Vol. 25 - Num. 97
Original Papers
Assessment of the maturity of the minor in the health field: the perspective of parents and pediatricians
M.ª Alba Gairí Burguésa, Montse Esquerda Aresteb, Josep Pifarré Parederoc, Eva Miquel Fernàndezd, Eduard Solé Mira
aServicio de Pediatría. Hospital Universitario Arnau de Vilanova. Lleida. Facultad de Medicina. Universidad de Lleida. Lleida. España.
bHospital Sant Joan de Deu. Terres. Lleida. Facultad de Medicina. Universidad de Lleida. Lleida. Instituto Borja de Bioética-Universidad Ramon Llull. Barcelona. España.
cHospital Sant Joan de Deu. Terres. Lleida. Facultad de Medicina. Universidad de Lleida. Instituto de Investigación Biomédica de Lleida. Lleida. España.
dInstituto Catalán de la Salud. Lleida. España.
Correspondence: M Esquerda. E-mail: mesquerda@ibb.url.edu
Reference of this article: Gairí Burgués MA, Esquerda Areste M, Pifarré Paredero J, Miquel Fernàndez E, Solé Mir E. Assessment of the maturity of the minor in the health field: the perspective of parents and pediatricians . Rev Pediatr Aten Primaria. 2023;25:13-9.
Published in Internet: 17-01-2023 - Visits: 14961
Abstract
Introduction: the model of respect for autonomy and progressive participation in the pediatric context requires that attending pediatricians be able to assess minor maturity, and the and decide the degree of participation. The objective of this study is to determine the correlation between the assessment made subjectively by paediatricians and parents, with the maturity of the minor carried out by means of an objective test, the Lleida Maturity Assessment Scale, MadurTest.
Material and methods: prospective, observational and cross-sectional study. 199 adolescents between 12 and 16 years old, affected by acute and chronic pathology. The maturity of the patients was evaluated with the MadurTest scale and pediatricians and parents assessed the maturity of the minor in the form of the Likert maturity scale.
Results: the mean of the MadurTest score is 6.39, girls present a higher level of maturity than boys in most age groups. The maturity assessment by pediatricians is 3.18 on average and by parents 3.18. No correlation is observed between the score obtained with the MadurTest and the assessment by professionals or by parents. However, a correlation is observed between the assessments made by parents and professionals (r = 0.73, p <0.00001)
Conclusions: the maturity of minors assessed subjectively by paediatricians and parents does not correlate with the maturity assessed objectively using the MadurTest.
Keywords
● Bioethics ● Capacity ● Minor mature ● Shared decision makingINTRODUCTION
In recent years, the doctor-patient relationship has undergone a profound transformation with the progressive integration of the respect to the autonomy of the individual in health care decision-making in accordance to the individual’s own beliefs and values.1,2 In the field of paediatrics, there has also been a shift in relation to minors, who have gone from being a subject of protection to a subject of rights, with the recognition of their right to be involved in the making of decisions regarding their own health.3 Several authors have emphasised that this participation should be customary and routine in health care settings and individualised according to the maturity of the minor.4,5
This issue is more complex in paediatric practice, as it requires the participation in decision-making of not only the parents, but also the children, increasingly and proportionately to their maturity, while promoting the development of autonomy.6-9
The contributions of Piaget in the field of cognitive development and of Kohlberg in the field of moral development demonstrate that moral maturity develops progressively over time as opposed to at a specific point in life.2,10-12 Most adolescents reach moral maturity allowing them to participate in decision-making between ages 12 and 15 years.13,14 Studies in developmental psychology have given rise to what is known as the “mature minor doctrine”. This doctrine entails that, from age 12 years, minors may gain certain individual rights, including the right to participate in the decision-making process and make choices on issues pertaining to their health according to their level of maturity. Laws and regulations have been developed in line with this doctrine: the age of majority is set at 18 years; from age 12 years, minors can participate in decision-making according to their level of maturity; and the medical age of majority is 16 years, except in specific cases that carry serious risk, in which parents must be informed and their opinion will be taken into account in making the final decision.3,15
This model of progressive participation requires that paediatricians or other health care providers who manage minors to be able to assess and decide whether a minor is sufficiently competent to make health care decisions or the degree to which the minor can be involved in decision-making. Decision-making competence is a multidimensional variable that depends on the moral maturity of the minor, the capacities involved in understanding and assessing the given health care situation, the type and seriousness of the decision and the context in which it must be made.16-18
Despite the changes in the conceptualization of the doctor-patient relationship and the corresponding legal framework, there is little evidence on how maturity and competence are actually assessed in clinical practice. As Hein et al. remarked,19 for decades the debate on the maturity and competence of minors in relation to medical decision-making focused primarily on regulatory and legal aspects as opposed to scientific evidence and clinical practice. Standardised instruments need to be developed to facilitate the assessment of both the level of maturity and the competence of the minor in relation to medical decision-making, and the training and knowledge of providers on the assessment of maturity and decision-making competence must also be improved.
