Vol. 24 - Num. 95
Originales
Conocimiento y opinión sobre la atención integrada del niño con parálisis cerebral desde Atención Primaria
Lidia Aguilera Nietoa, M.ª José Peláez Canterob, Daniel Hinojosa Nogueirac, Josep Vicent Balaguer Martínezd
aPediatra. CS Palma-Palmilla. Málaga. España.
bPediatra. Unidad de Crónicos Complejos y Cuidados Paliativos Pediátricos. Hospital Regional Universitario de Málaga. Málaga. España.
cDepartamento de Nutrición y Bromatología. Instituto de Nutrición y Tecnología de los Alimentos. Centro de Investigación Biomédica. Universidad de Granada. Granada. España.
dPediatra. CAP Sant Ildefons. Cornellà de Llobregat. Barcelona. España.
Correspondencia: L Aguilera . Correo electrónico: lidia.agnil@hotmail.com
Cómo citar este artículo: Aguilera Nieto L, Peláez Cantero MJ, Hinojosa Nogueira D, Balaguer Martínez JV. Conocimiento y opinión sobre la atención integrada del niño con parálisis cerebral desde Atención Primaria . Rev Pediatr Aten Primaria. 2022;24:261-71.
Publicado en Internet: 11-10-2022 - Número de visitas: 9760
Resumen
Introducción: los pacientes con parálisis cerebral infantil (PCI) precisan de múltiples cuidados y terapias. El objetivo principal del estudio es describir la opinión, percepción y conocimiento sobre el abordaje integral del niño con PCI de pediatras de Atención Primaria (AP), así como su manejo actual sobre el mismo.
Material y métodos: estudio transversal, descriptivo y de ámbito nacional, mediante encuesta en línea, a pediatras y médicos de familia dedicados a la pediatría que ejercían en AP entre enero y febrero de 2021.
Resultados: se recibieron 335 respuestas. El 91% piensa que no dispone de formación suficiente y que su conocimiento es limitado, reconociendo el 65% que no está capacitado para el manejo del niño con PCI. Un 97,3% opina que es necesaria la formación en esta patología y el 99% que es necesaria la creación de protocolos específicos. Al 57,2% le gustaría ser pediatra coordinador trabajando con el pediatra hospitalario. El 75% estima que los cuidadores no están satisfechos con la atención que reciben, considerando que la atención integral al niño con PCI desde AP o disponer de unidades específicas para ello mejoraría la satisfacción familiar, resultando estadísticamente significativo.
Conclusiones: la mayoría de los pediatras no se sienten capacitados para llevar a cabo el manejo del niño con PCI desde AP y consideran necesario la formación y creación de guías específicas. Opinan que la atención integral del paciente con PCI mejoraría la calidad de vida de las familias, abogando para ello por modelos mixtos de coordinación.
Palabras clave
● Atención Primaria de Salud ● Parálisis cerebralINTRODUCCIÓN
La parálisis cerebral infantil (PCI) es la causa más frecuente de discapacidad infantil. Presenta una prevalencia general de 2,11 por cada 1000 recién nacidos vivos1, siendo mayor en recién nacidos <1500 g (59,2/1000 recién nacidos vivos) y prematuros menores de 28 semanas (111,8/1000 recién nacidos vivos)1,2. Entre las causas de PCI, existen múltiples motivos que provocan lesiones a nivel cerebral (consumo de tóxicos durante el embarazo, infección congénita, hipoxia…) aunque se desconoce en el 80% de las ocasiones3.
Esta patología engloba un grupo de trastorno del movimiento y de la postura permanente, pero no invariable, que provocan limitación de la actividad, causadas por lesiones no progresivas que ocurrieron en el sistema nervioso en desarrollo del feto o del lactante4. Estas alteraciones se acompañan con frecuencia de otras comorbilidades, como dolor crónico musculoesquelético, trastornos del sueño, epilepsia, problemas sensitivos (visual, auditivo), alteración del comportamiento, entre otros, que condicionan de manera importante la calidad de vida y el pronóstico de estos niños5-7. Esto la convierte en una entidad muy heterogénea que requiere un enfoque multidisciplinar.
En las últimas décadas, la figura de los padres como principales cuidadores cada vez es tenida más en cuenta en el manejo del paciente con PCI. Sin embargo, estos se siguen mostrando insatisfechos en el cuidado que sus hijos reciben8. Al tratarse de pacientes pluripatológicos y frágiles, estos niños requieren múltiples cuidados y terapias por todas las comorbilidades que presentan, con un gran consumo de recursos y tiempo, que influye en la salud tanto física como mental del cuidador, con el consecuente agotamiento del mismo9,10. El malestar del cuidador surge especialmente por la falta de coordinación en la asistencia sanitaria que estos pacientes requieren11 y está asociada fundamentalmente a aspectos organizativos en la prestación de servicios de la atención sanitaria más que a la intervención específica de los mismos12. En este sentido, sería fundamental crear la figura del “pediatra coordinador” en el paciente con PCI, a fin de que llevase una atención integrada del mismo y facilitase la coordinación entre Atención Primaria (AP) y el medio hospitalario, lo que mejoraría notablemente la calidad de vida del paciente y de la familia8,13. El pediatra de AP desempeña un papel fundamental en la atención al niño con PCI, y dada su mayor accesibilidad y cercanía a la familia, podría considerarse la figura ideal para organizar ese manejo integral del que hablamos. Para ello, debe conocer las comorbilidades asociadas con el fin de prevenirlas y, en caso de diagnosticarlas, saber cuándo derivarlas y sus opciones de tratamiento. Sin embargo, prácticamente no existen protocolos sobre el seguimiento del niño con PCI desde la consulta de AP.
