Vol. 26 - Num. 103
Original Papers
Profile of the limping child
Verónica Gimeno-Hernández Garzaa, Álvaro García Atarésb, Marisol Camacho Lovilloc
aServicio de Pediatría. Hospital Ernest Lluch. Calatayud. Zaragoza. España
bPediatra. CS de Caspe. Zaragoza. España
cServicio de Pediatría. Hospital Virgen del Rocío. Sevilla. España.
Correspondence: V Gimeno-Hernández . E-mail: vgimenohernan@salud.aragon.es
Reference of this article: Gimeno-Hernández Garza V, García Atarés A, Camacho Lovillo M. Profile of the limping child . Rev Pediatr Aten Primaria. 2024;26:255-62. https://doi.org/10.60147/194309a5
Published in Internet: 16-09-2024 - Visits: 8817
Abstract
Introduction: lameness is a frequent reason for primary care and emergency department visits.
Material and methods: observational, longitudinal, retrospective study in patients who presented with lameness to the emergency department of a tertiary care hospital between 2019-2022. Patients were included by systematic random sampling. The study variables were: age, sex, time from onset, associated symptoms, history of trauma, personal and family history, source of referral (provider vs self), examination findings, diagnostic tests and results, treatment, diagnosis in emergency department, final diagnosis, aetiological group and discharge destination.
Results: 321 patients, 65.1% male, with a mean age of 5.5 ± 3.4 years. Sixty percent sought care within 24 hours of onset and 81.6% were self-referred. Diagnostic tests were ordered in 87.5% (X-rays in 55.7%). The most common aetiology was inflammatory (29%), chiefly on account of transient synovitis (24%). We found an association between provider referral and a higher priority in triage (p=0.03), the use of ultrasound (p=0.009) and referral to outpatient specialists (p=0.003).
The mean age of patients with abnormal sonographic findings (5.65 years) was higher compared to patients with normal results (3.84 years). There were also mean differences in the ages of the different aetiological groups (p=0.000) and in the different diagnoses made in the emergency department (p=0.002). We found an association between the presence of previous symptoms and the aetiological group (p=0.000) and between the time elapsed from onset to the visit and the aetiological group (p=0.002), interconsultation with traumatology (p=0.000) and destination after discharge (p =0.000).
Conclusions: most causes of lameness are banal, but a high index of suspicion should be maintained for less frequent alternative diagnosis that may have more serious repercussions, such as JIA.
Keywords
● Gait ● LimpINTRODUCTION
Lameness is a change in the normal gait pattern in a child resulting in difficult, erratic or uneven walking, with an acute or subacute onset, resulting from pain, muscular weakness or skeletal deformities.
It is important to differentiate physiological gait variants (genu varum/valgus, flat feet, metatarsus adductus or idiopathic toe walking). In young children, it may manifest as refusal to bear weight on the affected limb. Based on the presence or absence of pain, it can be classified as antalgic gait or abnormal gait unrelated to pain.
This is one of the most frequent reasons for primary care and emergency department visits, with a reported incidence of 1.8 cases per 1000 children under 14 years excluding cases secondary to traumatic injury.1 In consequence, limping requires an expeditious approach to screen for causes that require urgent treatment or are potentially serious, and close follow-up until its resolution.2 The differential diagnosis can be made with a thorough history and physical examination, which together constitute the first and most important step in the diagnostic process.
The following information should be collected in the history-taking:
- Age and sex.
- Time of onset and time elapsed from onset to visit, characteristics of the limp.
- Presence or absence of pain, location of pain, mechanical (worsens with activity), inflammatory (worsens with rest) or mixed pain, factors that make the pain better or worse, impact on daily life and on sleep.
- History of trauma: a fall may be due to pre-existing pain and not necessarily the cause of the pain. Up to one in three patients with lameness associated with osteoarticular infection has a history of trauma, so the history of trauma should be carefully assessed, especially in children aged less than 3 years.
