Vol. 22 - Num. 86
Originales
Impacto en el consumo de antibióticos del test de diagnóstico rápido de Streptococcus pyogenes en Atención Primaria
M.ª Rosario Bachiller Luquea, M.ª Nazaret Sánchez Sierrab, Ana M.ª Ruiz San Pedroc, M.ª Ana Prado Prietoc, Tomás Maté Enríquezc, Laura Melero Guijarrod, José M.ª Eiros Bouzae
aPediatra. CS Pilarica Circular. Valladolid. España.
bCS Pilarica Circular . Valladolid. España.
cGerencia de Atención Primaria de Valladolid Este. Valladolid. España.
dMIR-Medicina Familiar y Comunitaria. CS Pintor Oliva. Palencia. España.
eGerencia de Atención Primaria Valladolid Oeste. Valladolid. España.
Correspondencia: MN Sánchez. Correo electrónico: nazaret91.ns@gmail.com
Cómo citar este artículo: Bachiller Luque MR, Sánchez Sierra MN, Ruiz San Pedro AM, Prado Prieto MA, Maté Enríquez T, Melero Guijarro L, et al. Impacto en el consumo de antibióticos del test de diagnóstico rápido de Streptococcus pyogenes en Atención Primaria. Rev Pediatr Aten Primaria. 2020;22:153-9.
Publicado en Internet: 25-05-2020 - Número de visitas: 18891
Resumen
Objetivos: analizar el empleo de los test de detección rápida de antígeno estreptocócico en Pediatría de Atención Primaria (AP), su impacto en la prescripción de antibióticos y la reducción de costes del tratamiento antibiótico.
Material y métodos: estudio descriptivo transversal, en menores de 15 años atendidos en AP, en 24 centros de salud, desde abril de 2017 hasta febrero de 2018. Se elaboró un protocolo de utilización del test de detección rápida de antígeno estreptocócico (TDRS). Se incluyeron pacientes con escala Centor mayor o igual a 2 puntos. Se extrajeron del sistema de facturación de recetas datos del número de dosis diaria definida (DDD) e importe de antibióticos en dicha temporada, comparándose con el gasto en los 12 meses previos.
Resultados: se realizaron 819 TDRS. Resultaron positivos 250 (30,5%), negativos 557 (68%) y 12 no valorables (1,5%). Se prescribió antibiótico al 33% de los pacientes (todos los positivos, 18 negativos, 3 no valorables). En 539 pacientes (97%) con resultado negativo no se instauró antibiótico. El número de DDD total disminuyó en 21 960 (12%), de las cuales 19 023 (86,6%) corresponden a los antibióticos más utilizados (penicilinas, amoxicilina, amoxicilina-clavulánico y azitromicina). La reducción económica fue de 11 320 € (12,5%) y el gasto en TDRS fue de 991 €, lo que supone un ahorro de 10 329€.
Conclusiones: la introducción del TDRS en consultas de Pediatría de AP ha permitido que se eviten un elevado número de tratamientos antibióticos. Su utilización ha demostrado ser eficiente en la optimización del consumo de antibióticos, consiguiendo reducir su utilización, evitar efectos adversos y reducir el gasto farmacéutico innecesario.
Palabras clave
● Streptococcus pyogenes ● Amigdalitis ● Análisis de costes ● Atención Primaria ● Evaluación de utilización de fármacos ● Kit de test diagnósticoINTRODUCCIÓN
La faringoamigdalitis aguda (FA) es una de las enfermedades más comunes en la infancia y supone hasta un 30% de las consultas pediátricas en Atención Primaria (AP)1,2. Predomina en países de clima templado, con picos de incidencia en invierno y primavera en el hemisferio norte. Se trata de una inflamación de las mucosas de la faringe o de las amígdalas faríngeas, en las que se puede observar la presencia de eritema, edema, exudados, úlceras o vesículas.
El origen generalmente es infeccioso, siendo en su mayoría de etiología vírica (40-80%), que cursa como un cuadro autolimitado y de evolución benigna3.
