Vol. 18 - Num. 71
Originales
Hallazgos clínicos inusuales en un brote de escarlatina
Verónica Fernández Romeroa, Isabel Rodríguez Sáncheza, Gema Gómez Fernándezb
aPediatra. CS Vélez-Sur. UGC de Pediatría y Neonatología Málaga-Este Axarquía. Málaga. España.
bMédico de Familia. CS Vélez-Sur.UGC Vélez-Málaga Sur. Área de Gestión Sanitaria Este de Málaga Axarquía. Málaga. España.
Correspondencia: V Fernández. Correo electrónico: veronicafernandez565@gmail.com
Cómo citar este artículo: Fernández Romero V, Rodríguez Sánchez I, Gómez Fernández G. Hallazgos clínicos inusuales en un brote de escarlatina. Rev Pediatr Aten Primaria. 2016;18:231-41.
Publicado en Internet: 12-09-2016 - Número de visitas: 98178
Resumen
Introducción: la escarlatina es una enfermedad infecciosa producida por Streptococcus pyogenes que produce un cuadro característico de faringoamigdalitis y exantema. Su diagnóstico suele ser fácil, pero los casos atípicos pueden pasar desapercibidos o ser confundidos con otros cuadros.
Pacientes y método: estudio descriptivo retrospectivo de los casos de escarlatina en la población pediátrica adscrita a un centro de salud en la temporada 2013/2014. Describimos la epidemiología, las características clínicas, las pruebas microbiológicas, el tratamiento y la presencia de recidivas.
Resultados: se obtuvieron 91 casos, resultando una incidencia de 3,2%, de los que 76 fueron confirmados microbiológicamente con test rápido o cultivo. La edad media fue 4,15 años. Los principales motivos de consulta fueron “fiebre y dolor de garganta” y “fiebre y erupción cutánea”. Las alteraciones faríngeas más frecuentes fueron la hiperemia y petequias en paladar, y en pocos pacientes se encontró exudado amigdalar. Casi un 40% de pacientes tenían síntomas catarrales, 71 pacientes presentaban un exantema típico, y 20 uno atípico. La mayoría se trató con amoxicilina o penicilina durante diez días; 15 pacientes tuvieron recidivas.
Conclusiones: de los datos obtenidos destacan el gran número de casos, la presencia de síntomas catarrales y la poca frecuencia de exudado amigdalar. Fue llamativa la variabilidad de los exantemas con hallazgos como eritrodermia extensa, urticaria, exantema macular, petequias en localizaciones atípicas y edema facial y de miembros. El test rápido en Atención Primaria permite, por su utilidad, el diagnóstico de casos dudosos.
Palabras clave
● Streptococcus pyogenes ● Escarlatina ● Exantema ● Niños ● Test de detección rápidaINTRODUCCIÓN
La escarlatina es una enfermedad causada por la infección del Streptococcus pyogenes del grupo A (EGA) productor de exotoxinas pirogénicas (antes llamada toxinas eritrogénicas) en individuos que no disponen de anticuerpos antitoxina. Es una infección de la vía respiratoria superior que se asocia con un exantema característico1.
Los niños con escarlatina no tratada diseminan el EGA a través de las gotitas de saliva de la vía respiratoria y de las secreciones nasales, aunque se han documentado casos de transmisión por alimentos y fómites. La transmisión se ve favorecida por el contacto estrecho, y por tanto las guarderías, colegios y el hogar constituyen ambientes de importante diseminación1-3.
El periodo de incubación es de dos a cinco días. Los niños dejan de ser infectivos en general 24 horas después del inicio del tratamiento antibiótico adecuado, aunque recientemente se ha publicado que 12 horas pueden ser suficientes. Los portadores faríngeos crónicos del EGA rara vez transmiten ese organismo a los demás1,4.
En numerosos textos clásicos y algunos artículos se considera que la escarlatina es actualmente poco frecuente; sin embargo, numerosas publicaciones refieren un aumento de casos en los últimos años. Su incidencia es cíclica y depende de la prevalencia de las cepas productoras de toxinas y del estado inmunitario de la población, siendo mayor en niños de 5 a 15 años, especialmente en los escolares más jóvenes, pero no es excepcional en otras edades1,5,6.
Clásicamente la clínica se ha descrito como sigue. La exploración faríngea muestra hallazgos similares a la faringitis estreptocócica. La lengua suele presentar papilas engrosadas que le dan un aspecto blanquecino (lengua saburral) y posteriormente las papilas se tornan enrojecidas (lengua en fresa). El exantema aparece a las 24-48 horas tras el inicio de los síntomas, pero también puede ser el signo inicial. Se trata de una erupción difusa, eritematosa, papular, que produce una coloración roja intensa de la piel que se blanquea a la presión y la piel se vuelve áspera al tacto (piel de lija). En general es más intensa a lo largo de los pliegues (líneas de Pastia) y respeta el triángulo nasogeniano, lo que da aspecto de palidez perioral (fascies de Filatov). Al cabo de los 3-4 días el exantema empieza a apagarse y le sigue una ligera descamación1,7.
