Vol. 26 - Num. 102
Original Papers
The speciality of Paediatrics continues to be of interest to residents
Pedro J. Gorrotxategi Gorrotxategia, Concepción Sánchez Pinab, Carmen Villaizán Pérezc, M.ª Teresa Cenarro Guerrerod, M.ª Dolores Cantarero Vallejoe, Eva Suárez Vicentf, Marianna Mambié Meléndezg
aPediatra. CS Pasajes San Pedro. Pasajes. Guipúzcoa. España.
bPediatra. CS San Andrés. Madrid. España.
cPediatra. CS Toledo 4-Santa Bárbara. Toledo. España.
dPediatra. CS José Ramón Muñoz Fernández-Ruiseñores. Zaragoza. España.
ePediatra. CS Illescas . Illescas. Toledo. España.
fPediatra. CS. Burriana II. Burriana. Castellón. España.
gPediatra. CS Son Serra-La Vileta. Palma de Mallorca. España.
Correspondence: PJ Gorrotxategi. E-mail: pedro.gorrotxa@gmail.com
Reference of this article: Gorrotxategi Gorrotxategi PJ, Sánchez Pina C, Villaizán Pérez C, Cenarro Guerrero MT, Cantarero Vallejo MD, Suárez Vicent E, et al. The speciality of Paediatrics continues to be of interest to residents . Rev Pediatr Aten Primaria. 2024;26:147-54. https://doi.org/10.60147/a45613e8
Published in Internet: 13-06-2024 - Visits: 15518
Abstract
Introduction: the objective of our work as to analyse the interest of residents who begin their training in the specialty of paediatrics and its specific areas, based on the order in which open residency spots were filled throughout the years.
Methodology: analysis of data obtained from the register of the medical intern resident (MIR) selection process in the past 9 years, current paediatrician positions in the National Health System and a study on the projected need for medical specialists in 2021-2035.
Results: in the last nine years, there has been an increase in the number of available spots from 392 to 501. Since more spots are available now, the last one is, as expected, filled later in the selection process. Thus, the delay in spot allocation has been of 49%, but if the number of spots had not increased, it would have been of 17%. The number of candidates who could not choose paediatrics because all residency spots had been filled when their turn arrived increased by 28% from 2703 to 3469. Given that the rate of transfer or attrition in the paediatrics residency programme is minimal, it would be possible to offer more spots, as they would be filled appropriately. Most job openings in paediatrics are in primary care (65%) followed by hospital-based paediatric care (35%).
Conclusions: paediatrics continues to be an appealing speciality for candidates to MIR training. If more MIR spots were offered, more residents would choose the paediatrics specialty. Given that most job opportunities are ins primary care, training in this setting should be reinforced in the MIR programme.
Keywords
● Primary Care Paediatrics ● Resident Training ● TeachingINTRODUCTION
Amid the dire challenges currently faced by the primary care (PC) system, spots for training in the family medicine speciality are being left unfilled in the medical intern-resident (MIR) selection process. In the words of Armando Martín-Zurro, “the current situation of PC in Spain could be described as ‘concerning’. Work overload, a lack of professionals to cover substitute positions and posts in particularly challenging settings, excessive paperwork, the limited prospects for personal and professional growth, problems with work-life balance, low wages and precarious work are among the root causes of burnout, which is spreading like wildfire through the PC system.”1 This situation could also affect the speciality of paediatrics, as most jobs in the field are at the PC level, which may reduce the satisfaction of residents with the available spots in paediatrics.
Some reports in the press have described a waning interest in paediatrics among residents, suggesting that this specialty is losing its appeal. One such article, titled Los médicos con las mejores notas MIR ya no quieren ser paediatricians: así se “desinfla” la especialidad (Doctors with the best marks in the MIR exam no longer want to become paediatricians: how the speciality “deflates”)2 asserted that the speciality had “deflated” and attributed the problem to the on-call shift requirements: “In first-call specialities, like paediatrics, the on-call shift requirement has turned into working at a breakneck pace 24 hours a day”. A paediatrician interviewed for the article also commented on the poor working conditions: “If future residents see that PC paediatricians have crushing workloads and their working conditions are not good, it is no surprise that they end up choosing a different speciality”, and, lastly, a representative of the Asociación Española de Pediatría de Atención Primaria (AEPap, Spanish Association of Primary Care Paediatrics) expressed a totally opposite opinion, remarking that paediatrics was very appealing for doctors because it is a speciality in which providers are in contact with patients and concluded that “paediatrics is not in a slump”.
