Vol. 22 - Num. 88
Originales
Prescripción de antibióticos en niños en Atención Primaria. Estudio en un área administrativa de Osakidetza-Servicio Vasco de Salud
José M.ª Arginzoniz Marzanaa, Ane Antón Ladislaob, Nekane Jaio Atelac, María Armendáriz Cuñadoc
aPediatra. CS de Iurreta. Vizcaya. España.
bUnidad de Investigación. Hospital Galdakao-Usansolo. Red de Investigación en Servicios de Salud en Enfermedades Crónicas (REDISSEC). Vizcaya. España.
cFarmaceútica de Atención Primaria. OSI Barrualde-Galdakao. Osakidetza-Servicio Vasco de Salud. Vizcaya. España.
Correspondencia: JM Arginzoniz. Correo electrónico: txemarginzoniz@gmail.com
Cómo citar este artículo: Arginzoniz Marzana JM, Antón Ladislao A, Jaio Atela N, Armendáriz Cuñado M. Prescripción de antibióticos en niños en Atención Primaria. Estudio en un área administrativa de Osakidetza-Servicio Vasco de Salud. Rev Pediatr Aten Primaria. 2020;22:363-70.
Publicado en Internet: 23-11-2020 - Número de visitas: 12000
Resumen
Introducción: según los estudios disponibles, el consumo de antibióticos en niños es elevado en España. No obstante, puede haber grandes diferencias territoriales incluso entre áreas geográficas pequeñas. El objetivo del estudio es conocer la prescripción de antibióticos en la edad pediátrica y describir sus características en el área administrativa de la Organización Sanitaria Integrada (OSI) Barrualde-Galdakao del Servicio Vasco de Salud-Osakidetza.
Material y métodos: se han estudiado retrospectivamente las prescripciones antibióticas realizadas a niños de 0 a 13 años a lo largo de los años 2015, 2016 y 2017. Los datos han sido extraídos de la base de datos Presbide del Servicio Vasco de Salud-Osakidetza. Se han determinado tasas de episodios tratados con antibiótico y su prevalencia, así como tipos de antibióticos utilizados.
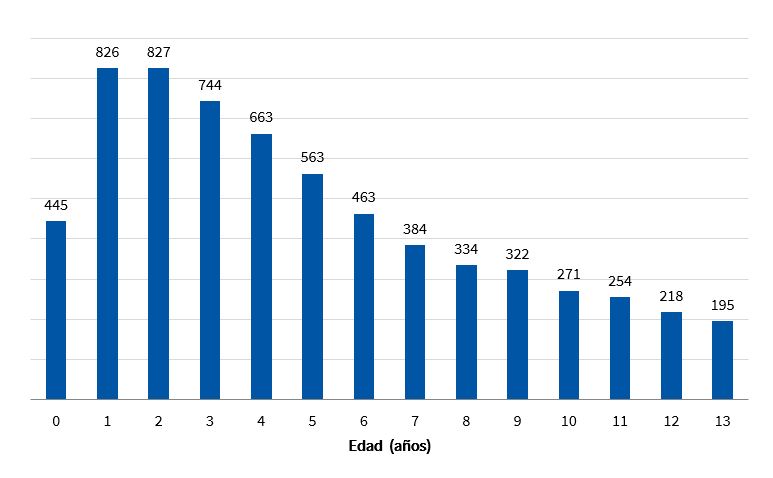
Resultados: se han analizado 56 974 prescripciones de antibiótico dispensado a 40 824 niños a lo largo de tres años. El número de episodios tratados con antibiótico por 1000 niños/año fue de 465,20. El porcentaje de niños que recibió al menos una dispensación antibiótica/año fue de 30,72. La máxima incidencia de prescripción se dio en niños de uno y dos años (826 y 827 episodios tratados/1000 niños/año respectivamente). El 64,61% de las dispensaciones fueron de amoxicilina.
Conclusión: nuestras cifras de prescripción de antibióticos en niños son elevadas en comparación con los países poco prescriptores del norte de Europa y sensiblemente inferiores a los datos disponibles de estudios hechos en España y de otros países del área mediterránea.
Palabras clave
● Antibióticos ● Atención Primaria ● Farmacoepidemiología ● Niños ● PrescripciónINTRODUCCIÓN
El uso inadecuado de los antibióticos, además de producir daños individuales e incremento del gasto sanitario puede generar desarrollo de resistencias bacterianas1 con graves problemas de salud pública2. La gran mayoría de los antibióticos se prescriben en Atención Primaria3 y la de 0 a 4 años es la franja de edad con mayor prevalencia antibiótica3,4.
