Vol. 21 - Num. 83
Original Papers
Employment outcomes of residents of Paediatrics, 2014-2017 period
María Álvarez Casañoa, Pedro J. Gorrotxategi Gorrotxategib, Lourdes Castillo Camposc, Amaia Cámara Oteguid, Rocío Martín Moyae, Talía Fuentes Redondof, María Letona Luquig
aPediatra. CS Alcolea. Córdoba. España .
bPediatra. CS Pasaia San Pedro. Pasajes. Guipúzcoa. España.
cMIR-Pediatría. Hospital Clínica Benidorm. Benidorm. Alicante. España.
dMIR-Pediatría. Hospital Universitario Donostia. San Sebastián. Guipúzcoa. España.
eMIR-Pediatría. Hospital Materno-Infantil de Jaén. Jaén. España.
fMIR-Pediatría. Complejo Hospitalario de Toledo. Hospital Virgen de la Salud. Toledo. España.
gCAP de Usurbil. Usurbil. Gipuzkoa. España.
Correspondence: PJ Gorrotxategi. E-mail: pedro.gorrotxa@gmail.com
Reference of this article: Álvarez Casaño M, Gorrotxategi Gorrotxategi PJ, Castillo Campos L, Cámara Otegui A, Martín Moya R, Fuentes Redondo T, et al. Employment outcomes of residents of Paediatrics, 2014-2017 period. Rev Pediatr Aten Primaria. 2019;21:247-53.
Published in Internet: 06-09-2019 - Visits: 19987
Abstract
Introduction: given the shortage of paediatricians in the Spanish health care system and the high demand for them in primary care, where approximately 25% of positions are filled by non-specialists in paediatrics, we wanted to know the initial employment destination of residents who had finished his training period in the last 4 years.
Methods: analysed job placement outcomes of residents that completed their practical training in Spanish hospitals in the 2014-2017 period. We collected data through the members of medical resident committees in the different autonomous regions of Spain and the regional representatives of the Asociación de Pediatría de Atención Primaria.
Results: we collected data on the employment outcomes of 75.7% of the residents, which corresponded to the first destination of 1263 residents that completed their training in the past 4 years. In this period, the proportion that chose to work in primary care decreased from 30.77% to 24.5%, and there was also a decrease in employment in inpatient care units or outpatient hospital clinics from 43.8% to 32.85%, while the number that worked on-call and emergency care shifts increase, along with the proportion that entered the private medicine sector.
Conclusions: the percentage of residents whose destination is primary care is insufficient. The working conditions of paediatricians are getting worse, with an increase in contract work for on-call and emergency care shifts. The percentage of residents that seek employment in private medicine is increasing.
Keywords
● Employment opportunities ● Primary care ● ResidentsINTRODUCTION
For years, there has been a shortage of paediatrics in primary care. A proportion of the posts in primary care paediatrics are filled by physicians that are not specialised in paediatrics. This leads to delivery of unspecialised care at the primary level of care that could have repercussions in the management of children.1 The shortage has been estimated at approximately 30%,2 although a recent study calculated a proportion of 25.1%.3
In light of this situation, the Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics), its committee of medical residents and its professional working group set out to investigate the employment destinations of paediatric residents in recent years.
The project started in 2017 with the collection of data for the previous 3 years and was presented as a poster communication at the 65th Congress of the Asociación Española de Pediatría (Spanish Association of Paediatrics).4 We followed this initial analysis with the collection of follow-up data, 5 which we present in the current article.