Taking into account these differing perspectives of professionals in the field of paediatrics, we undertook a study to analyse, first of all, whether there has indeed been a reduction in the acceptance of paediatrics speciality MIR spots by doctors in training and the extent to which these spots are filled out later than before; and, secondly, the outlook for careers in paediatrics as a medical speciality.
METHODS
We analysed data for the allocation of the last MIR training spot in paediatrics in the past 9 years. To do so, we used the report of the Centro de Estudios del Sindicato Médico de Granada (Centre of Studies of the Union of Physicians of Granada): Distribución adjudicaciones de plazas MIR en 2023.3
We analysed the number of spots offered for paediatrics training at the PC and hospital levels in the past 10 years based on data from the Ministry and assessed the current situation in the field of paediatrics through the study on the needs for specialists for the 2021-2035 period.
First, we considered the process by which MIR training spots are filled and asked the following questions: Has the delay in the allocation of spots in paediatrics increased in the yearly MIR selection? What factors contributed to the delay in candidates choosing paediatrics spots? How many candidates seeking to train in paediatrics failed to secure a MIR spot in this speciality?
Secondly, to assess the current situation of the field, we considered aspects concerning professional opportunities and the field of primary care paediatrics: What are the career opportunities for residents in paediatrics? Is the field of primary care paediatrics at risk?
RESULTS
Has the delay in the allocation of spots in paediatrics increased in the yearly MIR selection?
We answer this question with the data from the MIR selection process report of May 9, 2023 of the Centro de Estudios del Sindicato Médico de Granada, titled: Distribución adjudicaciones de plazas MIR en 2023 (Distribution of allocation of MIR training spots in 2023).3 The report details every open spot, and the order in which the first and the last spot were filled for each speciality based on the ranking and preferences of the candidates.
The report offers this information for the past 9 years, and a first perusal suggests that there has been considerable delay in the order in which candidates chose paediatrics spots: in 2015 the last paediatrics spot was allocated in 3399th place compared to 5081st place in 2023, a 49% delay. However, this is not an accurate picture, as in the same period the number of spots in paediatrics increased from 392 to 501. Adjusting the calculation to the increase in the number of spots, the actual delay in the allocation of spots was 17%, as can be seen in Figure 1.
| Figure 1. Trends in the allocation of the last spot in paediatrics residency training |
|---|
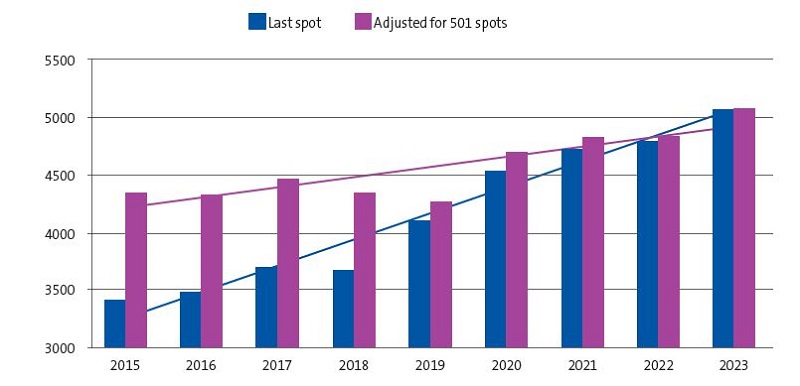 |

What factors contributed to the delay in candidates choosing paediatrics spots?
An important contributing factor in when in the selection process spots are filled is the total number of spots open for training in a given speciality.
As an example, we can consider the legal and forensic medicine speciality. It was the fifth in having all spots filled. However, only 8 spots were available, and the last was filled in 3231th place, whereas the last spot in paediatrics was filled in 5081th place. Therefore, the candidate ranking number at which all spots have been allocated must be considered in relation to the total number of available spots.
