Vol. 20 - Num. 78
Originales
Influencia de los recursos especializados en cuidados paliativos pediátricos en los pediatras de Atención Primaria
Victoria Caballero Péreza, Manuel Rigal Andrésb, Sara Beltrán Garcíac, Fátima Parra Plantagenet-Whyted, M.ª Concepción Moliner Robredoe, Lorena Gracia Torralbaf, Claudia Orden Ruedag, Ricardo Javier Martino Albab
aPediatra. CS Cella. Teruel. España.
bUnidad de Cuidados Paliativos Pediátricos. Hospital Niño Jesús. Madrid. España.
cPediatra. CS Valdespartera. Zaragoza. España.
dUnidad de Cuidados Paliativos Pediátricos. Hospital Infantil Miguel Servet. Zaragoza. España.
eAsesora técnica. Diputación General de Aragón. España.
fPediatra. CS Torre Ramona. Zaragoza. España.
gServicio de Pediatría. Hospital de Alcañiz. Zaragoza. España.
Cómo citar este artículo: Caballero Pérez V, Rigal Andrés M, Beltrán García S, Parra Plantagenet-Whyte F, Moliner Robredo MC, Gracia Torralba L, et al. Influencia de los recursos especializados en cuidados paliativos pediátricos en los pediatras de Atención Primaria. Rev Pediatr Aten Primaria. 2018;20:133-42.
Publicado en Internet: 11-06-2018 - Número de visitas: 14156
Resumen
Introducción: el papel de los pediatras de Atención Primaria en el cuidado de niños con necesidades paliativas es fundamental. El objetivo del estudio es conocer la influencia que las unidades específicas de cuidados paliativos pediátricos tienen en la asistencia de los niños subsidiarios de los mismos por sus pediatras de Atención Primaria.
Método: se realizó un estudio transversal mediante el envío de una encuesta en línea a los pediatras de Atención Primaria del territorio español.
Resultados: se registraron 202 respuestas. El 68% nunca habían recibido formación específica en cuidados paliativos pediátricos. En aquellas provincias en las que existen recursos específicos de cuidado paliativos pediátricos, los profesionales de Atención Primaria muestran mayor predisposición para participar en las actividades propias de esta disciplina cuando sus pacientes lo precisen (media 4,37 frente a 3,89; p = 0,104) y han tenido más oportunidades de recibir formación sobre la materia (p = 0,007, OR: 2,18; IC 95: 1,24 a 3,84). Si hubiese una unidad de cuidados paliativos pediátricos accesible 24 horas por teléfono, el número de actividades potenciales en las que participarían es significativamente superior (p <0,001) (diferencia de medias 4,28; IC 95: 3,92 a 4,65).
Conclusiones: la existencia de recursos específicos de cuidados paliativos pediátricos con disponibilidad telefónica 24 horas tiene un impacto positivo en la disposición de los pediatras de Atención Primaria para participar en el plan de tratamiento de pacientes con necesidades paliativas. Para implementar los cuidados paliativos desde este ámbito es necesario reforzar los programas formativos.
Palabras clave
● Capacitación profesional ● Cuidados paliativos ● Encuestas y cuestionarios ● PediatrasINTRODUCCIÓN
Los cuidados paliativos pediátricos (CPP) constituyen la asistencia activa, continua y total al niño o adolescente afecto de una enfermedad que amenaza su vida. Dicha atención debe incluir a la familia como unidad de cuidado e implica la adaptación de la atención a la persona en su contexto y proyecto vital. El cuidado puede ser exclusivamente paliativo o combinado con tratamientos curativos (o dirigidos a modificar el curso de la enfermedad)1.
Se estima que en España cada año entre 5574 y 7432 niños pueden necesitar recursos específicos de CPP que den respuesta a sus necesidades2. Las enfermedades de los niños subsidiarios de CPP son infrecuentes y heterogéneas, por lo que suponen un auténtico reto para los profesionales que se ocupan de ellas. Además, a diferencia de los adultos, los niños se encuentran en continua evolución, lo que añade complejidad a la atención.
