Vol. 16 - Num. 62
Originales
Atención en las primeras 48 horas tras el alta de maternidad en la consulta de enfermería o Pediatría
M.ª Teresa Asensi Monzóa, Elena Fabregat Ferrerb, M.ª Dolores Gutiérrez Siglerc, Javier Soriano Faurad
aPediatra. CS Serrería1. Valencia. España.
bPediatra. CS Gran Vía. Castellón. España.
cPediatra. CS Nou Molés. Valencia. España.
dPediatra. CS Fuensanta. Valencia. España.
Correspondencia: MT Asensi. Correo electrónico: maite.asensi@gmail.com
Cómo citar este artículo: Asensi Monzó MT, Fabregat Ferrer E, Gutiérrez Sigler MD, Soriano Faura J. Atención en las primeras 48 horas tras el alta de maternidad en la consulta de enfermería o Pediatría. Rev Pediatr Aten Primaria. 2014;16:117-24.
Publicado en Internet: 30-06-2014 - Número de visitas: 21291
Resumen
Introducción: desde el momento en que el recién nacido es dado de alta de la maternidad hasta que es atendido en su centro de salud (CS) pasa un periodo de tiempo crucial y, a veces, excesivamente prolongado.
Objetivo: conocer la edad en que son atendidos por primera vez los recién nacidos en Atención Primaria (AP) en la Comunidad Valenciana.
Material y métodos: encuesta dirigida a los pediatras de AP.
Resultados: participaron 46 CS de las provincias de Castellón y Valencia (de un total de 162 centros). Se declararon datos de 248 recién nacidos durante el periodo del 9 de abril al 30 de junio del año 2013. El 58% de los recién nacidos fueron vistos por primera vez en su CS a partir del quinto día de vida. Los niños nacidos en un hospital público tienen casi dos veces más probabilidades de acudir al CS antes de los seis días de vida que los niños nacidos en un hospital privado (odds ratio [OR]: 1,97; intervalo de confianza del 95% [IC 95%]: 0,92 a 4,1; p=0,07). El 56,93% de las lactancias maternas y mixtas fueron vistas después del quinto día de vida. El 24,2% de los casos estudiados no tenía la tarjeta de asistencia sanitaria (TAS) al salir de la maternidad. La mayoría de los niños nacidos en maternidades privadas no tenía la TAS al alta, requisito imprescindible para solicitar cita en su CS.
Conclusiones: desde el momento en que el recién nacido es dado de alta de la maternidad hasta que es atendido por primera vez por el equipo de pediatra-enfermera, pasa un periodo de tiempo importante.
Palabras clave
● Lactancia materna ● Prevención en recién nacido ● Recién nacido ● Visita posnatalNota:
Los autores son miembros del Grupo Asesor Técnico para la Pediatría de Atención Primaria (GATPAP), de la Sociedad Valenciana de Pediatría y de la Asociación Valenciana de Pediatría de Atención Primaria.
INTRODUCCIÓN
España tiene un sistema público de sanidad universal y gratuito, donde el tránsito de cuidados desde la maternidad al equipo de Atención Primaria (AP) no está adecuadamente establecido y está excesivamente burocratizado. El acceso a los centros de AP (centro de salud [CS]) depende de la acreditación del recién nacido (RN) con su tarjeta de asistencia sanitaria (TAS) y de la asignación a un pediatra de su zona básica de salud, y estos dos trámites no siempre se realizan de manera inmediata al alta en todas las maternidades de la Comunidad Valenciana. Pero además, depende de la solicitud de cita previa al equipo de Pediatría de AP, de lo que no consta que existan normas o procedimientos de urgencia para habilitar un encuentro entre la familia y el pediatra, matrona o enfermera con la premura que se precisa.
Esta misma problemática se plantea en otros países desarrollados, como EE. UU., donde encuentran que los RN no reciben la atención posnatal recomendada1, sobre todo los más vulnerables, con un nivel socioeconómico más bajo, aunque los motivos parecen ser diferentes, debidos a la no universalidad ni gratuidad del sistema sanitario norteamericano.