- Presence or absence of associated symptoms: malaise, fever or low-grade fever in the past few days or at the time of consultation, respiratory infection, cutaneous lesions, vomiting, diarrhoea or constipation, personal history (vaccination, infection, trauma, etc.) and family history (rheumatic/autoimmune disease, history of acute or chronic pain in a relative, psychosocial problems, etc.).
The physical examination should include an assessment of the patient's general health, locomotor system and gait. It should also include a review of body systems, as lameness may be a manifestation of a systemic disease, with particular emphasis on the search for cutaneous lesions, abdominal signs or signs of neurological involvement. In some cases, the examination is difficult due to the patient's lack of cooperation, especially in younger patients, taking more time to complete.
In some cases, the information obtained in the history-taking and physical examination does not suffice to reach a definitive clinical diagnosis and, depending on the clinical condition of the patient, the duration of symptoms and the possible diagnoses, it may be necessary to perform laboratory tests3 (essentially acute phase reactants such as: C-reactive protein [CRP], procalcitonin [PCT], erythrocyte sedimentation rate [ESR], a complete blood count with creatin kinase [CK] in the case of suspected acute myositis) and/or imaging tests (X-ray, ultrasound, bone scintigraphy scan or magnetic resonance scan).4
If we classify lameness according to the suspected aetiology, the main groups are:
- Traumatic, such as toddler’s fractures, sprains, stress fractures associated to sport, etc.).
- Inflammatory or immune-related, such as some forms of arthritis, transient synovitis (TS) and benign acute myositis.
- Infectious, such as arthritis, osteomyelitis and discitis. It may be associated with fever/low grade fever and/or malaise and/or elevation of acute phase reactants (CRP and ESR).
- Other osteoarticular causes, such as osteochondritis/osteochondrosis, Perthes disease, slipped capital femoral epiphysis, developmental dysplasia of the hip not diagnosed in the neonatal period.
- Neuromuscular, such as mild cerebral palsy undetected in the first months of life.
- Oncological/haematological: systemic symptoms such as asthenia, unjustified irritability, anorexia, weight loss, pallor or fever of unknown source, among others, are red flags suggestive of potential malignant disease.5
- Factitious/pretend.
As we can see, the range of possible diagnoses for paediatric limp is broad, which is compounded by the difficulties that may be encountered in the assessment of the locomotor system in non-cooperative children. Therefore, lameness can pose a challenge for the professional managing these patients and lead to underdiagnosis of less common conditions, like rheumatic diseases, in the initial visit. Awareness and early suspicion in primary care and emergency departments would allow appropriate referral, preventing diagnostic delays and, consequently, potentially serious sequelae.6-8
Hypothesis: in paediatric practice, there is a low index of suspicion of rheumatic disorders as a cause of lameness, especially in the first visit, which results in diagnostic delay compared to other aetiological groups.
The primary objective of the study was to analyse patients presenting to the paediatric emergency department of a tertiary care hospital with abnormal gait or lameness.
The secondary objectives were:
- Describing the characteristics of these patients.
- Assessing the aetiological trends in these patients, grouping causes into traumatic, inflammatory, infectious, other osteoarticular, neuromuscular, oncological/haematological and factitious/pretend.
- Analysing which signs and symptoms were associated with each of the described aetiological profiles.
- Analysing the diagnostic tests ordered at the emergency department.
- Finding out the definitive diagnoses in these patients.
- Assessing whether the final diagnosis was consistent with the suspected diagnosis made in the emergency department.
- Establishing the time elapsed to correct diagnosis in this type of patient and whether there were differences in the diagnostic delay between aetiological groups.
MATERIAL AND METHODS
We conducted a retrospective, observational, descriptive, and analytical study. The study universe consisted of the patients who visited the emergency department of a tertiary care hospital between January 1, 2019 and December 31, 2022.
The inclusion criteria were:
- Age 0 to 14 years, visiting the emergency department of the Miguel Servet Children's Hospital, limping/lameness/abnormal gait as the reason for the visit assigned at triage.