En 2017 se publicaron la guía NICE, sobre valoración y manejo de la parálisis cerebral en menores de 25 años14 y, desde la comunidad de Castilla y León, una guía titulada Guía para el seguimiento de la parálisis cerebral en Atención Primaria15, que hace referencia a muchas de las cuestiones citadas, como el cribado precoz o el reconocimiento de las principales comorbilidades.
Recientemente, se ha publicado Abordaje integral del niño con parálisis cerebral, propuesta de seguimiento y derivación a especialistas dirigida a los pediatras de AP para a la atención integral del niño con PCI con afectación leve-moderada16. Sería, por tanto, deseable la elaboración y difusión de protocolos generalizados que unificasen las actividades a realizar y los criterios de derivación entre los diferentes profesionales.
Estas cuestiones nos llevan a plantearnos si realmente el pediatra de AP es la figura idónea para coordinar el manejo multidisciplinar del niño con PCI, si está preparado y se siente capacitado para hacerlo y cómo percibe el manejo que realiza de estos pacientes actualmente. Con el fin de valorar todos estos aspectos se ha realizado el presente estudio.
MATERIAL Y MÉTODOS
Diseño del estudio
Se realizó un estudio descriptivo y transversal, de ámbito nacional, llevado a cabo desde enero a febrero de 2021.
Población de estudio
La población de estudio estuvo compuesta por pediatras y médicos de familia dedicados a la pediatría que ejercían en AP a nivel nacional. Según el portal estadístico del Ministerio de Sanidad en 2019 había 6502 plazas de Pediatría de AP a nivel estatal17. Los criterios de inclusión fueron ser facultativo especialista en Pediatría o Medicina de Familia y trabajar en AP en el área de Pediatría. Se excluyeron médicos internos residentes o facultativos en Pediatría no dedicados a AP.
Tamaño muestral
Se estimó una muestra necesaria para que los resultados fueran representativos de 364 respuestas. Los cálculos se realizaron para obtener un margen de error de 0,05 y una confianza del 95% según la máxima variabilidad posible (50%)18.
Método de recogida de datos
Para la recogida de datos se diseñó un cuestionario pilotado previamente en pediatras. Se trató de un cuestionario en línea, anónimo y voluntario, con respuesta única, enviada a través de la plataforma Google Drive® mediante el Grupo de Investigación de la Asociación Española de Pediatría de Atención Primaria (AEPap) y lista de distribución de PEDIAP, quien invitaba a los profesionales a participar en el estudio, previa información sobre el mismo.
En él se incluyó información sobre datos sociodemográficos, manejo clínico del paciente con PCI y opinión sobre la capacidad de asistencia actual de estos pacientes, la figura de médico coordinador y la necesidad de formación (Tabla 1).
| Tabla 1. Cuestionario |
|---|
| Datos sociodemográficos |
| 1. Titulación |
| 2. Edad |
| 3. Sexo |
| 4. Experiencia en pediatría (ámbito hospitalario y extrahospitalario) |
| 5. ¿Ha trabajado previamente como pediatra en alguna unidad especializada en pacientes con parálisis cerebral? |
| 6. Provincia/ciudad de trabajo |
| 7. Ámbito de trabajo (rural, semiurbano, urbano) |
| 8. ¿Tiene en su cupo de pediatría algún paciente afecto de parálisis cerebral? |
| 9. ¿Existe en su área de trabajo una unidad especialidad en el manejo integrado del niño con parálisis cerebral? |
| 10. ¿Quién es el pediatra coordinador del niño con parálisis cerebral en su área de trabajo? |
| Manejo del paciente con parálisis cerebral desde la consulta de Atención Primaria |
| 11 ¿Deriva usted a los pacientes con parálisis cerebral a Atención Temprana? |
| 12. ¿Deriva usted a los pacientes con parálisis cerebral a rehabilitación? |
| 13. Los niños con parálisis cerebral presentan un importante riesgo de disfagia. ¿Qué realiza para su detección? |