El estreptococo betahemolítico del grupo A (EbhGA) o Streptococcus pyogenes es la causa bacteriana más frecuente: es responsable de aproximadamente el 15-30% de los casos4. Suele presentarse en edades superiores a los tres años, y es raro a edades inferiores (6-10%). Sin embargo, algunos autores refieren una frecuencia en torno al 20% en menores de un año y alrededor del 26% entre los 2-3 años5,6 (posiblemente incluyan los portadores asintomáticos, hasta un 12% del total). Por ello, a pesar de su baja prevalencia, algunos estudios plantean que sería aconsejable realizar estudios diagnósticos, así como valorar tratamiento en caso preciso, de niños menores de tres años en contacto con casos de faringoamigdalitis por EbhGA en familiares o escolares, para reducir su diseminación y contagio7.
Más del 50% de los casos de FA con diagnóstico clínico reciben prescripción antibiótica de forma empírica4-8. Clásicamente se ha recomendado tratamiento antibiótico de las faringoamigdalitis por EbhGA para reducir la duración de los síntomas clínicos, evitar la transmisión y prevenir las complicaciones tanto supurativas como no supurativas8.
Sin embargo, la presentación clínica no es suficiente para discriminar entre la etiología vírica o bacteriana de una faringoamigdalitis9. Por ello, las pruebas diagnósticas pretenden establecer esas diferencias. La introducción de los test de detección rápida de antígeno estreptocócico (TDRS), fáciles de realizar en Atención Primaria, permite hacer un diagnóstico e inicio de tratamiento precoz con una alta especificidad, con lo que se podría reducir el uso innecesario de antibióticos.
Este estudio pretende analizar el efecto del empleo de los TDRS en consultas de Pediatría de Atención Primaria en el diagnóstico de faringoamigdalitis estreptocócica, su impacto en la decisión de prescripción de antibióticos y, principalmente, la reducción de costes del tratamiento antibiótico en estos pacientes.
MATERIAL Y MÉTODOS
Se realizó un estudio descriptivo transversal en 34 consultas de AP de 24 centros de salud del Área de Salud Este de Valladolid. El periodo de estudio fue desde abril de 2017 hasta febrero de 2018.
Se incluyeron todos aquellos pacientes con edad igual o inferior a 14 años atendidos en la consulta por cuadro clínico de FA de probable etiología estreptocócica. Para ello se aplicó la escala de Centor modificada por McIsaac (Tabla 1)10,11, recogiendo todos los casos que tuvieran una puntuación igual o superior a 2 puntos. Los criterios de exclusión fueron pacientes con puntuación inferior a 2 en escala de Centor, es decir, aquellos con bajo riesgo de presentar faringoamigdalitis estreptocócica, y segundas consultas por el mismo episodio.
| Tabla 1. Criterios de Centor modificados por McIsaac | |
|---|---|
| Parámetros | Puntuación |
| 1. Fiebre >38° | 1 |
| 2. Hipertrofia o exudado amigdalar | 1 |
| 3. Adenopatía laterocervical anterior dolorosa | 1 |
| 4. Ausencia de tos | 1 |
5. Edad:
|
1 0 |
Riesgo de infección por estreptococo (%)
|
|

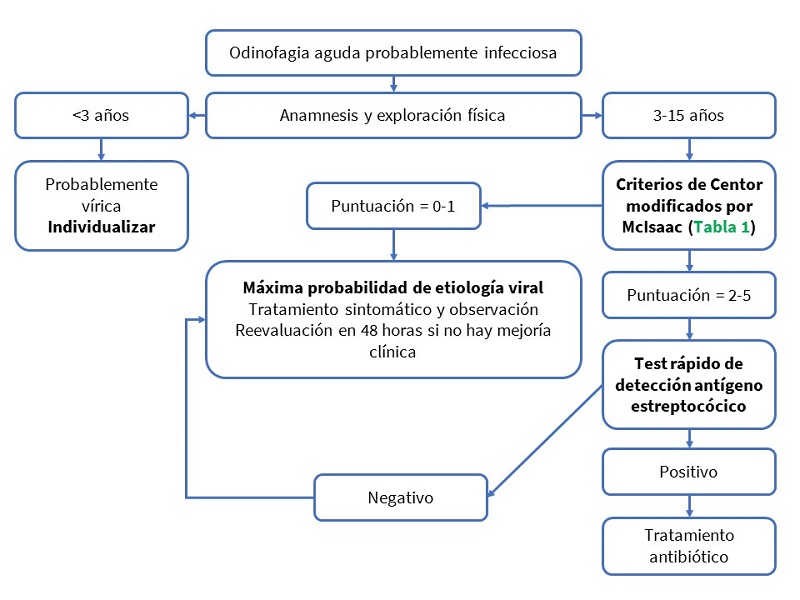
Se elaboró un protocolo de actuación (Fig. 1), basado en la edad y puntuación en la escala de Centor modificada por McIsaac, para seleccionar aquellos pacientes que se beneficiarían de la realización de TDRS, así como determinar la actitud terapéutica según el resultado de este.
