Vol. 19 - Num. 75
Original Papers
Can intussusception be managed at the outpatient level?
Paula Ortolá Fortesa, Anna Domènech Tàrregaa, Patricia Rodríguez Iglesiasa, Lucía Rodríguez Caraballoa, Cinta Sangüesa Nebotb, Juan José Vila Carbóa
aServicio Cirugía Pediátrica. Hospital Universitario y Politécnico La Fe. Valencia. España.
bServicio de Radiodiagnóstico. Hospital Universitario y Politécnico La Fe. Valencia. España.
Correspondence: P Ortolá. E-mail: paula.ortola.fortes@gmail.com
Reference of this article: Ortolá Fortes P, Domènech Tàrrega A, Rodríguez Iglesias P, Rodríguez Caraballo L, Sangüesa Nebot C, Vila Carbó JJ. Can intussusception be managed at the outpatient level? Rev Pediatr Aten Primaria. 2017;19:231-9.
Published in Internet: 04-07-2017 - Visits: 38523
Abstract
Introduction: intussusception is the most frequent cause of bowel obstruction in children under three years. Usually, after reduction, patients remain admitted for 24-48 hours. Ambulatory management has recently been proposed, based on clinical experience of follow-up of the patient's evolution in the Emergency Department of the hospital during the following 12 hours. Our objective is to evaluate the implementation of this new therapeutic attitude.
Material and methods: retrospective review of all the intussusceptions treated at our center during the last 12 years.
Results: 458 patients were included, 60.3% ot them were male. Mean age was 24.1 months (SD 24.6), with the ileo-colic location being the most frequent (77.7%). 2.4% had secondary causes. A pneumoenema was performed in 370 children, requiring surgery 10.7%. There were 78 relapses in 56 patients (12.2%), 15 of them during admission. The mean time to reintroduce feeding and the mean hospital stay was 28.6 and 64.4 hours respectively, with no significant difference between those who relapsed and those who did not (60.8 vs 69 hours, t = -0.4, p = 0.689).
There was no relationship between a longer clinical evolution and pneumoenema succeed rate (t = 0.478, p = 0.634). Although there were differences in the need for surgical intervention (χ² = 5.604, p = 0.018), there were no complications. Early reintroduction of feeding was not related to any recurrences or differences between groups (30.2% in the relapsed group and 23.1% in the non-recurrent group, p = 0.608).
Conclusions: hospital admission beyond 12 hours does not decrease the rate of complications. Therefore, we consider that outpatient observation for 12 hours after reduction is a safe and economical measure.
Keywords
● Children ● Enema ● Intussusception ● Outpatients ● Recurrence ● UltrasonographyINTRODUCTION
Intussusception is the most frequent cause of bowel obstruction in paediatric patients aged less than 3 years, although it can occur at any age.1-8 It consists of the invagination or entrance of one part of the intestine into a more distal portion of the bowel.4,5,7 Its incidence is approximately 1 to 4 per 1000 children, and it is higher in children aged 3 to 12 months of age (0.6 to 1 per 1000).2,4,5 It is more frequent in males, and the male:female ratio ranges between 1.2:1 and 2.4:1, depending on the published series.2,5
In 60%-90% of cases the aetiology is unknown, 1,2,5,7,8 although infection/inflammation leading to intestinal lymphoid hyperplasia has been suggested as the ‘lead point’ in its pathogenesis.3,5,6,9 Although less frequent (< 10%-12%), certain diseases should be ruled out as a secondary cause on account of their clinical significance: Meckel’s diverticulum, intestinal lymphoma, intestinal duplication cyst, celiac disease, cystic fibrosis or Henoch-Schönlein purpura, among others.3,5,7-14
The site of invagination is ileocolic in most patients, and less frequently ileoileal, colocolic or rectosigmoid (Table 1).2,6
| Table 1. Location and frequency of intussusception in the general population and in the sample under study | ||
|---|---|---|
| Type of intussusception | General population (%) | Study sample (%) |
| Ileocolic | 60-90 | 77.7 |
| Ileoileal | 5-10 | 10.5 |
| Colocolic | < 5 | < 1 |
| Rectosigmoid | < 1 | < 1 |