Hasta en el 60% de las ocasiones se utilizan para tratar infecciones respiratorias5, mayoritariamente víricas y según algunos autores pueden ser inadecuados hasta en el 50% de los casos6.
España, junto a otros países del área mediterránea, es uno de los mayores consumidores de antibióticos de Europa7 y los escasos estudios realizados en niños muestran datos en el mismo sentido8. No obstante, puede haber grandes diferencias en la utilización de antibióticos en niños, no solo entre países8,9, sino entre regiones del mismo país10 y entre profesionales de ámbitos geográficos más pequeños11,12.
El consumo general de antibióticos en el País Vasco es elevado, con valores muy similares a los de las demás comunidades autónomas13 pero no conocemos ningún estudio de la prescripción antibiótica en niños de esta comunidad.
El objetivo de nuestro estudio es conocer la prescripción de antibióticos en la edad pediátrica y describir sus características en el área administrativa de la Organización Sanitaria Integrada (OSI) Barrualde-Galdakao del Servicio Vasco de Salud-Osakidetza.
MATERIAL Y MÉTODOS
Presentamos un estudio de cohorte retrospectiva circunscrita a la OSI Barrualde-Galdakao, con un análisis descriptivo de la prescripción antibiótica en niños. La OSI Barrualde-Galdakao de Osakidetza-Servicio Vasco de Salud incluye 17 unidades de Atención Primaria (UAP) que dan servicio a una población de 313 000 personas. La población estudiada abarca niños de 0 a 13 años y el tiempo analizado corresponde a los años 2015, 2016 y 2017.
La fuente de datos es la base de datos Presbide, que recoge la prescripción medicamentosa a pacientes ambulatorios que se realiza en Osakidetza-Servicio Vasco de Salud. Dispone de información sobre el tipo de antibiótico prescrito según el código Anatomical, Therapeutic, Chemical Classification System (ATC), fecha de prescripción y dispensación, código del paciente, así como su edad, sexo y UAP de procedencia. Se han estudiado las prescripciones bajo código ATC J01 (antibióticos de uso sistémico); excluyéndose por lo tanto del análisis los tuberculostáticos, antifúngicos, antiparasitarios y antibióticos tópicos. Se han eliminado las prescripciones que no llegaron a dispensarse en farmacia. Si se han registrado dos o más dispensaciones del mismo antibiótico a un paciente en el intervalo igual o menor de 14 días, se han contabilizado como una dispensación (un episodio tratado).
Se han analizado las siguiente variables: número de dispensaciones o episodios tratados con antibiótico en 1000 niños/año (tasa de episodios tratados con antibiótico) y su distribución según edad, mes del año y UAP; porcentaje de niños que ha recibido al menos una dispensación antibiótica/año (prevalencia antibiótica) y su distribución según rangos de edad y sexo. Se ha estudiado también el tipo y proporción de antibióticos utilizados, así como su distribución por subgrupos clasificados como penicilinas de primera y segunda línea, macrólidos de primera y segunda generación, cefalosporinas y otros (Tabla 1).
| Tabla 1. Clasificación de antibióticos | |
|---|---|
| Penicilinas 1.ª línea | Amoxicilina, ampicilina, dicloxacilina, oxacilina, penicilina V potásica |
| Penicilinas 2.ª línea | Amoxicilina-ácido clavulánico |
| Macrólidos 1.ª generación | Eritromicina, josamicina |
| Macrólidos 2.ª generación | Azitromicina, claritromicina, roxitromicina |
| Cefalosporinas | Cefaclor, cefadroxilo, cefixima, cefuroxima, cefalexina, ceftibuteno, cefditoren, cefpodoxima, cefprozil |
| Otros | Quinolonas, clindamicina, doxiciclina, minociclina, nitrofurantoina, vancomicina, linezolid, trimetoprim-sulfametoxazol |

Para ello, se utilizaron frecuencias y porcentajes y la comparación de las tasas entre los diferentes grupos se midieron mediante la prueba de la χ2.
Los datos poblacionales se han obtenido de la base de datos de Osabide de Osakidetza-Servicio Vasco de Salud.
Todos los análisis se realizaron mediante el software estadístico SAS 9.4.
