Vol. 18 - Num. 70
Original Papers
Corrective effectiveness of Otostick® silicone prosthesis on prominent ears and its comparison with other existing methods
Reference of this article: Gómez Málaga CM. Corrective effectiveness of Otostick® silicone prosthesis on prominent ears and its comparison with other existing methods. Rev Pediatr Aten Primaria. 2016;70:119-25.
Published in Internet: 22-06-2016 - Visits: 175498
Abstract
Introduction and objective: prominent ears have an estimated incidence of 5%. According to the “Spanish Society of Plastic, Reconstructive and Cosmetic Surgery” almost half of the interventions of patients under 18 years are ears surgery and mostly due to psychological reasons. The objective of this study is to demonstrate the efficacy of early and conservative correction of prominent pinnae by silicone prosthesis Otostick® Bebé, to avoid psychological problems and surgery later.
Material and methods: children between 3 to 72 months, patients of pediatric primary care centers, with cephaloauricular distance greater than 15 mm, were selected. They were evaluated for 12 months, first weekly, then monthly and finally bimonthly.
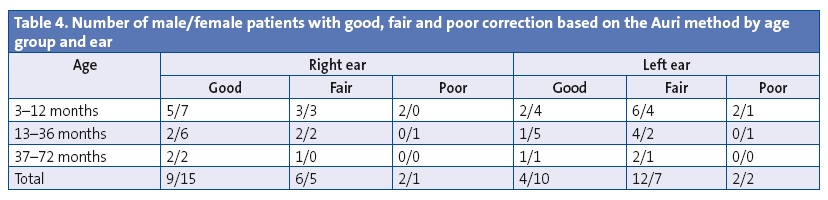
Results: 38 patients and 75 pinnae were finally evaluated from the initial 60 patients. Like Auri method, were considered good, fair and poor correction 6-10 mm, 3-5 mm and 1-2 mm respectively. We have obtained a 90.7% (68 pinnae) with good or fair correction.
Conclusions: the use of Otostick® Bebé baby for 12 months is considered an effective method for correcting prominent ears and can be an alternative to surgery, before psychological problems may arise. Further long-term studies are recommended.
Keywords
● Otoplasty ● Prominent ear ● Prominent earINTRODUCTION
Prominent ears are the most frequent congenital deformity of the head and neck, with an estimated incidence of 5%.1,2 Prominent ears are also known as bat ears or protruding ears. There are other congenital ear deformities, such as cup ears, cryptotia, microtia, lop ears or shell ears, that are treated with different approaches and will not be analysed in this study.
Along with preauricular skin tags, prominent ears are the ear deformity most frequently corrected with surgery in Spanish hospitals.1 According to data from the Spanish Society of Plastic, Repair and Cosmetic Surgery (Sociedad Española de Cirugía Plástica, Reparadora y Estética [SECPRE]) presented in the report La realidad de la cirugía estética en España 2014 (The reality of plastic surgery in Spain 2014), approximately 65 000 plastic surgeries were performed in 2013. Those performed on patients less than 18 years of age accounted for 1.3% of the total, and nearly half of these (46.5%) were otoplasties.3 Otoplasties were performed for psychological reasons and after being requested by the patient and his or her parents.
The aim of our study was to demonstrate the corrective effect of the Otostick® Baby silicon prostheses in children younger than 6 years that do not undergo surgery.
MATERIALS AND METHODS
This study corresponds to the third phase of the R&D&I project named “Prototype for a corrector of prominent ears”, which was approved by and conducted with the participation of the Centro para el Desarrollo Tecnológico Industrial (Center for Industrial Technological Development [CDTi]).
