Social-educative factors associated with low visual acuity in Peru
Mary Marcela Araujo Chumaceroa, FE Solano Zapataa, MA Vilela Estradab, Mario J. Valladares Garridoc, M Chumacero Aguilard, Christian R Mejiae
aEstudiante de Medicina. Universidad Nacional de Piura. Sociedad Científica de Estudiantes de Medicina Universidad Nacional de Piura (SOCIEMUNP). Piura. Perú.
bEstudiante de Medicina. Universidad Privada Antenor Orrego Campus Piura. Sociedad Científica de Estudiantes de Medicina Universidad Privada Antenor Orrego (SOCEM UPAO-PIURA). Piura. Perú.
cUnidad de Investigación en Enfermedades Emergentes y Cambio Climático (Emerge). Universidad Peruana Cayetano Heredia. Lima. Federación Latinoamericana de Sociedades Científicas de Estudiantes de Medicina (FELSOCEM). Unidad de Apoyo a la Docencia e Investigación(UADI). Hospital de la Amistad Perú Corea II-2. Santa Rosa. Piura. Perú.
dMédico en Jefe. CS San José. Piura. Perú.
eEscuela de Medicina Humana. Universidad Continental. Huancayo. Escuela de Postgrado. Universidad Privada Antenor Orrego. Trujillo. Perú.
Correspondence: MM Araujo. E-mail: marymarcela06@gmail.com
Reference of this article: Araujo Chumacero MM, Solano Zapata FE, Vilela Estrada MA, Valladares Garrido MJ, Chumacero Aguilar M, Mejia CR. Social-educative factors associated with low visual acuity in Peru. Rev Pediatr Aten Primaria. 2015;17:e261-e266.
Published in Internet: 23-11-2015 - Visits: 27711
Abstract
Introduction: it is important for students to have a good physical and mental health in order to acquire the knowledge properly. A study was conducted to determine the socio-educational factors associated with low visual acuity in primary schoolchildren from the National College of San Pedro-Piura.
Matherial and methods: using a cross-sectional analytical study involving 655 primary school students. The principal variable was the low visual acuity, considered in those with values greater than 20/25, as assessed with the Snellen chart. p values, prevalence ratios and confidence intervals at 95% were obtained using generalized linear models. Data were analyzed using STATA version 10.0.
Results: a total of 599 students were evaluated, 17% (99) had low visual acuity. Sex was not related to the low visual acuity (p=0.832). While increasing age, it was found that children who were between 8-10 and 11-15 years were 46% (p=0.005) and 68% (p<0.001) less prevalence of having low visual acuity, respectively, compared to the children who were 5-7 years old.
Conclusions: it is concluded that one in six students had a visual disability associated with their age and grade level, this is important as putting on shows that one of six students are visually impaired, which makes them more prone to problems in their grades, which may have implications for the rest of their lives. This should be taken into account by the institutions to monitor the proper education of children.
Keywords
● Emmetropia ● Peru ● Students ● Visual acuityINTRODUCTION
Low visual acuity is an educational problem of worldwide relevance1 that can be avoided with early detection and the active cooperation of parents.2 The Modelo de Atención Integral de Salud (Integral Health Care Model [MAIS]), which is the current health care framework in Peru, provides essential care to meet the health needs of children and adolescents by means of an integral evaluation, which includes visual acuity as an indicator of the eye health status of an individual.1,3
Most studies on the subject are descriptive, such as a study performed in our region that found a prevalence of refractive errors of 46% in a population of schoolchildren in Lima,4 demonstrating that vision problems do not only concern adults and the elderly, but also manifest at early ages. On the other hand, a study conducted in Cuba showed that 70% of paediatric visits to ophthalmology clinics were due to abnormalities in visual acuity.5 Our search did not find many studies that identified factors associated with vision problems, but it did find studies describing specific problems, such as one on retinopathy of prematurity carried out at the Hospital Las Mercedes in Chiclayo (Peru).6
There is a dearth of medical literature on this subject, despite its importance in health prevention and promotion in children and adolescents, as it directly affects their academic performance.7,8 As a result, vision problems are a latent problem in public health, and thus our aim was to determine the socioeducational factors associated with low visual acuity in the elementary education pupils of a public school in the north of Peru.