- Date of emergency department visit between 1 January 2019 and 31 December 2022.
On the other hand, the exclusion criteria were:
- Age 15 or more years, as the study focused on the paediatric population, which in our autonomous community (with some exceptions) encompasses children aged up to 14 years and 12 months, and admission to the emergency department of the Miguel Servet Children's Hospital for chronic/complex pathology in patients currently in followup in the hospital.
- Leaving the emergency department, before or after receiving care, without being discharged by the care team.
- Refusal of consent to diagnostic tests ordered by the physician in charge after the initial assessment.
The sample was obtained from the total pool of eligible patients through systematic random sampling, with selection every third case. The two primary outcomes of the study were: diagnosis at discharge from the emergency department and aetiological group corresponding to the diagnosis.
The secondary variables concerned the following aspects: epidemiological characteristics (sex, age, primary care centre and health area to which the patient was assigned), date of ED visit, history (patient referred from primary care/hospital or self-referred, personal or family history of trauma, rheumatic and/or neurologic disease, personal history of any other form of chronic disease, history of previous trauma or vaccination on that limb, concurrent or previous symptoms, limp pattern), physical examination (presence or absence of limping in emergency department, type of gait, involved limb and/or joint, presence of pain on palpation/mobilisation, generalised/localised pain and location of pain, presence of cutaneous lesions and/or local or regional inflammatory signs, and presence or absence of focal neurologic signs), testing (whether X-ray, ultrasound, blood tests, joint fluid analysis were performed, whether the results were normal/inconclusive/abnormal, performance of tests in other centres or in previous visits to our hospital’s ED including which tests were performed, total number of tests performed), patient management (monitoring by paediatrician, referral to outpatient clinic, monitoring in emergency department within 5 days, hospital admission, previous treatments, prescribed treatment and total number of prescribed therapeutic measures), and diagnosis (final diagnosis of the patient and date of final diagnosis).
The statistical analysis of the data was carried out with the SPSS software. We performed a descriptive analysis of the sample. To assess the normality of the distribution of quantitative variables, we used the Kolmogorov-Smirnov or Shapiro Wilk test as applicable based on the number of observations available for the variable. We used the chi square test to assess for the presence of significant associations between groups in the tabulated categorical variables. To assess the association between a qualitative variable and a quantitative variable, we used the Student t test or, for variables with more than 2 categories, analysis of variance (ANOVA). To assess the association between two quantitative variables, we calculated the Pearson's correlation coefficient. We considered results statistically significant if the p value was less than 0.05.
The study was approved by the Research Ethics Committee of our autonomous community.
RESULTS AND DISCUSSION
Lameness accounted for 0.53% of emergency department visits in our hospital. A total of 321 patients were analysed in our study, 65.1% male, with a mean age of 5.53 ± 3.46 years and epidemiological characteristics similar to those described by other authors.9,10
Approximately 80% of the patients were self-referred and classified as priority level 4 in triage. Furthermore, 59.92% visited within 24 hours of the onset of lameness. This suggests that, although most of the causes of lameness are benign and resolve spontaneously,1 this is a complaint that generates significant worry in families, who frequently seek care early and/or in the emergency or urgent care setting.
Of all patients, 22.7% had experienced flu-like or gastrointestinal symptoms before the onset of lameness, 8.1% had them at the time of the emergency department visit and 0.6% had isolated fever concurrent with the onset of lameness. There was a statistically significant association between the history of previous o concurrent systemic symptoms associated with lameness and the aetiological group (p = 0.000), which underscores the importance of a detailed history-taking in these patients including the history of recent viral illness for diagnosis of transient synovitis.11 The history-taking must thoroughgoingly explore the previous or current presence of fever/low-grade fever, asthenia, myalgia, weight loss (which could suggest a rheumatic, infectious or oncological/haematological aetiology), symptoms indicative of respiratory or gastrointestinal tract infection (which are more suggestive of an inflammatory aetiology such as TS or reactive arthritis). The physical examination, in addition to an exploration and description of gait abnormalities, local inflammatory signs in the lower extremities and range of motion and pain in the joints, should include a review of body systems to rule out organ enlargement, cutaneous lesions or inflammatory signs in other joints that could be key to the diagnosis. A thorough history-taking and physical examination could avoid the performance of unnecessary tests.