Las semanas previas al inicio del estudio se realizaron jornadas de aprendizaje dirigidas en sesión general a todos los pediatras y profesionales de enfermería de AP y formación específica en consultas, con instrucciones por escrito acerca de los criterios de indicación, así como la técnica de realización correcta de los TDRS.
El proyecto fue aprobado por el Comité de Ética de Investigación del Área de Salud de Valladolid Este. Los pediatras, después de explicar a los familiares las características del estudio y obtenido el consentimiento informado, realizaban la valoración clínica e indicaban a enfermería la recogida de una muestra faringoamigdalar. Dicha recogida se llevaba a cabo frotando un hisopo en la pared posterior de la faringe y ambas amígdalas, incidiendo en las zonas más hiperémicas o con exudado, evitando tocar la lengua, úvula o cualquier otra parte de la boca, para evitar la contaminación de la muestra con microbiota saprofita del tracto respiratorio. Posteriormente se realizaba el TDRS mediante inmunocromatografía (Strep A MonlabTest). A los 15 minutos se obtenía el resultado y se actuaba en función de este siguiendo el protocolo (Fig. 1).
Las variables recogidas fueron: el sexo, la edad en años, el lugar de consulta, los síntomas o signos de FA, puntuación de escala de Centor modificada por McIsaac, aplicación del TDRS y resultados del mismo, la instauración de antibiótico y el tipo empleado.
Del sistema de facturación de recetas CONCYLIA del sistema de Sanidad de Castilla y León (SACYL), se extrajeron datos del número de dosis diaria definida (DDD) y el importe de antibióticos en Pediatría en dicha temporada, comparándose con el gasto en los 12 meses anteriores, desde abril de 2016 hasta marzo de 2017.
Se realizó un análisis descriptivo de las variables del estudio; para las variables cuantitativas se utilizó la media y la desviación estándar, describiendo las variables cualitativas mediante frecuencias absolutas y relativas (porcentajes).
RESULTADOS
Se reclutaron un total de 819 pacientes con clínica de faringoamigdalitis aguda y escala de Centor modificada por McIsaac igual o superior a 2 puntos. La edad media fue de 7,5 años (1-14). No hubo diferencias por sexo en la edad ni en la presentación de síntomas o signos.
Los síntomas y signos predominantes por los que consultaron fueron fiebre, odinofagia y exudado o hiperemia faríngea. Un 8% de los pacientes asociaban exantema escarlatiniforme. Otros síntomas menos frecuentes fueron: abdominalgia (1,5%), cefalea (1,2%) y vómitos (0,6%).
Se realizó TDRS a todos los pacientes. Los resultados obtenidos fueron: 250 positivos (30,5%), 557 negativos (68%) y 12 no valorables (1,5%). Un 4% de los TDRS realizados correspondía a pacientes con edad inferior a tres años. De estos, en el 17,5% el resultado fue positivo. El motivo principal por el que se aplicó el TDRS en este grupo de edad fue por presentación de exantema escarlatiniforme en más de la mitad de los casos (53%), seguido de exudado faringoamigdalar con fiebre y sin tos (32%) y síndrome febril sin foco (15%).
