Attention deficit hyperactivity disorder (ADHD) in schoolchildren aged 6 to 17 years
Leónidas José Llanos Lizcanoa, Darwin José García Ruiza, Henry J. González Torresb, Pedro Puentes Rozoc
aResidente de Psiquiatría. Facultad de Ciencias de la Salud. Universidad Simón Bolívar. Barranquilla. Colombia.
bFacultad de Ciencias de la Salud. Universidad Simón Bolívar. Barranquilla. Colombia.
cGrupo de Neurociencias del Caribe. Unidad de Neurociencias Cognitivas. Universidad del Atlántico-Universidad Simón Bolívar. Barranquilla. Colombia.
Correspondence: LJ Llanos. E-mail: lllanos13@unisimon.edu.co
Reference of this article: Llanos Lizcano LJ, García Ruiz DJ, González Torres HJ, Puentes Rozo P. Attention deficit hyperactivity disorder (ADHD) in schoolchildren aged 6 to 17 years. Rev Pediatr Aten Primaria. 2019;21:e101-e108.
Published in Internet: 01-08-2019 - Visits: 32290
Abstract
Objective: we aimed to establish the prevalence of attention-deficit hyperactivity disorder (ADHD) in schoolchildren aged 6 to 17 years in Barranquilla, to obtain an epidemiological perspective of this disorder in the Caribbean region of Colombia.
Materials and methods: we selected 383 children enrolled in a single school and administered screening tests (symptoms checklist and BASC). In children with scores that suggested the presence of abnormalities, we scheduled another assessment by means of a structured interview (MINI).
Results: of the 383 children that underwent the initial assessment, 178 exhibited abnormalities, of which 59 (15%) received a final diagnosis of ADHD (38 male and 21 women, corresponding to a 2:1 ratio). The distribution by subtypes was 7.3% combined, 5% inattentive and 3.1% hyperactive. Overall, 23% of the children in the sample had some form of neuropsychiatric disorder, and we found that the inattentive type was significantly associated with agoraphobia and episodes of depression and the hyperactive type with oppositional defiant disorder and anxiety disorder, while in the combined type, depression was associated with an increased risk of suicide.
Conclusions: the prevalence of ADHD in Barranquilla was similar to the prevalence reported in other regions of Colombia, both overall and for each of the subtypes, and in its distribution by sex or comorbidities. These proportions were not associated to psychosocial factors, which supports the hypothesis of a multifactorial aetiology of ADHD.
Keywords
● Attention-deficit hyperactivity disorder ● Behavioral disorders ● Childhood neuropsychiatric disorders ● Neurodevelopmental disordersINTRODUCTION
Attention-deficit hyperactivity disorder (ADHD) is a prevalent neurologic syndrome characterised by a pattern of hyperactivity, impulsive behaviour and impaired attention considered abnormal for the developmental stage of the child.1 It is one of the most frequent diagnosis in children and adolescents and it is the most common diagnosis in young adults.2 There are no accurate data on its prevalence, but it is estimated at 2% to 12% in children2-7 and 2.5% to 5% in adults.5-11
The regions with the broadest variability in prevalence are Africa and Latin America, which also have the greatest prevalences, usually high above the mean.12 According to the Liga Latinoamericana para el Estudio del TDAH (Latin American League for the Study of ADHD), there are 36 million people affected by ADHD in Latin America, and less than one fourth are receiving adequate care.13
In Colombia, based on the study by Hoai Danh Pham published in 2015, which cites a 2001 article by doctor Pineda, Colombia is the country with the highest prevalence of ADHD in the world, amounting to 17.1% of the population.6,14 This was confirmed by Vélez in 2012, who described that the prevalence in Colombia was higher compared to other countries, and expressed the need to carry out more structured studies to standardise criteria in order to establish the actual prevalence in Colombia, as the figures reported by different studies conducted in different cities and with different methods vary widely.15
This disorder involves a disturbance of healthy development in affected individuals and is associated with significant problems in the family13; it is known that up to 50% of children with ADHD have poor relations with their peers and that up to 70% in the third grade do not have friends do to their severe limitations in participating harmoniously in the social interactions characteristic of this age.16 When family members of individuals with ADHD have been asked about the difficulties and disabilities that may be associated with the disorder, they have described a negative impact of ADHD on school life, everyday activity, social interaction and family relationships, in addition to self-esteem.17 These disturbances in social and academic development are among the main reasons why ADHD is associated with a higher prevalence of drug use and abuse in the ADHD population in comparison with controls without ADHD.18
Attention-deficit hyperactivity disorder is important because it manifests in childhood with a series of disturbances in individual, academic and social functioning that lead individuals at the stage when their personality and identity are being shaped to interact poorly with society, bringing a stigma that, without adequate management, may eventually result in marginalization.16,19-24 While different studies have demonstrated that these patients exhibit multiple qualities in creative and artistic subject areas,25 it is also important to highlight the role played by schools with standardised and rigid curricula in comparison to schools that are more specialised in a more progressive education with emphasis in the arts with more stimulating curricula and flexible classrooms and schedules that improve the adaptation of these children, an approach that is not common in our region.