La escarlatina típica no resulta difícil de diagnosticar; sin embargo, hay formas de presentación atípicas con hallazgos que la hacen más difícilmente reconocible y en las que es necesario realizar un diagnóstico diferencial con otras enfermedades. En caso de duda, la identificación del EGA en la faringe ayuda al diagnóstico1,7-11.
Las complicaciones son las mismas que las de la faringoamigdalitis, las precoces son supurativas, como otitis media, absceso faríngeo y sinusitis, y las tardías, no supurativas, glomerulonefritis y fiebre reumática7.
La escarlatina es una enfermedad que puede acontecer más de una vez en la vida de un individuo, debido a la existencia de varios linajes genéticos del EGA que dan lugar a diversas toxinas pirogénicas5, 9,11-14.
PACIENTES Y MÉTODO
Estudio descriptivo retrospectivo de los casos diagnosticados de escarlatina en el periodo comprendido entre el 1 de septiembre de 2013 (semana 35 de 2013) al 31 de agosto de 2014 (semana 35 de 2014).
El ámbito de estudio se situó en el municipio de Vélez-Málaga (España). La población que se estudió fueron los niños y niñas entre 0 y 13 años, adscritos durante este periodo a dos cupos de Pediatría del centro de salud Vélez-Sur. La población estudiada asiste a distintos centros educativos del municipio. El número total de usuarios obtenido de la base de datos del Sistema Andaluz de Salud en este rango de edad fue de 2852 que son el total de pacientes de los dos cupos.
Se incluyeron como casos a los pacientes que se diagnosticaron de escarlatina. Se estableció como definición de caso confirmado aquel que cumplía criterios clínicos (faringoamigdalitis y exantema) además de confirmación microbiológica y como caso probable aquel que solo tenía clínica compatible.
