¿Consejo o prescripción? Análisis de las recomendaciones pediátricas en las consultas del programa de salud infantil
Cristina Nunesa, Mariano Ayalab
aProfesora asociada. Centro de Investigação sobre Espaço e Organizações, Universidade do Algarve. Campus de Gambelas. Portugal.
bMédico, especialista en Salud Pública. SErvicio de Salud Pública. CS de Castro Marim. Portugal.
Correspondencia: C Nunes. Correo electrónico: csnunes@ualg.pt
Cómo citar este artículo: Nunes C, Ayala M. ¿Consejo o prescripción? Análisis de las recomendaciones pediátricas en las consultas del programa de salud infantil. Rev Pediatr Aten Primaria. 2013;15:305.e135-e143.
Publicado en Internet: 09-01-2014 - Número de visitas: 21412
Resumen
Introducción: razonar las recomendaciones aumenta la adhesión y satisfacción de las madres en las consultas del programa de salud infantil. Una recomendación puede ser considerada consejo o prescripción según sea razonada o no.
Objetivos: en el presente estudio describimos y analizamos el uso del consejo y la prescripción en las recomendaciones transmitidas a las madres en el ámbito del programa de salud infantil. Analizamos la cantidad y calidad de las recomendaciones, su contenido y su relación con la duración de la consulta, y con las características del niño y de la madre.
Material y métodos: grabamos 50 consultas de cinco pediatras y, a través del análisis de contenido, clasificamos las recomendaciones en seis categorías: prevención secundaria, prevención primaria, promoción de la salud, desarrollo, educación y relación familiar.
Resultados: los pediatras realizan 4,37 recomendaciones por consulta, el 69% por iniciativa propia y el 31% a petición de las madres. Los pediatras hacen sobre todo recomendaciones acerca de la promoción de la salud (32,87%), la prevención secundaria (17,13%) y la primaria (10,19%). La cantidad de recomendaciones está positivamente asociada con la duración de la consulta (M=16,10 minutos) y negativamente asociada con la edad del niño. Los pediatras utilizaron mucho más el consejo (70%) que la prescripción (30%). No observamos efecto del nivel de escolaridad de la madre.
Conclusión: en todas las variables observadas existe una gran heterogeneidad entre los pediatras, lo que sugiere que existen estilos pediátricos diferentes cuyas características y efectos merecen ser investigados en trabajos futuros para ayudar a los pediatras a mejorar su práctica profesional.
Palabras clave
● Atención Primaria ● Consejo ● Pediatras ● Prescripción ● Programa de Salud Infantil ● RecomendacionesINTRODUCCIÓN
Los pediatras son la principal fuente técnica de asesoramiento de los padres sobre el desarrollo y educación de sus hijos1-6, cuyo marco institucional en Andalucía es el programa de salud infantil. Este programa asigna a los pediatras no solo la prevención, la detección precoz y el tratamiento de enfermedades y alteraciones del desarrollo, sino también el apoyo a los padres en la educación de sus hijos para la adquisición de hábitos saludables7. Sin embargo, existe un conocimiento limitado sobre los contenidos y el modo concreto en que son realizadas sus recomendaciones. Aunque reciben poca atención en la formación pediátrica y en la investigación, las consultas del niño sano, en las que se desarrollan actividades de promoción de la salud y prevención de la enfermedad, constituyen un aspecto central de la práctica pediátrica8.
La agenda pediátrica está organizada según una perspectiva biomédica en la que los temas psicosociales y educativos ocupan un lugar secundario9-15. Sin embargo, los pediatras se adhieren a los principios generales de la promoción de la salud9,16 y la Academia Americana de Pediatría17 considera que los aspectos psicosociales tienen creciente importancia por su frecuencia y relevancia.
Por otro lado, una amplia base empírica indica que las madres desean más información de la que reciben5,12,14,18 y que se preste más atención al desarrollo y a la educación infantil en las consultas2,19.
La comunicación pediatra-madre es importante porque afecta a los resultados de la atención a la salud infantil. La eficacia de la comunicación está asociada con la satisfacción de las madres, la adhesión a las recomendaciones pediátricas y la discusión de temas psicosociales2,20-25. Por otro lado, la falta de información, la información errónea y la falta de sensibilidad a sus necesidades son las principales quejas expresadas por las madres22,23,25,26.