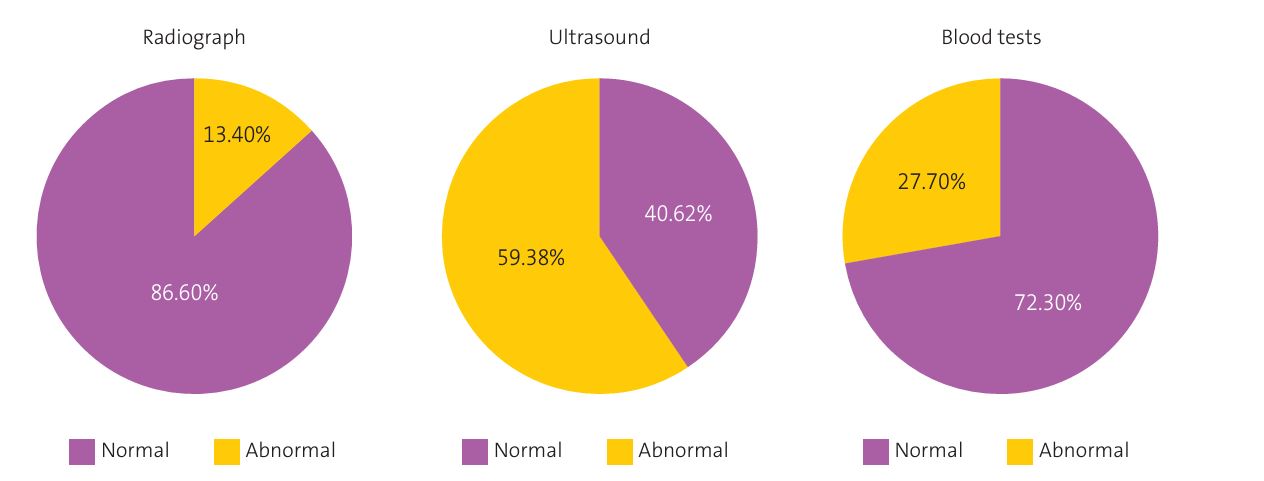
Diagnostic tests were ordered in a significant percentage of patients (87.5%), and the most frequently ordered test was the plain X-ray (55.76%), followed by ultrasound (19.93%), blood tests (11.21%) and arthrocentesis (0.62%). The yield of radiography and blood tests (abnormal results in 13.4% and 27.7% , respectively) was lower compared to ultrasound and arthrocentesis (abnormal results in 59.38% and 100%, respectively) (Figure 1). The frequency with which laboratory or imaging tests were ordered differed from previous reports by Tu et al.,10, who described ordering of imaging tests in 51% and laboratory tests in 39%, and by Murias et al.,12 who reported ordering of radiographs in 31.13%, ultrasound scans in 26.88% and blood tests in 64%. However, the data from these studies may not be comparable, since Tu et al.10 conducted a retrospective study in a paediatric emergency department that excluded patients with a history of traumatic injury and Murias et al.12 a study of patients referred to rheumatology.
We found a statistically significant association between referral by a provider and the performance of ultrasound examinations (p=0.009), which may have to do with the appropriateness of the test, in addition to the older age of patients with abnormal sonographic findings compared to those with normal findings (5.65 years vs. 3.843). A possible explanation of the latter is that in older children, ultrasound is requested on account of a more specific suspicion of synovitis or arthritis compared to younger children, in whom the nonspecificity of symptoms and the challenges in the physical examination may result in the ordering of diagnostic tests with the aim of ruling out diseases rather than making a more accurate diagnosis.