La búsqueda de los casos se realizó a través de la historia de salud digital del sistema de información Diraya del Sistema Sanitario Público de Andalucía.
Se evaluaron: el número de casos, el sexo, la edad de presentación, la distribución por meses y semanas y su expresión clínica (tanto signos y/o síntomas relatados en la anamnesis como hallazgos a la exploración física), así como las recidivas. Se consideró la realización de test microbiológicos y el tratamiento administrado.
Como prueba microbiológica principal se utilizó el test rápido OSOM® Strep A Test Genzyme sobre exudado faríngeo (Leti diagnóstica®) que según distintos estudios tiene una sensibilidad del 85-95%, especificidad del 92-98%, valor predictivo positivo 80-91% y valor predictivo negativo 95-98%15-18. Solo en algunos pacientes se realizó cultivo.
RESULTADOS
Se obtuvieron 91 casos, lo que corresponde a una incidencia sobre la población de estudio de un 3,2% (91/2852) en el periodo estudiado.
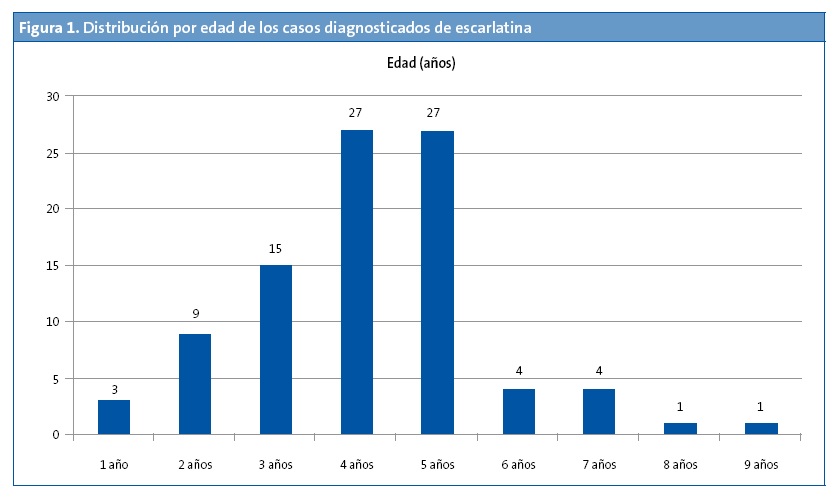
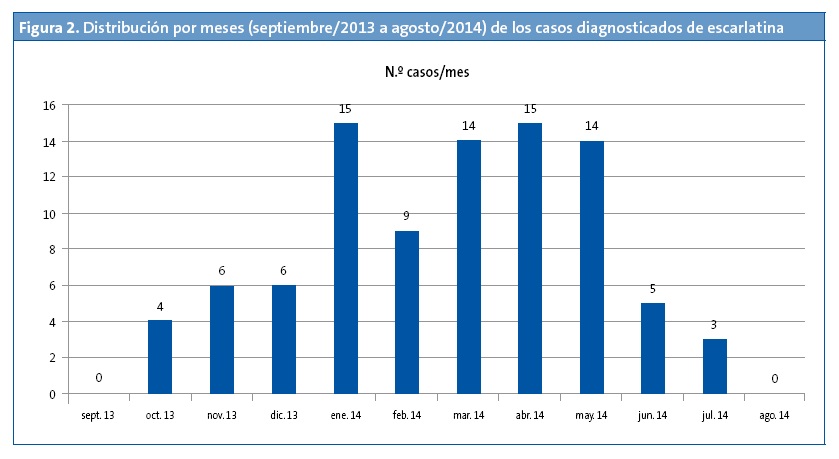
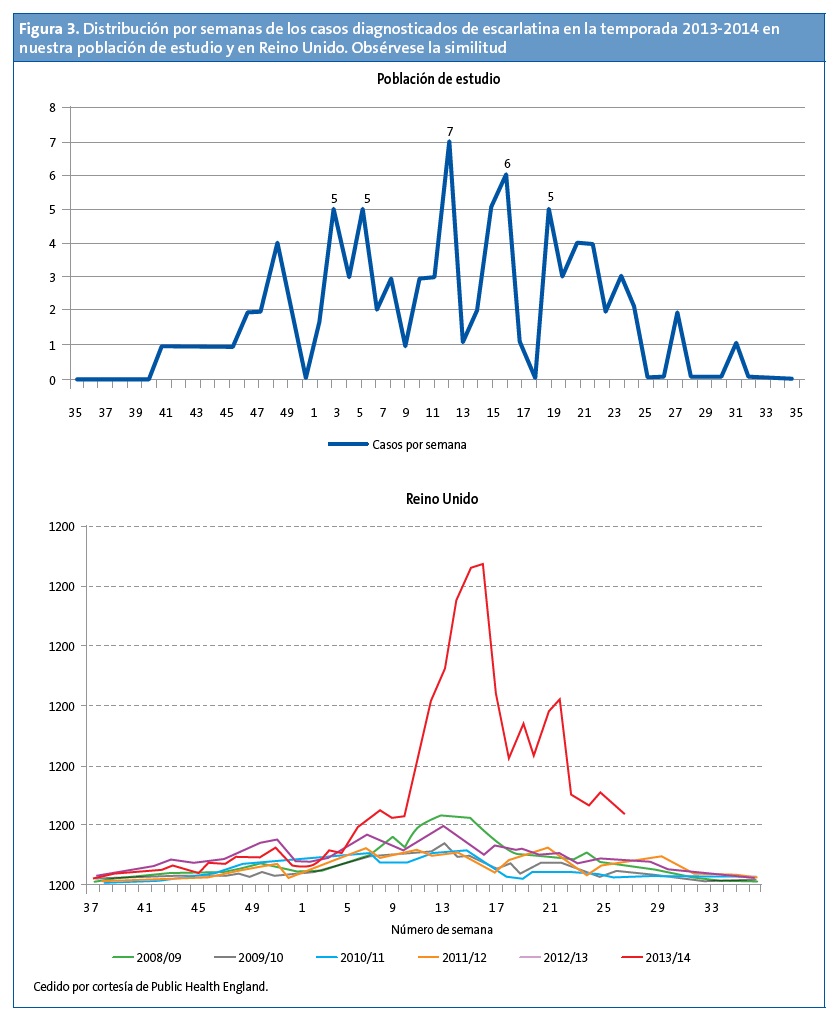
De los afectados, 52 eran varones (57,1%) y 39 mujeres (32,9%). La edad media fue de 4,15 años y se encontraron dos modas, a las edades de cuatro y cinco años (Fig. 1). Los meses en los que se registraron más casos fueron enero, marzo, abril y mayo (Fig. 2). La distribución por semanas muestra dos picos de mayor incidencia en las semanas 11 y 15 del año que se encuentran en el mes de marzo y abril respectivamente (Fig. 3).
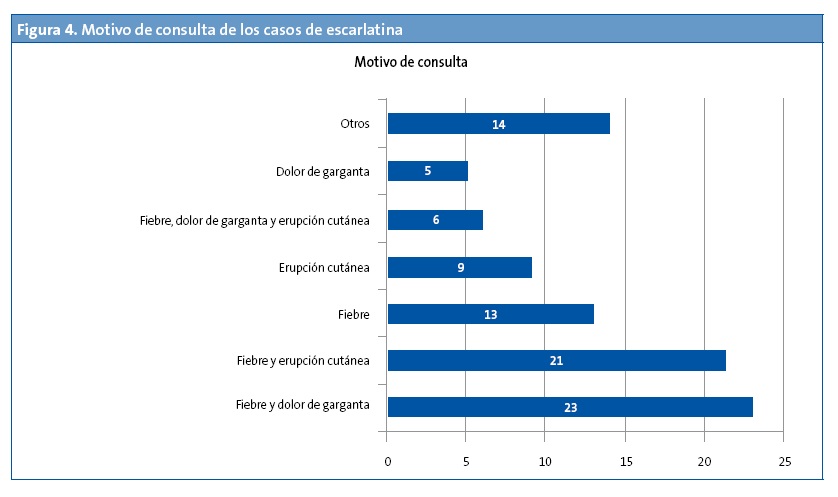
Los motivos de consulta más frecuentes fueron “fiebre y dolor de garganta” (25%) y “fiebre y erupción cutánea” (23%), el 14% solo consultó por fiebre y el 10% solo por exantema (Fig. 4).