MATERIALS AND METHODS
We conducted a cross-sectional analytical study in the Colegio Nacional San Pedro school in Piura, Peru. The sample consisted of 655 schoolchildren aged 5 to 15 years, and included all pupils whose parents or guardians consented to the study, excluding those that did not attend on the day of the evaluation and those that were unable to understand and/or strictly follow the directions given. We calculated a minimum sample size of 439 students for an infinite population, assuming a frequency of visual problems of 46%4 and a statistical difference between groups of 10%, for a statistical significance of 95% and a power of 99% (calculations were made with the Epitable® application version 3.1). We surveyed a total of 599 children and adolescents (refusal rate, 8.5%).
The outcome variable was visual acuity. It was measured by the Snellen method, which allows the detection of vision problems with simple means (with an 85% sensitivity and a 96% specificity when E charts are used);9 we used Snellen letter and E optotypes, the latter for evaluation of children that had difficulty recognising the letters or did not know how to read. We defined optimal visual acuity as 20/20 vision, normal acuity as up to 20/25; and low acuity as all values below that.
In the statistical analysis, the outcome variable was having low visual acuity, which was contrasted with sex, age (categorised into 5–7 years, 8–10 years and 11–15 years) and school year (from first to sixth year).
The pre-test data collection was performed over five days and by classroom. The assessment was performed by medicine students (who were first trained by specialists) in the schoolyard. There was adequate natural light, children were placed at a distance of six meters from the Snellen chart, and distractions were avoided. Each eye was evaluated separately while covering the opposite eye with an occluder.10
The data were collected in a data entry form with Microsoft Excel® (version 2010 for Windows®). We analysed the data with the Stata® application, version 11.1. The descriptive analysis summarised qualitative variables as absolute and relative frequency distributions, and quantitative variables as mean and standard deviation (SD) or median and interquartile range, depending on their distribution.
In the analytical study, we used general linear models (using the Poisson family and the log link function) to find p values, prevalence ratios and their respective 95% confidence intervals (CIs). We defined statistical significance as P < .05.
We obtained the written informed consent of the parents or guardians, as well as the consent of each student, before conducting the evaluation. All children whose results in the visual acuity assessment were not normal were referred to an ophthalmology specialist for assessment of its causes and vision correction.
RESULTS
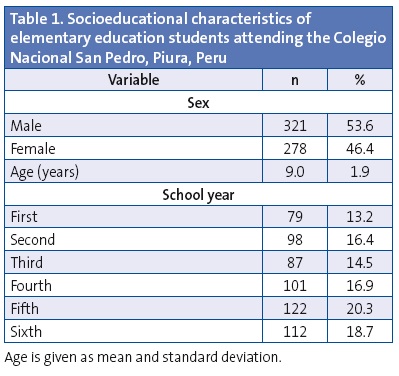
The sample included 599 schoolchildren with a mean age of 8.99 years (SD, 1.86), 53.6% were male. The fifth grade had the largest number of students (20.3%) (Table 1).
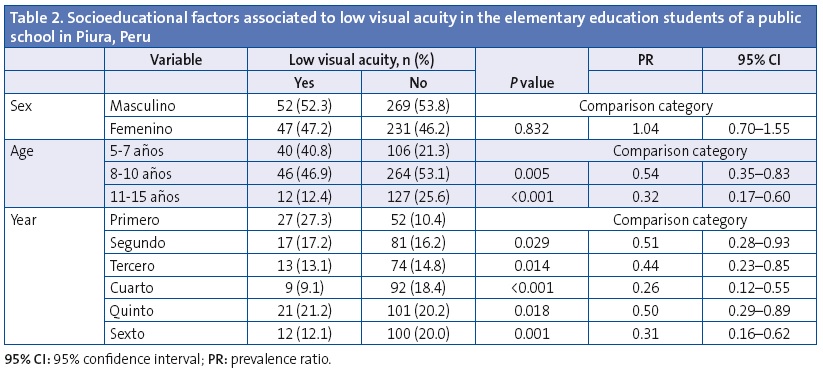
When we analysed the association of low visual acuity with socioeducational characteristics, we found that sex was not correlated to low visual acuity (P = .832). There was a significant correlation with increasing age, with a prevalence of low visual acuity 46% lower (P = .005) and 68% lower (P = .001) in children aged 8–10 and 11–15 years, respectively, compared to children aged 5 to 7 years. Last of all, as children progressed through the school years, the prevalence of low visual acuity decreased, by 49% less in the second year, 56% less in the third year, 74% less in the fourth year, 50% less in the fifth year, and 69% in the sixth year. Table 2 shows the results obtained.