Por su parte, las familias no solo deben enfrentarse a la muerte prematura de sus hijos, sino a la necesidad de cuidado creciente, en ocasiones con gran dependencia de tecnología médica3. En un reciente estudio realizado en Holanda, en el que se han llevado a cabo entrevistas a padres cuyos niños padecen enfermedades con un pronóstico de vida limitado, concluyen que sus objetivos son: controlar los síntomas y la enfermedad en lo posible, que su hijo enfermo tenga una vida que merezca la pena vivir y mantener el equilibrio y las rutinas familiares. Para ello, concluyen que lo ideal es recibir los cuidados necesarios en el propio domicilio del paciente4.
Los cuidados domiciliarios influyen positivamente en la calidad de vida del paciente. Pero algunos factores, como la complejidad clínica o el agotamiento familiar, hacen inevitable los ingresos hospitalarios o la institucionalización de la atención, sobre todo si no existen recursos de CPP accesibles5.
El pediatra de Atención Primaria (AP), por su estrecha relación con el niño y su familia, establece una alianza personal y profesional difícil de igualar por otros sanitarios que tratan al niño de manera puntual. No obstante, el papel que juegan los equipos de AP en los CPP en España puede considerarse insuficiente6. La falta de recursos humanos, la gran demanda asistencial, así como la falta de formación en CPP podrían ser factores limitantes para desarrollarlos. Además, Davies et al.7 identificaron como barreras principales para la derivación a CPP desde AP la percepción de un conocimiento insuficiente de la materia, la falta de recursos específicos de CPP y de feedback sobre los pacientes previamente derivados.
Por todo ello, la relación entre los equipos de AP –más próximos a la familia– y los recursos de CPP –que aportan conocimientos específicos– merece ser estudiada. Un contacto fluido entre ambos ámbitos y la existencia de recursos de CPP específicos podría capacitar y motivar a los profesionales de AP a atender a pacientes con necesidades paliativas.
El objetivo del presente estudio es valorar la influencia de la existencia de recursos de cuidados paliativos pediátricos en la actividad asistencial y formación específica de los pediatras de Atención Primaria.
MATERIAL Y MÉTODOS
Se realizó un estudio transversal, descriptivo y analítico mediante la autocumplimentación de una encuesta estructurada anónima por pediatras de AP de todas las regiones de España que aceptaron participar en el estudio.
El cuestionario (Tabla 1) fue elaborado por la investigadora principal. El mismo explora la filiación de los participantes, medio de trabajo, relación con recursos de CPP regionales, formación específica recibida, conocimientos básicos de CPP y preferencias sobre la implicación en la asistencia a pacientes con necesidades paliativas. Para evaluar su validez y aceptabilidad se remitió la encuesta a tres pediatras de AP de diferentes provincias. En los tres casos contestaron que era adecuada tanto en la claridad como en la idoneidad de las preguntas.
| Tabla 1. Encuesta enviada a los pediatras de Atención Primaria |
|---|
Filiación:
|
| Número aproximado de niños incluidos en su cupo |
Recursos de cuidados paliativos pediátricos:
|
Formación:
|
| ¿Ha tenido la oportunidad de asistir a talleres, congresos o jornadas sobre los cuidados paliativos pediátricos en su provincia? |
| ¿Conoce usted que es la PedPal? |
| ¿Ha oído hablar alguna vez de la clasificación ACT, que determina qué pacientes son subsidiarios de recibir cuidados paliativos pediátricos? |
| ¿Sabe a qué nos referimos al hablar del punto de inflexión? |
Si algún niño de su cupo precisa cuidados paliativos se siente preparado para participar en su asistencia, mediante (selección múltiple):
|
| Si tuviese contacto directo con un equipo de cuidados paliativos pediátricos por vía telefónica las 24 horas del día, así como un plan de cuidado conjunto, ¿en qué actividades de las previas se atrevería a participar (selección múltiple)? |
| ¿Le gustaría recibir formación específica de CPP? En caso afirmativo, ¿qué temas serían?: atención integral/control sintomático/apoyo psicológico/apoyo espiritual/garantías sociales/todos ellos |
| ¿Le gustaría realizar una rotación en una Unidad de Cuidados Paliativos Pediátricos? En caso afirmativo, ¿durante cuánto tiempo? |

La distribución de la encuesta fue realizada a través de la plataforma Google Drive®. Se envió el enlace a los pediatras de AP a través de las sociedades de Pediatría de las comunidades autónomas y foros específicos. El estudio se desarrolló en mayo de 2017. Dado que los participantes podían recibir la encuesta por varias vías, se indicó que debía ser contestada una sola vez y se comprobó posteriormente, para controlar duplicados. Por las características del estudio, se consideró que la acción de responder a la encuesta implicaba un consentimiento para la participación en el mismo.