La sintomatología descrita por el paciente y/o cuidador en la anamnesis aparece en la Tabla 1. Por orden decreciente son fiebre, dolor de garganta, erupción cutánea, mocos y/o tos, vómitos, dolor abdominal, cefalea y prurito. Otra sintomatología referida con menos frecuencia fueron estreñimiento, edema facial, disuria, otalgia y dolor de miembros.
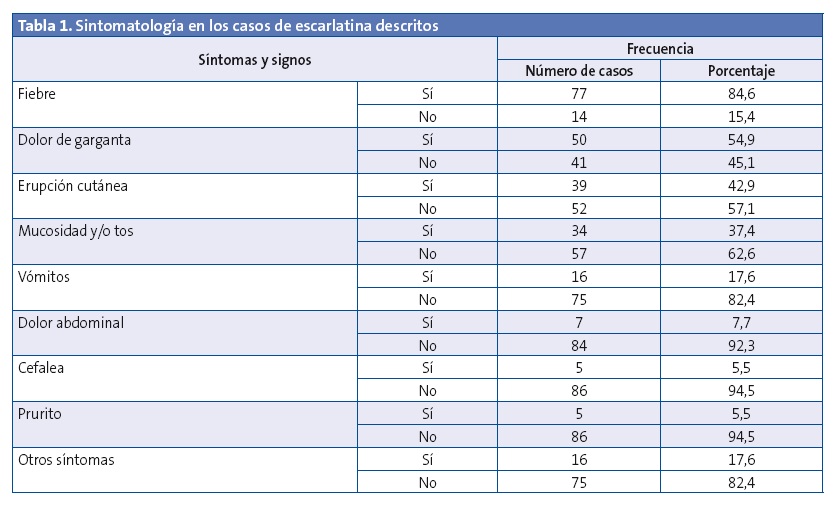
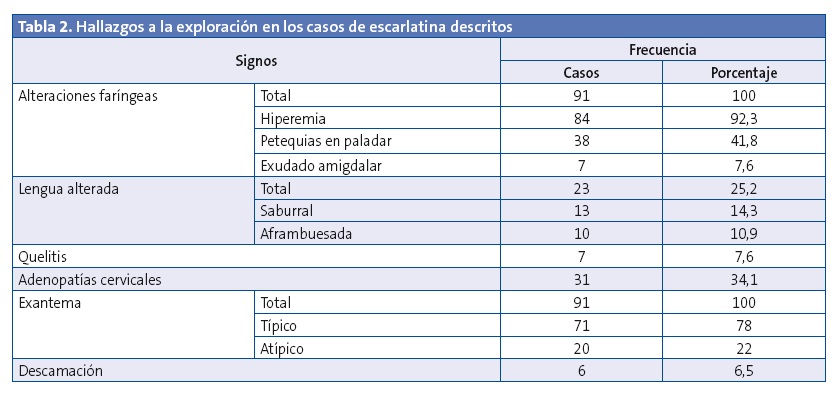
Los hallazgos en la exploración se describen en la Tabla 2. EL 100% de los pacientes presentaban alteraciones faríngeas y exantema, que consideramos hallazgos clínicos imprescindibles para el diagnóstico. Las alteraciones faríngeas más frecuentes fueron la hiperemia y las petequias en paladar, mientras que el exudado amigdalar se encontraba en un número escaso de pacientes. El exantema típico (se consideró como tal el que cumplía las características descritas en la introducción) estaba presente en 71 pacientes, mientras que en 20 pacientes observamos un exantema de características atípicas: cinco presentaban exantema maculoso no rasposo, uno tenía afectación palmoplantar, uno eritema y edema en pabellones auriculares, cinco eritrodermia extensa y dos eritrodermia localizada en la cara coincidiendo con el exantema rasposo típico en el resto del cuerpo, cinco edema palpebral y/o facial y/o distal de miembros, uno petequias en cara, cuello y axilas, un paciente presentó dos episodios de exantema urticarial (en uno de ellos asociaba también piel de lija). Todos los pacientes con exantemas atípicos tenían test microbiológico positivo, motivo por el cual se incluyeron en el análisis. Otros hallazgos exploratorios fueron alteraciones de la lengua, queilitis y adenopatías cervicales. La descamación está registrada solo en seis casos. En un paciente se encontró dermatitis perianal, cuyo exudado tanto faríngeo como perianal resultaron test estreptocócico positivos.