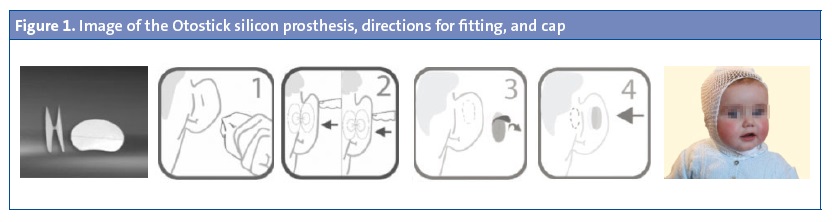
The Otostick® silicon prostheses has been developed by Innovaciones DisRas® and their use has been approved for cosmetic purposes. It consists of two very thin ovals that measure 18 × 15 mm connected by a central isthmus that measures 1 mm; their outer surfaces are coated with a hypoallergenic biological glue developed by researchers of the University of Alicante in collaboration with DisRas, 4 and are attached to the back of the ear and the skin of the temporal region. To facilitate the use of the Otostick® Baby model, especially in infants aged less than 12 months, it is recommended that the prostheses be used along with an elastic cotton mesh cap (Figure 1).
After reviewing the literature on the conservative approaches used in the past, the reference we chose for comparison was the Auri method, developed by Sorribes in Denmark and published in 2002, which employs a custom-made clip that is used at night in a single ear, and which has been shown to achieve adequate correction of prominent ears.5
The patients selected for the study, following the criteria of the Auri method, had prominent pinnae with flat anthelix and an abnormally long cephaloauricular distance, with a separation of at least 1.5 cm at the upper half of the helix. We included children aged 3 to 72 months that received care in primary care (PC) paediatric clinics between June 1 and October 31, 2013.
Of the 72 possible candidates, 65 met the inclusion criteria, and 60 finally participated in the study, grouped by age into: group 1, 3 to 12 months (mean, 7 months); group 2, 13 to 36 months (mean, 17 months); and group 3, 37 to 72 months (mean, 56 months). We explained the protocol of the study in an informed consent document, which was signed by the legal guardians of participants, and in a communication submitted to the Ethics Board of Extremadura.
During the first appointment (November and December 2013), measurements and front and side photographs of the patients were taken, and parents were taught how to attach the prostheses. Follow-up visits were scheduled weekly during the first month and monthly between the second and sixth months. Since the initial objectives had not been met at six months, the study was prolonged, setting up follow-up appointments every two months from the sixth to the twelfth month. We stopped collecting data in December 2014, and completed the study by making a survey of parents and legal guardians that included subjective questions rated on a scale from 1 to 10 (fit of the prostheses, ease of use, correction of problem) as well as objective questions (such as prosthesis duration), sent out in the first trimester of 2015.
RESULTS
We analysed data at six months and twelve months of the study.
Of the 60 participants at the beginning of the treatment, 28 were male (14 aged 3–12 months, 9 aged 13–36 months and 5 aged 37–72 months) and 32 female (17, 10 and 5 in the respective age groups) (Table 1). Of the 60 participants, 22 (36.7%) dropped out of the study, eleven from group 1 (six before and five after six months had elapsed) and five from group 3 (three before and two after six months had elapsed). Attrition in the first six months (14 participants [23.3%]) in groups 2 and 3 resulted from missing the follow-up visits, and in group 1 from the development of erythema and skin redness. Attrition in the last six months (8 participants [13.3%]) was due to a lack of additional improvement after what parents considered to be an “adequate” initial correction.
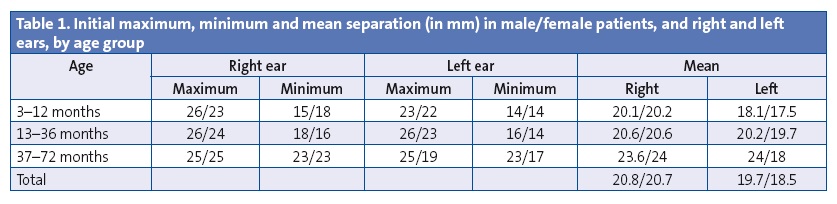
Thirty-eight patients (63.33%) completed the study after 12 months with the parents or guardians filling out the questionnaire, of whom 20 belonged to group 1 (10 boys and 10 girls), 13 to group 2 (8 girls and 5 boys) and five to group 3 (three boys and two girls).
