Vol. 17 - Num. 65
Original Papers
Importance of pesticides as a risk factor in child health in the practise of Canarian paediatricians
Raúl Cabrera Rodrígueza, M. E Guerra Rodríguezb
aPediatra. Centro de Salud de la Villa de Mazo. La Palma. España.
bFarmacéutica comunitaria. La Palma. España.
Reference of this article: Cabrera Rodríguez R, Guerra Rodríguez ME. Importance of pesticides as a risk factor in child health in the practise of Canarian paediatricians. Rev Pediatr Aten Primaria. 2015;17:39-45.
Published in Internet: 16-03-2015 - Visits: 16934
Abstract
Introduction: pesticides can be a risk factor for health. Pediatricians’ attitudes and knowledge about pesticides are unknown in the Canary Islands.
Objective: to know the perception that Canary Islands’ pediatricians have on the possible health risks for children that pesticides may cause.
Material and methods: design: transversal study. Electronic self-administered survey about professional data, general aspects and academic training about pesticides. Sample: eighty pediatricians.
Results: pediatricians considered pesticides an important factor in paediatric health but referred low frequency of problems due to them. They considered they had insufficient knowledge about biocides and demanded more training.
Keywords
● Environmental health ● PesticidesINTRODUCTION
The Food and Agriculture Organization (FAO) of the United Nations defines a pesticide1 as any substance intended to prevent, destroy, attract, repel or fight any pest, including unwanted plant or animal species, during the production, storage, transport, distribution and processing of foods, agricultural commodities or animal feeds, or which can be administered to animals to fight ectoparasites. The term includes substances used to regulate plant growth, defoliants, desiccants, fruit thinners or sprouting inhibitors, and substances applied to crops before or after harvesting to protect the product from deterioration during storage and transport. The term is usually not applied to fertilisers, plant and animal nutrients, food additives and animal drugs. The term biocide is used interchangeably with pesticide.
In recent years, various international organisations have warned of the risks of pesticide exposure to children’s health.2,3 Yet there has been neither an adequate evaluation of the environmental risks or educational measures regarding pesticides in our region.
OBJECTIVES
- To learn the importance of pesticides as a factor that influences child health in the practise of Canarian paediatricians.
- To evaluate the basic knowledge regarding exposure to biocides of Canarian paediatricians (source of exposure, susceptibility, and related health problems).
- To determine the extent of the education on pesticides of Canarian paediatricians.
MATERIALS AND METHODS
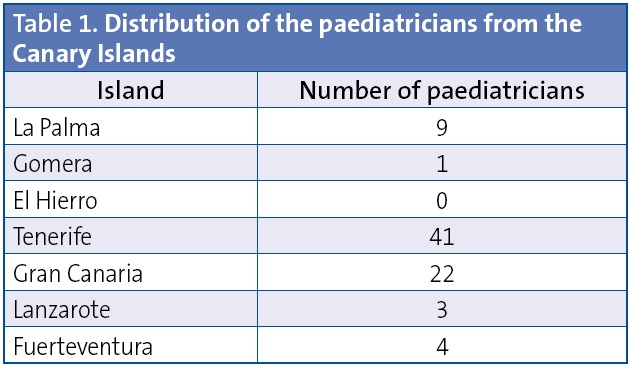
Our sample included 80 paediatricians distributed through six of the seven Canary Islands.
We collected data by means of a digital questionnaire designed for this study using Google Docs®.
The questionnaire consisted of 28 items arranged in six groups: a) professional data (profession, work setting, island and town); b) general aspects regarding pesticides (importance and frequency); c) susceptibility to biocides by age group and sex (children, men, women, pregnant women, elderly); d) sources of exposure (occupational, food, drinking water, pesticides used in the home, exposure of the home, exposure of the workplace, environmental exposure); e) health consequences (malignancies, pregnancy complications, neurodevelopmental abnormalities, endocrine abnormalities, allergies, neurologic and psychological problems, respiratory problems, and autoimmune problems); and f) education on biocides (current level of training, need for additional education). Save for items in the first group, all items were answered on a Likert scale (from 1 to 10).