RESULTADOS
La población examinada fue de 40 901 niños en 2015, 41 059 en 2016 y 40 512 en 2017, de los que el 48,12% eran mujeres.
Del periodo de tiempo estudiado se analizaron 56 974 prescripciones de antibiótico dispensado. No llegaron a dispensarse en farmacia 7814 prescripciones (12,06%). No se contabilizaron 6375 dispensaciones (10,06%), por ser una dispensación repetida del mismo antibiótico, al mismo paciente, en el intervalo igual o menor de 14 días.
En el periodo estudiado, la tasa de episodios tratados con antibiótico fue de 465,20/1000 niños/año y el porcentaje de niños con al menos un episodio tratado/año fue de 30,72%.
La distribución según edad de la tasa de episodios tratados (Fig. 1) muestra el pico de incidencia en los niños de uno y dos años (826 y 827 episodios tratados por 1000 niños/año respectivamente), con descenso relativamente uniforme en las edades posteriores.
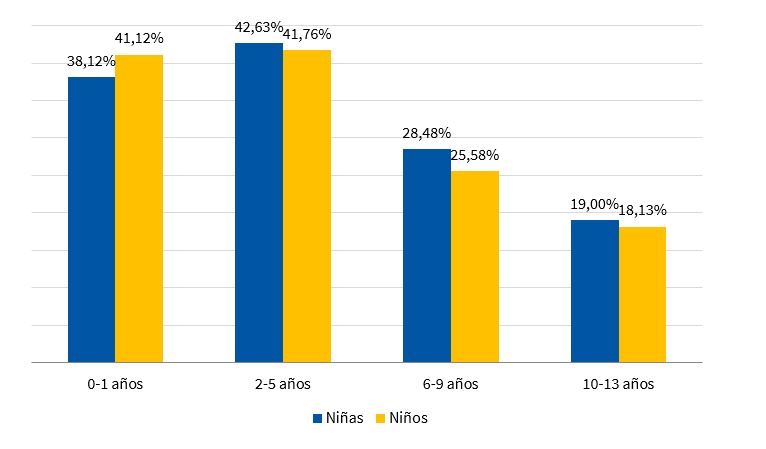
En la Fig. 2 podemos observar que la edad preescolar (2-5 años) fue el rango de edad con mayor prevalencia antibiótica (p <0,0001). La prevalencia también fue mayor en los niños que en las niñas lactantes (0-1 años; p <0,0001), invirtiéndose la relación entre sexos a partir de la edad preescolar.
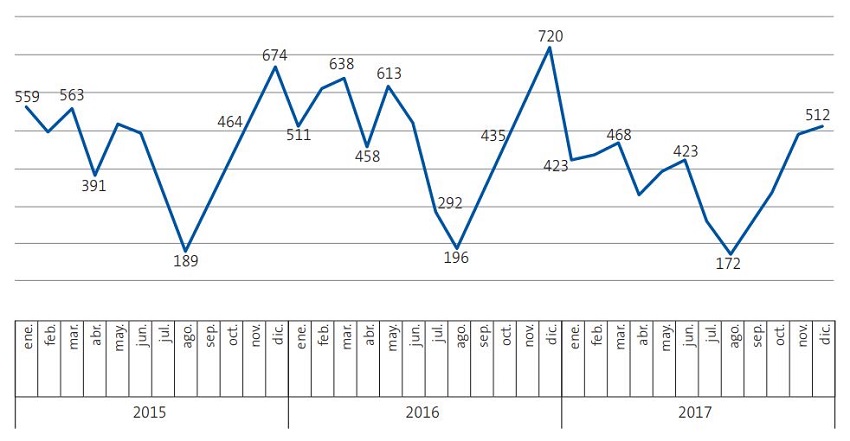
Durante el primero y último trimestres de los años estudiados se realizaron el 59,43% de los tratamientos, con una tasa de episodios tratados de 553/1000 niños/año, frente al semestre de abril a septiembre, que presentó una tasa de 378/1000 niños/año. En el conjunto de los trimestres citados, se prescribió un 32% más de antibióticos que el resto del año. En la Fig. 3 puede observarse la variabilidad mensual de la tasa de episodios tratados a lo largo de los años examinados.