We classified the grade of correction as it was done in the Auri method, with three categories: good correction (6–10 mm); fair correction (3–5 mm) and poor correction (1–2 mm).
At six months of treatment, we had collected data for 46 participants (a total of 90 ears, as only one ear was treated in two patients), and observed that the measurements of correction were lower than those achieved by the Auri method in the same amount of time, so we decided to prolong the study for another six months to complete 12 months of treatment.
The outcomes achieved at six months were good or fair correction in 39 ears (43.3%) and poor correction in 41 years. The mean correction at six months was 2.2 mm, with a maximum of 8 mm and a minimum of 0 mm. The outcomes achieved at 12 months since initiating treatment (38 patients and 75 ears) was good or fair correction in 68 ears (90.7%) and poor correction in 7 ears (9.3%).
The mean grade of correction was higher in females than in males, and was higher in the right ear than in the left in all groups except in males in group 2 (Tables 2, 3 and 4). As for the grade of correction for right and left ears combined, the highest was observed in group 3, but the patients in this group were few and had a high degree of separation at the outset, so the cosmetic effect was smaller.
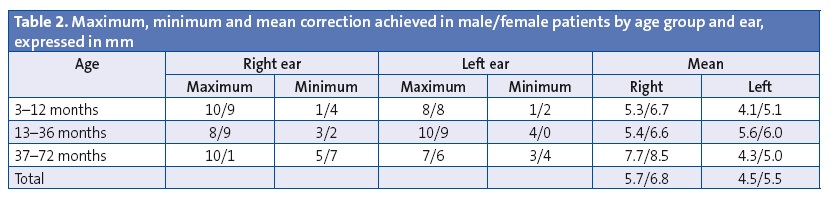
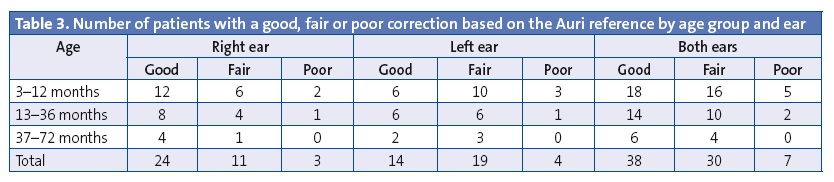
Given that groups 1 and 2 had a comparable number of patients, the grade of correction was higher in group 2, which therefore appears to be the ideal age for the placement of the prostheses. Furthermore, the highest frequency of skin redness and erythema and of attritions due to this reason corresponded to group 1.
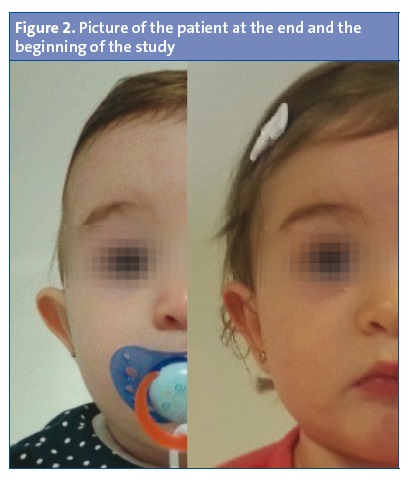
The cosmetic outcome can be seen in Figure 2, which shows one of the participants and the beginning and the end of the study.
The only side effect that we observed was skin irritation or redness, which developed in 23% of the initial participants in the first month of treatment and resolved over time, save in two cases, in which discontinuation of treatment was recommended. This complication also led other patients from group 1 to withdraw from the study. We did not observe any severe complications during the study. When the prostheses peeled off, they did so in one side with the other part remaining attached, which minimised the risk of children swallowing them, as it would be difficult for patients to remove them themselves. The cap was used routinely in 18% of the patients and only during sleep, so it cannot be considered a determinant of the grade of correction.
We estimated that the prostheses can last seven days; 18.4% lasted less than seven days and 81.6% reached optimal durability, with a median duration of 20 days, and durability improving as the study proceeded.
