Vol. 19 - Num. 76
Original Papers
Is emergency department use appropriate during the neonatal period?
Rosa Fornes Vivasa, Rocío Mustienes Bellotb, Agustín Navarro Juanesc, Luis Robledo Díazd, Eva Carvajal Rocae
aServicio de Urgencias de Pediatría. Hospital Católico Universitario Casa de Salud. Valencia. España.
bFacultad de Medicina y Odontología. Universidad Católica San Vicente Mártir . Valencia. España.
cServicio de Urgencias. Hospital Marina Alta. Denia. Valencia. España.
dDepartamento de Sociología y Antropología Social. Facultad de Ciencias Sociales. Universidad de Valencia. Departamento de Gestión. Hospital Católico Universitario Casa de Salud. Valencia. España.
eDepartamento de Pediatría, Ginecología y Obstetricia. Facultad de Enfermería, Medicina y Odontología. Universidad Católica San Vicente Mártir. Valencia. España.
Correspondence: R Fornes. E-mail: rfornes@comv.es
Reference of this article: Fornes Vivas R, Mustienes Bellot R, Navarro Juanes A, Robledo Díaz L, Carvajal Roca E. Is emergency department use appropriate during the neonatal period? Rev Pediatr Aten Primaria. 2017;19:301-9.
Published in Internet: 11-10-2017 - Visits: 22144
Abstract
Introduction: a high proportion of newborn visits to emergency departments correspond to non-urgent conditions and concerns regarding newborn care. Our aim was to assess the appropriate of emergency department use in newborns.
Materials and methods: analysis of discharge summaries of newborns that attended the emergency department of the Hospital Marina Salud de Denia (Alicante, Spain) in year 2014 and the appropriateness of emergency department use based on newly established criteria: hospital admission, referral, triage and diagnostic testing.
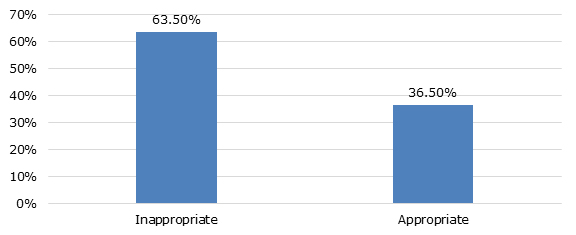
Results: emergency services were used by newborns for conditions considered non-urgent, crying, irritability or malaise (32.08%), and vomiting or regurgitation of the newborn (13.21%), and the most frequent discharge diagnosis was normal health (20%). Based on the appropriateness criteria established for the use of neonatal emergency services, 63.50% of the reasons for neonatal visits were inappropriate.
Conclusions: most neonatal visits were categorised as inappropriate use of emergency services and should therefore have been managed in primary care.
Keywords
● Emergency medical services ● Medical overuse ● NewbornINTRODUCTION
In recent years, there has been an increase in the demand for emergency department services.1,2 Newborns are subpopulation with a high rate of emergency department use, frequently with the purpose of obtaining information of basic newborn care or for non-urgent conditions that could have been managed at the primary care (PC) level.3,4
We conducted a broad literature review and identified the lines of research that have been established to approach the subject of newborn management, observing that published studies have mainly aimed at describing the most frequent reasons that newborns visit emergency departments and the associated socioeconomic factors.5 Thus, the aim of our study was to analyse whether the use of emergency services was appropriate.
The definition of a medical emergency is an acute illness or injury that poses an immediate risk to life and requiring immediate treatment.5 This definition diverges from what parents and relatives of paediatric patients consider constitutes and emergency, and excludes nearly two thirds of emergency visits.
The WHO5 defines inappropriate use of emergency services any situation that is not a life-threatening emergency or requires the use of diagnostic or therapeutic resources unavailable at the PC level.
Some authors6 propose to categorise emergency department visits as non-urgent when the patient has not been referred by another health provider, the diagnostic code at the time of admission is considered non-urgent, diagnostic tests are not needed at the time of evaluation in the emergency department, or the newborn has been recently discharged from hospital. Others have defined non-urgent presenting problems as those in which delays in care would not increase the risk of experiencing an adverse event, and inappropriate reasons for emergency department use as any visits, whether with referral from a health provider or with self-referral, for conditions that could have been managed at a different level of care on account of their severity or the resources required for their management.7
Some of the factors that contribute to the inappropriate use and overcrowding of emergency departments are anxiety in the family, lack of trust in the paediatrician (many families had not yet had their first appointment), parents not having received or understood health education, the incompatibility of parental working schedules with the opening hours of primary care centres or barriers to accessing primary care services, accessibility or physical proximity of the hospital, and easier access to testing in hospitals.8
Some authors have reported that early discharge from the maternity ward is associated with visits to the emergency department related to questions and concerns about basic newborn care, which traditionally were addressed during the hospital stay.