Una comunicación eficaz se basa en el uso de técnicas que faciliten la expresión de dudas y preocupaciones maternas y que aumenten la comprensión y adhesión a las recomendaciones. Una técnica muy importante es el uso de la racionalización y la explicación de las recomendaciones21,22,24,27. Razonar las recomendaciones facilita que las madres las integren en una explicación coherente del enorme conjunto de factores que determinan la salud, el desarrollo y la educación de su hijo.
Una recomendación médica puede ser dada como consejo o como prescripción21,27. Entendemos por consejo la recomendación de pautas de actuación de un modo razonado o elaborado y por prescripción la realizada sin explicación del objetivo ni de la cadena causal en que se inserta.
La validez de la mayoría de los estudios en este campo está afectada por la utilización de cuestionarios autocumplimentados o encuestas telefónicas. Ello limita las inferencias sobre las características y la calidad de la comunicación y realza la necesidad de estudios basados en la observación directa de las consultas.
El objetivo de este estudio es describir y analizar el uso del consejo y la prescripción en las recomendaciones transmitidas a las madres en el ámbito del programa del niño sano, mediante el análisis de las grabaciones íntegras de las consultas. Estudiaremos la cantidad y la calidad de las recomendaciones, su contenido y su relación con la duración de la consulta, y con las características del niño y de la madre.
MATERIAL Y MÉTODOS
Participantes
Se observaron 50 consultas de cinco pediatras (un hombre y cuatro mujeres) seleccionados en tres distritos sanitarios de la provincia de Sevilla (España), con un promedio de 45,60 años de edad (desviación típica [DT] 9,48; mínimo [mín.] 34; máximo [máx.] 63) y 16,80 años de experiencia profesional. Los criterios de selección fueron la accesibilidad y poseer más de cinco años de experiencia profesional en Atención Primaria. Todos los pediatras contactados accedieron a participar.
Los niños que acudieron a la consulta tenían un promedio de edad de 16,48 meses (DT 18,45; mín. 0,33; máx. 60), las madres tenían una media de edad de 32,05 años (DT4,16; mín. 22; máx. 41) y habían completado, de media, 9,70 años de estudios (DT 2,71; mín. 8; máx. 15).
Procedimiento
Después de obtener las autorizaciones necesarias y el consentimiento informado de las madres, observamos y grabamos en audio consecutivamente las diez consultas siguientes de cada pediatra ya inscritas en el libro de citas del centro de salud. Las grabaciones fueron íntegramente transcritas y luego analizadas para describir cuantitativa y cualitativamente las recomendaciones dadas por el pediatra y las solicitadas por las madres. Una consulta fue excluida porque el continuo llanto del niño imposibilitó su trascripción.
Para cuantificar las recomendaciones se utilizó el criterio de significación. Así, una recomendación puede ser dada por el pediatra con una sola frase: “No utilices el tacataca, porque provoca accidentes en casa y puede dañar las caderas” o desarrollado en varias frases secuenciales, como por ejemplo para introducir el tema del desarrollo psicomotor: “Ahora lo importante es estimularla. A ella [otra hermana] no le hace falta, que está muy bien. (…) Pero tampoco obligarlas a que estén de pie. Ni hacer cosas que no corresponden a su edad. Ahora mismo tienen un desarrollo que está perfecto para su edad”.
Tal como referimos anteriormente, distinguimos dos tipos de recomendaciones: consejo y prescripción. Entendemos por consejo la recomendación de pautas de actuación de un modo razonado o elaborado, esto es, utilizando por lo menos una de las siguientes explicaciones: detallar la conducta propuesta, dar ejemplos y explicar la base racional. Los consejos pueden referirse a conductas, sentimientos y maneras de enfrentarse a problemas como enfermedades o molestias. En estos dos ejemplos se explica la base racional de la evitación de un comportamiento por su relación causal con resultados indeseados:
“No utilices el tacataca, porque provoca accidentes en casa y puede dañar las caderas” (pediatra 1, consulta 4).
“Bueno, mira, es un niño muy inquieto, ¿eh?, y es muy frecuente en los niños de este tipo que a los tres, cuatro años tartamudeen, ¿eh?, Porque es que van muy rápido ellos y no son capaces de articular bien lo que quieren decir, ¿sabes? Eso es muy frecuente y no pasa nada. Se le va a quitar, a no ser que vosotros lo traumaticéis, insistiendo y forzándole, que es como se hacía antiguamente, y se queda tartamudo ya para toda la vida. Vosotros, cuando tú veas que está así un poco más excitado y que le cuesta organizar bien las palabras, tú le dices, 'tranquilo luego me lo cuentas'. Y ya después cuando él esté más tranquilo te lo cuenta. No dejes que nadie de la familia le fuerce” (pediatra 3, consulta 3).