Therefore, early intervention in these children and adolescents is of vital importance in order to decrease the negative repercussions in adolescence and adulthood, which manifest in the form of disorganization in school work, poor performance in school and work, difficulty completing tasks and working independently, high-risk behaviours, low self-esteem due to failure in several areas of life, increased risk of substance use or early sexual debut, among others.1
For this reason, we undertook an initial approximation to the epidemiology of ADHD at the local level, taking into account the social and cultural characteristics of our population, which differ significantly from those of populations in inland Colombia.26,27 In addition, we used different diagnostic tests to try to identify probable cases, and made the final diagnosis by means of a structured clinical interview, the Mini-International Neuropsychiatric Interview (MINI), thus increasing the validity and accuracy of diagnosis by not basing it exclusively on questionnaires and scales, which, as we already noted, are subject to interrater variability based on the application of different diagnostic criteria.
Our aim is for this first study to provide a local baseline allowing replication in similar studies conducted in other cities and to open the door for and justify broader studies with larger samples capable of detecting correlations with a greater number of more risk factors, associated disorders and comorbidities, with the ultimate purpose of developing specific guidelines for the population that could be included in the planning of public policies targeting early childhood so that the most vulnerable population can be managed from a multidisciplinary and therefore comprehensive approach, thus reducing the harm and negative impact on affected individuals.15
METHODS
We conducted a cross-sectional, prospective, quantitative analytical study. The setting of the study was a school in Barranquilla (Colombia). We selected the sample of children to be evaluated by simple randomization, obtaining a sample of 383 children, of who 178 exhibited neurobehavioural changes that justified assessment by MINI after obtaining the informed consent of parents and with agreement of the children. We excluded children with a previous diagnosis or undergoing treatment for any form of developmental or psychiatric disorder.
Once the parents had signed the informed consent and the children had assented to participation, the assessment was carried out as follows: to determine whether there was any form of neurodevelopmental or behavioural abnormality, children were assessed by the consecutive administration of the Behavior Assessment System for Children (BASC) and the ADHD symptom checklist.14,28-31
Children that exhibited abnormalities both in the BASC and the symptom checklist underwent a short structured diagnostic interview lasting an average of 15 minutes following the protocol of the MINI for children and adolescents (MINI KID), Spanish version 5.0.0, based on the DSM-IV.
We arranged the results of the BASC and ADHD symptom checklist and the results of the MINI in a table, calculating measures of central tendency (observed frequency, mean and standard deviation), by ADHD subtype. We also analysed the association between sex, age group and ADHD subtype by means of the χ2 test, and performed a simple correspondence analysis comparing ADHD subtypes and the presence of comorbidities. The analysis was performed with the statistical package R-CRAN. The study was overseen by the Bioethics Committee.