Los casos confirmados microbiológicamente fueron 76 (75 mediante test rápido y uno por cultivo), 15 fueron casos probables y correspondían a pacientes vistos con anterioridad en el servicio de urgencias, en el que no disponen de test rápido, que al ser atendidos en la consulta de Atención Primaria ya estaban con antibioterapia.
Como complicaciones supurativas, tres pacientes tuvieron otitis media aguda. Ningún paciente presentó complicaciones no supurativas.
Se describieron 15 casos recidivantes: diez casos (11%) presentaron recidivas en el mismo periodo de estudio (nueve de ellos dos episodios y un paciente tres episodios) y cinco (5,4%) se diagnosticaron de escarlatina en periodos anteriores al estudio (uno de ellos, dos episodios). Uno de los pacientes tuvo cuatro episodios en total, dos durante el periodo de estudio y dos en meses posteriores.
El tratamiento fue realizado con antibioterapia oral: penicilina en 23 pacientes (25,3%), amoxicilina en 60 (65,9%), amoxicilina-clavulánico en cinco (5,5%), un paciente alérgico a amoxicilina se trató con josamicina y un paciente con escarlatina recurrente en su tercer episodio con clindamicina. Solo un paciente, ante la sospecha de shock tóxico con eritrodermia extensa, se trató con cloxacilina, clindamicina y amoxicilina-clavulánico endovenosos. La duración de la antibioterapia prescrita fue de diez días, excepto en un paciente que solo se realizó durante ocho días.
DISCUSIÓN
En España la escarlatina dejó de ser enfermedad de declaración obligatoria a partir de 1996, por lo que no disponemos actualmente de datos epidemiológicos de referencia fiables7,9. En Reino Unido, país en el que se realiza vigilancia epidemiológica, se describe un patrón cíclico con picos de incidencia cada cuatro años.
El aumento de incidencia en nuestra población coincide con los aumentos de casos de escarlatina por encima de los niveles estacionales habituales en todo el Reino Unido en la temporada 2013/2014. Además, la distribución del número de casos agrupados por semanas del año también es similar, como se puede observar en la Fig. 3. En la temporada 2008/09 se detectó otro pico en Reino Unido que se acompañó de un aumento de la incidencia de enfermedad invasiva19,20. En nuestro centro de salud disponemos de test rápido estreptocócico desde el año 2007 y codificamos el diagnóstico de escarlatina mediante un código CIE.9 (código 034.1). Revisando la historia digital de nuestros pacientes desde esa fecha, se observó también un incremento de casos en esa misma temporada 2008/09 (Fig. 5)19-21. En Reino Unido continúa una incidencia mayor a la esperada en 2014/2015, no cumpliéndose el patrón cíclico22.
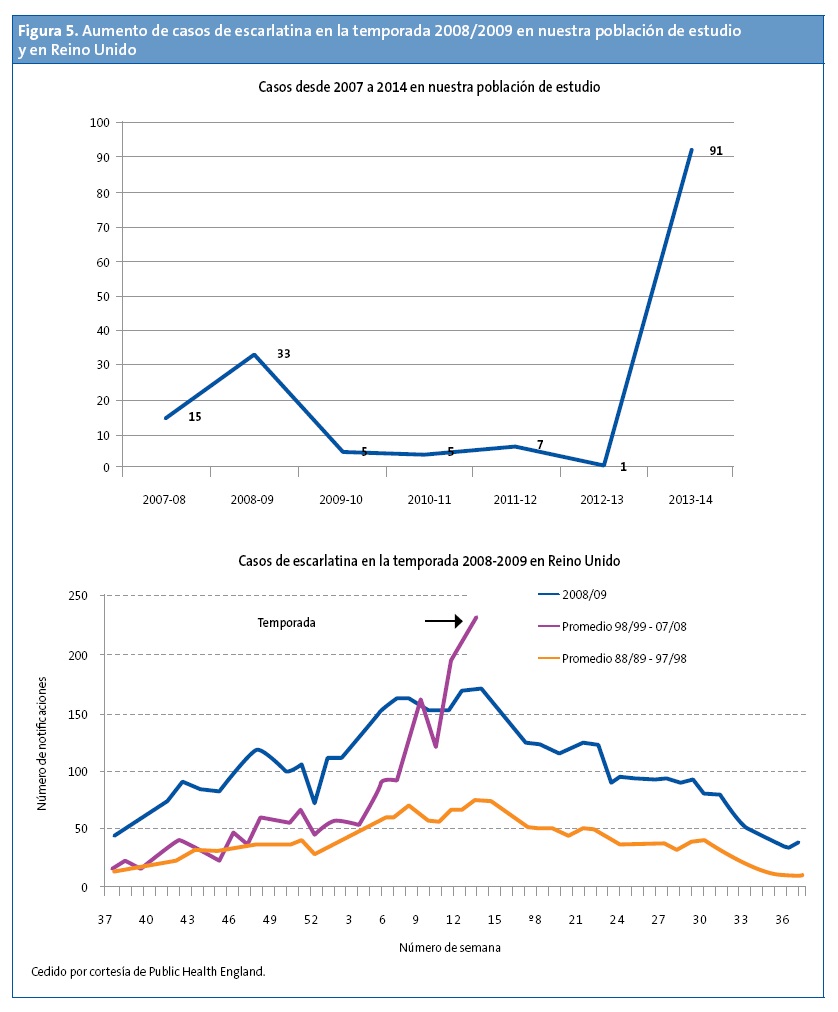
En nuestra muestra, la población de estudio era de 2852, que son los pacientes adscritos a los dos cupos, los casos se encontraban escolarizados en los distintos centros del municipio, hallándose casos en todos los colegios y guarderías, lo que nos hace pensar que no fue un brote localizado. La población infantil total del municipio es de 12 479, por lo que posiblemente la escarlatina afectó a muchos más niños. Además, teniendo en cuenta la similitud con Reino Unido, pensamos que el aumento de incidencia no fue circunscrito a nuestra localidad.