After 12 months, a questionnaire was completed by the parents or guardians of 38 participants. Questions of a subjective nature were answered on a scale from 1 to 10.
- Does the shape, size and material of the prostheses fit adequately? Mean rating, 9.3 (range, 7–10). Highest ratings for group 1 and female patients.
- Duration of prostheses: mean of 23 days in girls and 11 days in boys for the right ear, and 24 days in girls and 12 days in boys for the left ear.
- Is the product easy to use? Mean rating of 8.8 for girls and 9.4 for boys. Total mean of 9.1 (range, 3–10). Fitting the prostheses was easier at older ages and as time passed. At first it was harder to fit on girls, but there was no difference between male and female patients at the end of the study.
- Subjective perception of good correction. Mean rating of 9.1 for girls and 7.5 for boys for the left ear, and 8.7 for girls and 8.7 for boys for the right ear.
DISCUSSION
The reason for treating prominent ears is primarily psychological, rather than cosmetic. A study conducted in North Staffordshire, United Kingdom, reported that the correction of prominent ears in children aged 5 to 16 years achieved not being ridiculed in 100% and increased satisfaction levels in 97%, improved self-esteem in 92%, and led to a more active social life in 79%.6 More recent studies have also demonstrated the positive psychological impact of corrective surgery in patients aged 6 years or more7 and 8 years or more.8
Most surgeons advise parents to observe their children’s behaviour as relates their prominent ears, not pushing surgery unless the patient requests it. According to data gathered by the SECPRE, otoplasty is performed in children aged 4 to 14 years, because the growth of ears is nearly complete by age 4 years, and the sooner the surgery is performed, the less the child is mocked in school.9
Most studies on otoplasty in children report data from interventions in patients aged at least 6 years.2,7,8 More than 200 techniques have been described.10 In young children, the intervention is performed under general anaesthesia, lasts approximately two to three hours, and may lead to complications such as haematoma, infection, necrosis, outer ear canal stenosis, suture extrusion, insufficient correction or overcorrection, keloids and even an unexpected case of neurologic complication.10,11 While the complication rates reported are low, there are few studies on the subject. A review by Limandjaja et al of the medical literature on the complications of otoplasty found that the incidence of early complications ranged between 0% and 8% and the incidence of late complications between 0% and 47%.10
Different conservative, nonsurgical approaches have been described for the treatment of prominent ears, some of which can be applied as early as the neonatal period. These approaches have the advantage that intervention is possible before the child becomes aware of his or her appearance or can be mocked for it.
In this study, we analysed the efficacy of a prosthesis that is easy to fit and was well received by the patients and their families, comparing it to the Auri method. Although some patients dropped out of the study, the total number of ears studied (75) was greater than the number reported in the study that employed the Auri method (56), and all of these ears were studied for a period of 12 months, compared to the mean 5.5 months of the Auri study (with periods of one to ten months). The key features in which the approach differs from the Auri method are its ease of use, as it does not require having two different types of prostheses that are also custom-made, its low cost, the widespread availability of these prostheses, the fact that infants and young children can barely notice their presence, the better outcomes achieved, that it allows treating both ears simultaneously, and that the prostheses can be used without interruption, even during bathing and physical activity.
CONCLUSIONS
The provider that is best-suited to detect cases that could be managed conservatively in the early years of life and always when requested by parents or legal guardians is the primary care paediatrician. It is important that providers be aware of all treatment options in order to provide counselling at the outset. We believe that the Otostick® Baby silicon prostheses can effectively correct a high percentage of prominent ears in very young patients, preferably before age 3 years. Furthermore:
- Compared to the Auri method, the Otostick®Baby silicon prostheses are easier to use, can be used bilaterally and continuously, and are easy to obtain.
- The grade of correction achieved by Otostick®Baby after 12 months of use is good both based on the parameters applied in the Auri method and on the subjective perception of the parents or legal guardians of the patients (Figure 2).
- We observed a greater grade of correction in right ears, both in male and female patients.