RESULTS
We start by presenting the sociodemographic characteristics of the children that participated in the study. The mean age was 11 ± 3 years, 52.75% were male (n = 91), 60.11% were aged 6 to 11 years (n = 107), and 15% (confidence interval [CI]: 12 to 18) met the criteria for diagnosis of ADHD, as can be seen in Table 1.
| Table 1. Prevalence of ADHD in the sample | |||
|---|---|---|---|
| Absolute frequency | Relative frequency | Confidence interval | |
| Healthy | 205 | 54% | 49-59% |
| Healthy in MINI | 87 | 23% | IC 19-27% |
| ADHD | 59 | 15% | IC 12-19% |
| Another diagnosis | 32 | 8% | IC 6-11% |
| Total | 383 | 100% | - |

We found that 8% (CI: 6 to 10) of individuals that required assessment by means of the MINI exhibited criteria for other neuropsychiatric disorders. Children with ADHD or other diagnoses added up to 23%, which means that nearly one fourth of the children evaluated had a mental health diagnosis.
Of the group that met the criteria for ADHD, 62.7% (n = 37) were aged 6 to 11 years, with a statistically significant difference in age (p < 0.01). We also found a significant predominance of the male sex (64.4%; p < 0.01).
As for the distribution of diagnoses by subtype, we found that in the group of children diagnosed with ADHD (n = 59), the prevalence of the hyperactive type was 20%, the prevalence of inattentive type 32% and the prevalence of combined type 47%. We did not find a significant association between sex and ADHD subtype (χ2: 1.38; p > 0.05) or age group and ADHD subtype (χ2: 0.71; p > 0.05).
| Table 2. Frequency distribution of ADHD subtypes by sex and age group | |||||
|---|---|---|---|---|---|
| Sociodemographic variables | ADHD subtype | Total | |||
| Hyperactive | Inattentive | Combined | |||
| Sex | Male | 8 | 14 | 16 | 38 |
| Female | 4 | 5 | 12 | 21 | |
| Age group | 6-11 years | 8 | 13 | 16 | 37 |
| 12-18 years | 4 | 6 | 12 | 22 | |

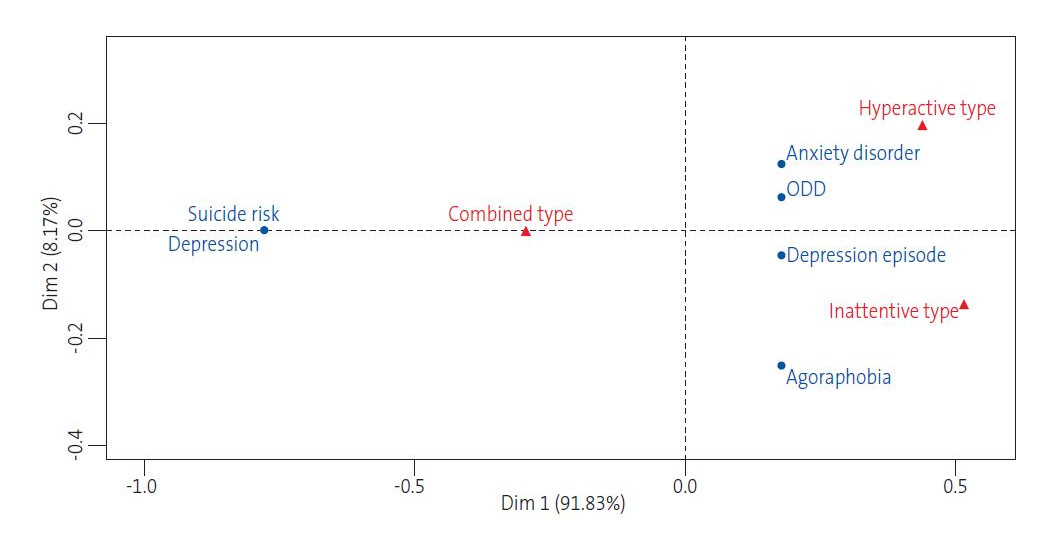
The comorbidities associated to the hyperactive type were anxiety and oppositional defiant disorder, while the inattentive type was mainly associated with episodes of depression and agoraphobia. We ought to note that the combined type appeared in the middle of the scatter plot, evincing a clear combination of the other 2 subtypes (hyperactive and inattentive). In children with combined type, we found that depression was associated with an increased risk of suicide.
| Figure 1. Simple correspondence analysis of the association between attention-deficit hyperactivity disorder subtypes and comorbidities |
|---|
 |

We evaluated other characteristics that ought to be highlighted: none of the students reported having intentionally set fires, deceived other people to steal their money or get their belongings, robbed others using weapons or intimidation, forced or coerced anyone to have sex, or being cruel to animals or enjoying causing them suffering.