Going back to the assessment of the allocation of paediatrics MIR spots throughout the years, if we were to analyse the data again as if the number of spots had not increased and had remained at the original 392 spots offered in 2019, as can be seen in Figure 2, the last paediatrics spot in 2023, which was actually filled in 5081th place, would have been filled in 3975th place.
| Figure 2. Trend in the allocation of the last spot if the number of spots had not changed throughout the 2015-2023 period |
|---|
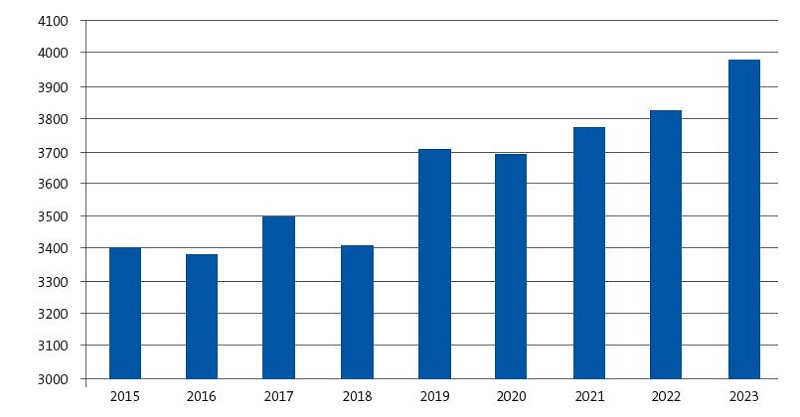 |

We found that the number of spots remained stable from 2015 to 2018 and increased from 2019. This was due to a substantial increase in the availability of spots, of 11.1%, that took place in 2019 as the number of spots offered in paediatrics went from 433 to 481.
How many candidates seeking to train in paediatrics failed to secure a MIR spot in this speciality?
If the total number of MIR spots is 8550 and the number at which the last paediatrics spot was filled was 5081, that means that 3469 MIR candidates could not choose paediatrics because there were no spots left. This is not to say that all these candidates wished to specialize in paediatrics, which is clearly not the case, but they did not have the option. So, has this number decreased or increased in the past few years?
Looking at the trends in MIR spots, we can see that the number of residents that did not have the option of a spot in paediatrics increased by 28%. In 2015, 2703 candidates that did not have the option of picking a spot in paediatrics because all spots had been filled by the time it was their turn to choose, and in 2023 this number had increased to 3469.
What are the career opportunities for residents in paediatrics?
Residents that choose the speciality of paediatrics are aware that most of the job opportunities will be in PC paediatrics. According to data of the Ministry for 2021, the number of paediatricians working in hospitals and in PC is of 47524 and 6474,5 respectively. Thus, 42% of jobs are in the hospital setting and 58% in the PC setting. This despite a proportional increase in the number of hospital positions in the past 10 years, as the distribution in 2010 was 38% of positions in hospitals and 62% in PC, as can be seen in Figure 3.
| Figure 3. Number of paediatrician positions in the hospital and primary care systems in the 2010-2021 period according to data from the Ministry of Health |
|---|
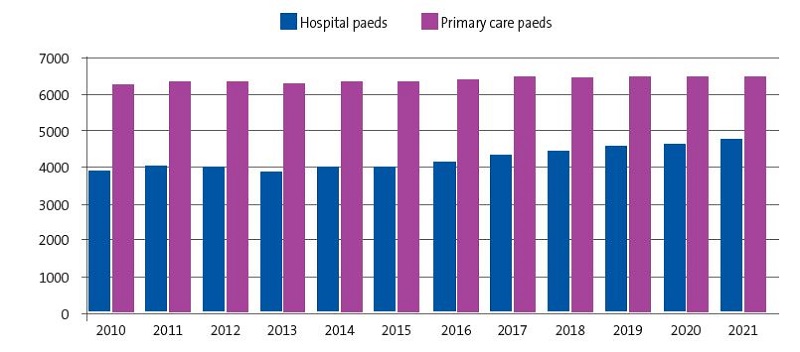 |

Another aspect to consider in terms of future career opportunities is the mean age of paediatricians currently employed in PC and in hospital settings, which differs widely. According to the report on the supply and demand of medical specialists for 2021-2035,6 the age distribution is very different for these two settings, with a higher age in PC. Primary care paediatricians are older: 52.8% are aged 50 years or more, compared to 27.6% of hospital-based paediatricians. While 1 in 5 paediatricians in the PC system will reach retirement age in the next 5 years, only 11% of hospital-based paediatricians are in this pre-retirement age interval (Figure 4).