At the same time, we must also consider that visits to emergency departments or any other hospital setting exposes newborns, who are highly vulnerable, to infection, a source of concern for paediatricians, as this interferes with adequate assessment.
Since there is no current consensus on what constitutes a non-urgent presenting problem, in this study we established a new definition of emergency department use appropriateness in the newborn population based on the studies we have previously mentioned.
The aim of this study was to assess the appropriateness of emergency department use in the newborns that attended the Hospital Marina Salud de Denia (HMSD) (Alicante, Spain) during 2014.
MATERIALS AND METHODS
We conducted a cross-sectional study that assessed the appropriateness of emergency department use by the newborns that attended it.
The study setting was the Hospital de Denia, a regional hospital belonging to the AB group of the Department of Health of the Government of Valencia, which has 266 beds and serves the population of Marina Alta in the Autonomous Community of Valencia (Spain). It operates in the framework of the private-public partnership model (“Modelo Alzira”). However, given its resources and the specialty services it offers, the IAMETRICS benchmarking system of IASIST classifies it as a tertiary care hospital. Since December 14, 2009, it has been accredited by AENOR as meeting the UNE-EN-ISO 9001:2008 quality management systems requirements, and its health care records have been integrated in the public health Cerner Millennium database.® The emergency department of the Hospital de Denia has a dedicated paediatrics waiting room, two paediatrics offices and one paediatric resuscitation bay. Paediatric patients are initially managed by emergency medicine physicians, and an on-call paediatrician is physically present at the site to provide consultation 24 hours a day.
Our analysis of the appropriateness of emergency department use included data for the period ranging between January 1 and December 31, 2014. We included newborns aged less than 28 days that attended the emergency room of the HMSD.
Our analysis did not require a sample size calculation, as we included all newborns that attended the emergency department during the period under study.
Data collection
Before starting the study, we requested authorisation from the Research Committee of the Department of Health of Denia by filing the applicable form (“Solicitud de autorización de proyectos de investigación por la Comisión de Investigación del Departamento de Salud de Denia”) and we signed the corresponding researcher’s agreement form (“Compromiso del Investigador”) vowing to conduct and supervise the study in adherence with the protocol authorised by the Research Committee of the Department of Health of Denia and current law on biomedical research and the protection of personal data. Having done so, we collected the data from the emergency department database and by reviewing the public health system electronic health records (Cerner Millenium®) of every newborn that attended the department in 2014.
Establishment of criteria to define appropriateness of emergency department use
Based on the studies cited in the introduction, we defined inappropriate use of the emergency department as visits that did not fulfil any of the following severity criteria (Table 1). We considered visits that fulfilled at least 1 of the criteria as appropriate.
| Table 1. Severity criteria |
|---|
| I. Referral criterion: newborn referred from Primary Care or another health care provider |
| II. Hospital admission criterion: newborn admitted to hospital on discharge from emergency department |
| III. Manchester Triage System (MTS) criterion: newborn classified as level ≤ 3 |
| IV. Need for diagnostic testing criterion: newborn requiring performance of one or more diagnostic tests |

Since the HMSD does not use a modified Manchester triage system for the paediatric population, we found that triage nurses assigned most newborns a level of urgency that was higher than corresponded to their presenting problem on account of their age.
Since one of the severity criteria was an MTS level ≤ 3 with the assumption that levels 1 and 2 corresponded to appropriate use of the emergency department, we attempted to discern which visits by level 3 newborns were actually appropriate. To do so, we applied the other appropriateness criteria to them: referral, hospital admission and need for diagnostic tests, which allowed us to detect a number of newborns who, while classified as level 3, had not made appropriate use of the emergency department.
We analysed the data in collaboration with the Department of Preventive Medicine and Public Health of the HMSD, receiving guidance from its head. We performed all the analysis with the statistical software packages Epidat® 3.1 and Intercooled Stata® 9.1 for Windows®.
We have described qualitative variables as absolute and relative frequencies, and quantitative data as mean and standard deviation or median and interquartile range when the variable distribution was not normal (p-value of less than 0.05 in kurtosis and skewness test). For graphical representation, we created bar and pie charts for qualitative variables and histograms for quantitative variables.