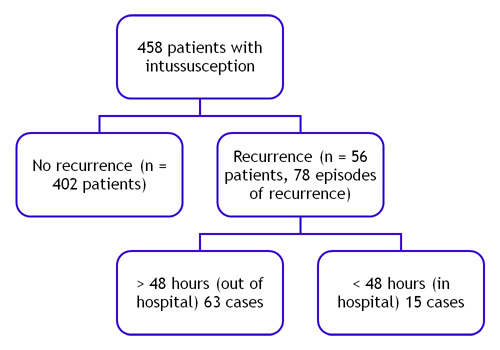
Patients typically present with intermittent abdominal pain, pulling the legs to the chest, followed by a period of lethargy. This may be accompanied by irritability, vomiting, decreased appetite and/or bloody bowel movements (currant jelly stools).2,3,5,10,13 Imaging tests play an important role in its diagnosis, which is primarily based on the clinical manifestations. Ultrasound examination, mainly, and plain chest radiography reveal characteristic findings (target, doughnut or pseudokidney signs) (Figures 1 and 2) that are very useful in the identification of this disease, as well as its localization and evaluation of potential complications.15-20
| Figure 1. Ultrasound images of intussusception: a) transverse view of ileoileal intussusception (doughnut or target sign); b) transverse view of ileocolic intussusception, containing enlarged lymph nodes; c) longitudinal view of ileocolic intussusception (pseudokidney sign) |
|---|
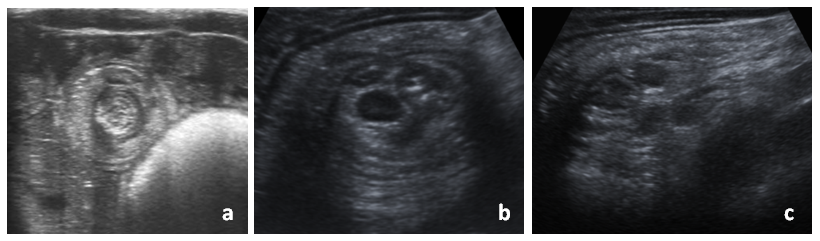 |

| Figure 2. Abdominal X-ray in patients with intussusception: a) silent abdomen; b) absence of air in the right bowel; c) intussusceptum at the level of the hepatic flexure |
|---|
 |

Symptomatic treatment of these patients with administration of analgesia and fluids should not be delayed. In addition, once the diagnosis is confirmed, aetiological treatment should promptly follow in cases that require it. At present, the most frequent method used to reduce uncomplicated ileocolic intussusception is the air enema, consisting of the controlled injection of air through the anus to reduce intussusception, which prevents the use of surgery in many patients. This procedure is guided by imaging and ends when the passage of air past the affected site, usually the ileocecal valve, is visualised.15-19 In the last few years, most facilities have been performing this procedure under sedation, since relaxation of smooth muscle minimizes the duration of the procedure, the pressure required for reduction and the patient’s exposure to radiation.21,22 This technique has a high success rate of 70% to 90% and a rate of associated complications of less than 1%, the most common being bowel perforation. Surgery is indicated in cases that are complicated, have a known cause or in which conservative treatment with air enema has been unsuccessful (usually after three attempts).15-20 The proportion of patients that finally require surgical intervention ranges between approximately 10% and 30%, depending on the reference consulted.15,19 In these patients, the procedure may simply consist in the reduction of intussusception by manual taxis manoeuvres or even require resection due to intestinal tissue damage.
Intussusception may recur in 8% to 15% of cases,1,5,7,10,15,16,18 most frequently within the first 24 to 48 hours, due to the underlying inflammation. Therefore, the current trend in most facilities is to keep patients hospitalised during this period, reintroducing previously established oral nutrition after discharge. However, with the purpose of decreasing the discomfort of patients and their families and of optimising health care resources, an increasing number of specialists and publications suggest that observation in the emergency department following reduction for a period of no more than 12 hours is a safe and cost-effective approach, as it has not been associated with less favourable outcomes in patients that experience recurrence after hospital discharge.1 There are protocols for the early reintroduction of oral feeding (fast-track), which are based on the introduction of feedings 6 to 12 hours following the intervention and that are used in other type of surgical conditions in which the implementation of this measure is advocated and has not been associated with increases in complications or recurrence.23-25
Our goal was to analyse different characteristics of episodes of intussusception, including recurrences, and their outcomes, with the purpose of obtaining reliable data that could be used to update the treatment protocol for this disease.