| 14. ¿Realiza la valoración nutricional con medidas antropométricas de los niños con parálisis cerebral en su consulta de AP de forma rutinaria? |
| 15. ¿Realiza analítica sanguínea para valoración nutricional de los niños con parálisis cerebral? |
| 16. Los niños con parálisis cerebral presentan mayor riesgo de baja densidad mineral ósea y osteoporosis. ¿Qué realiza para su detección? |
| 17. ¿Realiza derivación a Oftalmología de los pacientes con parálisis cerebral? |
| 18. ¿Realiza derivación a Odontología de los pacientes con parálisis cerebral? |
| Opinión sobre asistencia actual en el paciente con parálisis cerebral |
| 19. ¿Considera que dispone de suficiente formación para la atención de niños con parálisis cerebral? |
| 20. ¿Piensa que su conocimiento actual en el manejo de parálisis cerebral infantil es limitado? |
| 21. ¿Ha recibido cursos específicos de formación en esta patología? |
| 22. ¿Cree necesaria la formación específica en esta patología? |
| 23. ¿Existe en su comunidad autónoma algún protocolo específico sobre pacientes con parálisis cerebral infantil? |
| 24. ¿Considera que es necesaria la existencia de un protocolo específico de seguimiento y derivación al niño con parálisis cerebral en su ámbito de trabajo? |
| 25. ¿Le gustaría ser el pediatra coordinador del proceso trabajando de manera conjunta con los diferentes especialistas hospitalarios? |
| 26. ¿Quién considera que debería ser el médico coordinador del niño con parálisis cerebral infantil en su área de trabajo? |
| 27. ¿Considera que usted está capacitado para ser el médico coordinador de sus pacientes con parálisis cerebral? |
| 28. ¿Considera que las familias de sus pacientes con parálisis cerebral están satisfechas con la coordinación en la atención que reciben? |
| 29. ¿Considera que mejoraría la calidad de vida de sus pacientes con parálisis cerebral y sus familiares si usted fuera el médico coordinador? |
| 30. ¿Considera que sería necesaria la formación de unidades de atención multidisciplinar en el ámbito hospitalario para el seguimiento de pacientes con parálisis cerebral? |

Análisis estadístico
Se realizó análisis descriptivo de la muestra obtenida mediante el cálculo de porcentajes y valoración de la distribución de las respuestas obtenidas en las diferentes comunidades autónomas.
Se calculó el porcentaje global de respuesta que se dio a cada una de las preguntas del cuestionario. Posteriormente, se hizo el análisis de las respuestas por grupos de edad, por pediatras que actúan como pediatra coordinador de pacientes PCI y por pediatras que cuentan en su zona con unidades específicas para PCI. Entre los grupos estudiados se estimó si había diferencias estadísticamente significativas mediante la prueba de Chi-cuadrado. Se consideró que existían diferencias cuando el valor de la p era inferior a 0,05. Los cálculos se realizaron mediante el programa SPSS versión 23.0.
Aspectos éticos
Dado que no se incluyen datos de pacientes y las encuestas han sido anónimas y voluntarias, no se ha considerado necesaria la aprobación por un Comité de Ética.
RESULTADOS
Características de la muestra
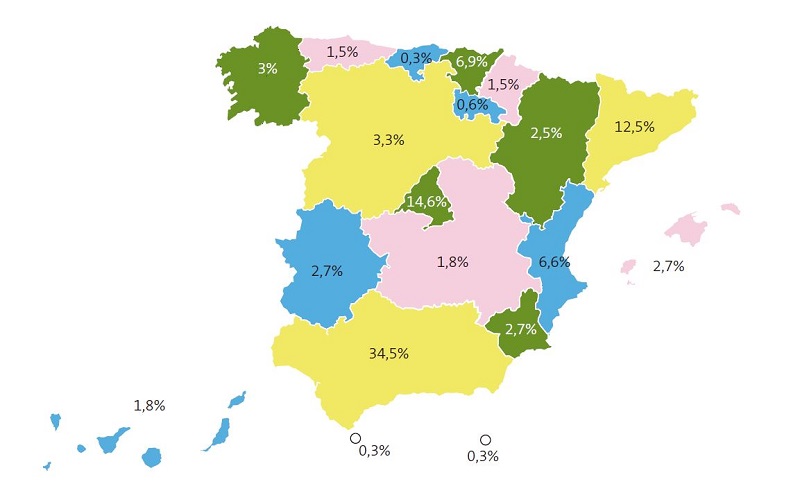
Se recibieron 335 respuestas. El 93,7% son pediatras y el 6,3% médicos de familia. El 84,5% fueron mujeres, siendo el grupo mayoritario la edad comprendida entre los 50 y 59 años (41,50%). Respecto a la experiencia laboral, la mayoría tenían una experiencia de más de 20 años (54,3%). El 76,4% trabajaban en un área urbana. Podemos observar la distribución de respuestas recibidas por comunidades autónomas en la Figura 1.
En cuanto a la experiencia con pacientes afectos de PCI, el 96,7% de los encuestados no habían trabajado previamente en unidades especializadas en pacientes con parálisis cerebral. Sin embargo, hasta el 78,5% tenían un niño o más con PCI en su cupo.