DISCUSSION
According to the results of our study, 16.5% of children had low visual acuity, which stands in contrast with results of similar studies in populations in other countries, such as India (4.3%)11 or Argentina (10.7%).2 The data also diverges from the results of a study carried out in Apurimac, Peru, in which only slightly more than 6% of participants had refractive errors; however, this study was performed on a sample with a narrower age range (3 to 11 years of age).12 Our results were consistent with those of a study conducted in Colombia in children aged 7 to 11 years, which found a prevalence of low visual acuity of 14.2%.13 One more study, which compared two types of charts for the evaluation of visual acuity, also found a similar prevalence (18.1%).14
We found that the age of participants was associated with their visual acuity: the older the age, the lower the prevalence of low visual acuity. This is inconsistent with similar studies performed in Asian populations (China and Saudi Arabia) that observed that low visual acuity increased with the age of the children.15,16 Furthermore, statistical significant differences in the prevalence of low visual acuity between children of different ages were not found in a study of children younger than 15 years in Oceania17 and one other study conducted in Vietnam.18 We did not find studies with populations similar to that in our study to compare our results regarding the association with increasing age, which opens the possibility of conducting further research with broader populations.
The prevalence also varied by age range: in our study, three-fourths of the participants with low visual acuity were children, which revealed a greater degree of visual impairment compared to adolescents. More specifically, we found a prevalence of low visual acuity of 35% at age 6 years, which support the conclusions of previous studies that set age six years as a reference point for the development of vision problems.2,16,19,20 We found a direct correlation between visual acuity problems and school year. This is consistent with the findings of a study conducted in a developing country in Africa, where refractive errors were associated with increasing school year.21
We found no association between low visual acuity and the sex of the child, which was consistent with the results of a similar study in Fiji.17
Our study had the following limitations: we could not measure additional variables or make comparisons with other populations; furthermore, due to the sampling method used, p values and confidence intervals could only be used as references for the strength of association. Nevertheless, our results are relevant, as this is one of the few studies in our region that analysed such associations, and may serve as a foundation for further research.
Based on the analysed data, we conclude that there is a high prevalence of low visual acuity in the population of students attending a public school in the north of Peru, and that this prevalence is associated with the age and school year of the students.
These results will foster further research addressing other aspects related to visual acuity, such as learning and academic achievement. We recommend that the pertinent authorities monitor the ophthalmologic evaluation of school-aged children and adolescents so that vision problems can be detected and treated early with the help of health care professionals, in order to avoid their progression and the problems that derive from poor performance in elementary education.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS: SD: standard deviation; 95% CI: 95% confidence interval; MAIS: Modelo de Atención Integral de Salud (Integral Health Care Model); SIS: Seguro Integral de Salud (Integral Health Insurance).
ACKNOWLEDGMENTS
We want to thank the management of the Colegio Nacional San Pedro school (Piura, Peru) for allowing us to carry out this research. We are also grateful to the San Pedro health care centre (Piura, Peru), which provided us with the tools required for the assessment of visual acuity, trained us in its evaluation, and contributed to data collection.
REFERENCES
- Guía Nacional de Operativización del Modelo de Atención Integral de Salud. In: Ministerio de Salud [online] [consulted on 17/11/2015]. Available in http://goo.gl/gffUXD
- Verrone P, Simi M. Prevalencia de agudeza visual baja y trastornos oftalmológicos en niños de seis años de la ciudad de Santa Fe. Arch Argent Pediatr. 2008;106:328-33.