MATERIALS AND METHODS
We conducted a retrospective study between January 2004 and December 2015 of all cases of intussusception in patients aged less than 15 years managed in our centre (a tertiary care hospital specialised in paediatric patients located in Valencia, Spain).
An ultrasound system (Siemens 2000) with a high-frequency linear transducer (9-4 MHz or 18-6 MHz) was used for radiological diagnosis. In cases of uncomplicated ileocolic intussusception, the Paediatric Radiology department performed an air enema in the presence of staff from the Paediatric Surgery and the Paediatric Anaesthesia departments, using a 24 Ch rectal Foley catheter and filling up the balloon with 20 to 22 cc of air.
We studied patients based on whether they had experienced recurrent episodes or a single episode of intussusception, comparing quantitative variables with categorical ones by means of the Student t test, and different qualitative variables using the χ² test. A 95% confidence interval was calculated for all tests (Excel® 2010, SPSSS® version 20).
RESULTS
A total of 458 patients were evaluated (60.3% male and 39.7% female). The mean age at the first episode was 24.1 months (standard deviation [SD] 24.6, range 0-151.6), with 379 cases (82.8%) documented in children aged less than 3 years. More than half (53.7%) were referred from another medical facility, and the mean time elapsed from the onset of symptoms to assessment in our hospital was 29.7 hours (SD 35.5; range 1-336).
The imaging tests performed at the time of acute presentation were abdominal radiograph in 81.7% of patients and ultrasound examination in 99.6%, with diagnostic findings in 88.7% and 91.3%, respectively. Additionally, an outpatient 99 mTc-pertechnetate scan was requested in 5% of cases with the purpose of ruling out Meckel’s diverticulum, which was found in one.
The ileocolic location was most frequent (356 cases, 77.7%), followed by the ileoileal location (48 cases, 10.5%). There were also cases of colocolic and rectosigmoid intussusception (Table 1).
In all patients, initial management consisted of total oral fasting, fluid therapy and analgesia. In our series, 370 patients (80.8%) were treated with air enema, and the first attempt was successful in 91.1% of them (mean number of attempts 1.2, range: 1-4) (Table 2). The pressures achieved were of 120-140 mmHg in non-sedated patients and 70-80 mmHg in sedated patients, with a sharp drop in pressure at the time that reduction occurred. There were no complications associated with this procedure.
| Table 2. Number of attempted air enemas (until reduction was achieved or surgery indicated) | ||
|---|---|---|
| Number of attempts | Frequency | Percentage (%) |
| 1 | 337 | 91.1 |
| 2 | 13 | 3.5 |
| 3 | 17 | 4.6 |
| 4 | 3 | 0.8 |
| Total | 370 | 100 |

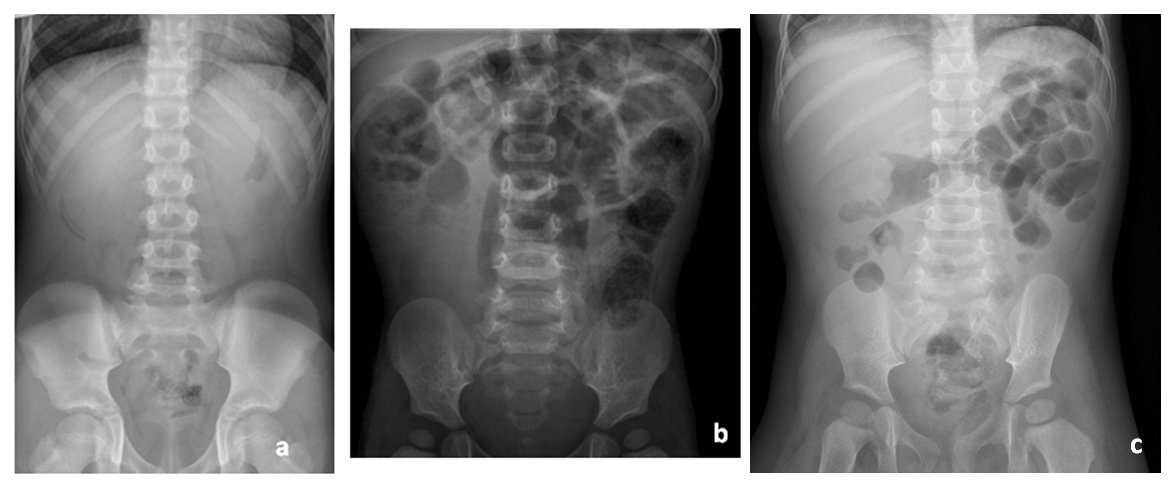
Overall, during the period under study, sedation during air enema was used in 48.2% of patients. However, analysing the documented episodes by year, we found that in the past five years the percentage of air enemas performed under sedation had been increasing, reaching 77.8% by 2010 and 98.3% by 2013 (Figure 3).