Por el contrario, denominamos prescripción a las recomendaciones sin explicación del objetivo ni explicitación de la cadena causal en que se insertan, como en los ejemplos siguientes:
“Hay que controlar un poco los programas de televisión que ven” (pediatra 1, consulta 3).
“¿Sigue usando chupe, o no? (...) También pronto se lo puedes ir retirando” (pediatra 3, consulta 7).
Los temas de las recomendaciones fueron agrupados en las siguientes categorías generales: prevención secundaria, prevención primaria, promoción de la salud, desarrollo, educación, centrada en los padres y relación familiar, que se articulan en torno a dos ejes: la historia natural de la enfermedad y el desarrollo psicosocial (Tabla 1).
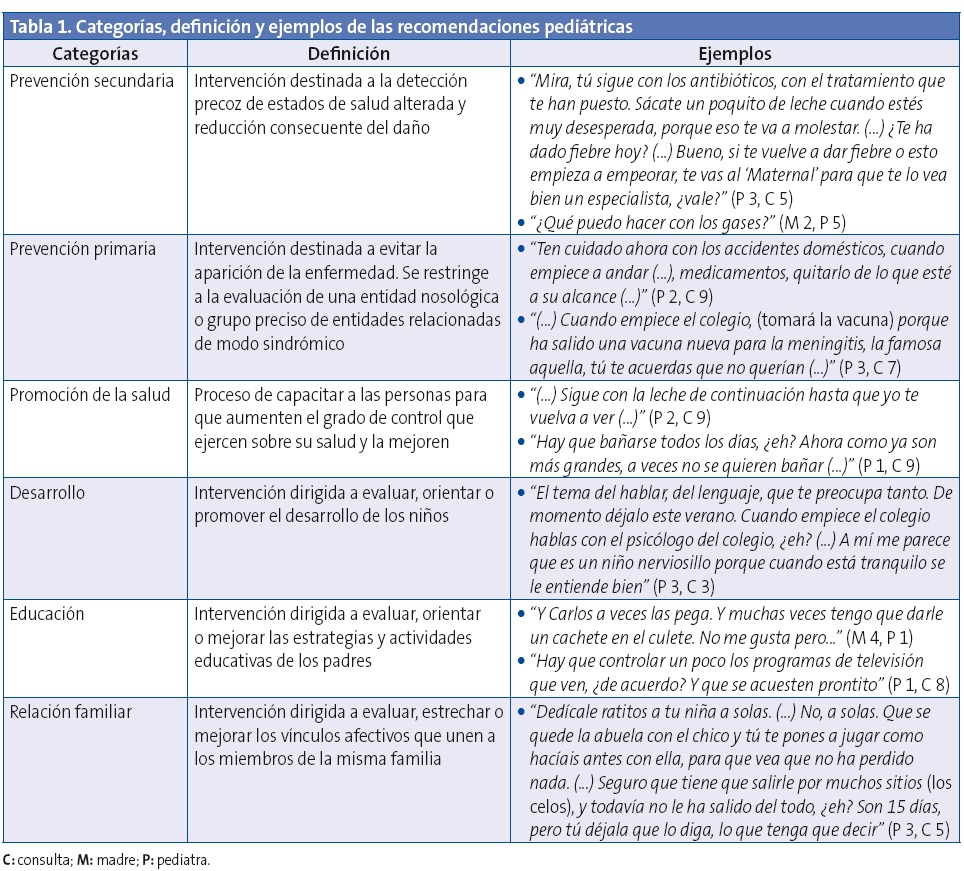
La validez facial (claridad y relevancia) de la lista de categorías puede ser estimada por su definición (Tabla 1). La validez de contenido fue satisfactoria, ya que todos los segmentos del texto trascrito se han incluido en las categorías definidas. El investigador principal y un asistente de investigación entrenado analizaron y codificaron todas las consultas independientemente. Los desacuerdos fueron infrecuentes (<3% de las observaciones) y se resolvieron por consenso.