At the Universidad de Lleida, we developed and validated a scale, called MadurTest, based on Kohlberg’s research on moral development, to assess the maturity of the minor in relation to health care.20,21. Based on the Moral Judgement Interview (MJI) developed by Kohlberg,11,12 the scale presents 9 moral dilemmas, and the answers are categorised as preconventional (immature) or conventional (mature). The analysis of the construct validity and criterion-referenced testing of the scale evinced a strong correlation with the scores obtained with the MJI and also with the level of maturity reported by teachers, rated on a Likert scale.
The aim of our study was to determine the correlation between the subjective assessment of maturity made by paediatricians and parents and the level of maturity determined by means of the MadurTest.
MATERIAL AND METHODS
We conducted a prospective cross-sectional observational and analytical study in adolescents aged 12 to 16 years with acute or chronic disease (asthma, diabetes, rehabilitation, mental health), between August 2014 and August 2018. The sample was recruited from the primary care paediatrics caseloads of the health area of Lleida (Calatonia, Spain) and the outpatient clinics of the Hospital Universitario Arnau de Vilanova of Lleida. We calculated we required a sample of a minimum of 30 patients in the acute group and 30 patients in the chronic group for a level of confidence of 95%, assuming that the standard deviation in the MadurTest is 1.7 points, which would allow the estimation of the median with an accuracy to 0.56 points in the analyses.
To assess the level of maturity of the patients, we used the Escala de Valoración de la Madurez de Lleida (Lleida Maturity Assessment Scale, EVMMLL T-9), or MadurTest.20,21 The scale is based on scenarios that present an ethical/moral dilemma. Each scenario in the test has 4 answer choices (2 mature or conventional answers and 2 immature or preconventional answers), therefore, the score can range from 0 to 9 points. The greater the number of conventional answers, the higher the level of moral maturity. In the validation of the scale,20 possible results were grouped in 2 categories: ≤5 conventional answers are interpreted as the adolescent being immature and >5 conventional answers as the adolescent being mature. The scale exhibited moderate reliability (≈0.45) with a high intraclass correlation coefficient (>0.6).
Parents and paediatricians assessed the maturity of the minors by means of a Likert scale ranging from 0 to 5 points (maturity as a discrete quantitative variable), following an explanation of the purpose and objectives of the study. In this Likert scale, a rating of 1 point indicates that the parent or professionals considers that the minor is less mature than peers of the same age, and a rating of 5 points that the adolescent is perceived as more mature than peers of the same age.
We obtained the consent of both the minors and their parents/legal guardians for their participation. The study was approved by the administration of the health care centres and the competent clinical research ethics committee.
The data analysis was performed with the software package IBM SPSS Statistics 20. To assess whether the subjective assessments performed by parents and teachers was consistent with the level of maturity determined by means of the EVMMLL T-9,19,20 we calculated the Pearson correlation coefficient for the comparison of the scores obtained by minors in the EVMMLL T-9 with the assessments of providers and parents (Likert scale).
RESULTS
We included 199 patients aged 12 to 16 years with acute and chronic disease; 128 patients had chronic diseases (asthma, diabetes, rehabilitation, mental health) and 71 had acute diseases. The mean age of the sample was 13.6 years and the standard deviation (SD) 1.22 years. Table 1 presents the distribution by age and sex of each group. The mean score in the MadurTest was 6.39, with a greater proportion of patients with mature versus immature answers, as can be seen in Table 2.