| Figure 4. Percentage of paediatricians aged more than 50 years and aged more than 60 years in primary care vs. hospital setting |
|---|
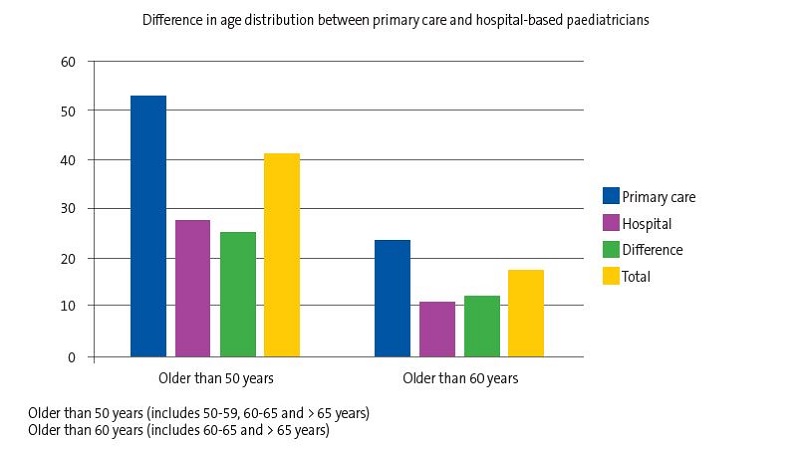 |

If we add the data on the professionals currently active that are going to retire in the next 15 years, 52.8% of those in PC and 27.6% of those in hospitals, then 9872 paediatricians will be needed in the PC system and 6063 to provide hospital-based care. This means that 62% of open positions correspond to PC and 38% to hospital-based care.
Another datum from the same report is that paediatrics, which happens to be the second speciality for which the most MIR training spots are offered each year, is the speciality for which the transfer or dropout rate is lowest among all speciality training programmes. Nearly all residents that start training in paediatrics complete it, which indicates that they find the speciality satisfactory.
DISCUSSION
The reasons that residents consider in choosing or ruling out a speciality are based on the image of it projected by practicing professionals or other residents. Therefore, we analysed the opinions shared by these groups. First, we will discuss the personal opinions of residents and then the findings of studies that gathered these opinions at the collective level.
As regards personal opinions, the coordinator of the MIR Group of the Asociación Española de Pediatría (AEP, Spanish Association of Pediatrics) highlighted the scarcity of research opportunities in primary care as one of the problems. She said: “Once you get familiarized with it and start working, you fall in love with the core work of the paediatrician, the prevention, diagnosis and treatment of disease in children and adolescents. The day-to-day practice is different for each professional, some paediatricians work exclusively in hospital, while others focus on PC, so their work is completely different. It is in PC, actually, which is so overburdened and lacking in resources, where the workloads are so heavy, that it is very difficult to carve out the time during working hours to devote to research.”7
A first-year resident in the Hospital Severo Ochoa of Leganés, in response to the question: “Are you contemplating the possibility of working in a primary care centre?”, replied: “In principle, I don’t consider it. Hospital work suits my personality better; now that I am young and eager, I want to experience the pace of the hospital and the on-call shifts. However, I do think that the primary care centre may offer an alternative in the future. After working a few years, once I start a family, I may want to slow down, and that may be possible at the primary care centre, to not have to do on-call shifts when I feel I no longer have the stamina for it and to devote myself to the followup of healthy children. I also like research, which is an essential part of being a medical professional. To stay up to date, to stimulate and promote research is essential in order to continue advancing in medicine. Without research, we would not be able to enjoy all the advances we have today.”8
It is clear that, like the previous resident, she believes that there is more going on in the hospital and that it is possible to conduct research in this setting.