La codificación, tabulación y presentación gráfica de los datos fue realizada en Excel® y el análisis estadístico en SPSS® v.18. En el análisis estadístico descriptivo utilizamos las siguientes medidas: media (M), desviación típica (DT), coeficiente de variación (CV), mínimo (mín.) y máximo (máx.). En el análisis estadístico inferencial utilizamos las pruebas Chi-cuadrado (Χ2), ANOVA (F), correlación de Pearson (r) y regresión lineal (R2). Las variables independientes consideradas fueron: pediatra, edad y sexo del niño, edad y estudios de la madre.
RESULTADOS
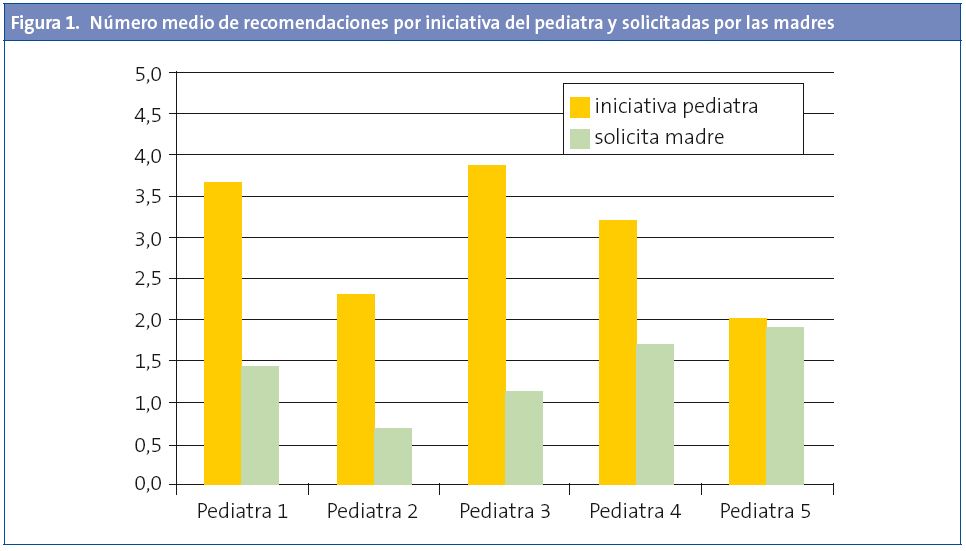
Los pediatras dieron alguna recomendación en casi todas las consultas (46 de 49; 94%). De un total de 214 recomendaciones, 147 (69%) fueron por iniciativa del pediatra y 67 (31%) a petición de las madres. Ello equivale a 4,37 recomendaciones por consulta (DT 2,83, mín. 0, máx. 11), tres dadas por iniciativa del pediatra (DT 2,15, mín. 0, máx. 8) y 1,4 solicitadas por las madres (DT 1,57, mín. 0, máx. 8). En la Fig. 1 observamos una gran variabilidad entre pediatras en la distribución de la iniciativa de las recomendaciones (CV iniciativa pediátrica 24%, CV iniciativa madres 32%, Χ2 107,00; p=0,0009).
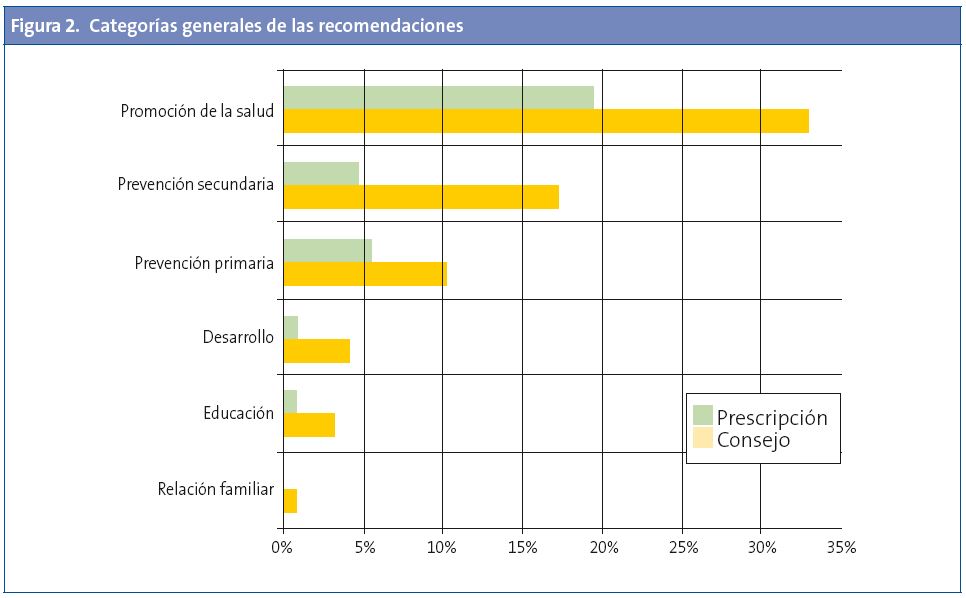
Al analizar los contenidos por categorías generales, se observa que la agenda pediátrica se centra sobre todo en los aspectos biomédicos (Fig. 2). Los pediatras hacen sobre todo recomendaciones acerca de la promoción de la salud (32,87%), prevención secundaria (17,13%) y primaria (10,19%). Desarrollo (4,17%), educación (3,24%) y relación familiar (0,93%) son objeto apenas de recomendaciones esporádicas (Χ2 237,89; p=0,000).