Análisis estadístico
Descriptivo: se calculó la distribución de frecuencias de los porcentajes de cada categoría para cada variable cualitativa. Las variables cuantitativas fueron exploradas con la prueba de conformidad de Kolmogorov-Smirnov. Por último, se calcularon indicadores de tendencia central y de dispersión.
Analítico: la asociación entre los factores estudiados y la existencia de recursos de CPP se investigó mediante pruebas de contraste de hipótesis. Se comprobó que todas las variables se ajustaban a una distribución normal por lo que solo fue necesario el uso de test paramétricos. Se utilizó la t de Student para variables cuantitativas. Las variables categóricas se estudiaron en forma de tabla de contingencia y la asociación fue explorada mediante prueba de χ2, sustituyéndose por el test exacto de Fisher si se cumple la condición. Para explorar la posible variación en las categorías antes-después de la existencia de CPP se utilizó el test de McNemar.
Se completó el análisis con la construcción de modelos de regresión logística binaria, tomando como variable dependiente la existencia de recursos específicos de CPP en su área de trabajo y covariables aquellas que presentaron diferencias estadísticamente significativas en los contrastes anteriores.
El análisis estadístico se realizó tomando como nivel de significación p<0,05 mediante el programa informático IBM® SPSS® Statistics 21 (SPSS Inc., Chicago, Ill).
RESULTADOS
Características de los participantes
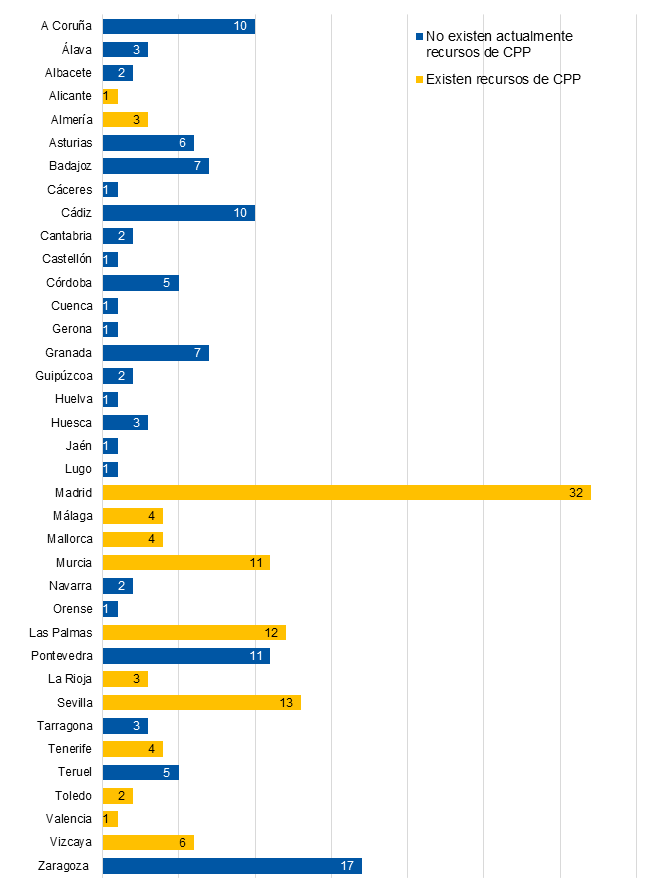
La encuesta la contestaron un total de 211 pediatras de AP. Se excluyeron del análisis nueve. En cuatro casos no se había rellenado la provincia de procedencia y en cinco había más de tres preguntas sin contestar. El tamaño muestral final fue de 202. La distribución de respuestas por provincia, así como si disponen de recursos de CPP, se observa en la Fig. 1.
| Figura 1. Distribución de las contestaciones en función de las provincias |
|---|
 |

El 75,2% de los participantes fueron mujeres. La edad media de los encuestados fue de 48,7 ± 9,9 años y la media de los años trascurridos desde que terminó el periodo formativo de la residencia 19,8 ± 10,3. El número medio aproximado de niños en el cupo fue 1067,5 ± 235,1. Con respecto a la localización del centro de salud, predominó el medio urbano (56,2%).