En poblaciones chinas como Hong Kong, Shanghái, Pekín y Taiwán se han notificado también aumentos importantes de escarlatina en otras temporadas distintas a las nuestras, diferencia que puede deberse a que son países más alejados con una climatología diferente23-26. Sin embargo, en Polonia, un país más cercano a nuestro entorno, en el que se realiza declaración obligatoria, se registraron un mayor número de casos en los años 2011/2012, temporada en la que la incidencia fue baja tanto en Reino Unido como en nuestra población de estudio27.
Dado el potencial aumento que podría producirse de la enfermedad invasiva por estreptococo, creemos necesario realizar una vigilancia epidemiológica a través de su declaración. En Reino Unido, debido a la preocupación que suscita este tema, se está proyectando una guía basada en la evidencia de directrices para el manejo de los brotes en escuelas, guarderías y otros servicios infantiles28.
El predominio que encontramos en varones coincide solo con algunos estudios, sin hallarse datos concluyentes en cuanto al sexo1,8-10. En nuestra muestra la edad de diagnóstico es más temprana que en los textos clásicos, coincidiendo con la mayoría de estudios más actuales, dato que podría ser debido al adelanto de la escolarización1,8-10.
Lo que más nos llama la atención de nuestro estudio es la discrepancia de los hallazgos clínicos con los descritos en los textos tradicionales. Para una enfermedad que se considera esencialmente febril, hubo ausencia de fiebre en un porcentaje alto de casos (15,4%). Esto podría deberse a que la escarlatina pueda cursar sin fiebre, o que esta se iniciara de forma más tardía a la aparición del exantema.
Los síntomas catarrales estaban presentes en casi un 40% de los pacientes, lo que nos hace pensar que bien existía una coinfección viral o que la escarlatina también pudiera ser responsable de ellos, opción que creemos menos probable. Otras publicaciones también refieren este hallazgo. Para aclararlo sería interesante realizar estudios que incluyeran pruebas de detección de virus respiratorios8.
La hiperemia faríngea estaba descrita en casi todos los casos, sin embargo, en muy pocos pacientes se observó el exudado faríngeo. El exudado faríngeo se considera un hallazgo típico en la bibliografía clásica, así como en las escalas de valoración de Centor y McIsaac en las que puntúa positivamente a favor de la etiología estreptocócica frente a la viral. Esto no concuerda con la escasez de casos de nuestra muestra ni con los datos de otros estudios clínicos que ponen en duda la validez de estas escalas6,8,29,30.
Lo más interesante de nuestros hallazgos fue la variedad de exantemas. Por una parte, muchos de los exantemas que cumplían criterios típicos eran de poca intensidad y extensión, razón por lo cual pensamos que pueden pasar desapercibidos tanto a los cuidadores como a los profesionales sanitarios.
En un 20% de los casos encontramos exantemas atípicos, todos ellos con confirmación microbiológica, que junto con el resto de la exploración compatible y la situación epidemiológica nos llevaron al diagnóstico de escarlatina. Por otra parte, cabe la posibilidad de que se trataran de cuadros virales en pacientes portadores faríngeos de EGA, algo que creemos poco probable al tener el resto de datos a favor.
De los exantemas atípicos destacamos: la eritrodemia, el exantema urticarial y la presencia de edema facial y en región distal de miembros. Uno de los pacientes con eritrodermia generalizada sin aspereza tuvo un episodio anterior con el mismo exantema que motivó su ingreso en el hospital por sospecha de shock tóxico; la evolución del cuadro, así como la aparición meses después del mismo exantema con test estreptocócico positivo que desapareció tras 24 horas de amoxicilina, sugiere que el cuadro por el que ingresó fue una escarlatina. Otro exantema atípico llamativo fue de tipo habonoso compatible con una urticaria. Este aconteció en dos episodios febriles en un mismo paciente y se acompañó de faringe muy hiperémica con test positivo a EGA, uno de los episodios además de la urticaria asociaba piel de lija.