| Figure 3. Percentage of air enema procedures performed under sedation. Note the increase in the use of sedation through the years, with practically no use until 2008 and a gradual increase to present, when it is used in every intussusception reduction procedure |
|---|
 |

In cases of ileoileal intussusception, treatment was exclusively medical (symptomatic), with clinical improvement in all.
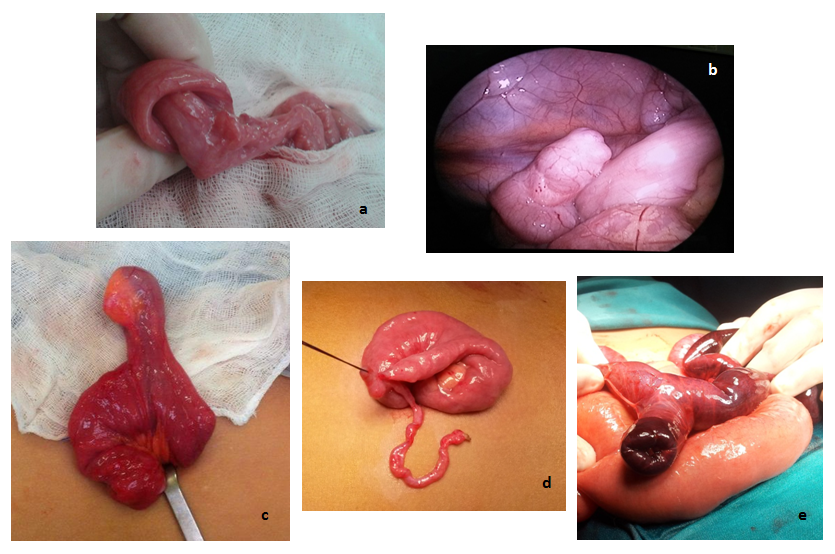
Surgery was performed when reduction could not be accomplished by performance of air enema, or when the patient was clinically unstable or in poor general health. In our series, 49 cases (10.7%) required surgical intervention after the first episode of intussusception. Table 3 summarises the surgical findings. The most frequent diagnoses were: intussusception (of any type), managed by manual reduction by means of taxis manoeuvres; mesenteric lymphadenitis and Meckel’s diverticulum (Figure 4). Intestinal resection was necessary in 11 patients (22.4% of surgeries) due to bowel ischaemia or perforation.
| Table 3. Surgical findings | ||
|---|---|---|
| Surgical findings | Frequency | Percentage (%) |
| Intussusception with no associated findings | 16 | 32.6 |
| Meckel’s diverticulum | 9 | 18.4 |
| Mesenteric lymphadenopathy | 3 | 6.1 |
| Acute appendicitis | 2 | 4.1 |
| Adhesions | 2 | 4.1 |
| Intestinal duplication cyst | 2 | 4.1 |
| Intestinal lymphoma | 1 | 2.0 |
| Intestinal ischaemia or perforation | 11 | 22.5 |
| Normal | 3 | 6.1 |
| Total | 49 | 100 |

| Figure 4. Surgical images: a) intussusception; b) Meckel’s diverticulum, found by laparoscopy; c) Meckel’s diverticulum exposed through an umbilical incision; d) continuation of Meckel’s diverticulum with obliterated vitelline duct; e) Meckel’s diverticulum complicated by intussusception |
|---|
 |

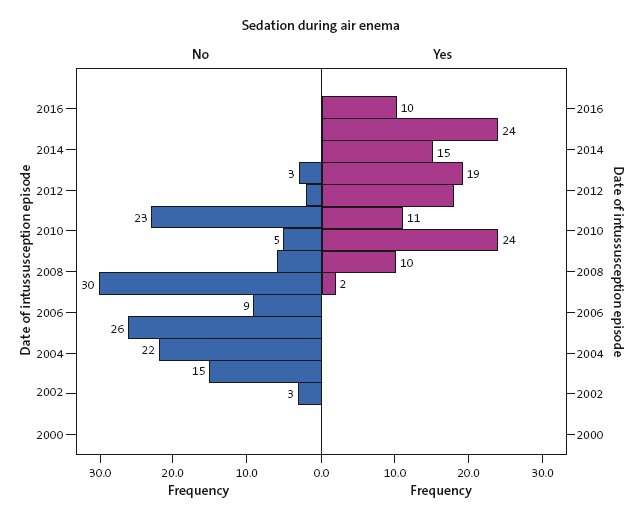
There were records of 78 recurrences in 56 patients (12.2% of cases, range 1-4), with a mean time elapsed from the first episode of 173.4 days (SD 284.7, range 0-1292). Fifteen such cases (19.2%) occurred in hospital, 11 patients had a single recurrence, and 2 patients had two recurrences (Figure 5). Air enema was the initial treatment used in 90% of first recurrences and 81.8% of second recurrences. There were no complications from this intervention and no patients died.