En lo que respecta a la organización en la atención de pacientes afectos de PCI, un 58,2% refieren no existir en su área de trabajo una unidad especialidad en el manejo integrado del niño con PCI, un 22,1% afirman la existencia de estas unidades y un 19,7% lo desconoce. Sobre la figura del pediatra coordinador en estos pacientes, en un 43,6% de los casos no hay figura coordinadora, en el 31,9% es el pediatra hospitalario y, finalmente, en el 9% es el pediatra de AP. Un 15,5% desconoce quién ejerce la figura de médico coordinador.
Respuestas generales al cuestionario
Respecto al manejo del paciente con PCI desde la consulta de AP, se realizaron 8 preguntas que se muestran en la Tabla 2.
| Tabla 2. Porcentajes de respuestas respecto al manejo del paciente con PCI | |
|---|---|
| Derivación a Atención Temprana | |
| Sí, tras la sospecha, aunque no haya sido valorado por Neuropediatría | 66,9% |
| Sí, pero solo tras la indicación de Neuropediatría | 1,8% |
| Dependiendo del paciente (a veces deriva abAtención Temprana y otras a Neuropediatría) | 25,1% |
| No, es Neuropediatría quien deriva | 6,2% |
| Derivación a Rehabilitación | |
| Sí, tras el diagnóstico | 52,2% |
| Sí, pero si aparecen deformidades articulares | 4,8% |
| No, la derivación la realiza el pediatra hospitalario | 43% |
| Derivación a Oftalmología | |
| Sí, siempre | 21,3% |
| Sí, pero si aparece patología (nistagmo, falta de atención visual…) | 29,2% |
| No, la derivación la realiza el pediatra hospitalario | 49,5% |
| Derivación a Odontología | |
| Sí, siempre | 35,2% |
| Sí, pero si aparecen patologías | 42,4% |
| No, la derivación la realiza el pediatra hospitalario | 22,4% |
| Detección de la disfagia y derivación a Gastroenterología | |
| Deriva siempre a Gastroenterología | 5,8% |
| Interroga de forma periódica a la familia la presencia de signos de disfagia derivando si presenta sintomatología | 50,4% |
| No interroga habitualmente a la familia. Solo si la familia refiere síntomas deriva a Gastroenterología | 30,7% |
| Ni interroga ni deriva. La derivación la realiza el pediatra hospitalario | 13,1% |
| Valoración nutricional rutinaria con medidas antropométricas | |
| Sí, periódicamente | 37% |
| No, se realiza por gastroenterología o pediatra hospitalario | 63% |
| Valoración nutricional con controles analíticos | |
| Sí, sistemáticamente cada 6 meses | 1,5% |
| Sí, cada año | 3,2% |
| Sí, cuando presenta indicación por inadecuada ganancia ponderal | 28,1% |
| No, los realiza el pediatra hospitalario | 67,2% |
| Detección de la baja densidad mineral ósea y osteoporosis y derivación a Reumatología | |
| Deriva a todos los niños a Reumatología | 1,2% |
| Solicitaría, si pudiera, una densitometría en aquellos niños con factores de riesgo (fracturas previas, menor movilidad) | 26,2% |
| Solicitaría, si pudiera, densitometría a todos los niños antes de derivar a Reumatología | 8,1% |
| Sólo deriva a Reumatología si sospecha de fracturas óseas | 6% |
| No deriva. La derivación la realiza el pediatra hospitalario | 58,5% |

Finalmente, se preguntó la opinión y percepción sobre la asistencia actual a los niños con PCI.
La gran mayoría de los encuestados consideran que no disponen de formación suficiente para la atención de niños con PCI (91,1%) y que su conocimiento es limitado para el manejo de los mismos (94,6%). Casi la totalidad opinan que es necesaria la formación específica en esta patología (97,3%) y tan solo un 10,1% ha recibido cursos de la misma. Dentro de la minoría que ha recibido algún tipo formación, un 94% corresponde a pediatras que tienen en su cupo algún paciente con PCI, resultando estadísticamente significativo.
Se indagó acerca de la necesidad de un protocolo específico para el seguimiento y derivación de los niños con PCI desde AP; prácticamente todos los encuestados afirmaban dicha necesidad (99,1%). Se interrogó sobre la existencia de protocolos específicos para el manejo de estos pacientes en la comunidad autónoma correspondiente, de modo que un 10,2% sí los conoce, pero la mayoría lo desconoce (62,8%) o afirman que no los hay (27%). A pesar de que Castilla y León es la única comunidad donde existe un protocolo conocido, tan solo 2 pediatras (18%) de los que participaron en el presente estudio desde aquella comunidad conocen su existencia.