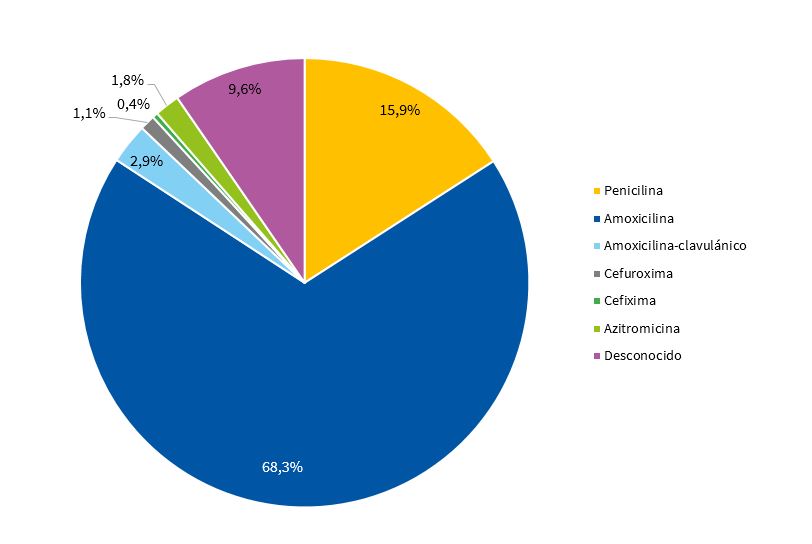
Se prescribió antibiótico a 271 pacientes (33,1%) que correspondían a todos aquellos que presentaron resultado positivo en el TDRS, 18 casos con resultado negativo (3,2%) y tres con TDRS no valorables (25%). En 539 pacientes (96,8%) con resultado negativo no se instauró tratamiento antibiótico. Los antibióticos utilizados se muestran en la Tabla 2 y en la Fig. 2.
| Tabla 2. Antibiótico prescrito | ||
|---|---|---|
| Antibiótico | Frecuencia | Porcentaje |
| Penicilina | 43 | 15,9% |
| Amoxicilina | 185 | 68,3% |
| Amoxicilina-clavulánico | 8 | 2,9% |
| Cefuroxima | 3 | 1,1% |
| Cefixima | 1 | 0,4% |
| Azitromicina | 5 | 1,8% |
| Desconocido | 26 | 9,6% |
| Total | 271 | 100% |

Todos los pacientes presentaron resolución completa tras completar el ciclo antibiótico, sin registrar complicaciones secundarias a dicha medicación.
Tras el análisis del sistema de facturación de recetas, se observó que el número de DDD total disminuyó en 21 960 (12%), con respecto al mismo periodo del año anterior, de las cuales 19 023 (86,6%) corresponden a los antibióticos más utilizados en FA (penicilinas, amoxicilina, amoxicilina-clavulánico y azitromicina).
La reducción en importe fue de 11 320 € (12,5%) y el gasto en TDRS fue de 991 €, lo que supone un ahorro de 10 329 € de gasto (11,4%) en nuestra área de salud.
DISCUSIÓN
Los TDRS son fáciles de realizar, permiten obtener el resultado en escasos minutos, a pie del paciente, e iniciar el tratamiento de forma individualizada y precoz. De esta forma se reducen los contagios, el absentismo escolar y, sobre todo, se optimiza el uso de antibióticos. Presentan una especificidad mayor o igual al 95% y una sensibilidad variable entre un 70 y un 90%12-18 en el diagnóstico de FA por EbhGA. Sus principales desventajas son que no permiten detectar otros serotipos y que un resultado negativo no nos permite descartar en todos los casos una infección por EbhGA. En aquellos casos en los que el TDRS es negativo, pero existe una alta sospecha de FA estreptocócica, podría ser útil el cultivo faríngeo19,20, ya que presenta una especificidad cercana al 99% y, si la recogida es correcta, puede tener una sensibilidad de hasta un 90-95%12,21. Aunque es un método más tardío (24-48 horas), tiene la ventaja de determinar diferentes bacterias y serotipos, así como establecer sensibilidad y resistencias antimicrobianas. Ninguna de las dos pruebas diagnósticas permite diferenciar entre FA por EbhGA o estado de portador. A pesar de ello, ante la baja prevalencia de portadores asintomáticos (entre un 6 y un 12%), no se recomienda de forma general el tratamiento antibiótico de estos pacientes3, tan solo en casos concretos11.