| Figura 3. Tasa de episodios tratados con antibiótico (por 1000 niños/año) por meses y años del estudio |
|---|
 |

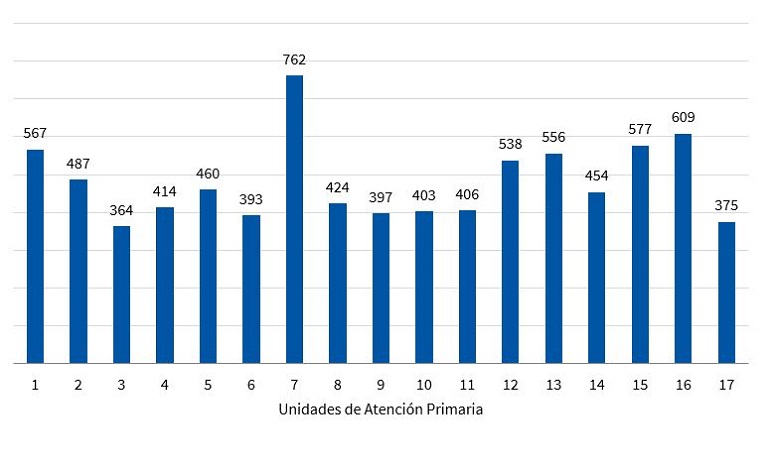
Las tasas de episodios tratados con antibiótico en las diferentes UAP oscilaron entre 364/1000/niños/año y 762/1000 niños/año, presentando diferencias estadísticamente significativas (p <0,0001) entre muchas de ellas. En la Fig. 4 pueden observarse los valores de las 17 UAP.
| Figura 4. Tasas de episodios tratados con antibiótico (por 1000 niños/año) según unidad de Atención Primaria |
|---|
 |

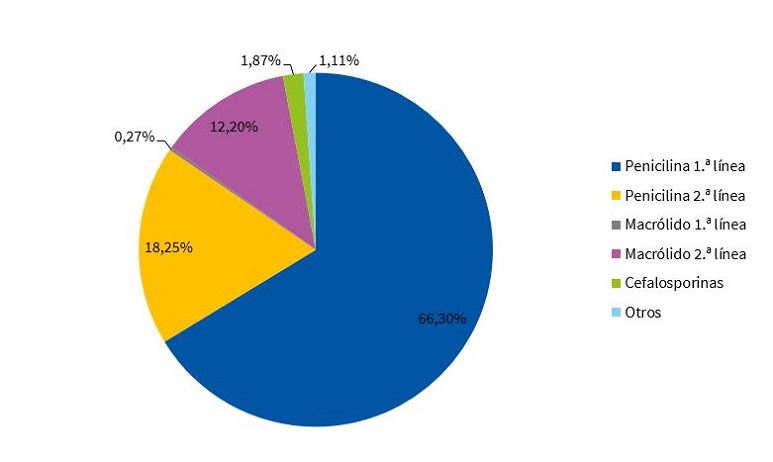
Los antibióticos más frecuentemente utilizados aparecen en la Tabla 2. Más del 90% del total de las dispensaciones correspondió a tres antibióticos: amoxicilina, amoxicilina-ácido clavulánico y azitromicina. Este dato se confirmó en 15 de las 17 UAP analizadas. Resaltar los valores bajos de uso de cefalosporinas (1,87%) penicilina V (1,62%), eritromicina (0,24%) y cloxacilina (0,07%).
| Tabla 2. Antibióticos prescriptos más frecuentemente | ||
|---|---|---|
| Antibiótico | Dispensaciones (N) | % |
| Amoxicilina | 36 811 | 64,61 |
| Amoxicilina + ácido clavulánico | 10 401 | 18,25 |
| Azitromicina | 5927 | 10,40 |
| Otros | 3835 | 6,73 |

Los antibióticos utilizados según la clasificación en subgrupos pueden verse en la Fig. 5. El 66,3% de la prescripción se realizó con penicilinas de primera línea, correspondiendo a la amoxicilina prácticamente la totalidad de este subgrupo (97%). La azitromicina supuso el 91% de los macrólidos utilizados.
DISCUSIÓN
La tasa de 465,34 episodios tratados con antibiótico por 1000 niños/año y una prevalencia antibiótica anual de 30,72% indica que la prescripción de antibióticos en niños en nuestra área es elevado en comparación con países clásicamente poco prescriptores como Holanda9,14,15 y Noruega8, pero resulta sensiblemente inferior, según los datos que disponemos, al que se da en otros puntos de España4,8,16 y en países del área mediterránea8,10,17. Nuestras cifras de dispensación antibiótica son también inferiores a estudios hechos en Alemania8,9,18 y similares a Gran Bretaña9,14,19.