We did not find an association between the source of referral to the emergency department (provider/self) and the total number of ordered tests, which could be due to the small percentage of patients referred by providers and the high percentage of cases in which tests were ordered. We also found no association between the history of trauma prior to onset of lameness and the presence of radiographic abnormalities, which suggests that X-rays may be unnecessary in the case of mild trauma, nor between the history of trauma and subsequent interconsultation with the trauma department, which may be due to the history of previous trauma being unrelated to current complaint (correctly treated previous fracture or hip dysplasia).
We found significant differences in mean age between the different aetiological groups, for instance, between cases with an inflammatory cause vs. a different osteoarticular cause (p = 0.00) (Table 1), which was consistent with previous evidence that an inflammatory aetiology is more frequent in infants and young children, while other osteoarticular aetiologies, such as osteochondritis, are more frequent in school-aged children and adolescents.13
| Table 1. Differences in mean age between the different aetiological groups | ||||
|---|---|---|---|---|
| Aetiological group | n | Mean | SD | p |
|
Traumatic Other osteoarticular |
84 31 |
5.53 8.71 |
3.62 3.34 |
0.000 |
|
Inflammatory Other osteoarticular |
93 31 |
4.53 8.71 |
2.45 3.34 |
0.000 |
|
Unknown Other osteoarticular |
91 31 |
5.46 8.71 |
3.61 3.34 |
0.000 |
|
n: number of patients; SD: standard deviation. |
||||

The most frequent aetiology of lameness was inflammatory (29%), followed by trauma (26.25%), other osteoarticular causes (9.7%), neuromuscular (2.2%), infectious (1.6%) and oncological/haematological (0.6%). The aetiology of lameness was not identified in the emergency department visit in as many as 28.3% of patients. The most frequent discharge diagnosis was synovitis of the hip (24%), followed by lameness (23.1%), pain of the lower extremity (15.3%) and bruising (9.03%). In 2.49% of patients (n = 8), the definitive diagnosis was different from the initial diagnosis in the emergency department, most frequently JIA. Thus, 5 patients had a final diagnosis of arthritis as the cause of lameness. This corresponds to an incidence in our sample of 0.015 cases per patient presenting with lameness in our hospital. In 2 of these patients (one with septic arthritis and another with reactive arthritis) the diagnosis was suspected in the emergency department, while the 3 cases of JIA were diagnosed later on in the outpatient rheumatology clinic, indicating that there is a low index of suspicion of rheumatic disease at first contact with the health care system.
Among the possible future lines of research, one would be to carry out the same study in patients presenting with lameness in primary care and see if the results differ. Another possibility would be to repeat the study after delivery of specific training in the assessment of the locomotor system to emergency care paediatricians, primary care paediatricians and medical residents (who are usually the provider that carry out the initial evaluation for this complaint), in order to assess whether this intervention decreases the number of tests ordered through the improvement of the initial clinical diagnosis.
CONCLUSION
Lameness accounted for 0.53% of emergency department visits in our hospital. The mean age of the patients was 5.53 ± 3.46 years. Of this total, 81.6% were self-referred and almost 60% visit within 24 hours of the onset of lameness. Diagnostic tests were ordered in 87.5% of the patients, most frequently plain radiographs (55.76%), followed by ultrasound examinations (19.93%). The sonographic findings were abnormal in 59.38% of the performed ultrasound scans.
The most frequent aetiology of lameness was inflammatory (29%) and the most frequent diagnosis at discharge from the emergency department was TS (24%). In 2.49% of patients, the final diagnosis was different from the diagnosis at discharge from the emergency department, most frequently JIA.
Referral from a provider was significantly associated with higher triage priority, more frequent performance of ultrasound examinations and more frequent referral of the patient to outpatient speciality care.