En la Tabla 2 se muestran las principales variables del estudio en función de si en la provincia donde ejercen su actividad profesional existe algún recurso de CPP. No se han encontrado diferencias estadísticamente significativas en la distribución de las principales características demográficas, el número de pacientes del cupo o la localización del centro de salud.
| Tabla 2. Comparación de las principales variables en función de la existencia de cuidados paliativos pediátricos en la región | |||
|---|---|---|---|
| Variable | Existencia CPP (n = 92) |
No existencia CPP (n = 110) |
p |
| Sexo (%) | |||
| Femenino Masculino |
69,6 30,4 |
80 20 |
0,102a |
| Edad (media años ± DE) | 50,6 (9,99) | 47,09 (9,73) | 0,805b |
| Años desde la finalización residencia (media años ± DE) | 21,63 (10,46) | 18,26 (9,96) | 0,504 b |
| Pacientes cupo (media número ± DE) | 1078,18 (207,4) | 1058,48 (256,7) | 0,272b |
| Localización centro salud (%) | |||
| Rural Urbano Mixto |
19,8 59,3 20,9 |
23,6 53,6 22,7 |
0,703a |
| Formación en CPP (%) | 31,8 | 30,4 | 0,879a |
| Asistencia jornadas/talleres (%) | 62,1 | 42,7 | 0,007a,* |
| Existencia PedPal (%) | 17,4 | 7,3 | 0,023a,* |
| Existencia grupos ACT (%) | 27,2 | 17,3 | 0,064a |
| Existencia punto inflexión (%) | 75,1 | 73,1 | 0,872a |
| Disposición a participar en actividades (%) | |||
| Visitas domiciliarias Control dolor AINE Control dolor opioides Tto. reagudizaciones respiratorias Tto. crisis convulsivas Tto. disnea en Oncología Tto. astenia en Oncología Apoyo psicológico Participación decisiones Sedación paliativa |
72,8 69,6 20,7 44,5 66,3 20,7 17,4 62,0 56,5 7,6 |
60,9 74,5 20,6 43,5 74,4 16,4 10 49,1 31,8 4,5 |
0,051a 0,264a 1,000a 0,888a 0,077a 0,469a 0,094a 0,045a,* 0,001a,* 0,267c |
| Número de actividades (media ± DE) | 4,37 (2,76) | 3,89 (2,49) | 0,104b |

De los profesionales que ejercen en provincias donde existen recursos de CPP, el 45,7% habían tenido contacto con estos por tener pacientes subsidiarios de los mismos. La patología más frecuente que habían atendido conjuntamente fue la parálisis cerebral (41,2%) y, en un 23,4% de los casos, niños con enfermedades oncológicas.
La frecuencia con la que habían recibido formación en CPP fue similar (en torno al 30%). En el caso de los profesionales que trabajaban en provincias con recursos de CPP la oportunidad de asistir a talleres o jornadas sobre este tema fue superior (p = 0,007, odds ratio [OR]: 2,18; intervalo de confianza del 95% [IC 95]: 1,24 a 3,84).
El 95% de los profesionales manifestaron su deseo de recibir formación en CPP, estando interesados en todos los temas propuestos (Tabla 1) el 77,3%. El 84,1% estarían dispuestos a rotar en un servicio específico de CPP durante un periodo de un mes.
Disposición a participar en la asistencia
Con respecto al deseo de participar en actividades relacionadas con los CPP, en todos los casos la proporción fue superior si existía recursos en la provincia, excepto en el control del dolor con el uso de antiinflamatorios no esteroideos (AINE) y el tratamiento de las crisis convulsivas. Se encontraron diferencias significativas en el caso del apoyo psicológico (p = 0,045; OR: 1,69; IC 95: 0,96 a 2,97) y la participación en la toma de decisiones (p = 0,001; OR: 2,79; IC 95: 1,57 a 4,95).