The mean time elapsed to reintroduction of oral feeding after resolution of disease was 28.6 hours (SD 31.3, range 4-144). In the group of patients that did not experience recurrences, early or fast-track reintroduction (within less than 6 hours) was practiced in 30.2% of cases, while in the group that experienced at least one recurrence, it was practised in 23.1% of cases, and did not lead to complications in any of the patients. The statistical analysis did not find significant differences between the two groups (P = .608).
The mean length of stay was 64.4 hours (SD 90.2, range 2-1280, median 40 hours): 63.8 hours in the no-recurrence group (SD 93.26, median 40) and 69 hours in the recurrence group (SD 64.46, median 45); the difference was not statistically significant (t = -0.4; P = .689). This prolonged stay in patients without recurrence, which was at the same time very similar to the stay of patients in the recurrence group, was essentially due to the isolated case of a patient that did not have a recurrence. This patient stayed in our hospital for 1280 hours due to septic shock and underwent manual reduction of an ileoileal intussusception in the context of paralytic ileus requiring surgery. Excluding this case, the mean length of stay would have been 61.8 hours overall, and 60.8 hours in the subset of patients that did not experience recurrences (t = -0.820; P = .454).
DISCUSSION
The sample of patients obtained in our study had a mean age and sex distribution that was consistent with the existing medical literature (with a majority of patients being male and aged less than 3 years). This was also the case when it came to the site of intussusception, which was most frequently ileocolic, and to the percentage of patients in which a cause for intussusception was identified (2.4%).
Ultrasonography was also the method most frequently used in our hospital to diagnose intussusception, although it was often preceded by abdominal radiography, which was performed to assess the bowel gas pattern and rule out perforation. However, the performance of the latter is under debate in our hospital and in the reviewed literature, as many experts claim that it does not provide sufficient information to justify the patient’s exposure to radiation, as it does not usually lead to changes in the approach to management (ultrasonography followed by air enema) and has a low sensitivity.17,20
Based on the existing literature, the conservative management of intussusception with air enema is safe and effective in most cases, with a low incidence of complications.15-20 This is consistent with what we found in our study (91.1% of cases were successfully reduced in the first attempt, with no complications and no deaths).
We ought to highlight that in recent years, and coinciding with an increase in the use of sedation during the procedure, the success rate has increased. This is due to a decreased resistance in the patient on account of muscle relaxation, which results in a shorter duration of the intervention, and the associated decrease in the exposure to radiation.21-22 Furthermore, in our sample, surgical intervention was required in 9% of the patients that were not sedated, a percentage that dropped by half in the subset that did receive sedation (4.5%). This difference, however, was not statistically significant (P = .133). Nevertheless, the proportion of patients that underwent surgery in our series (10.7%) was below or in the lower bound of the interval described in the reviewed sources (10%-30%).15,19
The percentage of recurrences in our sample (12.2%) was within the expected range (8%-15%),1,5,7,10,15,16,18 with a mean 5 to 6 months elapsed from the first episode, as we described above. Of the 78 episodes of recurrence, 15 occurred in hospital (19.2%), one in the first 24 hours and the rest during the second day of hospitalization. Still, there were no differences in patient outcomes (as regards morbidity and mortality) based on whether the recurrence occurred after discharge or during the hospital stay. Therefore, only this 19.2% could have been diagnosed with a hospital admission lasting 48 hours, an approach that was not associated with differences in morbidity or mortality.