RESULTS
We collected data on the first destination of 75.7% of the residents that finished their training period, corresponding to the employment destination of 1668 residents in the past 4 years (Table 1).
| Table 1. Proportions of medical residents for who we collected employment destination data | |||
|---|---|---|---|
| Year | Number of MIR positions | Number with available data | Percentage |
| 2014 | 419 | 278 | 66% |
| 2015 | 418 | 307 | 73% |
| 2016 | 413 | 331 | 80% |
| 2017 | 418 | 347 | 83% |
| TOTAL | 1668 | 1263 | 75.7% |

The proportion choosing primary care for employment in these years has decreased from 30.77% to 24.5% (by more than 6%); employment in inpatient care or hospital outpatient clinics has also decreased, in this case from 43.8% to 32.2% (by 11%), while employment in on-call and emergency shifts has increased: comparing the first 2 years to the last 2, by an average of 8.5%, as has employment in private medicine, which increased by 7%. When it came to the mean proportion for the entire 4-year period, the most frequent first destination was employment in inpatient care (37%), followed by primary care (28%) and emergency or on-call shifts (15.5%) (Table 2).
| Table 2. First destination of paediatrics residents from 2014 to 2017 | ||||||
|---|---|---|---|---|---|---|
| Primary care | Emergency, on-call shifts | Inpatient units | Training: masters. fellowships. etc. | Private medicine | Other | |
| 2014 | 30.77 | 8.36 | 43.81 | 2.34 | 3.01 | 4.68 |
| 2015 | 30.29 | 15.96 | 41.69 | 6.19 | 6.19 | 2.61 |
| 2016 | 26.20 | 23.79 | 30.42 | 10.84 | 3.01 | 5.12 |
| 2017 | 24.5 | 17.5 | 32.2 | 8.5 | 10.7 | 6.6 |
| Media | 27.94 | 15.50 | 37.03 | 6.97 | 5.73 | 4.75 |

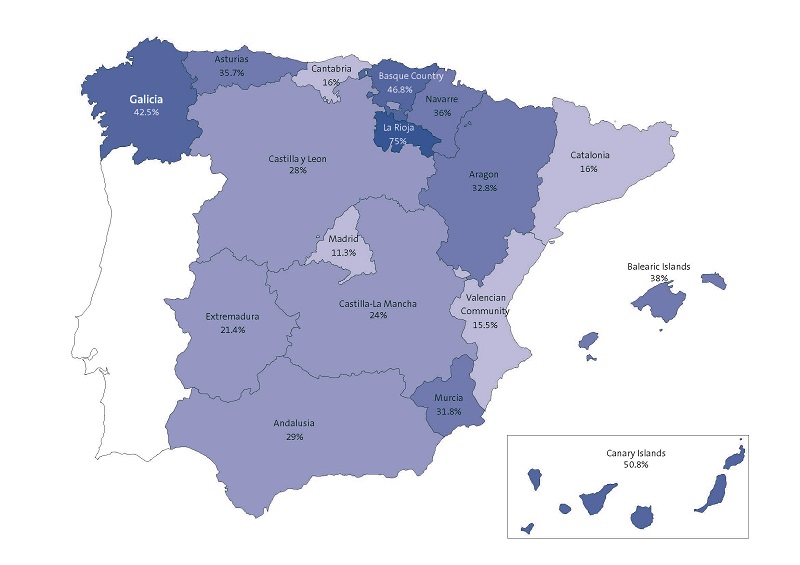
When it came to the employment in primary care by autonomous region in Spain, we found significant differences between regions, with the proportion ranging from 75% in la Rioja and 11.3% in Madrid, and a mean of 27.94% (Figure 1).
DISCUSSION
We will address three questions: Is there a demand for training in Paediatrics? Where is the demand for paediatricians higher, in hospitals or at the primary care level? And, could paediatric nurses contribute to solving this problem?
Is there a demand for training in the specialty of Paediatrics?