La deshidratación hipernatrémica (DHN) en RN alimentados con lactancia materna (LM) debida al ayuno suele precisar ingreso, como media, al séptimo día de vida, con un intervalo de 6-10 días2. En nuestro medio, la edad media de ingreso es de 4,58 días (2-11 días) y la incidencia de 1,4 casos por 1000 nacidos en el año3. En España, los ingresos más tempranos pueden tener relación con factores protectores, como la gratuidad,la universalidad y el fácil acceso a la red hospitalaria3.
Programas de control del peso a las 72-96 horas del parto consiguen detectar precozmente la DHN (media de tres días de diagnóstico frente a los seis días cuando no se realizan estos controles), y además, los niveles de sodio son más bajos (147 frente a 150 mmol/l). Otros resultados muy valorados de estos programas son los porcentajes de lactancias (73 frente a 22%) al inicio y a las cuatro semanas (57 frente a 22%). Todas estas diferencias fueron estadísticamente muy significativas según algunos estudios3,4.
A pesar de la variabilidad entre centros, el estudio de Escobar5 encuentra un factor protector significativo para disminuir las rehospitalizaciones de RN si han tenido visita en su CS antes de las 72 horas tras el alta de maternidad (odds ratio [OR] ajustada para reingresar: 0,83; intervalo de confianza del 95% [IC 95%]: 0,69 a 1,0).
Desde la perspectiva de la prevención y promoción, atendiendo al mantenimiento de la LM exclusiva hasta los seis meses de vida, el documento de la Organización Mundial de la Salud (OMS) “Pruebas científicas de los diez pasos hacia una feliz lactancia natural”6 encuentra evidencias de que el apoyo precoz, después del alta de maternidad, a través de los servicios de salud consiguió más LM a las cuatro semanas y a los seis meses de evaluación. Así, en Brasil, los lactantes que asistieron a centros de lactancia tenían más probabilidades que los que no lo hicieron de tomar LM exclusiva a los cuatro meses (43 frente a 18%) y a los seis meses (15 frente a 6%)6.
Un ensayo clínico aleatorizado en 100 mujeres puérperas agrupadas en un grupo de estudio con un primer control entre el cuarto y el quinto días de vida y un grupo control con un primer control ambulatorio más allá de la primera semana de vida, encontró que el 100% de todas las LM del grupo de estudio seguían de forma exclusiva al mes de vida, frente al 70% del grupo control. El único factor de riesgo independiente para el fracaso de la LM fue el control después de la semana de vida (p=0,06) con una OR de 4,1 (IC 95%: 1,19 a 14,35)6.
Otros estudios han demostrado que el momento en que se realiza la intervención de apoyo y educación en lactancia resulta determinante. Así, las dificultades con la LM ocurrían en un 6% de los niños que recibían visita el tercer día de vida frente a un 34% de aquellos que no la recibían (OR: 7,66; IC 95%: 6,03 a 9,71). Los que recibían el apoyo en la visita a la semana (séptimo día de vida) tenían 11,5 veces más probabilidad de tener problemas con la alimentación que aquellos visitados al tercer día7.
Un ensayo clínico aleatorizado realizado en 60 madres atendidas en un Hospital de la Iniciativa para la Humanización de la Asistencia al Nacimiento y la Lactancia (IHAN) (acreditación internacional de buenas prácticas en el manejo del nacimiento y la lactancia concedido por la OMS/UNICEF) encontró que, el recibir un apoyo extra, a domicilio, el tercer día de vida (grupo experimental) frente al grupo control que recibió una educación o atención estándar pocas horas después del parto, supuso un incremento significativo en el porcentaje de LM exclusiva a las dos semanas, a las seis semanas y a los seis meses; así como un incremento en la duración total de lactancia materna8.
Son varias las instituciones científicas y asistenciales que avalan, basadas en pruebas, la visita en los primeros días de vida, antes de finalizar la primera semana; la Academia Americana de Pediatría, la Asociación Española de Pediatría de Atención Primaria (AEPap) y el Grupo de Actividades Preventivas y de Promoción de la Salud recomendadas para la infancia y la adolescencia de la AEPap y del Programa de Actividades Preventivas y de Promoción de la Salud de la Sociedad Española de Medicina de Familia y Comunitaria (PAPPS-semFYC)9-16.