As we already noted, the mean time elapsed to reintroduction of oral feeding after reduction and/or the resolution of symptoms (in cases not treated with air enema) was 28.6 hours. We found no relevant or statistically significant differences when we compared the groups of patients with and without recurrences. Therefore, based on our experience, the implementation of this approach seems safe and would contribute to the earlier discharge of these patients.
The mean length of stay was 61.8 hours (60.8 hours in the no-recurrence group and 69 in the recurrence group). This difference between groups was also not statistically significant (t = -0.4; P = .689).
The analysis of the data revealed that an increase in the time elapsed between onset and arrival to hospital was not associated with a decrease in the success rate nor an increase in the number of air enema attempts required to achieve reduction of intussusception (t = 0.478; P = .634), but it did evince—with statistically significant results—an association with increased need of surgical treatment (χ² = 5,604; P = .018). This could be explained by a poorer clinical state or instability of patients on arrival to our hospital. Similarly, we observed that early reintroduction of oral nutrition (fast-track) was not associated with an increased number of recurrent episodes in our sample (χ² = 0.031; P = .608), as the test results were not statistically significant.
As for the limitations of our study, it had a retrospective design that made it susceptible to biases. We are aware of the limitation inherent in the missing data of episodes with onset at home that resolved spontaneously or were treated in other facilities, as opposed to being referred to our hospital. Furthermore, during the period under study, there were changes in the interventions used to treat intussusception (air enema with or without sedation), while radiologists and surgeons in our hospital gained experience in the management of this disease. The development of laparoscopic techniques that allow a surgical examination of the abdominal cavity in case of diagnostic uncertainty, and with a lower associated morbidity than open surgery, has also made the management of intussusception easier. On the other hand, the absence of complications makes us question whether the sample was not large enough to detect them.
While the obtained data support the proposed management of these patients based on observation without hospital admission (which is also facilitated by early or fast-track reintroduction of oral feeding), an appropriate selection of cases is important, as this approach should be used in stable patients, without complications, and without suspicion of an aetiological cause requiring surgical intervention. Furthermore, patients that live far from the health care facility or with socioeconomic difficulties are also not good candidates for this approach. In cases when this approach can be applied, outpatient followup by the primary care provider is of the essence, as is educating the family on the disease and the way to proceed in case of a recurrence.
CONCLUSIONS
The reduction in health care costs and the improvement of patient quality of life are objectives increasingly pursued by different health care facilities and their clinicians. A shorter length of stay, or even a short period of observation in the Emergency Department without hospital admission, could help advance these two objectives.
After conducting this study, and as proposed by a few working groups,1 we consider that the approach to the treatment of intussusception proposed at the beginning of this article is cost-effective and safe. Observation in the Emergency Department for a period of approximately 12 hours after the reduction of intussusception by air enema has not been associated with a greater incidence of complications compared to hospitalization. This has been greatly facilitated by the implementation of protocols such as sedation of the patient during performance of air enema21-22 and the early reintroduction of oral feeding (fast-track).23-25 However, we ought to underscore the importance of selecting patients correctly, providing adequate information and education to families, and close monitoring at the outpatient level by the primary care physician.
Nevertheless, prospective randomised trials are required to provide more reliable evidence on this approach and recommend its widespread practice.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
SD: standard deviation.
REFERENCES
- Beres AL, Baird R, Fung E, Hsieh H, Abou-Khalil M, Ted Gerstle J. Comparative outcome analysis of the management of pediatric intussusception with or without surgical admission. J Pediatr Surg. 2014;49:750-2.
- Bines J, Ivanoff B. Acute intussusception in infants and children: incidence, clinical presentation and management: a global perspective. Vaccines and biologicals. Document WHO/V&B/02.19. Geneva: World Health Organization; 2002.
- Wong CW, Chan IH, Chung PH, Lan LC, Lam WW, Wong KK, et al. Childhood intussusception: 17-year experience at a tertiary referral centre in Hong Kong. Hong Kong Med J. 2015;21:518-23.
- Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, Patel MM. Childhood intussusception: a literature review. PLoS One. 2013;8:e68482.