The questionnaire was distributed by electronic mail from the administrative departments of the four paediatrics associations of the Canary Islands (Sociedad de Pediatría de Canarias, chapters of Tenerife and Las Palmas, Asociación de Pediatría de Atención Primaria de Canarias and Sociedad Canaria de Pediatría Extrahospitalaria). We requested the paediatricians’ collaboration between July and October of 2014. Prior to its administration, we tested the questionnaire on a pilot group of health providers of the island of La Palma to verify that it was well understood.
Statistical analysis. We analysed the data using the IBM SPSS Statistics software version 20 for Windows©.
Results
Sample characteristics: we obtained the collaboration of a total of 80 paediatricians distributed across six of the seven Canary Islands. Table 1 shows their distribution by island. When it came to their work setting, 53 worked in primary care, 17 in inpatient specialised care, two in emergency departments, and 8 in a combination of settings.
The results are expressed as mean and standard deviation for every item in the questionnaire.
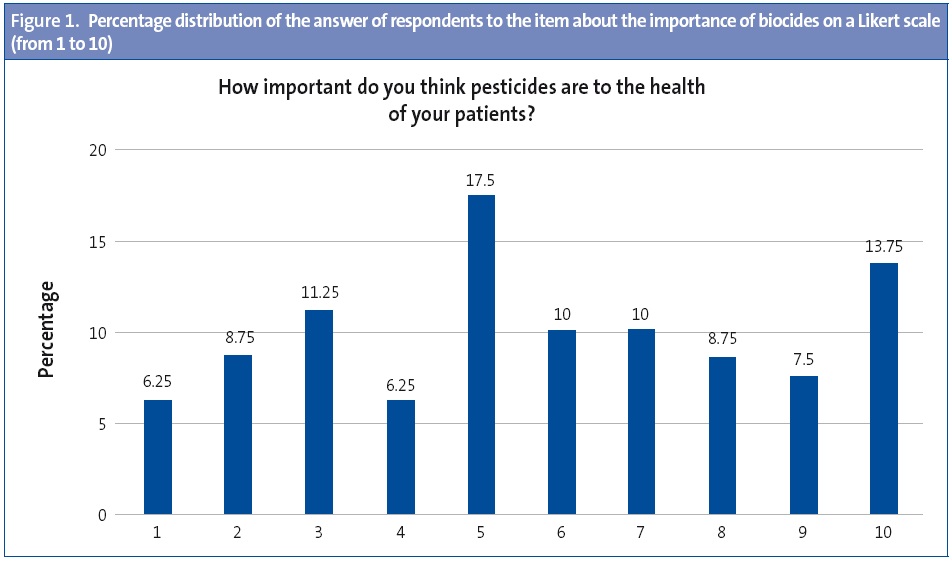
Importance of biocides: paediatricians rated the importance of biocides at 7.53 ± 2.5 (Likert scale). Fig. 1 shows the percentage distribution of the answers to this question.
Frequency of patients that sought care due to pesticides: the frequency was 2 ± 1.45 (Likert scale).
Susceptibility to pesticides: the respondents considered that the groups most susceptible to biocides were pregnant women (7.89 ± 2.5) and children (7.59 ± 2.5), compared to the rest of the population—men (5.64 ± 2.2), non-pregnant women (6 ± 2.2) and the elderly (7 ± 2.5).
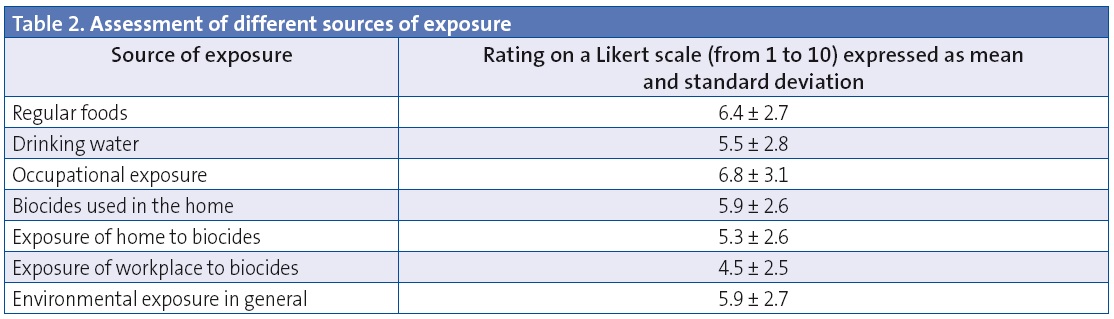
Source of exposure to pesticides: the respondents rated the various sources of exposure proposed. The results, expressed as mean and standard deviation, are shown in Table 2.