Respecto a la coordinación en la atención del paciente con PCI, la mayoría (78,2%) abogan por un modelo mixto de coordinación (pediatra hospitalario y pediatra de AP), un 14,9% considera que es el pediatra de AP quien debe ejercer este papel y el 6,9% restante, el pediatra hospitalario. Más de la mitad (57,2%) respondieron que les gustaría ser el pediatra coordinador trabajando de manera conjunta con los especialistas hospitalarios y consideran, en un 60,9%, que la calidad de vida de estos niños con PCI y sus familias mejorarían si así fuera. Sin embargo, un 65,1% piensa que no está capacitado para ejercer esta labor de médico coordinador y el 75% considera que la familia no está satisfecha con la atención actualmente recibida.
En la última cuestión, se planteó si consideran necesaria la formación de unidades de atención multidisciplinar en el ámbito hospitalario para el seguimiento de pacientes con PCI, siendo la respuesta afirmativa para la mayoría de la muestra (97,3%).
Respuestas por grupos de edad
Se analizaron las respuestas acerca de la opinión y percepción sobre la asistencia al niño con PCI clasificando la muestra según la edad en menores de 50 años (n = 144; 42,3%) y mayores de 50 años (n = 191, 57%). Observamos que a los pediatras de menor edad les gustaría ser el médico coordinador de los pacientes PCI y además creen que esto mejoraría la calidad de vida de los pacientes, resultando estadísticamente significativo. Podemos ver las diferencias entre ambos grupos de edad en la Tabla 3.
| Tabla 3. Odds ratio de respuestas afirmativas de los pediatras jóvenes respecto a los veteranos | |
|---|---|
| OR (IC 95%) pediatras jóvenes/pediatras veteranos | |
| ¿Considera que dispone de suficiente formación para la atención de niños con parálisis cerebral? | 0,76 (0,33-1,72) |
| ¿Piensa que su conocimiento actual en el manejo de parálisis cerebral infantil es limitado? | 0,56 (0,22-1,54) |
| ¿Ha recibido cursos específicos de formación en esta patología? | 1,05 (0,51-2,15) |
| ¿Cree necesaria la formación específica en esta patología? | 6,25 (0,77-3,15) |
| ¿Considera que es necesaria la existencia de un protocolo específico de seguimiento y derivación al niño con parálisis cerebral en su ámbito de trabajo? | 0,37 (0,03-4,1) |
| ¿Le gustaría ser el pediatra coordinador del proceso trabajando de manera conjunta con los diferentes especialistas hospitalarios? | 1,98 (1,27-3,01) |
| ¿Considera que usted está capacitado para ser el médico coordinador de sus pacientes con parálisis cerebral? | 1,03 (0,66-1,63) |
| ¿Considera que las familias de sus pacientes con parálisis cerebral están satisfechas con la coordinación en la atención que reciben? | 1,02 (0,61-1,68) |
| ¿Considera que mejoraría la calidad de vida de sus pacientes con parálisis cerebral y sus familiares si usted fuera el médico coordinador? | 2,1 (1,34-3,35) |
| ¿Considera que sería necesaria la formación de unidades de atención multidisciplinar en el ámbito hospitalario para el seguimiento de pacientes con parálisis cerebral? | 2,71 (0,55-1,32) |

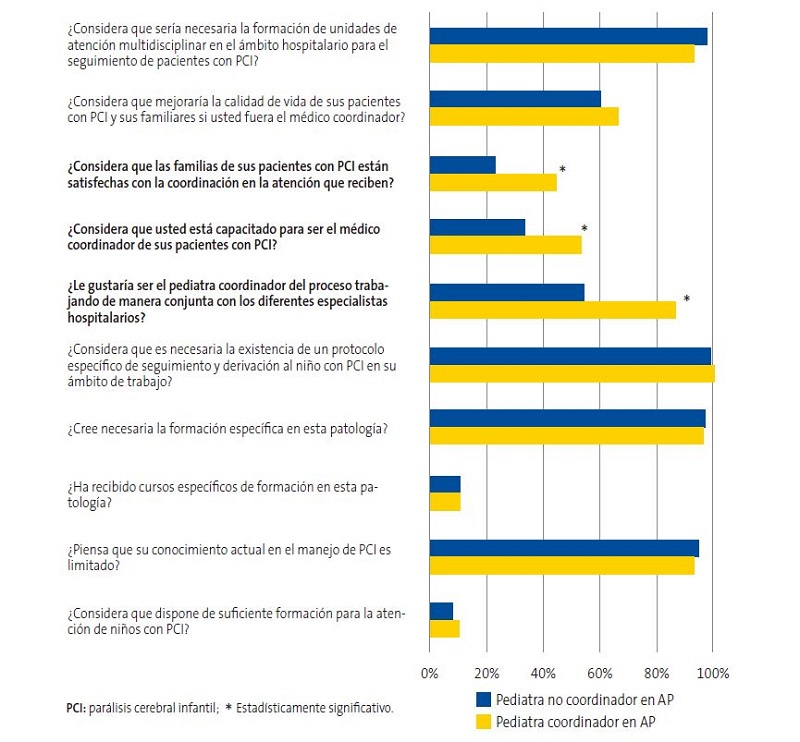
Respuestas de los pediatras que actúan como médico coordinador de pacientes con PCI
Se aplicó el test χ2 sobre las respuestas en el área de opinión entre aquellos pediatras que coordinan el abordaje de los pacientes con PCI desde AP frente a aquellos que no lo hacen (Fig. 2). Observamos que al pediatra que ejerce como médico coordinador le gusta ejercer como tal en un 86,6% de los casos y considera que las familias están satisfechas con su labor en un 46,6%, respecto al médico no coordinador, que respondió de manera afirmativa en un 54,5% y 22,2%, respectivamente, siendo estadísticamente significativo.