En la “Guía de atención al nacimiento y la lactancia materna para profesionales sanitarios del Comité de Lactancia Materna del Hospital 12 de Octubre y Centros de Salud de Atención Primaria”17 se propone facilitar la primera visita del RN y sus progenitores al CS por el personal administrativo, a ser posible antes del quinto día, independientemente de que posea o no la TAS.
Pero, para que las guías sean capaces de cambiar prácticas, deben usarse, por lo que se precisa desarrollar estrategias de implementación, implicando a todos los profesionales de los centros de salud que intervienen en el cuidado de madres y sus hijos18.
Objetivo
Conocer la edad a la que son atendidos por primera vez los RN tras el alta de la maternidad en la Comunidad Valenciana, y la relación de esta variable con otras consideradas importantes (si la TAS se obtuvo antes del alta de maternidad, tipo de alimentación en la primera visita al centro, hospital de procedencia…).
MATERIAL Y MÉTODOS
Se elaboró una encuesta en el entorno de herramientas de Google Drive®. Se incluyeron RN sanos, dados de alta de la maternidad antes de las 72 horas de vida. Excluidos los nacidos por cesárea e ingresados de RN en neonatos. Con las siguientes variables de estudio: a) edad de la primera visita en el centro de AP; b) hospital de nacimiento; c) tipo de alimentación al alta de la maternidad, y d) si se entregó la TAS antes del alta de maternidad.
La población a la que se dirigió el estudio fue a los pediatras de AP de la Comunidad Valenciana que quisieran colaborar accediendo a la encuesta, cumplimentándola a la recepción del RN en la consulta de enfermería, matrona o Pediatría.
Se usaron los siguientes protocolos de adhesión y colaboración de pediatras: a) solicitud de colaboración a la lista de distribución de pediatras de AP de la Asociación Valenciana de Pediatría de Atención Primaria (AValPap); b) solicitud de colaboración al estudio mediante correo electrónico a los afiliados de la AValPap; c) solicitud de colaboración al estudio mediante correo electrónico a los afiliados de la Sociedad Valenciana de Pediatría.
El periodo de estudio comprendió del 9 de abril al 30 de junio de 2013.
RESULTADOS
De un total de 162 centros de la provincia de Castellón y Valencia (incluidos sus centros auxiliares), 48 colaboraron aportando datos de uno o varios RN recibidos en el periodo de estudio; 248 RN se incluyeron en el estudio.
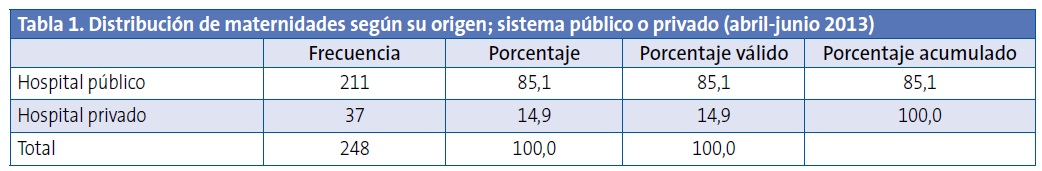
El 14,9% de los casos de estudio nacieron en maternidades privadas (Tabla 1).