La duración media de las consultas fue de 16,10 minutos (DT 5,72, mín. 6, máx. 24). Existe una diferencia significativa entre pediatras (F 4,55; p=0,004). La duración está intensa y positivamente asociada con el número de recomendaciones, cada tres minutos se produce una recomendación adicional (r 0,556; p=0,00003).
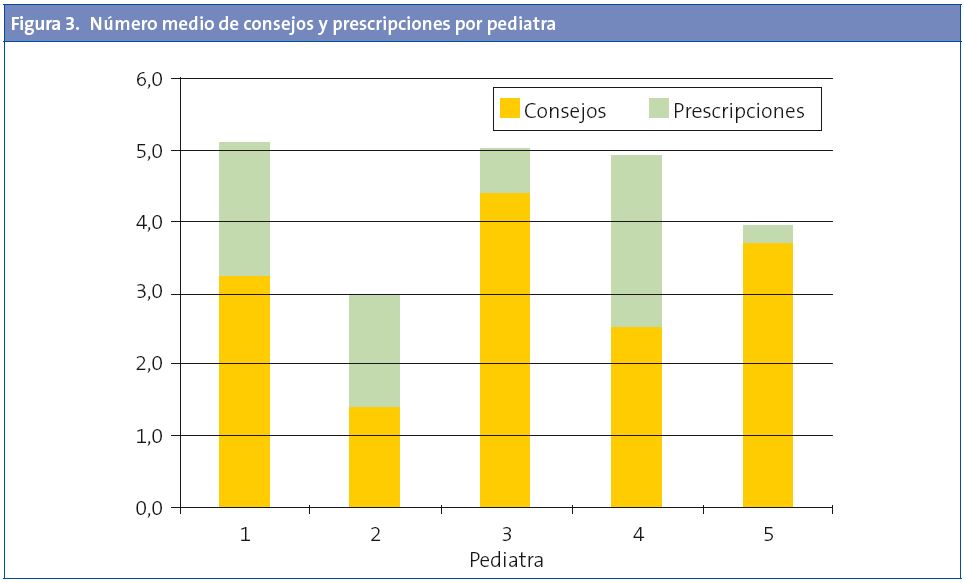
Como referimos anteriormente dentro de las recomendaciones, es importante distinguir entre consejos y prescripciones. Los pediatras utilizaron más el consejo (149/214; 70%) que la prescripción (65/214; 30%) (X2 32,97; p=0,000). En cada consulta se dieron una media de 3,04 consejos (DT 2,51, mín. 0; máx. 9) y 1,33 prescripciones (DT 1,48, mín. 0, máx. 7). El efecto de la duración de la consulta es más pronunciado en el consejo (R2 0,24; p=0,000) que en la prescripción (R20,06;p=0,100).
Existe una gran variabilidad entre pediatras tanto en la media de consejos dados (CV 38,38%) como en la de prescripciones (CV 40,75%) (Fig. 3).
Es más probable que una recomendación sea razonada si ha sido solicitada por la madre, aunque la diferencia no alcanza significación estadística. La relación consejo/prescripción es 3,47 cuando la iniciativa parte de la madre y 1,94 cuando parte del pediatra (X2 2,94; p=0,086).