We found significant differences in the mean age of patients in different aetiological groups, which was consistent with the previous literature, and the mean age of patients with abnormal sonographic findings was greater compared to those with normal findings.
Patients with lameness of an inflammatory aetiology were more likely to have had previous symptoms, chiefly febrile illness (57.1%), cold symptoms (66.7%) or gastrointestinal symptoms (81%).
Establishing the profile of patients with lameness managed in the emergency care setting will allow us to identify areas of improvement.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
AUTHORSHIP
Author contributions: study conception and design, database development, statistical analysis and interpretation of results, drafting of manuscript, approval of final version of manuscript (VGHG, AGA), study conception and design, critical review of the manuscript with relevant intellectual contributions, approval of final version of manuscript (MCL).
ABBREVIATIONS
CBC: complete blood count; CK: creatine kinase · CRP: C-reactive protein · ESR: erythrocyte sedimentation rate · JIA: juvenile idiopathic arthritis · PCT: procalcitonin · TS: transient synovitis.
REFERENCES
- Fischer SU, Beattie TF. The limping child: epidemiology, assessment and outcome. J Bone Joint Surg Br. 1999;81(6):1029-34. https://doi.org/10.1302/0301-620x.81b6.9607
- Staheli LT. Fundamentals of Pediatric Orthopedics. 4th Ed. Philadelphia: Lippincott Williams and Wilkins; 2006.
- Abbassian A. The limping child: a clinical approach to diagnosis. Br J Hosp Med (Lond). 2007;68(5):246-50. https://doi.org/10.12968/hmed.2007.68.5.23330
- Jain N, Sah M, Chakraverty J, Evans A, Kamath S. Radiological approach to a child with hip pain. Clin Radiol. 2013;68(11):1167-78. https://doi.org/10.1016/j.crad.2013.06.016
- Jones OY, Spencer CH, Bowyer SL, Dent PB, Gottlieb BS, Rabinovich CE. A multicenter case-control study on predictive factors distinguishing childhood leukemia from juvenile rheumatoid arthritis. Pediatrics. 2006;117(5):e840-4. https://doi.org/10.1542/peds.2005-1515
- Antón J, Camacho Lovillo M, Núñez Cuadros E. Reumatología Pediátrica, de dónde venimos y a dónde vamos. An Pediatr (Barc). 2020;92(3):121-3. https://doi.org/10.1016/j.anpedi.2020.01.003
- De Inocencio J, Antón J. Reumatología pediátrica. Breve historia y situación de la especialidad en España. Acta Reumatológica. 2014;1(2):37-43.
- Spencer CH. Why should pediatric rheumatology be recognized as a separate subspecialty: an open letter to medical councils and government agencies. Pediatr Rheumatol Online J. 2007;21(5):21. https://doi.org/10.1186/1546-0096-5-21
- Sawyer JR, Kapoor M. The limping child: a systematic approach to diagnosis. Am Fam Physician. 2009;79(3):215-24.
- Tu J, Haines M, Gowdie P, Craig S. Paediatric acute non-traumatic limp presenting to the emergency department: a retrospective observational study. Emerg Med J. 2023;40(3):182-8. https://doi.org/10.1136/emermed-2022-212624
- Irfan A, Starr RJ, Foster S, Smith ID, Huntley JS. 'Irritable Hip': Diagnosis in the Emergency Department. A Descriptive Study Over One Year. Cureus. 2018;10(10):e3481. https://doi.org/10.7759/cureus.3481
- Murias S, Remesal A, Quiles MJ, Merino R. Características de los pacientes con cojera en Reumatología. An Pediatr (Barc). 2012;76(5):290-3. https://doi.org/10.1016/j.anpedi.2011.10.011
- Santili C, Lino Júnior W, De Oliveira Goiano E, Barreto Lins RA, Waisberg G, Dos Reis Braga S, et al. Limping in Children. Rev Bras Ortop. 2015;44(4):290-8. https://doi.org/10.1016/S2255-4971(15)30156-7