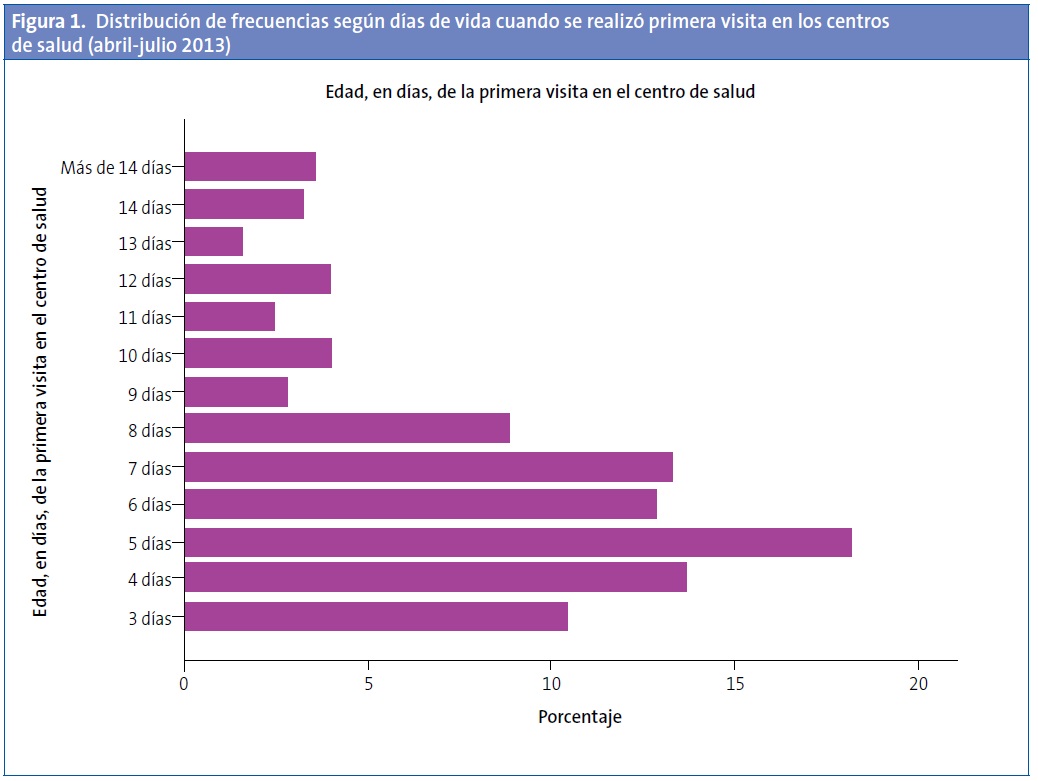
El 58% de los RN acudieron después del quinto día de vida. El 15% de los niños aún no habían sido vistos por ninguna enfermera o pediatra de AP a los diez días de vida (Tabla 2; Fig. 1).

El tipo de maternidad, pública o privada, tenía relación (p<0,05) con la demora en ser visitado por primera vez en el centro (Tabla 3).
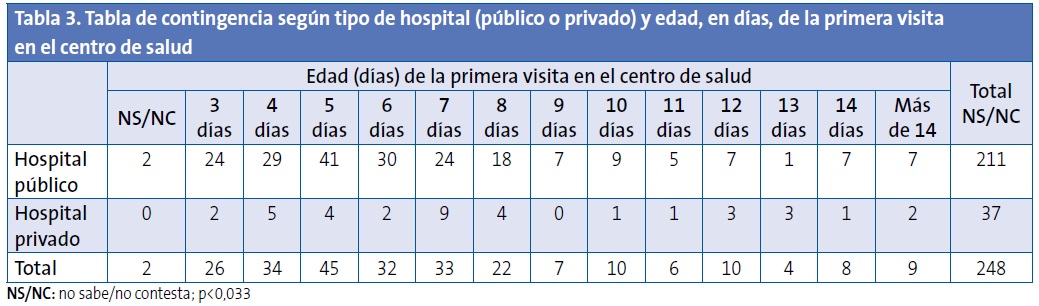
Los niños nacidos en hospital público tienen casi dos veces más probabilidades (OR: 1,97; IC 95%: 0,92 a 4,1; p=0,07) de acudir al CS antes de los seis días de vida que los niños nacidos en hospital privado.
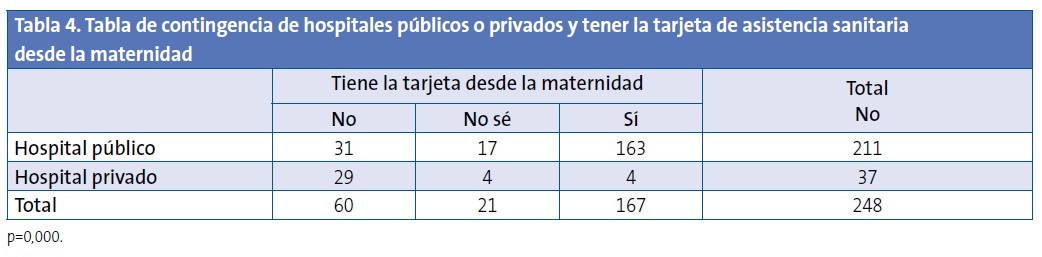
El 24,2% de los casos estudiado no tenía la TAS al salir de la maternidad, requisito imprescindible para solicitar cita en su CS. La mayoría de los niños/as nacidos en maternidades privadas no tenía la TAS al alta. El 19% de las maternidades públicas no entregaron la tarjeta TAS al alta, a pesar de tener mecanismos habilitados para hacerlo (Tabla 4).