RESULTS
General analysis of the data collected from health records
During the period under study, the emergency department of the HMSD received a total of 8893 paediatric visits of children aged 0 to 15 years, of which a total of 1382 (15.54%) corresponded to infants aged 0 to 12 months, including 228 aged 0 to 30 days that amounted to 16.49% of patients aged less than 12 months and 2.56% of the total paediatric patients. Of the group of patients aged less than 1 month, a total of 167 were newborns (12.08% of infants aged less than 1 month).
The distribution of newborns that visited the emergency department by days of age was not normal (test for skewness and kurtosis, P < .0001).
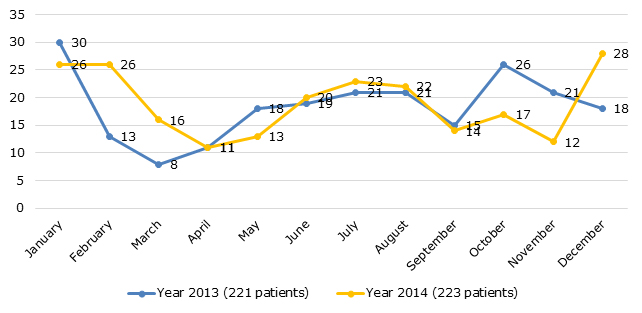
The distribution of visits by season was 17.96% in spring, with 20% of patients admitted to hospital; 28.74% in summer, with 12.50% admitted; 19.76% in autumn, with 21.20% admitted; and 33.76% in winter, with 33.90% admitted (Figure 1).
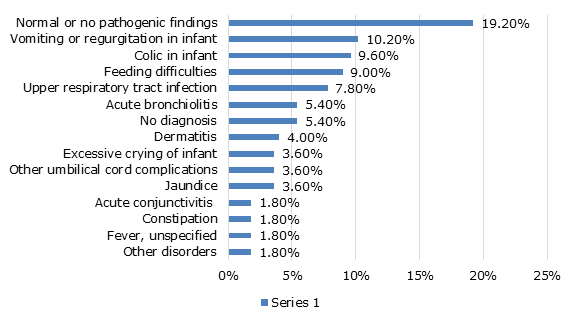
When it came to the discharge diagnoses, which were coded according to the ICD 9, the most frequent were: normal/no pathological findings in 19.20%, vomiting or regurgitation of the newborn in 10.20%, colic in 9.60%, feeding problems in 9% and upper respiratory tract infection in 7.8%, while no ICD diagnostic code was recorded in 5.4% (Figure 2).
Analysis of appropriateness based on the established severity criteria
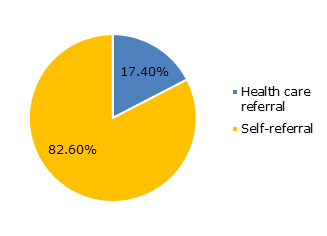
Criterion I (referral): 17.36% (n = 29) visited the emergency department after being referred by another facility or specialist, and 82.64% of newborns (n = 138) visited the department on the initiative of their parents (Figure 3).
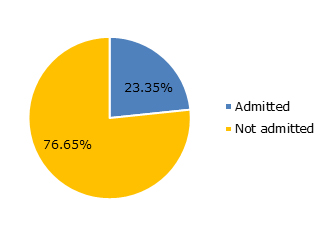
Criterion II (hospital admission): 23.4% (n = 39) of the newborns managed in the emergency department required hospital admission, while 76.65% (n = 128) were discharged home after evaluation in the emergency department (Figure 4).
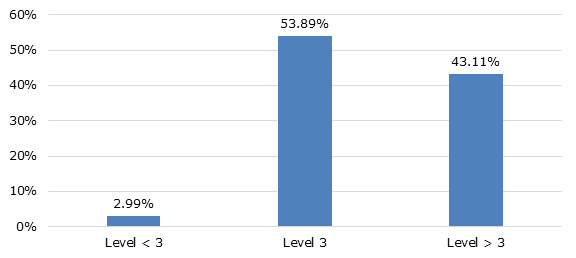
Criterion III (classification based on the Manchester Triage System [MTS]): we found that 3% (n = 5) of newborns were classified as level less than 3 (1-2), 53.9% (n = 90) as level 3, and 43.1% (n = 72) as level greater than 3 (4-5) (Figure 5).
The results of the statistical analysis performed to exclude newborns who were assigned to level 3 solely on the basis of age are the following: of the newborns classified as level 3 based on the MTS, 28.9% (26 newborns) required hospital admission, 14.4% (n = 13) had been referred by PC, another health facility or another health specialist, and 85.6% were self-referred by parents (77 newborns).
Of the newborns classified as level 3 according to the MTS, 96.67% did not require diagnostic tests, and we found that none of the patients who were not referred by health services or admitted after evaluation in the emergency department required diagnostic tests.