| Figura 2. Porcentajes de respuestas afirmativas de los pediatras que actúan como médicos coordinadores de pacientes PCI desde AP vs. pediatras no coordinadores. |
|---|
 |

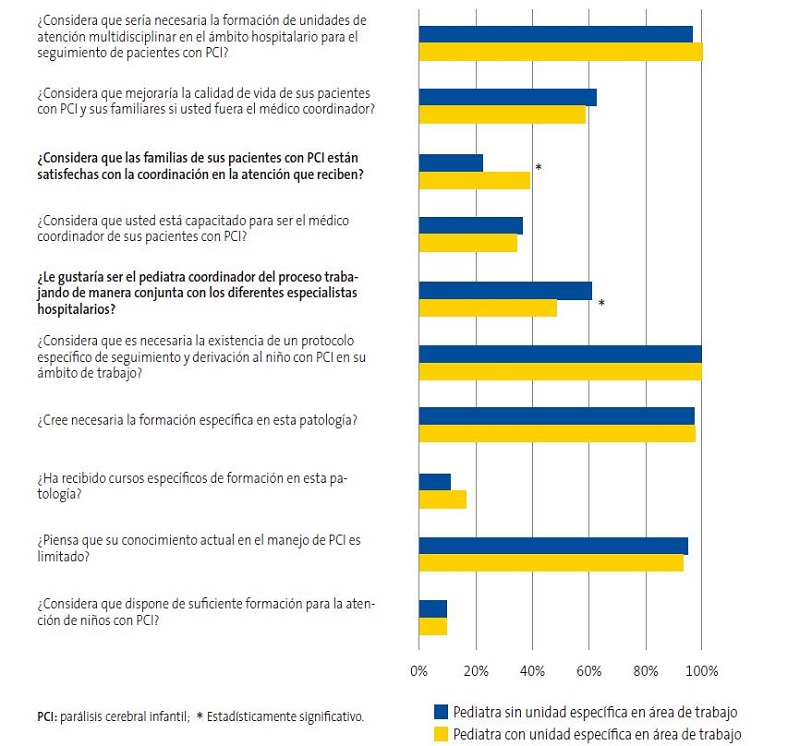
Respuestas de los pediatras que tienen unidades específicas de manejo de PCI en su área de trabajo
Así mismo, se empleó el mismo test en las respuestas de opinión entre los profesionales que trabajan en áreas donde existen consultas específicas para el manejo de niños con PCI respecto a aquellos que no disponen de dichas consultas (Fig. 3). Entre los resultados, comprobamos que aquellos profesionales de AP que tienen consultas específicas en su área de trabajo manifiestan en un 47,2% que les gustaría ejercer como médico coordinador y consideran que las familias están satisfechas en un 37,8% de los casos, respecto al pediatra que no dispone de dicha unidad, que respondió de manera afirmativa en un 60,15% y 21,07%, respectivamente, resultando estadísticamente significativo.
| Figura 3. Porcentajes de respuestas afirmativas de los pediatras que tienen unidades específicas de pacientes con PCI en su área de trabajo vs. pediatras sin unidades específicas |
|---|
 |

DISCUSIÓN
La gran mayoría de los encuestados consideran que los conocimientos y la formación de que disponen para el manejo del paciente con PCI son insuficientes. A pesar de que más de la mitad tiene algún paciente con PCI en su cupo, tan solo uno de cada diez ha recibido algún curso de formación. De igual modo, en torno al 90% desconoce si existen protocolos específicos en su comunidad para el seguimiento del niño con PCI desde AP. En el caso de Castila y León, única comunidad autónoma que posee una guía de manejo del paciente con PCI desde AP15, tan solo el 18% de los pediatras que respondieron al cuestionario lo conocían. Teniendo esto en cuenta, prácticamente la totalidad de la muestra reivindica que sería fundamental la formación y la creación de protocolos en los que poder guiarse.
La coordinación del manejo integral del niño es otro punto preocupante. En un 59,9% de los casos afirman no haber ningún médico coordinador o desconocen quién ejerce tal función. De la totalidad de los encuestados, tan solo un 9% ejerce como coordinador desde AP. Es llamativo que, pese a los resultados, a más del 50% de los pediatras les gustaría ejercer supervisando la atención integral de los niños con PCI, abogando por un modelo mixto de coordinación. Sin embargo, tan solo un tercio se siente capacitado para hacerlo. Por tanto, probablemente se trate más de un problema de aptitud que de actitud. La satisfacción familiar sobre el cuidado que recibe su hijo enfermo es otro tema a destacar. Tan solo una cuarta parte de los pediatras considera que los cuidadores están satisfechos con la atención recibida, aunque esta percepción varía según los recursos que el sistema sanitario puede ofrecer. Así pues, aquellos profesionales que dan una atención integral al niño con PCI o disponen de unidades específicas que lo hacen, consideran que las familias están más satisfechas frente a los que no disponen de estos servicios, siendo este resultado estadísticamente significativo.