- Correction was most efficacious in the 13-to-36-months age group.
Nevertheless, given the limitations of the study, we need to continue to monitor long-term results and carry out further research.
CONFLICTS OF INTEREST
This study was carried out as a collaborative effort of Innovaciones Disras L.L.C., the Health Care Cluster of Extremadura and the Society of Primary Care Paediatrics of Extremadura (Sociedad de Pediatría de Atención Primaria de Extremadura [SPAPEX]). The SPAPEX received a donation from Disras L.L.C that will be used for the purposes of the Society and conforming to its statutes. None of the researchers or paediatricians that collaborated in the study were personally remunerated for their participation..
ABBREVIATIONS: CDTi: Centro para el Desarrollo Tecnológico Industrial · PC: primary care ·SECPRE: Sociedad Española de Cirugía Plástica, Reparadora y Estética.
ACKNOWLEDGMENTS
We want to thank the PC paediatricians that participated in the recruitment of patients for the study: M. Arce, E. Benito Alonso, M. I. Botana del Arco, J. J. Cuervo Valdés, E. M. García Sabido, R. Gimeno, C. M. Gómez Málaga, R. González Cervera, C. González Galindo, N. González Salguero, J. Jiménez, M. I. Jiménez Álamo, M. P. Leo Canzobre, N. Menéndez, A. Montes Salas, J. J. Morell Bernabé, L. Ortiz, I. Santos Ruiz and C. Sosa.
REFERENCES
- Alonso Peña D, Redondo Pardo UL, Alonso Peña J, Zaragoza Fernández M. Las orejas despegadas en la consulta de Atención Primaria. Rev Pediatr Aten Primaria. 2006;8:671-8.
- García Palacios M, Molina Vázquez ME, Lema Carril A, Somoza Argibay I, Gómez Veiras J. Técnica mínimamente invasiva para la corrección de las orejas procidentes. An Pediatr (Barc). 2008;68:219.
- Presentación del informe “La realidad de la cirugía estética en España 2014”. SECPRE Newsletter, diciembre 2014. In: Sociedad Española de Cirugía Plástica Reparadora y Estética [online] [consulted on 22/06/2016]. Available in http://secpre.org/newsletter/newsletter/newsletter_diciembre.html#informe
- Investigadores de la Universidad de Alicante colabora con la firma extremeña DisRas en el desarrollo de un sistema no quirúrgico para corregir las orejas de soplillo. In: Actualidad Universitaria. Universidad de Alicante [online] [consulted on 22/06/2016]. Available in http://goo.gl/NJvn6i
- Miravet M, Tos M. Nonsurgical treatment of prominet ears with the Auri method. Arch Otolaryngol Head Neck Surg. 2002;128:1369-73.
- Cooper-Hobson G, Jaffe W. The benefits of otoplasty for children: Further evidence to satisfy the modern NHS. J Plast Reconstr Aesthet Surg. 2009;62:190-4.
- Fioramonti P, Serratore F, Tarallo M, Ruggieri M, Ribuffo D. Otoplasty for prominet ears deformity. Eur Rev Med Pharmacol Sci. 2014;18:3156-65.
- Papadopulos NA, Niehaus R, Keller E, Henrich G, Papadopoulos ON, Staudenmaier R, et al. The psychologic and psychosocial impact of otoplasty on children and adults. J Craniofac Surg. 2015;26:2309-14.
- Cirugía de las orejas. In: Sociedad Española de Cirugía Plástica Reparadora y Estética [online] [consulted on 22/06/2016]. Available in http://secpre.org/pacientes/cirugia-estetica/cirug%C3%ADa-facial/cirug%C3%ADa-de-las-orejas
- Limandjaja GC, Breugem CC, Mink van der Molen AB, Kon M. Complications of otoplasty: a literature review. J Plast Reconstr Aesthet Surg. 2009;62:19-27.
- Kayabasoglu G, Nacar A. An unexpected otoplasty complication: temporal nerve paresis. Aesthetic Plast Surg. 2015;39:114-6.