Therefore, 33.5% (n = 56) of the newborns met at least one of the 3 severity criteria: admission to hospital, referral from other health services or level ≤ 3 in the MTS. Those that met more than 1 criterion were counted as a single unit in the analysis.
Overall, 36.66% (n = 33) of the 90 newborns classified as level 3 had been referred to the emergency department or required hospital admission after evaluation in the emergency department.
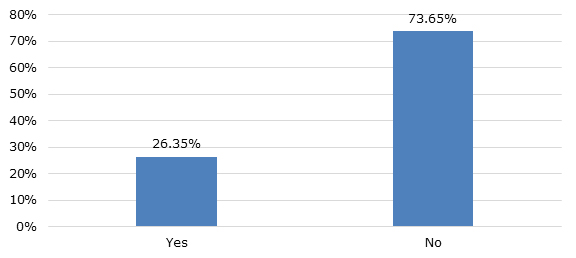
Criterion IV (diagnostic tests): 73.65% (n = 123) of the newborns did not require any diagnostic tests, while 26.35% (n = 44) did (Figure 6).
Of the 44 newborns who required diagnostic tests, 11.36% (n = 5) had not met any of the previous criteria (referred by health provider, admitted to hospital or MTS classification ≤ 3), and we added them to the 33.5% of newborns (n = 56) that had met them.
In total, to the 56 newborns that made appropriate use of emergency services based on the established criteria (admission/referral/critically ill), we added another 5 newborns that, having met none of these criteria, did require diagnostic tests.
Thus, of the 167 newborns included in the analysis, 36.5% (n = 61) were classified as having made appropriate use of emergency services, while 63.50% (n = 106) were classified as having made inappropriate use of them (Figure 7).
When it came to age, we did not find statistically significant differences in the proportion of appropriate use by groups of age at 15-day intervals (χ2, P = .713). Sixty-five percent of newborns that attended the emergency department in the first 14 days of life made inappropriate use of the services, as did 65% of newborns who attended the department in the second fortnight of life.
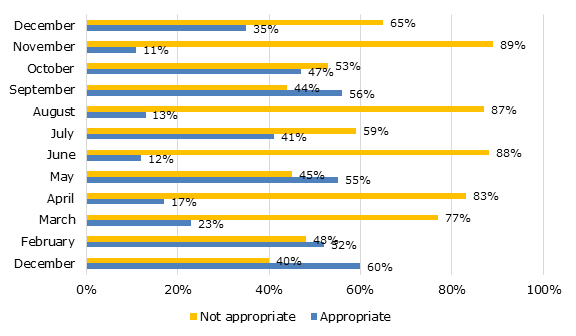
We found statistically significant differences in the proportion of appropriate use based on the month of the year (Fisher’s exact test, P = .024) (Figure 8).
DISCUSSION AND CONCLUSIONS
The increase in the number of visits to emergency departments has continued to grow in recent years1,2 despite the improvements made in health services at the PC level, with an excessive demand of hospital services in the newborn population. There is wide variability in the reasons newborns seek emergency care, which continue to be the subject of study for researchers who focus on this particular issue.6,9
In the emergency department of the HMSD, which received a total of 8893 paediatric emergency visits by children aged up to 14 years in 2014, newborns constitute a relatively small proportion of paediatric users (2.56%). However, this age group has a series of particular characteristics that differentiate it from the rest of paediatric patients and related to the considerable anxiety elicited in the family by the appearance of any symptoms.
Many of the works published to date3,9,10 conclude neonatal visits to emergency departments are usually for non-urgent illnesses and could have been avoided if carers had basic knowledge of newborn care/management.
When we analysed the discharge diagnoses documented in the health records, we found that the most frequent diagnosis, in nearly 20% of cases, was normal health, that is, the absence of disease. Other frequent diagnoses were vomiting or regurgitation in the infant, colic or feeding difficulties. Thus, most of the clinical diagnoses at discharge could be considered an unremarkable problem in newborns within the bounds of basic newborn care. This was consistent with the data reported by most studies on infant use of emergency services, which suggested a new line of research to investigate the potential association and agreement between the presenting problem and the discharge diagnosis.
In our study, a high percentage (82.64%) of the newborns that attended the emergency department did so on the initiative of their parents as opposed to being referred by a PC centre or another health provider, and only a small percentage of them, as low as 19.56%, required admission to hospital. We also found that the majority of newborns who were self-referred by parents were discharged home after evaluation in the emergency department, suggesting that the presenting problem could have been managed in other care settings.