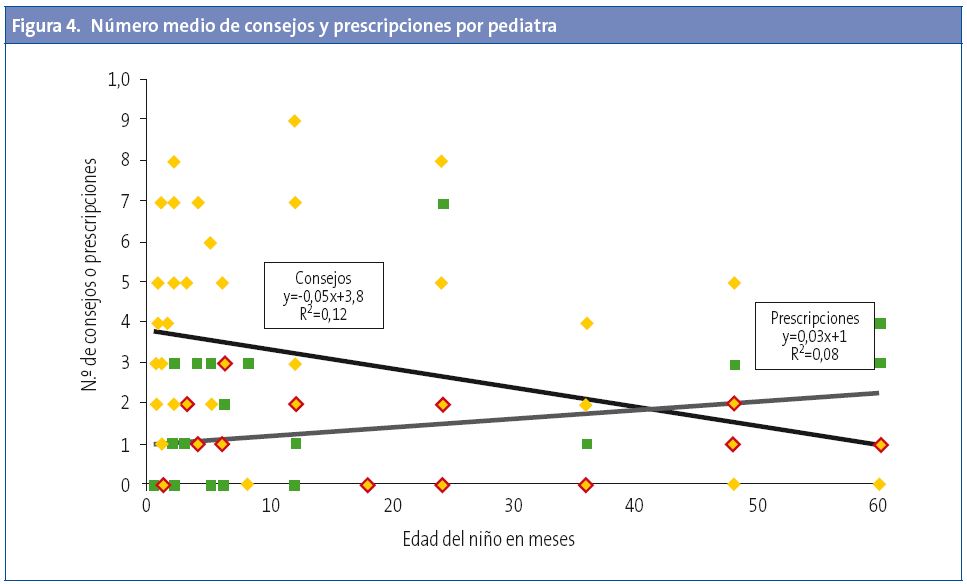
Por otro lado, las rectas de regresión de la Fig. 4 muestran que, a medida que aumenta la edad del niño, se hace más frecuente la prescripción (p=0,048) y menos el consejo (p=0,015). La relación consejo/prescripción se invierte hacia los tres años y medio. Ninguna otra característica del niño ni de la madre se asocia a la cantidad de consejos o prescripciones.
DISCUSIÓN
En las consultas del niño sano observadas, los pediatras dan un número apreciable de recomendaciones. Solo en el 6% de las consultas no se dan recomendaciones. Este dato coincide con el observado en otros estudios28,29. Es sin duda positivo que la mayoría de las recomendaciones sean consejos y no prescripciones. Acompañar las recomendaciones de razonamientos tiene múltiples efectos positivos: mejora la comprensión de su utilidad, incrementa su cumplimiento, eleva la satisfacción, capacita y da seguridad a las mujeres en el desempeño de su rol materno2,20-24.
El hecho de que casi un tercio de las recomendaciones sean solicitadas por las madres, y que en estos casos los pediatras razonen más su respuesta, sugiere que adecuan su discurso a las necesidades maternas. De hecho, dar la oportunidad a los padres de expresar sus dudas y preocupaciones es de primordial importancia en la efectividad y calidad de los cuidados preventivos infantiles30,31. Tanto la oportunidad de expresar dudas como la de recibir consejo fueron independientes del nivel de escolaridad de la madre, lo que sugiere que los pediatras dirigen su actividad en el sentido de neutralizar los efectos de la desigualdad social y constituye un aspecto muy positivo de su práctica profesional.
La duración de las consultas, 16 minutos, está dentro de los valores recomendados18,28,32,33 y se relaciona positiva e intensamente con la cantidad de consejos y sin afectar apenas a la de prescripciones. Ello sugiere que, hasta un determinado límite, la duración de la consulta se relaciona con su calidad. De hecho, algunos autores consideran que no es posible realizar en tan pocos minutos la larga lista de actos y consejos médicos que integran el programa del niño sano8,31.
A medida que los niños se van haciendo mayores, aumentan las prescripciones y disminuyen tanto la duración de la consulta como los consejos. Este empobrecimiento de contenidos del programa ha sido también observado en otros estudios9,12,14 y está probablemente relacionado con el hecho de que la agenda pediátrica esté tan centrada en los aspectos biomédicos. Los aspectos psicosociales, la relación familiar y la educación son abordados apenas esporádicamente y son estos los temas que se van haciendo más importantes a medida que el niño crece. Creemos que existe aquí una clara oportunidad de mejora, ya que sabemos que estos problemas son frecuentes y que las familias desean recibir consejo pediátrico sobre ellos8,16,19,35.