Another resident, in the fourth year of the training programme in the Hospital Materno-Infantil de Málaga, had a very different perspective, saying: “The reason I feel passionate about PC may be that it entails providing holistic care to the patients while participating in their growth and development, as PC allows an ongoing relationship both with the ‘healthy’ child and with children who have any kind of illness, and you can track the course of children in your caseload and become acquainted with their personal characteristics and those of their families. There is more rapport between physician and patient and more engagement on both sides. The primary care paediatrician tends to be the first contact when any health problem arises, which makes one feel useful and have a sense of responsibility. On the other hand, the paediatrician is also a parent educator, trying to foster habits and procedures that will have a positive impact on the health of their children. A certain bond forms with the families and caregivers that promotes mutual learning. Primary care is like a large and very varied salad that comes with different ingredients each day. Even if the basic elements are the same, there are multiple possibilities for novelty. Primary care paediatricians should feel proud of the work they do every day and be aware of the very relevant role they play in our society and the enormous good they do for millions of families that entrust them with what is most precious to them, their children.”9 The same resident went on to say, “In my first years in the hospital, PC was hardly ever mentioned. Still, I was surprised at how short the rotation in PC was, given the large proportion of residents in paediatrics that end up working in PC centres. From the outside, and for some people (thankfully, not most people), this area appears monotonous, boring and, even, something they view with a touch of derision. However, this view is biased and distorted. One must go out there and see for oneself, we should not take what they say at face value, we should keep an open mind and see this different world with our own eyes.” Thus, this resident that feels “passionate about PC” mentions touches on two key aspects, the short duration of the rotation in primary care and the contempt with which primary care is perceived in some fields of paediatrics.
As regards the second aspect, the gathering of opinions of groups of residents, we are presenting two examples.
In 2009, a survey of 61 residents who attended the XIV Course of Continuing Education for Fourth-Year Residents in Paediatrics in Spain,10 which had the limitations intrinsic to a survey in a restricted group whose representativeness of the entire population of residents cannot be determined, yielded the following results: most residents (90%) considered the residency mentor an important role, however, the ratings they gave their MIR mentors varied widely between 0 and 10 points, with a median of 6, 35% of mentors received a score under 5 points. All considered the rotation in PC useful, although most respondents (70%) reported a short duration of the rotation of 2 to 3 months. Lastly, we ought to mention that as they neared completion of the MIR programme, 2 out of 3 residents already had secured a position, chiefly in hospitals (80% of those who had a confirmed job offer).
In 2017, the AEPap conducted a survey with participation of 117 residents, amounting to 7% of the total residents in Spain, finding that 98% considered a rotation in PC necessary. In addition, 75% believed they would eventually work at the PC level, 43% wanted to work in PC and 55% would not mind although it would not be their first choice. Fifty-one percent considered that the adequate duration for the rotation would be 4 months, and only 11% considered a duration of less than 3 months adequate.11 In this survey, which took place 8 years after the survey of attendees to the course of the AEP, we see that the duration of the AP rotation considered necessary by residents has increased, as has the proportion of residents considering the option of PC for their future careers.
The increase in paediatrics resident rotations in PC has been contemplated in the Strategic Framework for Primary Care.12 Similarly, the AEPap has stated that [they] “propose a more flexible duration of the rotations of paediatricians-in-training so that future general paediatric practitioners can acquire necessary basic knowledge in areas such as child psychiatry, dermatology or orthopaedics, among others.” Primary care paediatricians expect that the “hospital-centric” bias in the training of medical residents specialising in a field in which professionals are needed to be in close contact with families and at a short distance from newborns, infants, children and adolescents, will be changing in upcoming years. The AEPap, along with all other paediatric scientific societies, is willing to seek solutions in collaboration with health care administrations to achieve a better fit between the training of residents and the actual career opportunities in the public health system.13
CONCLUSION
We could make the following statements to conclude:
- Paediatrics continues to be an appealing speciality for MIR candidates.
- The fact that the last paediatrics spot is filled later than in the past is influenced, in part, by the increase in the number of available spots, since adjusting for this factor the delay in the past 9 years has only been of 17%.
- If a greater number of spots were offered for paediatrics training, there could be more doctors choosing this speciality.
- Residents in paediatrics have the lowest attrition rate for any speciality, which suggests that they are satisfied with their training programme.
- The perception of residents of primary care as a future employment opportunity after specialising in paediatrics is improving, and since a majority of positions are in fact in this care setting, training in primary care should be reinforced within the MIR curriculum.