Se calcularon los porcentajes de participación potencial en las diferentes actividades en función de si había existido contacto previo o no con una unidad de CPP. Los resultados que se obtuvieron fueron similares, excepto el incremento de participación en visitas domiciliarias, que alcanzó significación estadística (p = 0,042; OR: 2,14; IC 95: 0,96 a 4,78) y la media del número de actividades potenciales fue superior (4,76 ± 2,46).
Posteriormente, se dio la opción de elegir en qué actividades participarían si hubiese una unidad de CPP en su provincia con la que existiese la opción de tener contacto telefónico 24 horas y la posibilidad de desarrollo de plan conjunto de cuidados. En todas las actividades se registró un gran incremento en la motivación a participar. Las mayores diferencias porcentuales se encontraron en el tratamiento del dolor con opioides, la disnea y astenia en niños con patología oncológica y la sedación paliativa ante síntomas refractarios (Tablas 3 y 4). Se determinó si existían factores que influyesen en el deseo de participación en la asistencia domiciliaria (Tabla 5). No se encontró asociación con la localización del centro de salud (urbano o rural), sexo, media de niños incluidos en el cupo, ni con si habían recibido formación específica en CPP (aunque sí que la proporción de profesionales que querían participar en la asistencia era superior si la habían recibido). Por otro lado, la edad media de los profesionales, así como el número de años que había trascurrido desde la finalización de la residencia en Pediatría fue superior en el caso de los facultativos que sí deseaban participar en las visitas domiciliarias (p <0,05).
| Tabla 3. Número de actividades asistenciales en las que participaría en función de existencia de unidad accesible 24 horas | ||||
|---|---|---|---|---|
| Variable | Sin unidad (media ± DE) n = 202 |
Con unidad (media ± DE) n = 202 |
Diferencia de medias (IC 95) |
p |
| Actividades asistenciales | 4,11 (2,62) | 8,40 (2,34) | 4,28 (3,92-4,65) | <0,001* |

| Tabla 4. Actividades asistenciales en que participaría en función de existencia de unidad accesible 24 horas | ||||
|---|---|---|---|---|
| Actividades asistenciales | Sin unidad | Con unidad | Diferencia porcentual | p |
| Visitas domiciliarias (%) | 66,3 | 91,6 | 25,6 | <0,001* |
| Control del dolor con AINE (%) | 72,3 | 92,6 | 20,3 | <0,001* |
| Control del dolor con opioides (%) | 20,8 | 79,7 | 58,9 | <0,001* |
| Tratamiento reagudizaciones respiratorias (IRA restrictiva; %) | 44,1 | 84,7 | 40,6 | <0,001* |
| Crisis convulsiva aguda (%) | 71,8 | 90,1 | 18,3 | <0,001* |
| Control disnea (Oncología; %) | 18,3 | 78,7 | 60,4 | <0,001* |
| Control astenia (Oncología; %) | 13,4 | 82,2 | 68,8 | <0,001* |
| Apoyo psicológico familiar (%) | 55,0 | 84,2 | 29,2 | <0,001* |
| Toma de decisiones (%) | 43,1 | 83,7 | 40,6 | <0,001* |
| Sedación paliativa (%) | 5,9 | 72,3 | 66,4 | <0,001* |

| Tabla 5. Factores que influyen en la asistencia domiciliaria | ||||
|---|---|---|---|---|
| Variable | Visita domiciliaria | p | ||
| Sí (n = 134) | No (n = 68) | |||
| Edad (media años ± DE) | 49,23 (9,98) | 46,23 (9,59) | 0,009a* | |
| Años desde la finalización residencia (media años ± DE) | 21,14 (10,43) | 17,15 (9,58) | 0,013a* | |
| Pacientes cupo (media número ± DE) | 1070,24 (196,05) | 1061,98 (299,25) | 0,813a* | |
| Sexo (%) | Mujer | 65,8 | 34,2 | 0,964b |
| Hombre | 68 | 32 | ||
| Localización centro salud (%) | Rural | 67,0 | 33 | 0,468b |
| Urbano | 65,5 | 34,5 | ||
| Formación específica en CPP (%) | Sí | 96,8 | 3,2 | 0,071b |
| No | 89,2 | 10,8 | ||

Necesidades de formación
La proporción de profesionales que conocía qué es la Sociedad Española de Cuidados Paliativos Pediátricos (PedPal) y los grupos ACT (clasificación internacional propuesta para los niños subsidiarios de CPP por la Asociación para Niños con Situaciones que Amenazan la Vida o en Situación de Terminalidad y sus Familias) no sobrepasó en ninguna cohorte el 30%. En ambas variables, la proporción fue superior en el grupo en el que existen CPP en la provincia, con un nivel de significación de 0,023 en el caso del conocimiento de la PedPal (OR: 2,68; IC 95: 1,09 a 6,59) y de un 0,064 para los grupos ACT (OR: 1,79; IC 95: 0,91-3,51).