La formación, muy centrada en los aspectos biológicos del proceso salud-enfermedad, tiene también como consecuencia un entendimiento de la comunicación con los pacientes y las familias casi exclusivamente basado en las características personales de los pediatras. Solo recientemente se está generalizando el entendimiento de la relación médico-paciente como un ámbito técnico susceptible de aprendizaje y entrenamiento21-25.
Existe más heterogeneidad de la esperada en un grupo profesional con un patrimonio técnico-científico común en las principales variables estudiadas: consejos, prescripciones, facilitación del discurso materno y duración de la consulta. Aunque todos los pediatras usan más el consejo que la prescripción, algunos casi nunca prescriben, esto es, casi nunca dan recomendaciones sin razonar, y otros prescriben más que aconsejan.
La generalización de los resultados de este estudio está limitada por el reducido tamaño de la muestra de pediatras y por su selección no aleatoria. No obstante, la muestra de las madres atendidas por cada pediatra puede ser considerada representativa de sus usuarias. Por otro lado, en un ámbito en que la mayoría de los estudios utilizan cuestionarios aplicados a pediatras o padres, el método de observación directa y grabación de las consultas permite estudiar el contenido real de las consultas en vez de la opinión de los intervinientes, por lo que consideramos que es una fortaleza de nuestro estudio.
Nuestros datos sugieren que existen estilos pediátricos diferentes cuyas características y efectos deben ser investigados para fundamentar estrategias de formación pediátrica adaptadas a la práctica profesional en Atención Primaria.
AGRADECIMIENTOS
Este trabajo fue parcialmente financiado por la Fundação para a Ciência e Tecnologia (FCT), Portugal.
CONFLICTO DE INTERESES
Los autores declaran no presentar conflictos de intereses en relación con la preparación y publicación de este artículo.
ABREVIATURAS: CV: coeficiente de variación • DT: desviación típica • F: ANOVA • M: media • máx.: máximo • mín.: mínimo • r: correlación de Pearson • R2: regresión lineal • Χ2: Chi-cuadrado.
BIBLIOGRAFÍA
- Berkule-Silberman SB, Dreyer BR, Huberman HS, Klass PE, Mendelsohn AL. Sources of parenting information in low SES mothers. Clin Pediatr. 2010;49:560-8.
- Nunes C, Ayala A. ¿Qué piensan las madres sobre el programa de seguimiento de la salud infantil? Rev Pediatr Aten Primaria. 2007;9(35):411-25.
- Hidalgo MV, Menéndez S, López I, Sánchez J. Nacer a la vida: un programa de apoyo y formación durante la transición a la maternidad y la paternidad. Infancia y Aprendizaje. 2004;27:407-15.
- Young K, Davis K, Schoen C, Parker S. Listening to parents: a national survey of parents with young children. Arch Pediatr Adolesc Med. 1998;152:255-62.
- Schuster MA, Duan N, Regalado M, Klein DJ. Anticipatory guidance: what information do parents receive? What information do they want? Arch Pediatr Adolesc Med. 2000;154:1191-8.
- Cheng T, Savageau J, Bigelow C, Charney E, Kumar S, DeWitt T. Assessing mothers’ attitudes about the physician’s role in child health promotion. Am J Public Health. 1996;86:1809-12.
- Dirección General de Atención Primaria y Promoción de la Salud. Guía para la salud infantil. Sevilla: Junta de Andalucía e Consejería de Salud; 1990.
- Schor EL. Rethinking well-child care. Pediatrics. 2004;114:210-6.
- Nunes C. Pediatricians’ ideas about child development and education. Psicologia: Reflexão e Crítica. 2011;24(2):765-72.
- Cheng TL, DeWitt TG, Savageau JA, O’Connor KG. Determinants of counseling in primary care pediatric practice. Physicians attitudes about time, money, and health issues. Arch Pediatr Adolesc Med. 1999;153:629-35.
- Nunes C, Ayala M. ¿De qué hablan los pediatras y las madres en la consulta de seguimiento de la salud infantil? An Pediatr (Barc). 2011;75(4):239-46.
- Olson LM, Inkelas M, Halfon N, Schuster MA, O’Connor KG, Mistry R. Overview of the content of health supervision for young children: reports from parents and pediatricians. Pediatrics. 2004;113:1907-16.