DISCUSSION
Prevalence studies are very important, especially in areas where there are gaps in knowledge. Although ADHD is one of the most frequent neurodevelopmental disorders in childhood, the epidemiological data in the medical literature is insufficient to establish the prevalence with certainty, which is why our study focused on this aspect.1,2 In Colombia, few studies have analysed the prevalence of ADHD, and those published focused on the inland population of the country; there are still no data on the Caribbean region of Colombia allowing us to assess the epidemiology of this disorder and to make comparisons with the findings of other authors domestically and abroad, so with our study we aimed at making an initial approximation to estimate the prevalence of ADHD in schoolchildren in Barranquilla and to spur future research on this subject.
The prevalence of ADHD varies across the world, with some authors estimating it at approximately 7.2%32 and other studies ranges as broad as 4% to 13.3%.3,33 In Colombia, the prevalence diverges from what has been generally reported worldwide, as the evidence published to date shows a prevalence of 15% to 17%.1,14 Our findings were consistent with those of studies performed previously in Colombia, which corroborates the 15% prevalence found in the sample under study, evidence that is indicative of a high risk of mental health disorders in school children in the city of Barranquilla and in Colombia overall.
When it came to the sex distribution, we found that ADHD was more frequent in male than female students, with a ratio of 2:1, which was consistent with the findings worldwide and in other Colombian populations.1,14,34 Similarly, the prevalence by age group found in our study found a higher proportion of ADHD in younger children (6 to 11 years), which reached 62.7% compared to the prevalence of 37.3% in children aged more than 12 years. These findings are similar to those reported by other authors,7 and some researchers have attributed them to changes in brain maturation, for according to the experts patients with ADHD have levels of cortical maturation and thickening that are delayed by 2 to 3 years compared to children without ADHD.35
In a study of the population of Sabaneta in Antioquía in 2005, Cornejo JW et al. described that the most frequent subtype was the combined type, followed by the inattentive type and then the hyperactive type, which was consistent with the findings of our study, with a similar distribution and proportions (7.3%, 5.0% and 3.1%, respectively).1
Of the 16 psychiatric disorders included in the analysis as comorbidities, based on the selection of the structured interview (MINI), we found that the most prevalent was oppositional defiant disorder, corresponding to a proportion of 44.06%, which we found was a common feature in our review of the medical literature21,36 and has a significant impact, as it is one of the most important factors associated with poor outcomes in ADHD. This disorder is characterised by hostility toward authority figures, disobedience and confrontational attitudes that result in a series of disturbances in the family, school and social life at large that may ultimately lead to criminal and high-risk behaviours.
Mood disorders were the second most frequent comorbidity in children with ADHD, present in 30.5% of the total, which was similar to the findings of the study conducted by Artigas-Pallares in 2003. In an article published in 2007, Birmaher described that ADHD is frequently associated with mood disorders. The causes of the association of these disorders and ADHD has not been elucidated. Some authors propose that problems in the family, school and social relationships, such as arguments with parents and other relatives, difficulties interacting with peers and poor academic performance, are associated with decreases in self-esteem.13 Other authors consider that it is the genetic and molecular changes characteristic of ADHD that underlie the association with mood disorders, with the possible contribution of environmental factors.37
Considering that the most frequent psychiatric disorders in the paediatric population are anxiety disorders, we ought to highlight that in our study we found a prevalence of anxiety as a comorbidity of ADHD of 20.3%, a high percentage that could be partly explained, in addition to what we just mentioned, by the genetic hypothesis that while these 2 disorders are inherited separately, they do potentiate one another.1
At present there are no known biological markers that can be used to diagnose ADHD with certainty, and the use of clinical tests or evaluations is not considered objective enough, as there is a risk of error or inaccuracy in making the diagnosis, all of which makes it difficult to compare the prevalences of ADHD reported by different studies conducted at the national and international levels.1,22,38
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article. This article is part of the dissertation for the degree in the specialty of Psychiatry of Leónidas José Llanos Lizcano and Darwin José García Ruiz. It was funded with the authors’ own resources.