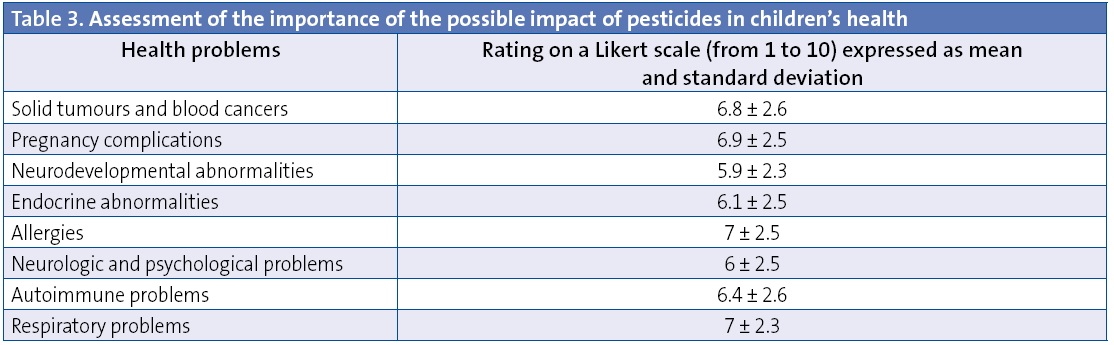
Consequences of chronic exposure to pesticides: the respondents estimated the potential health consequences of chronic exposure to biocides. The results are shown in Table 3 expressed as mean and standard deviation.
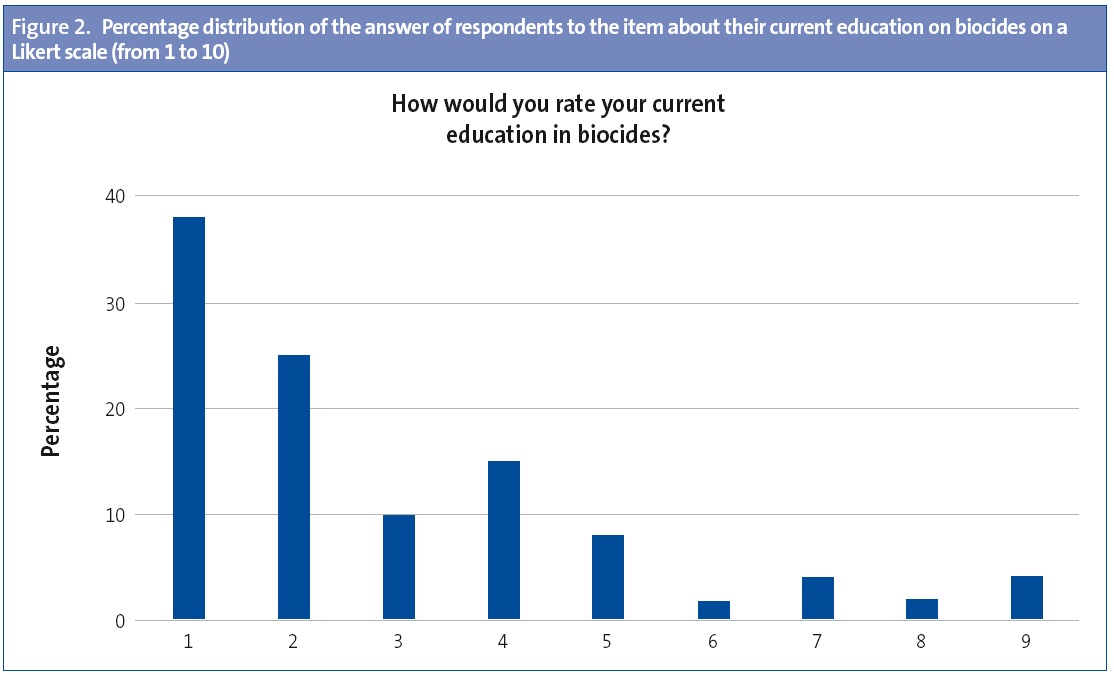
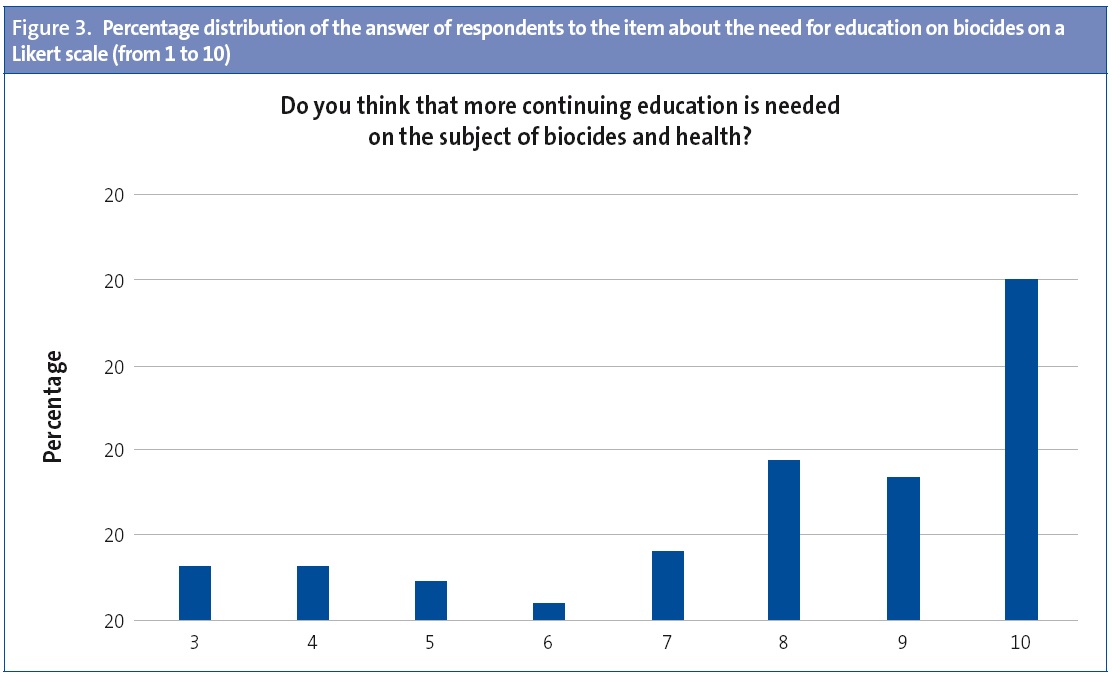
Training in pesticides: we asked about the extent of their personal training on biocides and the need for training on this subject. Their current training on pesticides was rated with a mean score of 2.7 ±1.9 and the need for further training on pesticides was rated at 8.2 ± 2.2 (Likert scale).
DISCUSSION
Paediatricians can reduce environmental exposure to different risk factors related to children’s health. To this end, the American Academy of Pediatrics created its Council on Environmental Health and published a reference book on environmental health.4
Pesticides are one of most important environmental factors affecting children’s health, as demonstrated by multiple scientific studies published in recent years.
The use of pesticides particularly affects the Canary Islands due to the distribution of its crops. Most of the central territory of the seven islands has some time of environmental protection (national parks, nature parks, areas of particular interest, etc.), with crops located in terrain near the coast, adjacent to residential and touristic areas.
We have no knowledge of any previous study assessing the importance of pesticides as a risk factor for the health of the children seen by individual paediatricians, although studies in the United States have assessed the overall training on environmental health of some paediatricians.5,6
We are aware of the limitations involved in the use of Likert scales, and the grouping of responses as means and standard deviations to analyse the results of a questionnaire to assess knowledge and attitudes, although we believe that this suffices for an initial approach to the subject of interest.
As for the importance of pesticides, it is worth noting that the surveyed paediatricians believed that pesticides are a significant factor in children’s health, as this item obtained the highest score of all (7.5 ± 2.5). This stood out in contrast to the low frequency of patients that received care for potential adverse effects of pesticides (2 ±1.4), which perhaps was due on the respondents rating this based only on their acute effects (acute poisoning) and not on the effects of chronic exposure.