Hasta la fecha, hay escasas publicaciones en España que aborden el cuidado del niño con PCI y más aún si nos centramos en el ámbito de AP, salvo la citada guía de Castilla y León15 y la reciente propuesta de seguimiento Abordaje integral del niño con parálisis cerebral16. Tampoco hay nada publicado sobre la percepción y opinión de los pediatras respecto a dicho tema. Existe un documento de consenso nacional sobre la atención de los niños con necesidades de cuidados paliativos entre los que podrían incluirse algunos de los niños con PCI. Dicho documento propone un modelo de atención integral que considere el área física, psicológica, espiritual y social del niño basado fundamentalmente en el domicilio19.
Actualmente, la atención del niño con PCI no se organiza de manera homogénea en nuestro país. Solo en algunos hospitales existen unidades específicas que abordan al paciente crónico-complejo, pero no todos los niños con PCI tienen acceso a ellas20. En este sentido, sería fundamental centralizar los cuidados en el lugar donde reside el paciente, tal y como plantean Dewan et al.21. Según los diferentes estudios, más de la mitad de las familias de pacientes complejos no están satisfechos con los recursos sanitarios de que disponen11,22. Consideran que, finalmente, es la familia la que acaba asumiendo toda la responsabilidad en la coordinación del cuidado de su hijo, lo que conlleva un importante desgaste emocional y problemas económicos12,23. Si desde AP se ejerciera este abordaje integral del paciente con PCI, quizás pudieran paliarse estas desigualdades. De esta manera, no solo el niño enfermo tendría garantizada una atención coordinada de fácil acceso, sino que la familia podría abandonar su rol de “coordinador”, pudiendo dedicarse exclusivamente al cuidado en casa, mejorando probablemente la calidad de vida del niño y su familia.
El presente trabajo presenta una serie de limitaciones. Por una parte, hay que señalar que, aunque no se ha alcanzado el número de cuestionarios esperados (364 respuestas), se obtuvieron 335 respuestas, de tal modo que no se ha modificado la precisión al estar muy próximos al número deseado. El margen de error final que tiene este estudio con la muestra obtenida es 5,21%24. Por otra parte, hay que destacar el desequilibrio de la muestra entre los diferentes territorios. Sin embargo, dado que se ha obtenido representación de todas las comunidades autónomas y el funcionamiento de la asistencia en AP es similar en todo el Estado, no cabe encontrar grandes diferencias entre comunidades.
A pesar de las limitaciones expuestas, hay que indicar que los resultados, hasta ahora no estudiados, son muy homogéneos y todos conducen hacia una misma dirección: la necesidad de formar al pediatra de AP, organizar consultas que permitan el trabajo coordinado del paciente con PCI y crear protocolos en los que los profesionales de AP sean partícipes y puedan difundirse adecuadamente para que todos conozcan su existencia. Esto podría ser un punto de partida para la creación de nuevos modelos organizativos en los que el pediatra de AP, como médico de confianza y más accesible para la familia, se encargara de ese abordaje integral del niño con PCI tras una formación previa y con la colaboración de los pediatras especialistas. Sería interesante estudiar la percepción de las familias según la atención que reciben actualmente y ver el cambio de la misma, así como la nueva opinión de los pediatras, si esto se llevara a cabo.
CONCLUSIÓN
En conclusión, el presente trabajo aporta datos preocupantes respecto a la opinión y percepción de los pediatras respecto al abordaje integral del paciente con PCI. La mayoría piensan que es fundamental el manejo holístico del niño con PCI y que el pediatra de AP participe del mismo. Son conscientes de que los cuidadores están desbordados, insatisfechos y de que la complejidad de los cuidados no está cubierta. Sin embargo, prácticamente la totalidad de los pediatras encuestados reconocen que no están capacitados y que carecen de conocimientos para coordinar la atención de estos pacientes. Así mismo, consideran necesaria la creación de protocolos y la realización de cursos que los formen, así como colaborar de manera conjunta con los centros hospitalarios para abordar todas las necesidades del niño con PCI.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS
AP: Atención Primaria · PCI: parálisis cerebral infantil.
BIBLIOGRAFÍA
- Oskoui M, Coutinho F, Dykeman J, Jetté N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55:509-19.
- Hafström M, Källén K, Serenius F, Maršál K, Rehn E, Drake H, et al. Cerebral Palsy in Extremely Preterm Infants. Pediatrics. 2018;141:e20171433.