- Huppertz HI, Soriano-Gabarró M, Grimprel E, Franco E, Mezner Z, Desselberger U, et al. Intussusception among young children in Europe. Pediatr Infect Dis J. 2006;25:22-9.
- Mehendale S, Kumar CP, Venkatasubramanian S, Prasanna T. Intussusception in children aged less than five years. Indian J Pediatr. 2016;83:1087-92.
- Esmaeili-Dooki MR, Moslemi L, Hadipoor A, Osia S, Fatemi SA. Pediatric intussusception in Northern Iran: comparison of recurrent with non-recurrent cases. Iran J Pediatr. 2016;26:e3898.
- Trotta F, Da Cas R, Bella A, Santuccio C, Salmaso S. Intussusception hospitalizations incidence in the pediatric population in Italy: a nationwide cross-sectional study. Ital J Pediatr. 2016;42:89.
- Abbas T, AlShahwani N, Jabbour G, Ali M. Retrospective surveillance over 11 years for intussusception in children younger than 14 years in the state of Qatar. Open J Pediatr. 2014;4:1-11.
- Blanch AJ, Perel SB, Acworth JP. Paediatric intussusception: epidemiology and outcome. Emerg Med Australas. 2007;19:45-50.
- Navarro O, Dugougeat F, Kornecki A, Shuckett B, Alton DJ, Daneman A. The impact of imaging in the management of intussusception owing to pathologic lead points in children. A review of 43 cases. Pediatr Radiol. 2000;30:594-603.
- Ludvigsson JF, Nordenskjöld A, Murray JA, Olén O. A large nationwide population-based case-control study of the association between intussusception and later celiac disease. BMC Gastroenterol. 2013;13:89.
- Fallon SC, Lopez ME, Zhang W, Brandt ML, Wesson DE, Lee TC, et al. Risk factors for surgery in pediatric intussusception in the era of pneumatic reduction. J Pediatr Surg. 2013;48:1032-6.
- Singhal BM, Kaval S, Sagar S, Kumar V. Ileoileal intussusception due to Meckel’s diverticulum: An uncommon aetiology. OA Surgery. 2013;1:2.
- Applegate KE. Intussusception in children: diagnostic imaging and treatment. In: Medina LS, Blacmore CC, Applegate KE (Eds). Evidenced-based imaging: improving the quality of imaging in patient care. Atlanta: Springer; 2011. p. 501-14.
- Williams H. Imaging and intussusception. Arch Dis Child Educ Pract Ed. 2008;93:30-6.
- Daneman A, Navarro O. Intussusception Part 1: a review of diagnostic approaches. Pediatr Radiol. 2003;33:79-85.
- Daneman A, Navarro O. Intussusception Part 2: an update on the evolution of management. Pediatr Radiol. 2004;34:97-108.
- Khorana J, Singhavejsakul J, Ukarapol N, Laohapensang M, Wakhanrittee J, Patumanond J. Enema reduction of intussusception: the success rate of hydrostatic and pneumatic reduction. Ther Clin Risk Manag. 2015;11:1837-42.
- Hernandez JA, Swischuk LE, Angel CA. Validity of plain films in intussusceptions. Emerg Radiol. 2004;10:323-6.
- Díaz-Aldagalán González R, Pérez-Martínez A, Pisón-Chacón J, Ayuso-González L, Salcedo-Muñoz B, Goñi-Orayen C. Rescue by pneumoenema under general anaesthesia of apparently non-reducible intestinal intussusceptions. Eur J Pediatr. 2012;171:189-91.
- Ilivitzki A, Shtark LG, Arish K, Engel A. Deep sedation during pneumatic reduction of intussusception. Pediatr Radiol. 2012;42:562-5.
- Adekunle-Ojo AO, Craig AM, Ma L, Caviness AC. Intussusception: postreduction fasting is not necessary to prevent complications and recurrences in the Emergency Department Observation Unit. Pediatr Emerg Care. 2011;27:897-9.
- Sholadoye TT, Suleiman AF, Mshelbwala PM, Ameh EA. Early oral feeding following intestinal anastomoses in children is safe. Afr J Paediatr Surg. 2012;9:113-6.
- Zhuang CL, Ye XZ, Zhang CJ, Dong QT, Chen BC, Yu Z. Early versus traditional postoperative oral feeding in patients undergoing elective colorectal surgery: a meta-analysis of randomized clinical trials. Dig Surg. 2013;30:225-32.