Con el fin de facilitar el diagnóstico de FA por EbhGA y seleccionar aquellos pacientes a los que se va a realizar algún tipo de prueba, se han propuesto varias escalas. Entre ellas la más utilizada es la escala de Centor modificada por McIsaac. Se basa en la presencia o ausencia de determinados criterios clínicos: fiebre >38 °C, exudado o hipertrofia amigdalar, adenopatía laterocervical anterior dolorosa, ausencia de tos; y pondera, a su vez, la edad. Presenta un alto valor predictivo negativo22, de tal manera que la probabilidad de un resultado positivo en las pruebas de diagnóstico microbiológico es ≤3% en los pacientes que no cumplen ninguno de los criterios clínicos, y de un 38-63% en los que reúnen 4 o 5 puntos19. Está indicado realizar algún tipo de prueba (TDRS o cultivo) en los casos que presenten puntuación mayor o igual a 2 puntos salvo en presencia de síntomas virales, donde se anularía dicha indicación23.
La introducción del TDRS en las consultas de Pediatría de Atención Primaria ha permitido que se eviten un elevado número de tratamientos antibióticos. Como se ha descrito anteriormente, el número de DDD total disminuyó en 21 960 (12%) de las cuales 19 023 (86,6%) corresponden a los antibióticos más utilizados en FA (penicilinas, amoxicilina, amoxicilina-clavulánico y azitromicina). Estos datos son concordantes con lo descrito en la literatura médica. En 2008, Maltezou et al.24 recogían que el uso de los TDRS supuso una reducción en la tasa de prescripción de antibióticos de un 61% en comparación con el manejo clínico de los pacientes. En 2016, Kose et al.25 observaron que el uso exclusivo de criterios clínicos en el diagnóstico de faringoamigdalitis estreptocócica suponía altas proporciones de prescripción de antibióticos (79,8%), que disminuían hasta un 42,6% al aplicar el TDRS.
Por tanto, el empleo de TDRS en este ámbito ha demostrado ser útil en la optimización del consumo de antibióticos, consiguiendo reducir su utilización a la vez que permite frenar el desarrollo de resistencias y efectos adversos evitables.
Otro aspecto que hay que destacar es que la utilización de los TDRS en AP permite reducir el gasto farmacéutico innecesario.
Phof et al.26 calcularon que el coste médico promedio por caso fue de 118 $ (58% del coste total). El coste de los antibióticos fue responsable del 20% (23,60 $). Kose et al.25 determinaron que el coste antibiótico del tratamiento empírico por paciente fue de 7,20 $ que disminuyó en un 76,4% (5,50 $) con la individualización de tratamiento tras el uso de TDRS. Considerando el coste del TDRS (el coste por paciente fue de 1,14 $), el valor del tratamiento por paciente disminuyó en un 60,6%.
En nuestro estudio, la reducción en importe fue de 11 320 € (12,5%) y el gasto en TDRS fue de 991 €, lo que supone un ahorro de 10 329 €.
Por todo lo expuesto, la utilización de los test de detección rápida de antígeno estreptocócico parece ser una medida eficiente y recomendable en las consultas de Pediatría de Atención Primaria.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
FINANCIACIÓN
Servicio de Farmacia de la Gerencia de Atención Primaria de Valladolid Este.
ABREVIATURAS
AP: Atención Primaria · DDD: dosis diaria definida · EbhGA: estreptococo betahemolítico del grupo A · FA: faringoamigdalitis aguda · TDRS: test de detección rápida de antígeno estreptocócico.
BIBLIOGRAFÍA
- García Vera C. Faringoamigdalitis estreptocócica en la infancia. FAPap Monogr. 2016;2:26-33.
- Kronman MP, Zhou C, Mangione-Smith R. Bacterial prevalence and antimicrobial prescribing trends for acute respiratory tract infections. Pediatrics. 2014;134:e956.
- Oliver J, Malliya Wadu E, Pierse N, Moreland NJ, Williamson DA, Baker MG. Group A Streptococcus pharyngitis and pharyngeal carriage: a meta-analysis. PLoS Negl Trop Dis. 2018;19;12:e0006335.
- Regueras G, Santos PM, Villa L, Pérez A, Arbesú E, Barreiro L, et al. Utilidad de una técnica antigénica rápida en el diagnóstico de faringoamigdalitis por Streptococcus pyogenes. An Pediatr (Barc). 2012;77:193-9.
- Tellechea AL, Salvo MG, Méndez JH, Cavagnaria B. Frecuencia del estreptococo betahemolítico del grupo A en las fauces de niños sintomáticos menores de 15 años según el grupo etario. Arch Argent Pediatr. 2012;110:516-9.