Recordando que el EGA produce otras enfermedades, en un paciente la escarlatina coincidió con enfermedad estreptocócica perianal. De hecho, el motivo de consulta fue estreñimiento con dolor intenso a la defecación. El test estreptocócico fue positivo tanto en exudado de faringe como de la región perianal.
Otros hallazgos clínicos, como cambios en la lengua, queilitis y descamación cutánea, no están bien relatados en nuestro estudio debido a su retrospectividad y falta de seguimiento longitudinal.
La variabilidad clínica en la forma de presentación hace que la escarlatina pueda confundirse con otras enfermedades como cuadros virales, la enfermedad de Kawasaki o el shock tóxico. Es en estos cuadros dudosos en los que cobra máxima importancia los test microbiológicos para ayudar al diagnóstico. Aunque bien es cierto que un test positivo no debe descartar otra enfermedad como las mencionadas, la pronta respuesta a la antibioterapia podría evitar tratamientos más agresivos e ingresos prolongados ante la sospecha de otras patologías más graves.
En cuanto a las recidivas, no hay datos bibliográficos acerca de su incidencia. Los textos clásicos refieren la posibilidad de tener hasta tres episodios; sin embargo, tenemos un paciente que presentó cuatro. Estudios recientes están hallando nuevas variedades de toxinas pirogénicas que hacen posible que los pacientes puedan sufrir múltiples ataques. Se han descrito al menos hasta nueve toxinas diferentes5,6,11,12,14,25,31.
A pesar de las limitaciones de nuestro estudio, este informe destaca varios hallazgos clínicos importantes poco reportados previamente. Es necesario trabajos más amplios acerca de los síntomas y signos de la escarlatina, ya que su conocimiento podría ayudar a evitar la confusión con otras enfermedades. Recomendamos realizar test microbiológico en los casos en los que el diagnóstico está en duda. También sería interesante clarificar la epidemiología en nuestro país, para ello sería necesario que la escarlatina fuera una enfermedad de declaración obligatoria.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS: EGA: Streptococcus pyogenes del grupo A.
BIBLIOGRAFÍA
- Gerbe MA. Estreptococo grupo A. En: Kliegman RM, Stanton BF, Schor NF, Geme JW, Behrman RE. Nelson Tratado de Pediatría. 19.ª edición. Barcelona: Elsevier España. 2013; 955-60.
- Yang SG, Dong HJ, Li FR, Xie SY, Cao HC, Xia SC, et al. Report and analysis of a scarlet fever outbreak among adults through food-borne transmission in China. J Infect. 2007;55:419-24.
- Eisenhut M. Food as source of outbreaks of group A streptococcal disease. Arch Dis Child. 2011;96:323.
- Schwartz RH, Kim D, Martin M, Pichichero ME. A Reappraisal of the minimum duration of antibiotic treatment before approval of return to school for children with Streptococcal pharyngitis. Pediatric Infect Dis J. 2015;34:1302-4.
- Herranz Jordán B, Acitores Suz E, Payá López A, Hernández Merino A, Lamela Lence MT, Sánchez Casado M, et al. Escarlatina recurrente: presentación de cuatro casos. Rev Pediatr Aten Primaria. 2001;3:551-60.
- Chiesa C, Pacifico L, Nanni F, Orefici G. Recurrent attacks of scarlet fever. Arch Pediatr Adolesc Med. 1994;148:656-9.
- Pericas Bosch J. Escarlatina. FMC. Form Med Contin Aten Prim. 2002;9:352-3.
- Ortigosa Gómez S, Sánchez Buenavida A, Crehuet Almirall M, Martínez-Roig A. Diagnóstico de escarlatina en 151 casos en el servicio de urgencias pediátricas durante 2006-2008. Rev Enferm Infect Pediatr. 2011;24:154-61.
- Casaní Martínez C, Morales Suárez-Varela M, Santos Durántez M, Otero Reigada MC, Pérez Tamarit D, Asensi Botet F. Estudio epidemiológico de un brote de escarlatina. Rev Pediatr Aten Primaria. 2001;3:41-9.
- Fernández-Prada M, Martínez-Diz S, Colina López A, Almagro Nievas D, Martínez Romero B, Huertas Martínez J. Brote de escarlatina en un colegio público de infantil y primaria en Granada en 2012. An Pediatr (Barc). 2014;80:249-53.
- Silva-Costa C, Carriço JA, Ramírez M, Melo-Cristino J. Scarlet fever is caused by a limited number of Streptococcus pyogenes lineages and is associated with the exotoxin genes ssa, speA and speC. Pediatr Infect Dis J. 2014;33:306-10.