- 3. Medicus Mundi. MAIS. Un modelo incluyente e integral bajo un concepto de derecho a la salud (2011-2014). In: Salud Integral Incluyente [online] [consulted on 17/11/2015]. Available in http://saludintegralincluyente.com/previos/mais-peru.html
- Carrión C, Gálvez F, Morales J, Guevara V, Jaramillo R, Gazzani M. Ametropía y ambliopía en escolares de 42 escuelas del programa Escuelas Saludables en la DISA II, Lima. Perú, 2007-2008. Acta Med Per. 2009;26:17-21.
- García E, Estrada Y, Aparicio A. Frecuencia de ametropías en niños. Rev Cubana Pediatr. 2010;82:28-37.
- Gutiérrez C, Wekselman EFV, Herrerera PR, Palacios CL. Retinopatía de la prematuridad en el Hospital Regional Docente Las Mercedes. Chiclayo 2007-2009. Rev Cuerpo Méd. HNAAA. 2012;5:30-2.
- Toledo C, Paiva A, Camilo G, Maior M, Leite I, Guerra M. Early detection of visual impairment and its relation with school effectiveness. Rev Assoc Med Bras. 2010;56:415-9.
- Costa Lança C, Serra H, Prista J. Reading performance in children with visual function anomalies. Int J Ophthalmol Clin Res. 2014;1:1-5.
- Méndez M, Delgado J. Oftalmología: exploración del niño estrábico; detección precoz. Detección precoz de los trastornos de refracción y ambliopía. Rev Pediatr Aten Primaria. 2011;13:163-80.
- Manual de Atención Primaria de salud ocular. In: Instituto Nacional de Oftalmología [online] [consulted on 17/11/2015]. Available in www.ino.org.pe/menu/pnlcc/manual_atencion_salud_ocular.pdf
- Ghosh S, U Mukhopadhyay, Maji D, Bhaduri G. Visual impairment in urban school children of low-income families in Kolkata, India. Indian J Public Health. 2012;56:163-7.
- Latorre S, Gil D, Enciso O, Phelan A, Garcia A, Kohler J. Reducing visual deficits caused by refractive errors in school and preschool children: results of a pilot school program in the Andean region of Apurimac, Peru. Glob Health Action. 2014;7:22656.
- López Ceromeca M. Evaluación de la agudeza visual en estudiantes de una institución educativa de la ciudad de Santiago Cali 2011. Rev Medica Fusm. 2013;1:33-8.
- Peña J, Rubiano D, López M. Concordancia entre el test de números de Snellen y el test de números de Lea en niños entre cuatro y siete años. Cien Tecnol Salud Vis Ocul. 2012;10:115-21.
- Wu JF, Bi HS, Wang SM, Hu YY, Wu H, Sun W, et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS ONE. 2013;8:e82763.
- Wadaani FAA, Amin TT, Ali A, Khan AR. Prevalence and pattern of refractive errors among primary school children in Al Hassa, Saudi Arabia. Glob J Health Sci. 2012;5:125-34.
- Cama A, Sikivou B, Keeffe J. Childhood visual impairment in Fiji. Arch Ophthalmol. 2010;128:608-12.
- Paudel P, Ramson P, Naduvilath T, Wilson D, Phuong HT, Ho SM, et al. Prevalence of vision impairment and refractive error in school children in Ba Ria – Vung Tau province, Vietnam. Clin Experiment Ophthalmol. 2014;42:217-26.
- García L, Bernardo J. Prevalencia y caracterización de errores refractivos en niños de 6 a 12 años, que viven en la Delegación Gustavo A. Madero del Distrito Federal. In: Instituto Politécnico Nacional [online] [consulted on 17/11/2015]. Available in http://goo.gl/ZIBRQ0
- Figueroa LF, Molina N, López Y, Bermúdez M. Agudeza visual, error refractivo, curvatura corneal, visión cromática y estereopsis en niños entre tres y siete años en la localidad de Chapinero de la ciudad de Bogotá. Cien Tecnol Salud Vis Ocul. 2013;11:55-65.
- Sewunet SA, Aredo KK, Gedefew M. Uncorrected refractive error and associated factors among primary school children in Debre Markos District, Northwest Ethiopia. BMC Ophthalmol. 2014;14:95.