La variación estacional de las dispensaciones en nuestra área muestra el perfil de prescripción elevado de antibióticos en procesos epidémicos del periodo invernal, de etiología vírica bien conocida. Grandes variaciones estacionales se relacionan con altos consumos de antibióticos9, pero no hemos encontrado estudios que cuantifiquen esa variabilidad en la edad pediátrica, que en nuestro caso fue del 32%.
Nuestros datos muestran una gran uniformidad de criterio entre los profesionales a la hora de la selección de antibióticos a utilizar, que podría indicar una alta adherencia a protocolos o guías clínicas.
Aunque el 66,3% de la antibioterapia se realizó con penicilinas de primera línea, los datos muestran un uso muy escaso de antibióticos de pequeño espectro como penicilina V y penicilinas antiestafilocócicas. Las dificultades para la administración oral de estos antibióticos (incompatibilidad con alimentos, mal sabor) son probablemente la causa principal de su desplazamiento por otros de espectro mayor. La utilización de amoxicilina-clavulánico y de cefalosporinas en nuestro caso es muy inferior a la que presentan otros estudios de ámbito estatal8,20.
Las diferencias significativas en la prescripción entre UAP vienen a corroborar los datos de otros estudios10,12 sobre la variabilidad en el uso de antibióticos, incluso en áreas geográficas muy pequeñas. La actitud prescriptora de los profesionales, a menudo condicionada por el manejo de la incertidumbre diagnóstica y las expectativas de los padres, probablemente es una de las causas más importantes de esa variabilidad12. Pensamos, como otros autores10,21, que el conocimiento por parte de los profesionales de las características de su prescripción y un enfoque más local de los planes de mejora en la prescripción antibiótica deberían ser un complemento imprescindible de medidas más generales.
En conclusión, presentamos el primer estudio de prescripción de antibióticos en niños en el País Vasco. Nuestras cifras de dispensación antibiótica presentan valores intermedios entre países de consumos altos y los poco prescriptores de Europa. Se constata una significativa uniformidad de criterio entre profesionales en la selección de antibióticos a utilizar y gran variabilidad en la cuantía de la prescripción entre unidades de Atención Primaria. La mayoría de la antibioterapia se realiza con penicilinas de primera línea, siendo muy escaso el uso de antibióticos de pequeño espectro. Conviene señalar algunas limitaciones del estudio que presentamos: nuestros datos subestiman la antibioterapia recibida por los niños, al carecer de datos del sector privado, y, por otra parte, no conocemos los diagnósticos que han motivado los tratamientos, limitando la valoración de la idoneidad de la prescripción de los antibióticos.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS
ATC: Anatomical, Therapeutic, Chemical Classification System · OSI: Organización Sanitaria Integrada · UAP: unidades de Atención Primaria.
AGRADECIMIENTOS
Grupo Lehen Arreta Pediatrikoa Miatzen (LAPM): Iñaki Ávalos Román (pediatra, CS de Ermua), Nahia Arantzamendi Artola (pediatra, CS de Ermua), Itziar Fernández Repaldiza (pediatra, CS de Durango), Esther Gorostiza Garai (pediatra, CS de Matiena), Isabel Molina Zelaia (pediatra, CS de Durango), Nekane Morato Rodríguez (pediatra, CS de Durango), Amaia San Sebastián Ruiz (médico de familia, CS de Elorrio), M.ª Jesús Sarrionandia Uribelarrea (pediatra, CS de Abadiño), Aranzazu Lorena Tajada Zabalbeitia (pediatra, CS de Durango) y Oihane Zubiaur Alonso (CS Berriz-Zaldibar). Vizcaya, España.
BIBLIOGRAFÍA
- Costelloe C, Metcalfe C, Lovering A, Mant D, Hay A. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096-3006.
- Chung A, Perera R, Brueggemann AB, Elamin AE, Harnden A, Mayn-White R. Effect of antibiotic prescribing on antibiotic resistance in individual children in primary care: Prospective cohort study BMJ. 2007;335:429-33.
- Blix HS, Engeland A, Litleskare I, Ronning M. Age- and gender-specific antibacterial prescribing in Norway. J Antimicrob Chemother. 2007;59:971-6.