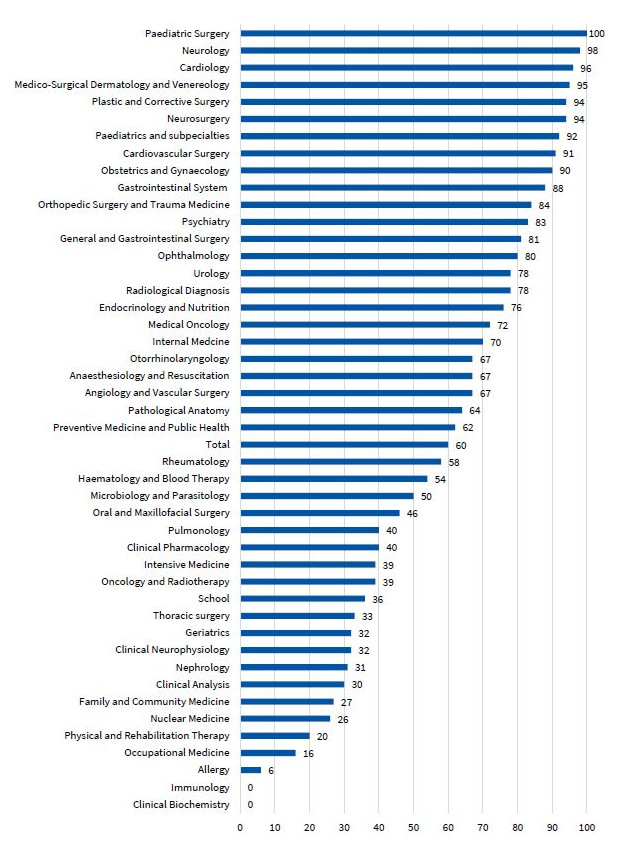
According to the descriptive report of the Medical Intern Resident (MIR) R1 Survey of 2014,6 the “placement system success” is defined as the percentage of applicants that were able to obtain a training spot in their preferred specialty. To calculate it, residents were asked which specialty and facility they would have chosen if they had not been limited by their scores, that is, if all positions and institutions had been available to them. In the case of Paediatrics, the success rate is of 92%, and there is a shortage of spots, as a higher percentage of residents would have chosen this speciality if there had been more spots available (Figure 2).
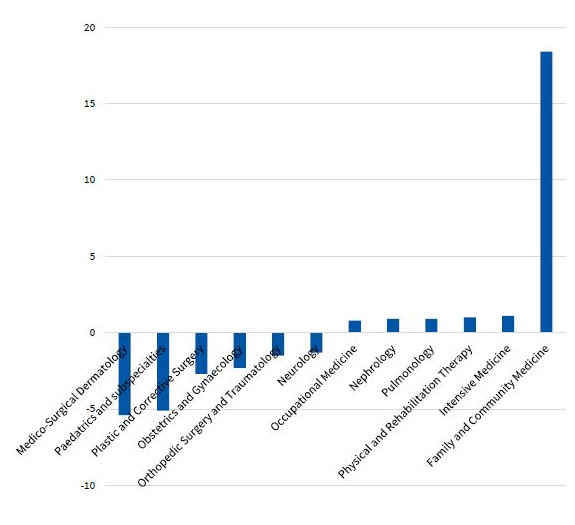
Another aspect we analysed was the difference between the desired positions and the selected positions. There are 5 specialties in which residents would have chosen more spots, and among them, the second with the greatest shortage of residency spots, with 5.1%, was Paediatrics (Figure 3), following only Dermatology, which is in highest demand, so that if more spots were offered, all positions would be filled while satisfying the wishes of the residents.
| Figure 3. Shortage-surplus: percent difference between the desired and the available medical residency (MIR) openings in 2013-2014 |
|---|
 |

Where the demand for paediatricians greater, in hospitals or in primary care?
To assess whether the employment destinations of residents fit the demand for paediatricians, we took into account the number of positions in each setting and the employment destinations observed in our sample. According to official data from 2016, in Spain there are 6410 paediatricians employed in primary care7 and 4154 in hospitals,8 corresponding to 60.7% and 39.3%, respectively. This contrasts with the first destinations of new paediatricians, which go in reverse: 52% stay in the hospital setting and 28% enter primary care, which means that the shortage of primary care paediatricians is getting worse.
In a nationwide survey of residents in Spain,9 75% reported that they thought they would work in primary care, with 43% expressing a desire to do so and 55% not minding working in this setting. The problems that they perceived in working in primary care were the low availability of diagnostic tests (30%), the excessive expectations of parents in cases of mild, common diseases (20%) and the wish to continue to do on-call shifts (20%).