- Marret S, Vanhulle C, Laquerriere A. Pathophysiology of cerebral palsy. Handbook Clin Neurol. 2013;111:169-76.
- Rosenbaum P, Paneth N, Leviton A, Goldstein M. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol. 2007;49:8-14.
- Smithers-Sheedy H, McIntyre S, Gibson C, Meehan E, Scott H, Goldsmith S, et al. A special supplement: findings from the Australian Cerebral Palsy Register, birth years 1993 to 2006. Dev Med Child Neurol. 2016;58:5-10.
- Palisano RJ, Hanna SE, Rosenbaum PL, Russell DJ, Walter SD, Wood EP, et al. Validation of a Model of Gross Motor Function for Children With Cerebral Palsy. Phys Ther. 2000;80:974-85.
- Novak I, Hines M, Goldsmith S, Barclay R. Clinical Prognostic Messages From a Systematic Review on Cerebral Palsy. Pediatrics. 2012;130:e1285-312.
- Martínez de Zabarate JM, Ros I, Peña JL, García R, Rodríguez G. Carga del cuidador del paciente con parálisis cerebral moderada-grave: ¿influye el estado nutricional? An Pediatr (Barc). 2021;94:311-7.
- Byrne MB, Hurley DA, Daly l, Cunningham CG. Health status of caregivers of children with cerebral palsy: Caregiver health in CP. Child Care Health Dev. 2010;36:696-702.
- Tseng M-H, Chen K-l, Shieh J-Y, Lu l, Huang C-Y, Simeonsson RJ. Child characteristics, caregiver characteristics, and environmental factors affecting the quality of life of caregivers of children with cerebral palsy. Disability and Rehabilitation. 2016;38:2374-82.
- Liptak GS, Orlando M, Yingling JT, Theurer-Kaufman KL, Malay DP, Tompkins LA, et al. Satisfaction With Primary Health Care Received by Families of Children With Developmental Disabilities. J Pediatr Health Care. 2006;20:245-52.
- Hayles E, Jones A, Harvey D, Plummer D, Ruston S. Delivering healthcare services to children with cerebral palsy and their families: a narrative review. Health Soc Care Community. 2015;23:242-51.
- Schwabe AL. Comprehensive Care in Cerebral Palsy. Phys Med Rehabil Clin N Am. 2020;31:1-13.
- Shaunak M, Kelly VB. Cerebral palsy in under 25 s: assessment and management, 2017. En: NICE Guideline [en línea] [consultado el 13/09/2022]. Disponible en www.nice.org.uk/guidance/ng62
- Guía para el seguimiento de la parálisis cerebral en Atención Primaria. En: Portal de Salud de la Junta de Castilla y León, Consejería de Sanidad, 2017 [en línea] [consultado el 13/09/2022]. Disponible en www.saludcastillayleon.es/institucion/es/biblioteca/materiales-consejeria-sanidad/buscador/guia-seguimiento-ninos-paralisis-cerebral-atencion-primaria
- Peláez Cantero MJ, Moreno Medinilla EE, Cordón Martínez A, Gallego Gutiérrez S. Abordaje integral del niño con parálisis cerebral. An Pediatr (Barc). 2021;95:276.e1-276.e11.
- Recursos, población asignada y actividad. Ministerio de Sanidad, Consumo y Bienestar Social. En: Portal Estadístico del SNS-Portal Estadístico del SNS, 2019 [en línea] [consultado el 13/09/2022]. Disponible en www.mscbs.gob.es/estadEstudios/estadisticas/docs/siap/Resumen_grafico_2019.pdf
- Calculadora de tamaño de muestras. QuestionPro [en línea] [consultado el 13/09/2022]. Disponible en www.questionpro.com/es/calculadora-de-muestra.html
- Cuidados Paliativos Pediátricos en Sistema Nacional de Salud: Criterios de Atención. Ministerio de Sanidad, Servicios Sociales e Igualdad, 2014 [en línea] [consultado el 13/09/2022]. Disponible en www.sanidad.gob.es/ca/organizacion/sns/planCalidadSNS/pdf/01-Cuidados_Paliativos_Pediatricos_SNS.pdf
- Gimeno Sánchez I, Muñoz Hiraldo ME, Martino Alba RJ, Moreno Villares JM. Atención específica para los niños con complejidad médica en España: buscando el mejor modelo. An Pediatr (Barc). 2016;85:56-7.
- Dewan T, Cohen E. Children with medical complexity in Canada. Paediatr Child Health. 2013;18:518-22.
- Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130:e1463-70.
- Brehaut JC, Garner RE, Miller AR, Lach LM, Klassen AF, Rosenbaum PL, et al. Changes over time in the health of caregivers of children with health problems: growth-curve findings from a 10-year Canadian population-based study. Am J Public Health. 2011;101:2308-16.
- Calculadora de margen de error. QuestionPro [en línea] [consultado el 13/09/2022]. Disponible en www.questionpro.com/es/calculadora-de-margen-de-error.html