Ante la pregunta de qué pacientes son el grueso que se asiste en las unidades de CPP, la mayor parte de los pediatras contestaron que niños con patología oncológica. Si consideramos que la respuesta correcta sería la patología de tipo neurológica –estática o degenerativa–, el porcentaje de aciertos en el grupo que cuenta como un recurso de CPP sería de un 38%, frente a 28,4% en caso de que no (p = 0,149).
DISCUSIÓN
Los facultativos que ejercen en AP constituyen una pieza clave dentro del proceso asistencial, ya que conocen al niño desde su nacimiento, así como la trayectoria completa de la enfermedad. Goldstein et al.8 mostraron las percepciones de los padres sobre la implicación de los profesionales en el cuidado de sus hijos gravemente enfermos. Aunque los pediatras de AP se mantuvieron informados sobre la situación del niño, no participaron en procesos importantes como la toma de decisiones al final de la vida. No obstante, son pocos los estudios realizados que se interesan por el sentir de los pediatras de AP acerca de los CPP, y ninguno que abarque diferentes áreas de la geografía española.
Aunque la realización de investigaciones mediante encuestas en línea supone asumir sesgos como el de participación y respuesta, constituye una forma efectiva de llegar a profesionales de diferentes comunidades autónomas, algo importante para el desarrollo del objetivo del presente estudio.
Este trabajo muestra que la existencia de una unidad de CPP tiene un impacto positivo en la disposición de los pediatras de AP a participar en el plan de tratamiento de pacientes con necesidades paliativas. En términos generales, se muestran inseguros hacia la asunción de actividades que son características de esa disciplina: menos de la mitad se reconocen capaces de tratar el dolor intenso o la astenia y disnea de origen tumoral, por ejemplo. En todos los casos, la proporción de pediatras que desearía implicarse en estas actividades fue superior si existían recursos de CPP en la provincia.
El control del dolor con opioides y la sedación paliativa ante síntoma refractario suscitaron un bajo deseo de participación. El manejo de los opioides no es usual entre los pediatras de AP y muy pocos tienen acceso a recetarios de estupefacientes. En un trabajo realizado en Alemania, mediante encuestas dirigidas a pediatras de AP, concluían que el control del dolor no estaba bien resuelto en muchos de sus pacientes que se encontraban en final de vida, por lo que era necesario el asesoramiento por especialistas expertos9. La sedación paliativa es uno de los procedimientos al que los pediatras están menos acostumbrados. Además de los conocimientos farmacológicos, se ponen en juego otros factores que en ocasiones dificultan dar la mejor respuesta posible al sufrimiento del niño y su familia. Por un lado, la influencia mediática que en ocasiones impide el discernimiento entre conceptos como eutanasia, suicidio asistido y sedación paliativa y, por otro lado, la creencia de que la sedación acorta la vida. Mientras que para la primera son necesarias medidas educativas poblacionales sobre legalidad y derechos del paciente, la segunda exige una comunicación abierta con la familia, ofreciendo las diferentes opciones posibles basándonos en la mejor evidencia científica5. Sobre este aspecto, existen diversos estudios y revisiones sistemáticas en los que se demuestran incluso supervivencias superiores en aquellos pacientes que fueron sedados bajo estricto criterio médico frente a los que no lo fueron10,11.