- Schmitz FJ, Beyer A, Charpentier E, Henriques Normark B, Schade M, Fluit AC, et al. Toxin-gene profile heterogeneity among endemic invasive european group a Streptococcal isolates. J Infect Dis. 2003;188:1578-86.
- Po-Chuang W, Wen-Tsung L, Shyi-Jou C, Chih-Chien W. Molecular characterization of group A streptococcal isolates causing scarlet fever and pharyngitis among young children: a retrospective study from a northern Taiwan medical center. J Microbiol Immunol Infect. 2013;47:304-10.
- Sanz JC, Bascones MA, Martin F, Sáez-Nieto JA. Escarlatina recurrente por reinfección reciente causadas por cepas no relacionadas de Streptococcus pyogenes. Enferm Infecc Microbiol Clin. 2005;23:388-92.
- Ficha técnica. Test rápido OSOM® Strep A Test Genzyme. En: Laboratorios LETI Diagnósticos [en línea] [consultado el 08/09/2016). Disponible en http://diagnosticos.leti.com/es/osom-strep-a-test_7735
- Llor C, Hernández Anadón S, Gómez Bertomeu FF, Santamaría Puig JM, Calviño Domínguez O, Fernández Pages Y. Validación de una técnica antigénica rápida en el diagnóstico de la faringitis por estreptococo betahemolítico del grupo A. Aten Primaria. 2008;40:489-96.
- Gieseker KE, McKenzie T, Roe MH, Toss JK. Comparison of two rapid Streptococcus pyogenes diagnostic tests with a rigorous culture standard. Pediatr Infect Dis J. 2002;21:922-7.
- Wright CM, Williams G, Ludeman L. Comparison of two tests for detecting group A streptococcal pharyngitis in the pediatric population at Wright-Patterson air Force Base. Mil Med. 2007;172:644-6.
- Guy R, Williams C, Irvine N, Reynolds A, Coelho J, Saliba V, et al. Increase in scarlet fever notifications in the United Kingdom, 2013/2014. Euro Surveill. 2014;19:20749.
- Lamden KH. An outbreak of scarlet fever in a primary school. Arch Dis Child. 2011;96:394-7.
- Group A streptococcal infections: third update on seasonal activity, 2008/09. Health Protection Report. En: Health Protection Agency (HPA) [en línea] [consultado el 08/09/2016]. Disponible en www.hpa.org.uk/hpr/archives/2009/news1309.htm#igas3
- Group A streptococcal infections: sixth update on seasonal activity, 2014/15. En: Public Health England Health [en línea] [consultado el 08/09/2016]. Disponible en www.gov.uk/government/uploads/system/uploads/attachment_data/file/442058/hpr2315_sf-gas6.pdf
- Luk EYY, Lo JYC, Li AZL, Lau MCK, Cheung TKM, Wong AYM, et al. Scarlet fever epidemic, Hong Kong, 2011. Emerg Infect Dis. 2012;18:1658-61.
- Chen M, Yao W, Wang X, Li Y, Chen M, Wang G, et al. Outbreak of scarlet fever associated with emm12 type group A Streptococcus in 2011 in Shanghai, China. Pediatr Infect Dis J. 2012;31:158-62.
- Wu PC, Lo WT, Chen SJ, Wang CC. Molecular characterization of Group A streptococcal isolates causing scarlet fever and pharyngitis among young children: A retrospective study from a northern Taiwan medical center. J Microbiol Immunol Infect. 2014;47:304-10.
- Yang P, Peng X, Zhang D, Wu S, Liu Y, Cui S, et al. Characteristics of group A Streptococcus strains circulating during scarlet fever epidemic, Beijing, China, 2011. Emerg Infect Dis. 2013;19:909-15.
- Staszewska E, Kondej B, Czarkowski MP. Scarlet fever in Poland in 2012. Przegl Epidemiol. 2014;68:209-12.
- Public Health England. Interim guidelines for the public health management of scarlet fever outbreaks in schools, nurseries and other childcare settings. En: Public Health England [en línea] [consultado el 08/09/2016]. Disponible en www.gov.uk/government/publications/scarlet-fever-managing-outbreaks-in-schools-and-nurseries
- Roggen I, van Berlaer G, Gordts F. Centor criteria in children in a paediatric emergency department: for what it is worth. BMJ Open. 2013;3:e002712.
- Cohen JF, Cohen R, Levy C, Thollot F, Benani M, Bidet P, et al. Selective testing strategies for diagnosing group A streptococcal infection in children with pharyngitis: a systematic review and prospective multicentre external validation study. CMAJ. 2015;187:23-32.
- Casaní Martínez C, Morales Suárez-Varela M, Santos Durántez M, Otero MC, Pérez Tamarit D, Asensi Botet F. Escarlatina recurrente. An Esp Pediatr. 1999;51:300-2.