Tomar LM es un factor importante para realizar la primera visita del recién nacido/a en las primeras 48 horas tras el alta de maternidad, ya que facilita lactancias adecuadamente establecidas y evita riesgos de alimentación ineficaz por ausencia de ayuda al binomio madre-hijo/a. Cerca del 85% de los niños/as tomaban LM (exclusiva o mixta) al alta de maternidad.
Atendiendo a la maternidad de nacimiento, no se encontraron diferencias significativas en el tipo de alimentación (materna, mixta, exclusiva con fórmula).
Agrupadas por tipo de maternidad, pública o privada, tampoco se encontraron diferencias significativas con el tipo de alimentación (Fig. 2).
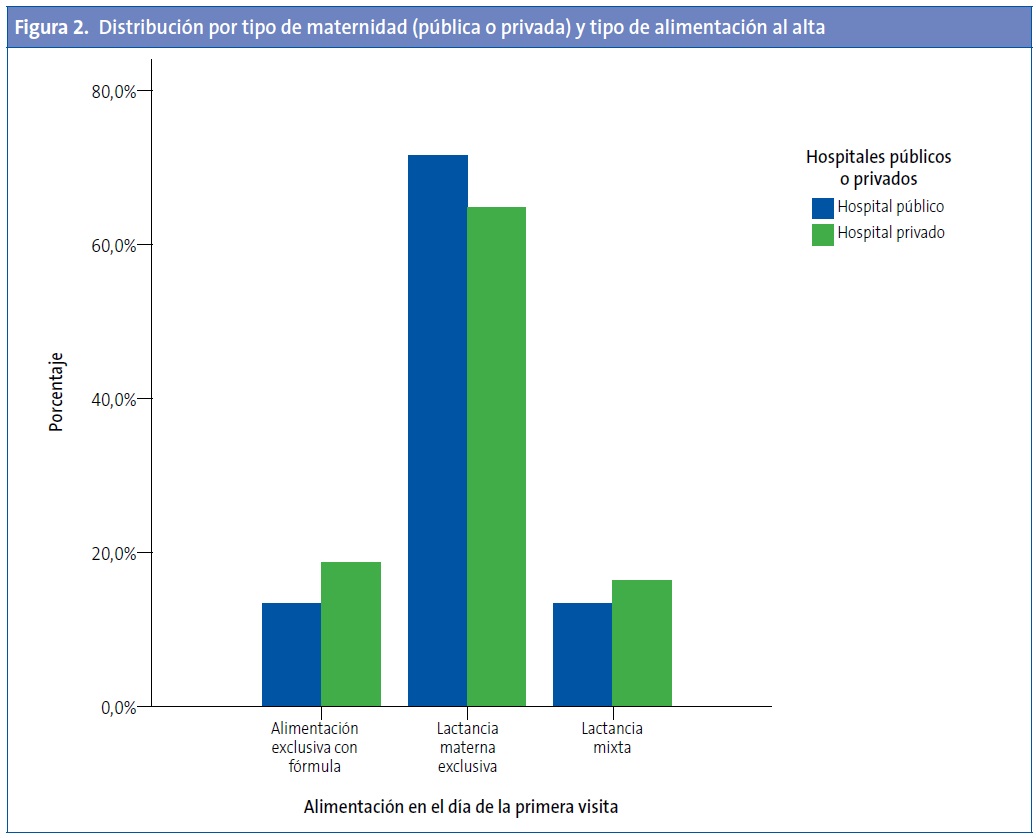
Los niños nacidos en hospital público tienen 1,57 más probabilidades de ser alimentados con LM exclusiva que los nacidos en hospital privado (OR: 1,57; IC 95%: 0,61 a 4; p=0,34).