La toma de decisiones al final de la vida es referida por padres y profesionales como uno de los procesos más difíciles a los que tienen que enfrentarse12. Anteriormente se ha citado un trabajo en el que la percepción de los padres era que sus pediatras de AP no habían participado en este proceso8, mientras que otros estudios refieren que una relación terapéutica larga con el profesional lo facilita, ya que asegura el conocimiento multidisciplinar de la persona, y no solo de la enfermedad13. Si existe una relación de confianza estrecha entre la familia y su pediatra de AP, este debería participar y acompañar a la familia en este duro trance. Para ello, deben existir adecuados cauces de información con Atención Especializada (Oncología Pediátrica, Neuropediatría…), así como recursos de CPP, que integren a sus pediatras en el proceso asistencial.
Con respecto a los factores que influyen en la voluntariedad de llevar a cabo visitas a domicilio, los pediatras con más experiencia mostraron mayor predisposición. En una reciente publicación del Ministerio de Sanidad, Servicios Sociales e Igualdad, los índices de participación más bajos en cuanto a visitas domiciliarias se encuentran en el ámbito de la Pediatría14. Sin embargo, en lo que a los cuidados paliativos se refiere, debería integrarse como una actividad más. Para ello, los profesionales deben disponer del tiempo necesario y la posibilidad de tener contacto telefónico 24 horas con una unidad especializada en CPP como recoge el documento Cuidados paliativos pediátricos en el Sistema Nacional de Salud: criterios de atención2.
Según nuestro trabajo, en aquellas áreas en las que se cuenta con dispositivos de CPP la posibilidad de asistir a jornadas formativas es superior. Este hecho es acorde con el documento IMPaCCT publicado por la Asociación Europea de Cuidados Paliativos, que aboga por que todos los profesionales que atienden niños tengan acceso a formación en CPP y, por otra parte, que los recursos específicos de CPP impartan enseñanza reglada sobre esta materia15.
Un dato llamativo es que pocos profesionales conocen la existencia de la PedPal, que se enmarca en la Asociación Española de Pediatría. Podría ser debido a que es una sociedad de reciente creación. No obstante, dentro de sus estatutos está incluida la educación en cuidados paliativos en el ámbito de la Pediatría y para ello es importante llevar a cabo una correcta difusión de su existencia16.
Por otra parte, existe un grado de desconocimiento general sobre qué pacientes son subsidiarios de CPP, lo que coincide con la literatura médica17. Es más sencillo reconocer a aquellos niños que se encuentran en la fase de final de vida de forma secundaria a una enfermedad oncológica que aquellos que sufren parálisis cerebral o alteraciones cromosómicas. Esta situación podría subsanarse si hubiese mayor difusión de los grupos ACT que, aunque con limitaciones, da una información clara sobre las enfermedades amenazantes para la vida y por tanto, subsidiarias de CPP.
En esta encuesta queda manifiesto la deficiente formación recibida en CPP de los médicos españoles, algo que contrasta con el deseo de aprender e implicarse de los pediatras, tal como se ha visto en estudios previos6. Es necesario un esfuerzo importante para integrar los cuidados paliativos pediátricos en los programas formativos de pregrado y posgrado, así como la promoción de cursos y jornadas.
CONCLUSIONES
La existencia de recursos específicos de CPP incrementa las posibilidades de formación del resto de profesionales, da difusión a conceptos importantes y fomenta la participación de los responsables iniciales de los niños en el proceso asistencial. Además, el desarrollo de programas de CPP en el marco de una sociedad de ámbito nacional como la PedPal, promueve la creación de una red de asistencia que favorezca el intercambio de experiencia e información entre profesionales de diferentes disciplinas que se traduzca en un incremento de la calidad asistencial.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS
ACT: clasificación internacional propuesta para los niños subsidiarios de CPP por la Asociación para Niños con Situaciones que Amenazan la vida o en Situación de Terminalidad y sus Familias • AINE: antiinflamatorios no esteroideos • AP: Atención Primaria • CPP: cuidados paliativos pediátricos • IC 95: intervalo de confianza del 95% • OR: odds ratio • PedPal: Sociedad Española de Cuidados Paliativos Pediátricos.