- Woods WA, Carter CT, Schlager TA. Detection of group A streptococci in children under 3 years of age with pharyngitis. Pediatr Emerg Care. 1999;15:338-40.
- Martí Fernández J, Gascón Casaredi I, Sandiumenge Durán M. Faringitis estreptocócica en niños menores de tres años. Algunas consideraciones. Rev Pediatr Aten Primaria. 2015;17:e125-8.
- Frost HM, Fritsche TR, Hall MC. Beta-hemolytic nongroup A streptococcal pharyngitis in children. J Pediatr. 2019;206:268-73.
- American Academy of Pediatrics. Group A streptococcal infections. En: Kimberlin DW, Brady MT, Jackson MA, Long SS (eds.). Red Book: 2018 Report of the Committee on Infectious Diseases. 31.ª ed. Itasca: American Academy of Pediatrics; 2018. p. 748.
- Roggen I, van Berlaer G, Gordts F, Pierard D, Hubloue I. Centor criteria in children in a paediatric emergency department: for what it is worth. BMJ Open. 2013;3:e002712.
- Piñeiro R, Hijano F, Álvez F, Fernández A, Silva JC, Pérez C, et al. Documento de consenso sobre el diagnóstico y tratamiento de la faringoamigdalitis aguda. An Pediatr (Barc). 2011;75:342.e1-13.
- Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan El, Lee G, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55:1279-82.
- Gieseker KE, Mackenzie T, Roe MH, Todd JK. Comparison of two rapid Streptococcus pyogenes diagnostic tests with a rigorous culture standard. Pediatr Infect Dis J. 2002;21:922-7.
- Gerber MA, Shulman ST. Rapid diagnosis of pharyngitis caused by group A streptococci. Clin Microbiol Rev. 2004;17:571-80.
- Tanz RR, Gerber MA, Kabat W, Rippe J, Seshadri R, Shulman ST. Performance of a rapid antigen-detection test and throat culture in community pediatric offices: implications for management of pharyngitis. Pediatrics. 2009;123:437-44.
- Lean WL, Arnup S, Danchin M, Steer AC. Rapid diagnostic tests for group A streptococcal pharyngitis: a meta-analysis. Pediatrics. 2014;134:771-81.
- Stewart EH, Davis B, Clemans-Taylor BL, Littenberg B, Estrada CA, Centor RM. Rapid antigen group A streptococcus test to diagnose pharyngitis: a systematic review and meta-analysis. PLoS One. 2014;9:e111727.
- Cohen JF, Bertille N, Cohen R, Chalumeau M. Rapid antigen detection test for group A streptococcus in children with pharyngitis. Cochrane Database Syst Rev. 2016;7:CD010502.
- McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE. Empirical validation of guidelines for the management of pharyngitis in children and adults. JAMA. 2004;291:1587-95.
- Dingle TC, Abbott AN, Fang FC. Reflexive culture in adolescents and adults with group A streptococcal pharyngitis. Clin Infect Dis. 2014;59:643-50.
- Gerber MA. Comparison of throat cultures and rapid strep tests for diagnosis of streptococcal pharyngitis. Pediatr Infect Dis J. 1989;8:820-4.
- Freer J, Ally T, Brugha R. Impact of Centor scores on determining antibiotic prescribing in children. Int J Health Care Qual Assur. 2017;30:319-26.
- Shapiro DJ, Lindgren CE, Neuman MI, Fine AM. Viral features and testing for streptococcal pharyngitis. Pediatrics. 2017;139:e20163403.
- Maltezou HC, Tsagris V, Antoniadou A, Galani L, Douros C, Katsarolis I, et al. Evaluation of a rapid antigen detection test in the diagnosis of streptococcal pharyngitis in children and its impact on antibiotic prescription. J Antimicrob Chemother. 2008;62:1407-12.
- Kose E, Sirin Kose S, Akca D, Yildiz K, Elmas C, Baris M, et al. The effect of rapid antigen detection test on antibiotic prescription decision of clinicians and reducing antibiotic costs in children with acute pharyngitis. J Trop Pediatr. 2016;62:308-15.
- Pfoh E, Wessels MR, Goldmann D, Lee GM. Burden and economic cost of group A streptococcal pharyngitis. Pediatrics. 2008;121:229-34.