Un 56,93% de las LM y mixtas fueron vistas después del quinto día de vida, lo cual constituye un riesgo para solucionar lactancias mal establecidas, pérdida de lactancias, riesgo de deshidratación e ictericia por ayuno, entre otras complicaciones.
DISCUSIÓN
Limitaciones del estudio: los resultados muestran un sesgo de colaboración, la muestra no se ha obtenido de manera estratificada por nacimientos, por centros hospitalarios, CS y provincias. Con todo y estas limitaciones, los resultados ofrecen una buena imagen de lo que acontece en nuestra comunidad y en ausencia de otros estudios anteriores podemos utilizarlos para reconocer la magnitud del problema, la relación con las variables independientes de estudio y la elaboración de conclusiones y recomendaciones para mejorar la calidad de atención del RN tras el alta de maternidad en los centros de AP.
Desde el momento en que el RN es dado de alta de la maternidad hasta que es atendido por primera vez por su pediatra, pasa un periodo de tiempo crucial y a veces excesivamente prolongado.
El 58% de los RN acudieron después del quinto día de vida. El 15% de los niños aún no habían sido vistos por ninguna enfermera o pediatra de AP a los diez días de vida.
La segunda prueba de detección de enfermedades metabólicas y genéticas tiene que realizarse entre el tercer y el quinto día de vida, pero con frecuencia se lleva a cabo más tarde; la tardanza en realizarse esta primera visita los hace especialmente vulnerables a DHN por ayuno en lactantes al pecho materno, ictericia patológica, problemas no detectados precozmente de alimentación al seno materno y rehospitalizaciones que estarían indicando un fallo en el tránsito de cuidados desde el alta de la maternidad hasta la primera visita en el CS.
Un 56,93% de las LM y mixtas fueron vistas en nuestro estudio después del quinto día de vida, lo cual constituye un riesgo para lactancias mal establecidas, pérdida de lactancias, riesgo de deshidratación, ictericia por ayuno, etc. Desde la perspectiva de la prevención de la enfermedad y promoción de la salud, atendiendo al mantenimiento de la LM exclusiva hasta los seis meses de vida, el documento de la OMS “Pruebas científicas de los diez pasos hacia una feliz lactancia natural” encuentra evidencias de que el apoyo precoz después del alta de la maternidad, a través de los servicios de salud, consiguió lactancias maternas que continuaban a las cuatro semanas y a los seis meses de evaluación6.
Un requisito imprescindible para acceder a la atención en el CS es estar en posesión, el RN, de la TAS al acudir al CS, esto es, que tenga dicha tarjeta al salir de la maternidad.
El 24,2% de los casos estudiados no tenía la TAS al salir de la maternidad. La mayoría de los niños/as nacidos en maternidades privadas no tenía TAS al alta, requisito imprescindible para solicitar cita en su CS.
La TAS se debe poder obtener de forma inmediata, aunque sea con datos mínimos, en el mismo CS, para permitir que la visita se realice en el mismo día en que acuden al CS por primera vez, ya sea por la enfermera, la matrona o el/la pediatra.
Los datos disponibles en este estudio nos llevan a plantearnos que los padres no tienen indicaciones en todas las maternidades de que deben acudir en las primeras 24-48 horas tras el alta; pensamos que en la recepción de los CS no se facilita la TAS en el mismo día en algunos de los recién nacidos, ni tampoco se considera su atención como no demorable, a realizar en el día por médico, enfermera o matrona. De otra forma no tendríamos hasta casi un 16% de niños que son vistos por primera vez pasado el décimo día de vida.
Recomendaciones
- La atención se realizará en el centro de AP 48-72 horas después del alta de la maternidad.
- La familia dispondrá de un informe del alta con descripción de las intervenciones realizadas, las intervenciones pendientes y los planes propuestos, incluida la comunicación al equipo de Pediatría de AP de los cuidados que precisa en este ámbito.
- Acreditación mediante la TAS al alta de la maternidad.