The survey showed that respondents thought the highest-risk groups were pregnant women and children, which is consistent with the scientific literature.7
When it came to the sources of exposure, we did not find statistically significant differences between the various proposed sources. Overall, the pesticides present in foods are the most important source of exposure in children, as demonstrated by different studies on pesticide surveillance, but we have no evidence available for our region on the contribution of each of the sources of exposure, all of which had a combined cumulative effect.
We found no statistically significant differences in the answers of respondents about the potential health consequences of pesticides in children. While all these potential consequences has been associated with pesticides, the current literature shows that the most important ones are obstetric problems,8 malignancies,9,10 and neurologic abnormalities.11-13
On the other hand, the study evinced that respondents had received little training on biocides (2.7 ±1.45) and their perceived need of receiving further education on the subject (8.2 ±2.2). Figures 2 and 3 show the percentage distribution of the answers to both of these items.
To conclude, we may say this is the first study on pesticides as a factor affecting children’s health conducted in our region. It is our belief that primary care paediatricians should be provided with continuing education on environmental health specific to their field.
In addition, when it comes to pesticides, we believe that with approximately 250 scientific studies on “pediatric pesticide exposure” indexed in PubMed in the past five years, there is enough scientific evidence for paediatricians to start actively informing our patients, and especially pregnant women and children in the first years of life, of the potential health risks of these substances and strategies to minimise them, as a cautionary measure.
ACKNOWLEDGMENTS
The authors thank the collaboration of the administrative departments of the four paediatrics associations of the Canary Islands in sending the survey to their members by electronic mail.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS: FAO: United Nations Food and Agriculture Organization.
REFERENCES
- Organización de las Naciones Unidas para la Agricultura y la Alimentación. Código Internacional de Conducta para la Distribución y Utilización de Plaguicidas. Roma: FAO; 2006.
- United Nations Environment Programme. Childhood Pesticide Poisoning. Information for Advocacy and Action; 2004.
- Publications from the Office of Pesticide Programs: General Consumer Publications. Protectin children. En: Enviromental Protection Agency [en línea] [consultado el 12/03/2015]. Disponible en www.epa.gov/oppfead1/Publications/catalog/subpage3.htm#children
- Etzel RU, Ruth A, Balk, Sphie J. Pediatric Environmental Health. 3.ª edición. AAP; 2012.
- Kilpatrick N, Frumkin H, Trowbridge J. The environmental history in pediatric practice: a study of paediatricians’ attitudes, beliefs, and practices. Environ Health Perspect. 2002;110:823-71.
- Trasande L, Schapiro ML, Falk R. Paediatricians attitudes, clinical activities, and knowledge of environmental health in Wisconsin. WMJ. 2006;105:45-9.
- Weiss B, Amler S, Amler RW. Pesticides. Pediatrics. 2004;113:1030-6.
- Yan SM, Zhai QF, Xing J, Li WWW, Gao XC, Qiu YG. Relationship between pesticide exposure and adverse pregnancy outcomes among famers: a meta-analysis.Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2012;30:859-62.
- Bayley HD, Fritschi L, Infante-Rivard C, Glass DC, Miligi L. Parenteral occupational pesticide exposure and the risk of childhood leukaemia in the offspring: findings from the childhood leukaemia international consortium. Int J Cancer. 2014;9:2157-72.
- Van Maele-Fabry G, Lantin A-C, Hoet P, Lison D. Residential exposure to pesticides and childhood leukaemia: a systematic review and meta-analysis. Enviroment Int. 2011;37:280-91.
- Rauh V, Arunajadai S, Horton M, Perera F, Hoepner L. Seven-year neurodevelopmental scores and prenatal exposure to chlorpyrifos, a common agricultural pesticide. Environ Health Perspect. 2011;119:1196-201.
- Lovasi GS, Quinn JW, Rauh VA, Perera FP, Andrews HF. Chlorpyrifos exposure and urban residential environment characteristics as determinants of early childhood neurodevelopment. Am J Public Health. 2011;101:63-70.
- Eskenazi B, Kogut K, Huen K, Harley KG, Bouchard KG. Organophosphate pesticide exposure, PON1, and neurodevelopment in school-age children from the CHAMACOS study. Environ Res. 2014;26:149-57.