- Wissow LS, Larson S, Anderson J, Hadjiisky E. Pediatric residents’ responses that discourage discussion of psychosocial problems in primary care. Pediatrics. 2005;115:1569-78.
- Bethell C, Reuland CH, Halfon N, Schor EL. Measuring the quality of preventive and developmental services for young children: national estimates and patterns of clinicians’ performance. Pediatrics. 2004;113:1973-83.
- Almeida PVB, Zanolli ML. O papel do pediatra no PSF-Paidéia de Campinas (SP). Cien Saude Colet. 2011;16(Supl. 1):1479-88.
- Tanner L, Stein MT, Olson LM, Radecki L, Frintner MP. Reflections on well-child care practice: a national study of pediatric clinicians. Pediatrics. 2009;124:849-57.
- American Academy of Pediatrics. The new morbidity revisited: a renewed commitment to the psychosocial aspects of pediatric care. Pediatrics. 2001;108:1227-30.
- Galuska DA, Fulton JE, Powell KE, Burgeson CR, Pratt M, Elster A, et al. Pediatrician counseling about preventive health topics: results from the Physicians’ Practices Survey, 1998-1999. Pediatrics. 2002;109:E83-3.
- Radecki L, Olson LM, Frintner MP, Tanner JL, Stein MT. What do families want from well-child care? Including parents in the rethinking discussion. Pediatrics. 2009;124:858-65.
- Hart CN, Kelleher KJ, Drotar D, Scholle SH. Parent-provider communication and parental satisfaction with care of children with psychosocial problems. Patient Educ Couns. 2007;68:179-85.
- Nunes C, Ayala A. Communication techniques used by pediatricians in the well-child program visits: A pilot study. Patient Educ Couns. 2010;78:79-84.
- Ammentorp J, Sabroe S, Kofoed P, Mainz J. The effect of training in communication skills on medical doctors’ and nurses’ self-efficacy. A randomized controlled trial. Patient Educ Couns. 2007;66:270-7.
- Worchel FF, Prevatt BC, Miner J, Allen M, Wagner L, Nation P. Pediatrician’s communication style: relationship to parent’s perceptions and behaviors. J Pediatr Psychol. 1995;20:633-44.
- Nobile C, Drotar D. Research on the quality of parent-provider communication in pediatric care: Implications and recommendations. J Dev Behav Pediatr. 2003;24(4):279-90.
- Clayman ML, Wissow LS. Pediatric residents’ response to ambiguous words about child discipline and behaviour. Patient Educ Couns. 2004;55:16-21.
- Baker LH, O’Connell D, Platt FW. What else? Setting the agenda for the clinical interview. Ann Intern Med. 2005;143:766-70.
- Borrell F. Manual de entrevista clínica. Barcelona: Doyma; 1988.
- Goldstein E, Dworkin PH, Bernstein B. Time devoted to anticipatory guidance during child health supervision visits: how are we doing? Amb Child Health. 1999;5:113-20.
- Manning KM, Ariza AJ, Massimino TK, Binns HJ. Health supervision visits of very young children: Time addressing 3 key topics. Clin Pediatr. 2009;48:931-8.
- Glascoe FP. Evidence-based approach to developmental and behavioural surveillance using parents' concerns. Child Care Health Dev. 2000;26:137-49.
- Sand N, Silverstein M, Glascoe FP, Gupta VB, Tonniges TP, O’Connor KG. Pediatricians’ reported practices regarding developmental screening: Do guidelines work? Do they help? Pediatrics. 2005;116(1):174-9.
- Cox ED, Smith MA, Brown RL, Fitzpatrick MA. Effect of gender and visit length on participation in pediatric visits. Patient Educ Couns. 2007;65:320-8.
- Halfon N, Inkelas M, Mistry R, Olson LM. Satisfaction with health care for young children. Pediatrics. 2004;113:1965-72.
- Yarnall KSH, Pollak KI, Østbye T, Krause KM, Michener JL. Primary Care: Is there enough time for prevention? Am J Public Health. 2003;93(4):635-41.
- Combs-Orme T, Nixon BH, Herrod HG. Anticipatory guidance and early child development: Pediatrician advice, parent behaviors, and unmet needs as reported by parents from different backgrounds. Clin Pediatr. 2011;50:729-37.
CONFLICTO DE INTERESES