BIBLIOGRAFÍA
- Chambers L, Dodd W, McCulloch R, McNamara K. A guide to the development of children’s Palliative Care Services. Bristol: Association for Children’s Palliative Care, 2009.
- Martino Alba R, Catá del Palacio E, Hernández García P, Muñoz Mellado A. Cuidados paliativos pediátricos en el Sistema Nacional de Salud: criterios de atención. En: Ministerio de Sanidad, Servicios Sociales e Igualdad [en línea] [consultado el 31/05/2018]. Disponible en www.msps.es/organizacion/sns/planCalidadSNS/pdf/01-Cuidados_Paliativos_Pediatricos_SNS.pdf
- Gimeno Sánchez I, Muñoz Hiraldo ME, Martino Alba RJ, Moreno Villares JM. Atención específica para los niños con complejidad médica en España: buscando el mejor modelo. An Pediatr (Barc). 2016;85:56-7.
- Verberne LM, Kars MC, Schouten-van Meeteren AY, Bosman DK, Colenbrander DA, Grootenhuis MA, et al. Aims and tasks in parental caregiving for children receiving palliative care at home: a qualitative study. Eur J Pediatr. 2017;176:343-54.
- García Salido A, Monleón Luque M, Barceló Escario M, del Rincón Fernández C, Catá del Palacio E, Martino Alba R. Retirada de asistencia respiratoria en domicilio: toma de decisiones en cuidados paliativos pediátricos. An Pediatr (Barc). 2014;80:181-3.
- Astray San Martín A. Encuesta sobre cuidados paliativos a pediatras de Atención Primaria en un área sanitaria de Madrid. Rev Pediatr Aten Primaria. 2010;12:33-40.
- Davies B, Sehring S, Partridge J. Barriers to palliative care for children: perceptions of pediatric health care providers. Pediatrics. 2008;121:282-8.
- Goldstein R, Rimer KP. Parents’ views of their child's end-of-life care: subanalysis of primary care involvement. J Palliat Med. 2013;16:198-202.
- Kremeike K, Eulitz N, Jünger S, Sander A, Geraedts M, Reinhardt D. Paediatric palliative home care in areas of Germany with low population density and long distances: a questionnaire survey with general paediatricians. BMC Res Notes. 2012;5:498.
- Barathi B, Chandra PS. Palliative Sedation in advanced cancer patients: does it shorten survival time? - A systematic review. Indian J Palliat Care. 2013;19:40-7.
- Maltoni M, Pittureri C, Scarpi E, Piccinini L, Martini F, Turci P, et al. Palliative sedation therapy does not hasten death: results from a prospective multicenter study. Ann Oncol. 2009;20:1163-9.
- Martino Alba R. Cuidados paliativos pediátricos: teniendo en cuenta al niño, a las familias y a los profesionales. Evid Pediatr. 2012;8:1.
- Zaal-Schuller IH, Willems DL, Ewals FV, van Goudoever JB, de Vos MA. How parents and physicians experience end-of-life decision-making for children with profound intellectual and multiple disabilities. Res Dev Disabil. 2016;59:283-93.
- Dirección General de Salud Pública (2015). Actividad asistencial ordinaria AP 2015. EN: Ministerio de Sanidad, Servicios Sociales e Igualdad [en línea] [consultado el 04/06/2018]. Disponible en www.msssi.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SIAP/Act_ord_AP_2015.pdf
- Comité de expertos del grupo de trabajo EAPC. IMPaCCT: estándares para cuidados paliativos pediátricos en Europa. Med Pal (Madrid). 2008;15:175-80.
- PedPal, Sociedad Española de Cuidados Paliativos Pediátricos. Estatutos, 2016. Disponible en www.pedpal.es/site/wp-content/uploads/2016/10/Estatutos-Pedpal.pdf
- Jünger S, Vedeer AE, Milde S, Fischbach T, Zernikow B, Radbruch L. Paediatric palliative home care by general paediatricians: a multimethod study on perceived barriers and incentives. BMC Palliat Care. 2010;9:11.