In agreement with our study, several others9 have concluded that newborns referred by other health providers require admission more frequently than newborns that seek emergency care on the initiative of their parents. However, some authors11 have not found evidence of this association, which may have been due to gaps on specific knowledge in neonatology in some paediatricians or other clinicians serving this population at the PC level, who therefore refer newborns to the emergency department for reasons that do not require hospital-level care.
In contrast with some authors9 that report no difference in the frequency of neonatal emergency department use during the summer months, our study found a higher percentage of visits during this season (87.97%), which may be due to the fact that the HMSD is located in an area that is a holiday destination. However, only 12.50% of the newborns that attended during these months required hospital admission. This increased use in the summer months may stem from the need to address common problems that develop in newborns in the first days of life when the family does not have access to their own paediatrician or a familiar PC centre.
Since there is no consensus on what constitutes appropriate use of emergency department services, in this study we developed a definition based on several criteria, such as the need for hospital admission, the source of referral for the newborn, the level of severity based on the Manchester Triage System and the need for diagnostic testing.
Based on the criteria established to define appropriateness of emergency department use, we found that of all the newborns who attended the department, only 36.5% (n = 61) made appropriate use of it, while 63.5% (n = 116), that is, more than half that visited the emergency department, made inappropriate use of it, while the most frequent discharge diagnosis was that of healthy newborn or newborn without abnormal findings.
Our study corroborates that emergency departments are frequently used for conditions that are considered non-urgent and for questions or concerns regarding newborn care, which would be more appropriately managed at the PC level without having to visit the emergency department. We believe that management of these problems at the appropriate level would prevent delays in care in emergency departments, where newborns are considered an at-risk population, so that the saved time could be devoted to urgent cases.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
HMSD: Hospital Marina Salud de Denia • ICD: international classification of diseases • MTS: Manchester triage system • PC: primary care • WHO: World Health Organization.
REFERENCES
- Millar K, Gloor J, Wellington N, Joubert G. Early neonatal presentations to the pediatric emergency department. Pediatr Emerg Care. 2000;16:145-50.
- Pérez Sánchez A, Begara de la Fuente M, Núñez Fuster J, Navarro González J. Consultas reiterativas en la urgencia hospitalaria pediátrica. An Esp Pediat. 1996:44:321-5.
- Ruiz L, Ruggeri N. Urgencias de recién nacidos en hospital pediátrico. X Reunión Anual de la Sociedad Española de Urgencias de Pediatría (IV). An Pediatr (Barc). 2006;65:278-300.
- Chimeti Camacho P, Iglesias Fernández C, Marsinyach Ros I, Crespo Medina M, Mínguez Navarro C, Marañón Pardillo R. Uso del servicio de urgencias por los menores de un mes de vida. X Reunión Anual de la Sociedad Española de Urgencias de Pediatría (IV). An Pediatr (Barc). 2006;65:278-300.
- Lapeña López de Armentia S, Reguero Celada S, García Rabanal M, Gutiérrez Fernández M, Abdallah I, González Aparicio H. Estudio epidemiológico de las urgencias pediátricas en un hospital general. Factores implicados en una demanda inadecuada. An Esp Pediatr. 1996;44:121-5.
- Kennedy TJT, Purcell LK, LeBlanc JC, Jangaard KA. Emergency Department use by infants less than 14 days of age. Pediatr Emer Care. 2004;20:437-42.
- Flanagan CF, Stewart M. Factors associated with early neonatal attendance to a paediatric emergency department. Arch Dis Child. 2014;99:239-43.
- Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Deciding to visit the Emergency Department for nonurgent conditions: a systematic review of the literature. Am J Manag Care. 2013;19:47-59.
- Sharma V, Simon S, Bakewell J, Ellerbeck E, Fox M, Wallace D. Factors influencing infant visits to Emergency Departments. Pediatrics. 2000;106:1031-9.
- Pérez Solís D, Pardo de la Vega R, Fernández González N, Ibáñez Fernández A, Prieto Espuñes S, Fanjul Fernández JL. Atención a neonatos en una unidad de urgencias pediátricas. An Pediatr (Barc). 2003;59:54-8.
- Fernández Ruiz C, Trenchs Sainz de la Maza V, Curcoy Barcenilla AI, Lasuen del Olmo N, Luaces Cubells C. Asistencia a neonatos en el servicio de urgencias de un hospital pediátrico terciario. An Pediatr (Barc). 2006;65:123-8.
- Assandri Dávila E, Ferreira García MI, Bello Pedrosa O, de Leonardis Capelo D. Hospitalización neonatal desde el servicio de urgencias en un centro hospitalario de Uruguay. An Pediatr (Barc). 2005;63:413-7.