- Asignación a pediatra y cita previa para la consulta de enfermería, matrona y/o Pediatría de AP antes del alta de maternidad.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS: AEPap: Asociación Española de Pediatría de Atención Primaria • AP: Atención Primaria • AValPap: Asociación Valenciana de Pediatría de Atención Primaria • CS: centro de salud • DHN: deshidratación hipernatrémica • IC 95%: intervalo de confianza del 95% • LM: lactancia materna • OMS: Organización Mundial de la Salud • OR: odds ratio • PrevInfad: Grupo de Actividades Preventivas y de Promoción de la Salud recomendadas para la infancia y la adolescencia de la AEPap y del Programa de Actividades Preventivas y de Promoción de la Salud (PAPPS-semFYC) • RN: recién nacido • TAS: tarjeta de asistencia sanitaria.
BIBLIOGRAFÍA
- Galbraith AA, Egeter SA, Marchi KS, Chavez G, Braveman PA. Newborn early discharge revisited: are California newborns receiving recommended postnatal services? Pediatrics. 2003;111:364-71.
- Oddie S, Richmond S, Coulthard M. Hypernatraemic dehydration and breast feeding: a population study. Arch Dis Child. 2001;85:318-20.
- Peñalver O, Gisbert J, Casero J, Bernal A, Oltra M, Tomás M. Deshidratación hipernatrémica asociada a lactancia materna. An Pediatr (Barc). 2004;61:340-3.
- Iyer N, Srinivasan R, Evans K, Ward L, Cheung W, Matthes J. Impact of an early weighing policy on neonatal hypernatraemic dehydtration and breast feeding. Arch Dis Child. 2008;93:297-9.
- Escobar G, Greene J, Hulac P, Kincannon E, Bischoff K, Gardner M, et al. Rehospitalisation after birth hospitalisation:patterns among infants of all gestations. Arch Dis Child. 2005;90:125-31.
- OMS. Pruebas científicas de los diez pasos hacia una feliz lactancia natural. Ginebra: OMS; 1998. p. 81-98.
- Aksu H, Kücük M, Düzgün G. The effect of postnatal breastfeeding education/support offered at home 3 days after delivery on breastfeeding duration and knowledge: a randomized trial. J Matern Fetal Neonatal Med. 2011;24:354-61.
- Gagnon AJ, Dougherty G, Jimenez V, Leduc N. Randomized trial of postpartum care after hospital discharge. Pediatrics. 2002;109:1074-80.
- Chung M, Raman G. Trikalinos T, Lau J, Ip S. Interventions in Primary Care to promote breastfeeding: An evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149:565-82.
- Hagan J, Shaw J, Ducan P (eds.). Bright Futures: Guidelines for Health Supervisions of Infants, Children and Adolescents, 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008.
- Rourke Baby Record: Evidence-based infant/child health supervision guide. 2006. The College of Family Physicians of Canada and the Canadian Paediatric Society [en línea] [consultado el 04/04/2009]. Disponible en http://www.rourkebabyrecord.ca/default.asp
- Brooke A.Health for all children, 4th ed. Editor: David Hall and David Elliman. Oxford: Oxford University Press; 2006. p. 422.
- Demott K, Bick D, Norman R, Ritchie G, Turnbull N, Adams C, et al. Clinical guidelines and evidence review for post natal care: Routine post natal care of recently delivered women and their babies. London: National Collaborating Centre for Primary Care and Royal College of General Practitioners; 2006.
- Asociación Española de Pediatría de Atención Primaria. Programa de Salud Infantil. Madrid: Exlibris Ediciones; 2009. p. 624.
- Grupo PrevInfad/PAPPS Infancia y Adolescencia. Guía de actividades preventivas por grupos de edad. En: Recomendaciones PrevInfad/PAPPS [en línea] [actualizado el 15/05/2014; consultado el 04/04/2009]. Disponible en www.aepap.org/previnfad/actividades.htm
- Guía de Atención al Nacimiento y la Lactancia Materna para Profesionales Sanitarios. Comité de Lactancia Materna, Hospital 12 de Octubre y centros de salud. Servicio Madrileño de Salud. Madrid; 2011.
- Martín-Iglesias S, del Cura-González I, Sanz-Cuesta T, Arana-Cañedo-Argüelles C, Rumayor-Zarzuelo M, Alvarez de la Riva M. Effectiveness of an implementation strategy for a breastfeeding guideline in Primary Care: cluster randomised trial. BMC Fam Pract. 2011;12:144.