ABBREVIATIONS
ADHD: attention-deficit hyperactivity disorder · BASC: Behavior Assessment System for Children · CI: confidence interval · MINI: Mini-International Neuropsychiatric Interview.
REFERENCES
- Cornejo Ochoa JW, Osío Uribe O, Sánchez Mosquera Y, Carrizosa J, Sánchez,Grisales H, et al. Prevalencia del trastorno por déficit de atención-hiperactividad en niños y adolescentes. Rev Neurol. 2005;40:716.
- Parker A, Corkum P. ADHD Diagnosis: as simple as administering a questionnaire or a complex diagnostic process? J Atten Disord. 2012;20:478-86.
- Polanczyk G, De Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942-8.
- Russell G, Rodgers LR, Ukoumunne OC, Ford T. Prevalence of parent-reported ASD and ADHD in the UK: Findings from the millennium cohort study. J Autism Dev Disord. 2014;44:31-40.
- Wolraich ML, McKeown RE, Visser SN. The prevalence of ADHD: its diagnosis and treatment in four school districts across two states. J Atten Disord. 2014;18:563-75.
- Pham HD, Nguyen HBH, Tran DT. Prevalence of ADHD in primary school children in Vinh Long, Vietnam. Pediatr Int. 2015;57:856-9.
- Huang CL, Weng S, Ho C. Gender ratios of administrative prevalence and incidence of attention-de fi cit/hyperactivity disorder (ADHD) across the lifespan: a nationwide population-based study in Taiwan. Psychiatry Res. 2016;244:382-7.
- Gao Q, Qian Y, He X, Sun L, Chang W, Li Y. Childhood predictors of persistent ADHD in early adulthood : Results from the fi rst follow-up study in China. Psychiatry Res. 2015;230:905-12.
- Demontis D, Walters RK, Martín J, Mattheisen M, Als TD, Agerbo E, et al. Discovery of the first genome-wide significant risk loci for ADHD. Nat Genet. 2019;51:63-75.
- Marwaha S, Thompson A, Bebbington P. Adult attention deficit hyperactivity symptoms and psychosis: Epidemiological evidence from a population survey in England. Psychiatry Res. 2015;229:49-56.
- Smalley SL, Loo SK, Hale TS. Mindfulness and attention deficit hyperactivity disorder. J Clin Psychol. 2009;65:1087-98.
- Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43:434-42.
- De la Peña F, Palacio J, Barragán E. Declaración de Cartagena para el Trastorno por Déficit de Atención con Hiperactividad (ADHD): rompiendo el estigma. Rev Ciencias Salud. 2010;8:93-8.
- Pineda DA, Lopera F, Henao GC, Palacio JD, Castellanos FX. Confirmación de la alta prevalencia del trastorno por déficit de atención en una comunidad colombiana. Rev Neurol. 2001;32:217-22.
- Vélez-Álvarez C, Vidarte Claros JA. Trastorno por déficit de atención e hiperactividad (ADHD), una prolematica a abordar en la política pública de primera infancia en Colombia. Rev Salud Pública. 2012;14:113-28.
- Wehmeier PM, Schacht A, Barkley RA. Social and emotional impairment in children and adolescents with adhd and the impact on quality of life. J Adolesc Heal. 2010;46:209-17.
- Caci H, Asherson P, Donfrancesco R. Daily life impairments associated with childhood/adolescent attention-deficit/hyperactivity disorder as recalled by adults: results from the European Lifetime Impairment Survey. Eur Psychiatry. 2014;29:316-23.