There are also residents that are enthusiastic about primary care. One titled a presentation given in a meeting of the AEPap “El residente de Pediatría: entusiasmo por la Atención Primaria” (The paediatrics resident: a passion for primary care)10, and stated: “My enthusiasm may stem from the fact that we offer comprehensive care to patients and we can participate in their development and growth, tracking the progress of children in our caseload, knowing their individual and family characteristics, so that there is a deeper trust and mutual involvement in the doctor-patient relationship”.
Could paediatric nurses contribute to solve this problem?
Although in 2010 the curriculum for paediatric nursing was established and the professional category defined as “the autonomous delivery of specialised nursing services during childhood and adolescents at every level of care, including health promotion and neonatal care, care of the healthy or ill child or adolescent and rehabilitation services”,11 there are still few paediatric nurses in the Spanish national health care system.
Thus, some of the salient findings of a nationwide survey were that in Andalusia the role of nurses dedicated preferentially to children did not exist, while in Madrid paediatric nurses were only found in 40% to 50% of caseloads. In the Basque Country and Murcia the percentage continued to be low, between 50% and 70%. In Aragon, Castilla-La Mancha, Galicia, Extremadura, La Rioja, Navarre and Valencia it ranged from 70% to 90% and in Galicia it was 81%. In Navarre, most paediatric caseloads have a specific nurse assigned to them, except in some small towns where the nurse divides the time between paediatric and adult patients. And last of all, in Castilla y Leon, Catalonia, Balearic Islands, Canary Islands and Asturias, most paediatrics clinics (more than 90%) have on staff a nurse dedicated exclusively to paediatric patients.12 Thus, at present the contribution of nurses to specialised paediatric care is limited.
According to the 2016 report,13 the primary care system in Spain employs 34 888 physicians and 29 441 nurses. There should be 0.8 nurses per paediatrician in primary care, a ratio that is not met in most autonomous regions.
The number of spots available each year for paediatric nursing is approximately 130,14 with nurses gaining employment both in hospitals and primary care centres, which is clearly insufficient to meet the demand for specialised nurses.
There is also a discrepancy between the nurses that care exclusively for children (paediatric nursing) and nurses caring for adult patients as well (family/mixed-care nursing). In a study that included 34 nurses, 11 paediatricians and 1004 parents of children, 99.6% of surveyed parents reported preferring a nurse exclusively devoted to paediatric care. All paediatricians shared this opinion. When it came to the nurses, only 7 (20.6%) preferred a mixed-care model (family nursing), so it is fair to conclude that in this study, a majority of qualified professionals and of the general population preferred a specific paediatric nursing care model.15
CONCLUSIONS
The percentage of residents that is employed in primary care is insufficient. The quality of the work as a paediatrician is decreasing, with an increase in on-call and emergency shifts. The percentage of residents that seek employment in private health care is increasing.
The only solution to the problem of the deficit in paediatricians is to increase the number of slots for medical residency training (MIR) and, in the case of primary care, to make the openings in the field more attractive to residents that end their training in paediatrics and its subspecialties.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article. Preliminary findings on the collected data were presented as an oral communication in the 66th Congress of the Asociación Española de Pediatría, held in Zaragoza in June 6-9, 2018.
REFERENCES
- Buñuel Álvarez JC, García Vera C, González Rodríguez P, Aparicio Rodrigo M, Barroso Espadero D, Cortés Marina BR, et al. ¿Qué profesional médico es el más adecuado para impartir cuidados en salud a niños en Atención Primaria en países desarrollados? Revisión sistemática. Rev Pediatr Aten Primaria. 2010;12:s9-s72.
- Comité Ejecutivo de la AEP. Construyendo la Pediatría del futuro. In: Asociación Española de Pediatría [online] [accessed 03/09/2019]. Available at www.aeped.es/sites/default/files/noticiasaep/noticiasaep.62.3.pdf
- Gorrotxategi Gorrotxategi P, García Vera C, Graffigna Lojendio A, Sánchez Pina C, Palomino Urda N, Rodríguez Fernández-Oliva CR, et al. Situación de la Pediatría de Atención Primaria en España en 2018. Rev Pediatr Aten Primaria. 2018;20:e89-e104.