- Lallana-Álvarez mj, Feja-Solana c, Armesto-Gómez J, Bjerrum L, Rabanaque-Hernández MJ. Prescripción extrahospitalaria de antibióticos en Aragón y sus diferencias por género y edad. Enferm Infecc Microbiol Clin. 2012;30:591-6.
- Bryant V, Timoner J, Oliva B, Gil M, Alegre P, de Abajo FJ. Análisis de la utilización de antibióticos en población pediátrica con patología respiratoria. Estudio en la base de datos BIFAP. Rev Pediatr Aten Primaria. 2009;11:s36-s36.
- Calvo C, Albañil MR, Sánchez M, Olivas A. Patrones de prescripción de antibióticos en Atención Primaria. ¿Usamos racionalmente los antibióticos en Pediatría? An Esp Pediatr. 2000;52:157-63.
- Cars O, Mölstad S, Melander A. Variation in antibiotic use in the European Union. Lancet. 2001;357:1851-3.
- Youngster I, Avorn J, Belleudi V, Cantarutti A, Díez-Domingo J, Kirchmayer U, et al. Antibiotic Use in Children - A Cross-National Analysis of 6 Countries. J Pediatr. 2017;182:239-44.
- Holstiege J, Schink T, Molokhia M, Mazzaglia G, Innocenti F, Oteri A, et al. Systemic antibiotic prescribing to paediatric outpatients in 5 European countries: a population-based cohort study. BMC Pediatr. 2014;14:174-83.
- Piovani D, Clavenna A, Cartabia M, Bonati M. The regional profile of antibiotic prescriptions in Italian outpatient children. Antibiotic Collaborative Group. Eur J Clin Pharmacol. 2012;68:997-1005.
- Vázquez ME, Pastor E, Bachiller MR, Vázquez MJ, Eiros JM. Variabilidad geográfica de la prescripción de antibióticos en la población pediátrica de Castilla y León durante el periodo 2001 a 2005. Rev Esp Quimioterap. 2006;19:342-8.
- Di Martino M, Lallo A, Kirchmayer U, Davoli M, Fusco D. Prevalence of antibiotic prescription in pediatric outpatients in Italy: the role of local health districts and primary care physicians in determining variation. A multilevel design for healthcare decision support. BMC Public Health. 2017;17:886-93.
- Indicadores clave del Sistema Nacional de Salud. En: Ministerio de Sanidad, Consumo y Bienestar Social [en línea] [consultado el 19/11/2020]. Disponible en http://inclasns.msssi.es/report/area/
- De Bie S, Kaguelidou F, Verhamme KM, De Ridder M, Picelli G, Straus SM, et al. Using Prescription Patterns in Primary Care to Derive New Quality Indicators for Childhood Community Antibiotic Prescribing. Pediatr Infect Dis J. 2016;35:1317-23.
- De Bont EG, van Loo IH, Dukers-Muijrers NH, Hoebe CJ, Bruggeman CA, Dinant GJ, et al. Oral and topical antibiotic prescriptions for children in general practice. Arch Dis Child. 2013;98:228-31.
- Serna MC, Ribes E, Real J, Galván L, Gascó E, Godoy P. Alta exposición a antibióticos en la población y sus diferencias por género y edad. Aten Primaria. 2011;43:236-44.
- Kourlaba G, Kourkouni E, Spyridis N, Gerber JS, Kopsidas J, Mougkou K, et al. Antibiotic prescribing and expenditures in outpatient paediatrics in Greece, 2010-13. J Antimicrob Chemother. 2015;70:2405-8.
- Holstiege J, Garbe E. Systemic antibiotic use among children and adolescents in Germany: a population-based study. Eur J Pediatr. 2013;172:787-95.
- Schneider-Lindner V, Quach C, Hanley JA, Suissa SJ. Secular trends of antibacterial prescribing in UK paediatric primary care. J Antimicrob Chemother. 2011;66:424-33.
- Vázquez Fernández ME, Luquero Alcalde FJ, Pastor García E, Bachiller Luque MR, Vázquez Fernández MJ, Eiros Bouza JM. Análisis del consumo de antibióticos en la población pediátrica de Castilla y León durante el periodo 2001 a 2005. An. Pediatr (Barc). 2007;67:11-7.
- Albañil Ballesteros MR, Calvo Rey C, Sanz Cuesta T. Variación de la prescripción de antibióticos en Atención Primaria. An Esp Pediatr. 2002;57:420-6.