- Biederman J, Wilens TE, Mick E, Faraone SV, Spencer T. Does attention-deficit hyperactivity disorder impact the developmental course of drug and alcohol abuse and dependence? Biol Psychiatry. 1998;44:269-73.
- Salmeron PA. Childhood and adolescent attention-deficit hyperactivity disorder: Diagnosis, clinical practice guidelines, and social implications. J Am Acad Nurse Pract. 2009;21:488-97.
- Abikoff H, Hechtman L, Klein RG. Symptomatic improvement in children with ADHD Treated with long-term methylphenidate and multimodal psychosocial treatment. J Am Acad Child Adolesc Psychiatry. 2004;43:802-11.
- Barra FE de la, Vicente B, Saldivia S, Melipillan R. Epidemiology of ADHD in Chilean children and adolescents. Atten Defic Hyperact Disord. 2013;5:1-8.
- Artigas Pallarés J. Comorbilidad en el trastorno por déficit de atención/hiperactividad. Rev Neurol. 2003;36:68-78.
- Yoshimasu K, Barbaresi WJ, Colligan RC. Childhood ADHD is strongly associated with a broad range of psychiatric disorders during adolescence: a population-based birth cohort study. J Child Psychol Psychiatry Allied Discip. 2012;53:1036-43.
- Hong SB, Kim JW, Choi BS. Blood manganese levels in relation to comorbid behavioral and emotional problems in children with attention-deficit/hyperactivity disorder. Psychiatry Res J. 2014;220:418-25.
- Cramond B. Attention-deficit hyperactivity disorder and creativity - what is the connection? J Creat Behav. 1994;28:193-210.
- Song J, Leventhal BL, Koh Y. Cross-cultural aspect of behavior assessment system for Children-2, Parent Rating Scale-Child: standardization in Korean children. Yonsei Med J. 2017;58:439-48.
- Timimi S, Taylor E. ADHD is best understood as a cultural construct. Br J Psychiatry. 2004;184:8-9.
- Pineda DA, Lopera F, Palacio JD, Ramírez D, Henao GC. Prevalence estimations of attention-deficit/hyperactivity disorder: differential diagnoses and comorbidities in a Colombian sample. Int J Neurosci. 2003;113:49-71.
- Pineda D a, Kamphaus RW, Mora O, Restrepo MA, Puerta IC, Palacio LG, et al. Sistema de evaluación multidimensional de la conducta. Escala para padres de niños de 6 a 11 años, versión colombiana. Rev Neurol. 1999;28:672-81.
- Pineda D, Acosta J, Cervantes-Henríquez M. Conglomerados de clases latentes en 408 miembros de 120 familias nucleares de Barranquilla con un caso índice afectado de trastorno de atención hiperactividad (ADHD). Acta Neurol Col. 2016;32:275-84.
- Pineda DA, Henao GC, Puerta IC, Mejía SE. Uso de un cuestionario breve para el diagnóstico de deficiencia atencional. Rev Neurol. 1999;28:365-72.
- Thomas R, Sanders S, Doust J, Beller E. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135:e994-1001.
- Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490-9.
- Barrios O, Matute E, Ramírez-Dueñas ML, Chamorro Y, Trejo S, Bolaños L. Características del trastorno por déficit de atención e hiperactividad en escolares mexicanos de acuerdo con la percepción de los padres. Suma Psicol. 2016;23:101-8.
- Shaw P, Eckstrand K, Sharp W. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc Natl Acad Sci U S A. 2007;104:19649-54.
- Joffre-Velázquez VM, García-Maldonado G, Martínez-Perales G. Trastorno por déficit de la atención e hiperactividad. Un estudio descriptivo en niños mexicanos atendidos en un hospital psiquiátrico. Bol Med Hosp Infant Mex. 2007;64:153-60.
- Dark C, Homman-Ludiye J, Bryson-Richardson RJ. The role of ADHD associated genes in neurodevelopment. Dev Biol. 2018;438:69-83.
- Gorga M. Trastorno por déficit de atención con hiperactividad y el mejoramiento cognitivo. ¿Cuál es la responsabilidad del médico? Rev Bioét. 2013;21:241-50.