- Castillo Campos L, Gorrotxategi Gorrotxategi P, Cámara Otegi A, Muñoz Calonge A, Lasa Aransti A, Laka Iñurrategi A. ¿A dónde van los residentes cuando terminan su periodo de formación? In: 65.º Congreso de la AEP [online] [accessed 03/09/2019]. Available at www.congresoaep.org/AEP2017
- Álvarez Casaño M, Gorrotxategi Gorrotxategi P, Castillo Campos L, Martín Moya MR, Fuentes Redondo T. Salidas laborales de los residentes de Pediatría. Datos 2014-2017. In: 66.º Congreso de la AEP [online] [accessed 03/09/2019]. Available at www.congresoaep.org/AEP2018
- Grupo de Investigación EcoSalud de la Universidad de Las Palmas de Gran Canaria. Tercer Informe descriptivo de la encuesta MIR-R1. Convocatoria 2013-2014. In: Ministerio de Sanidad, Servicios Sociales e Igualdad [online] [accessed 03/09/2019]. Available at www.mscbs.gob.es/profesionales/formacion/necesidadEspecialistas/doc/ACT2015InforDesMIR_convocatoria_2013_14.pdf
- Portal Estadístico. Área de Inteligencia de Gestión. Sistema de Información de Atención Primaria (SIAP). In: Ministerio de Sanidad, Consumo y Bienestar Social [online] [accessed 03/09/2019]. Available at http://pestadistico.inteligenciadegestion.msssi.es/publicoSNS/comun/Cubo.aspx?IdNodo=6407
- Portal Estadístico. Sistema de Información de Atención Especializada (SIAE). Actualizado el 22/06/2018 -Datos desde 2010 en adelante. In: Ministerio de Sanidad, Consumo y Bienestar Social [online] [accessed 03/09/2019]. Available at http://pestadistico.inteligenciadegestion.msssi.es/publicoSNS/comun/Cubo.aspx?IdNodo=140
- Álvarez Casaño M, Castillo Campos L, Gorrotxategi Gorrotxategi P, García Uzquiano R, Igarzabal Irizar A, Berridi Etxeberria A. ¿Qué opinan los residentes de la rotación por Atención Primaria? In: 66.º Congreso de la AEP [online] [accessed 03/09/2019]. Available at www.congresoaep.org/AEP2018
- López García R. El residente de Pediatría: entusiasmo por la Atención Primaria. Rev Pediatr Aten Primaria. 2012;14:s71-6.
- Orden SAS/1730/2010, de 17 de junio, por la que se aprueba y publica el programa formativo de la especialidad de Enfermería Pediátrica. BOE 157 of June 29, 2010, pp. 57251 to 57276. Available at: www.boe.es/diario_boe/txt.php?id=BOE-A-2010-10365
- Sánchez Pina C, Palomino Urda N, de Frutos Gallego E, Valdivia Jiménez C, Rodríguez Fernández-Oliva CR, Miranda Berrioategortua I, et al. “Puntos negros” de la asistencia a la población infantojuvenil en Atención Primaria en España (primera parte). Rev Pediatr Aten Primaria. 2011;13:15-31.
- Informe anual del Sistema Nacional de Salud 2016. In: Ministerio de Sanidad, Servicios Sociales e Igualdad [online] [accessed 03/09/2019]. Available at www.msps.es/estadEstudios/estadisticas/sisInfSanSNS/tablasEstadisticas/InfAnualSNS2016/Resumen.pdf
- El EIR 2019 ya tiene propuesta oficial: estas son todas las plazas. In: Redacción Médica [online] [accessed 03/09/2019]. Available at www.redaccionmedica.com/secciones/formacion/el-eir-2019-ya-tiene-propuesta-oficial-estas-son-todas-las-plazas-8871
- García Callejo V, Domínguez Pérez L. Enfermería pediátrica versus Enfermería de familia; opiniones de los profesionales y los padres de los niños de San Sebastián de los Reyes (Madrid). Rev Pediatr Aten Primaria. 2012;14:27-30.