- Associations in the field of paediatrics must issue messages that are more positive about the speciality to make it appealing to future residents.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article. This work did not receive any form of funding.
AUTHORSHIP
All authors contributed equally to the development of the published article.
ABREVIATURAS
AEP: Asociación Española de Pediatría · AEPap: Asociación Española de Pediatría de Atención Primaria · MIR: medical intern-resident · PC: primary care.
REFERENCES
- Martín-Zurro A. Situación actual de la Atención Primaria y Comunitaria en España. ENE. 2022;16(3):2-3
- García Santos P. Los médicos con las mejores notas MIR ya no quieren ser pediatras: así se 'desinfla' la especialidad. In: El Español [online] [accessed 10/06/2024]. Available at www.elespanol.com/ciencia/salud/20230425/medicos-mejores-mir-no-pediatras-desinfla-especialidad/758674299_0.html
- Centro de Estudios del Sindicato Médico de Granada. Distribución adjudicaciones de plazas MIR en 2023 (9 mayo 2023) [online] [accessed 10/06/2024]. Available at https://simeg.org/wp/wp-content/uploads/2023/05/Informe-MIR-2023.pdf
- Portal Estadístico. Sistema de Información de Atención Especializada (SIAE) [online] [accessed 10/06/2024]. Available at https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/C/siae/siae/hospitales/personal-y-formacion/areas-profesionales-y-especialidades
- Portal Estadístico. Sistema de Información de Atención Primaria (SIAP) [online] [accessed 10/06/2024]. Available at https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/C/sistema-de-informacion-de-atencion-primaria-siap/profesionales/equipos-de-atencion-primaria-eap
- Necesidades de Médicos Especialistas [online] [accessed 10/06/2024]. Available at www.sanidad.gob.es/areas/profesionesSanitarias/profesiones/necesidadEspecialistas/docs/2022Estudio_Oferta_Necesidad_Especialistas_Medicos_2021_2035V3.pdf
- Uhrig A. Pediatría, una especialidad “preciosa” en la que los pacientes sacan una carcajada cada día. In: ConSalud.es; 2022 [online] [accessed 10/06/2024]. Available at www.consalud.es/especial-mir/pediatria-especialidad-preciosa-pacientes-sacan-carcajada_113168_102.html
- Maldonado G. Los primeros días de una R1 en el hospital: “Quiero aprender, crecer y convertirme en la figura del médico que idealizo”. In: iSanidad.com; 2023 [online] [accessed 10/06/2024]. Available at https://isanidad.com/250505/los-primeros-dias-de-una-r1-en-el-hospital-quiero-aprender-crecer-convertirme-figura-medico-idealizo/
- López García R. El residente de Pediatría: entusiasmo por la Atención Primaria. Rev Pediatr Aten Primaria. Supl. 2012;(21):71-6.
- González de Dios J, Polanco Allue I, Díaz Vázquez CA. De las facultades de Medicina a la residencia de Pediatría, pasando por el examen de médico interno residente: ¿algo debe cambiar? Resultados de una encuesta en residentes de Pediatría de cuarto año. An Pediatr (Barc). 2009;70(5):467-76. https://doi.org/10.1016/j.anpedi.2009.02.009
- Goez Sanz C, Álvarez Casaño M, Castillo Campos l, Gorrotxategi Gorrotxategi PJ, Villaizán Pérez C. ¿Qué opinan los residentes de Pediatría de la rotación por Atención Primaria? Rev Pediatr Aten Primaria. 2021;23:e181-e184.
- Marco Estratégico para la Atención Primaria y Comunitaria. Ministerio de Sanidad, Consumo y Bienestar Social. Madrid. 2019 [online] [accessed 10/06/2024]. Available at www.sanidad.gob.es/areas/calidadAsistencial/estrategias/atencionPrimaria/docs/Marco_Estrategico_APS_25Abril_2019.pdf
- MIR 2022: los pediatras de Atención Primaria proponen más formación en los centros de salud para aumentar la capacidad docente y sortear el déficit de profesionales [online] [accessed 10/06/2024]. Available at www.aepap.org/sites/default/files/noticia/archivos-adjuntos/np_mir_pediatria_ap.pdf





