño Galán I, Fernández Somoano A, Navarrete Muñoz EM, Espada M, Vioque J, et al. Hipovitaminosis D y factores asociados a los 4 años en el norte de España. An Pediatr (Barc). 2017;86:188-96. https://doi.org/10.1016/j.anpedi.2016.02.003
- Rodríguez Rodríguez E, Aparicio A, López-Sobaler AM, Ortega RM. Vitamin D status in a group of Spanish schoolchildren. Minerva Pediatr. 2011;63:11-8.
- Martínez Redondo I, García Romero R, Calmarza P, De Arriba Muñoz A, Rodríguez Martínez G, Labarta Aizpún JI, et al. Deficiencia de vitamina D en niños aragoneses sanos. Nutr Hosp. 2018;35:782-8.
- Ruiz Ocaña P, Carrasco Fernández C, Zopeque García N, Sáez Benito A, Novalbos Ruiz JP, Lechuga Sancho AM. Niveles de vitamina D al final de la estación invernal en una población escolar sana. Rev Esp Endocrinol Pediátrica. 2014;5:19-27.
- Ramírez Prada D, De la Torre MJ, Llorente Cantarero FJ, Pérez-Navero JL, Gil Campos M. Evaluación de la exposición solar, ingesta y actividad física en relación con el estado sérico de vitamina D en niñas prepúberes españolas. Nutr Hosp. 2012;27:1993-8. https://dx.doi.org/10.3305/nh.2012.27.6.6065
- Valtueña J, González Gross M, Huybrechts I, Breidenassel C, Ferrari M, Mouratidou T, et al. Factors Associated with Vitamin D Deficiency in European Adolescents: The HELENA Study. J Nutr Sci Vitaminol (Tokyo). 2013;59:161-71. https://doi.org/10.3177/jnsv.59.161
- Sochorová l, Hanzlíková l, Černá M, Vosátková M, Grafnetterová AP, Fialová A, et al. Assessment of vitamin D status in Czech children. Cent Eur J Public Health. 2018;26:260-4. https://doi.org/10.21101/cejph.a5386
- Grossman Z, Hadjipanayis A, Stiris T, Del Torso S, Mercier JC, Valiulis A, et al. Vitamin D in European children—statement from the European Academy of Paediatrics (EAP). Eur J Pediatr. 2017;176:829-31. https://doi.org/10.1007/s00431-017-2903-2
- De Sotto Esteban D, Ursina Bëinbrech B, Ferrés Ramis l, Torbado Oliver P, Yánez Juan AM. Niveles de vitamina D y factores de riesgo asociados en recién nacidos sanos de Mallorca. Rev Esp Endocrinol Pediátrica. 2015;6:51-9.
- Ariño J, García A, Parada Ricart E, Albújar M. Relació entre les aportacions enterals de vitamina D i els nivells plasmàtics en nadons prematurs. Pediatr Catalana. 2019;79:127-32.
- Cabezuelo Huerta G, Vidal Micó S, Abeledo Gómez A, Frontera Izquierdo P. Niveles de 25-hidroxivitamina D en lactantes. Relación con la lactancia materna. An Pediatr (Barc). 2007;66:491-5. https://doi.org/10.1157/13102514
- Togo A, Espadas Maciá D, Blanes Segura S, Sivó Díaz N, Villalba Martínez C. ¿Existe déficit de vitamina D en los niños de una ciudad soleada del Mediterráneo? An Pediatr (Barc). 2016;84:163-9. https://doi.org/10.1016/j.anpedi.2015.05.003
- Blarduni E, Arrospide A, Galar M, Castaño l, Mar J. Factores asociados a la prevalencia de hipovitaminosis D en mujeres embarazadas y sus recién nacidos. An Pediatr (Barc). 2019;91:96-104. https://doi.org/10.1016/j.anpedi.2018.11.012
- Població estrangera a 1 de gener. Per comarques i Aran. Catalunya. En: Idescat [en línea] [consultado el 09/05/2024]. Disponible en www.idescat.cat/poblacioestrangera/?geo=cat&nac=a&b=4
- Sánchez Muro JM, Yeste Fernández D, Marín Muñoz A, Fernández Cancio M, Audí Parera l, Carrascosa Lezcano A. Niveles plasmáticos de vitamina D en población autóctona y en poblaciones inmigrantes de diferentes etnias menores de 6 años de edad. An Pediatr (Barc). 2015;82:316-24. https://doi.org/10.1016/j.anpedi.2014.05.007
- Yang l, Zhao H, Liu K, Wang Y, Liu Q, Sun T, et al. Smoking behavior and circulating vitamin D levels in adults: A meta-analysis. Food Sci Nutr. 2021;9:5820-32. https://doi.org/10.1002/fsn3.2488
- Masvidal Aliberch RM, Ortigosa Gómez S, Baraza Mendoza MC, Garcia Algar O. Vitamina D: fisiopatología y aplicabilidad clínica en pediatría. An Pediatr (Barc). 2012;77:279.e1-279.e10. https://doi.org/10.1016/j.anpedi.2012.05.019
- Thiering E, Markevych I, Kress S, Astell-Burt T, Feng X, Altug H, et al. Gene-environment interaction in the association of residential greenness and 25(OH) vitamin D. Environ Pollut Barking Essex 1987. 2023;327:121519. https://doi.org/10.1016/j.envpol.2023.121519
- Norval M, Lucas RM, Cullen AP, De Gruijl FR, Longstreth J, Takizawa Y, et al. The human health effects of ozone depletion and interactions with climate change. Photochem Photobiol Sci 2011;10:199-225. https://doi.org/10.1039/c0pp90044c
- Pallás Alonso CR. ¿Hay que hacer profilaxis con vitamina D? Rev Pediatría Aten Primaria. 2014;16:75-81. https://doi.org/10.4321/S1139-76322014000200011
- Baldasano JM, Soriano C, Flores H, Esteve J. Atlas de radiació solar a Catalunya. Universitat Politècnica de Catalunya (UPC) i Institut Català d’Energia (ICAEN); 2000. Report No.: 12. [en línea] [consultado el 09/05/2024]. Disponible en https://icaen.gencat.cat/ca/detalls/publicacio/Atlas-de-radiacio-solar-a-Catalunya-00003
- Solar resource maps of Europe. En: Solargis [en línea] [consultado el 09/05/2024]. Disponible en https://solargis.com/maps-and-gis-data/download/europe