| Table 1. Characteristics of the sample, summarised as mean and standard deviation | |||||||
|---|---|---|---|---|---|---|---|
| Total patients | Acute disease (n = 71) | Chronic disease (n = 128) | |||||
| Primary care setting | Inpatient ward | Asthma | Diabetes | RHB | MH | ||
| N | 199 | 36 | 35 | 35 | 31 | 33 | 29 |
| Age | 13.6 ± 1.2 | 13.36 ± 1.31 | 13.37 ± 0.97 | 13.57 ± 1.14 | 13.45 ± 1.54 | 14.12 ± 1.24 | 13.93 ± 0.88 |
| Sex |
115 male (57.2%) 84 female (42.8%) |
14 male (38.9%) 22 female (61.1%) |
17 male (48.6%) 18 female (51.4%) |
22 male (62.8%) 23 female (37.2%) |
18 male (54.5%) 13 female (45.5%) |
22 male (66.7%) 11 female (33.3 %) |
22 male (75.8%) 7 female (24.5%) |

| Table 2. Mean age and score in the maturity test and distribution of the sample by level of maturity | ||
|---|---|---|
| Total (n = 199) | ||
| Age, mean (SD) | 13.6 (1.22) | |
| MadurTest, mean (SD) | 6.39 (1.74) | |
| Level of maturity, n (%) | Immature ≤5 | 67 (33.7%) |
| Mature >5 | 132 (66.3%) | |
| Level of maturity, n (%) | Immature ≤5 | 67 (33.7%) |
| Mature, 6-7 | 67 (33.7%) | |
| Very mature, 8-9 | 65 (32.7%) | |

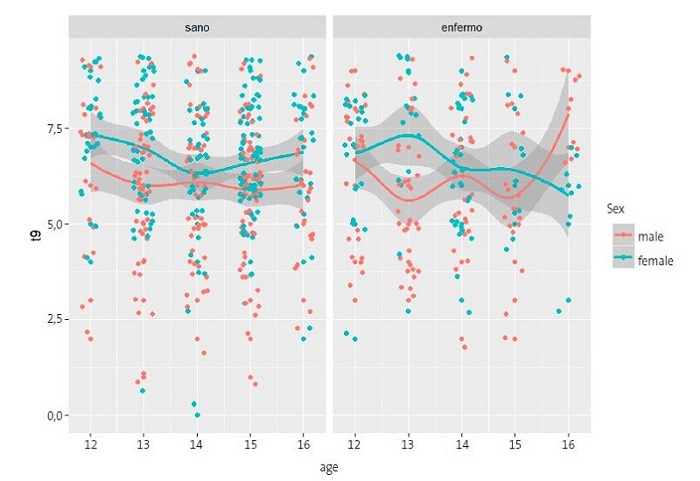
As regards the level of maturity observed in this sample based on age and sex, we found that girls were clearly more mature than boys in every age group, with the exception of boys aged 16 years, which were more mature than their female peers. We did not find an increasing trend in maturity with age, as can be seen in Figure 1.
The mean score in the paediatricians’ assessment of maturity was 3.18 de media (SD 1.21) and the mean score in the parental assessment was 3.18 (SD 1.21). We did not find a correlation between the scores obtained with the MadurTest and the assessments by providers and parents. On the other hand, there was a strong correlation between the maturity assessments of adolescents made by parents and providers (r = 0.73; p <0.00001) (Table 3).
| Table 3. Analysis of the correlation between the different maturity measures | ||
|---|---|---|
| Pearson correlation | p | |
| Adolescents vs. providers | 0.09 | 0.20 |
| Adolescents vs. parents | 0.05 | 0.45 |
| Providers vs. parents | 0.73 | <0.001 |

DISCUSSION
In our sample, minors exhibited an intermediate level of maturity, which was consistent with previous studies.21-24 As the literature demonstrates, female minors exhibit a higher level of maturity compared to male minors.20-23 One of the most salient criticisms of Kohlberg’s theory of moral development is Gilligan’s,25 who underscored the fact that girls appeared to be less mature because—according to this author—the theory of moral development relied on the principle of justice to assess maturity, as opposed to caring, which is more developed in the female sex. Different studies have evinced greater maturity in female adolescents,22,23,26-28 leading to the hypothesis that maturity develops quicker in female individuals during adolescence.
We did not find an increase in maturity with age, but rather differences between individuals in the same age group. This was already evident in the earliest studies on competence in minors. In 1982, Weithorn and Campbell29 used four hypothetical scenarios involving medical decisions in a group of children adolescents and young adults (aged 9, 14, 18 and 21 years), assessing the competence criteria proposed by Appelbaum (ability to express a choice, reasoning, appreciation and understanding of the choice). They found a significant difference between children aged 9 years and the rest of the groups, but adolescents aged 14 years made choices similar to those of the youths aged 18 and 21 years. Other studies have also not found a clear correlation between age and maturity in this age interval.11,23
The subjective assessment by paediatricians and parents also found an intermediate level of maturity, but there was no correlation to the level of maturity assessed objectively by means of the MadurTest. However, we found a strong correlation between the assessments of patients by paediatricians and of children by parents (r = 0’73; p <0.00001), as shown in Table 3.
This was in opposition to previous studies, for instance, with the study conducted to validate the scale,20,21 in which the assessment made by teachers was strongly correlated to the results of the MadurTest, in agreement with other studies conducted for other instruments.30 We think that this could be due to parents and, to a lesser extent, providers making assessments of the individual out of context, without taking into account the age group or making comparisons to a large group of minors (in particular, parents tend to compare to other siblings). In contrast, teachers or class tutors in school have large groups of students of the same age as the assessed minor and are thus exposed to a broader range of maturity levels.
The strong correlation between the assessments of paediatricians and parents could be explained by the fact that paediatricians often base their assessment of minors on parental comments and statements, without making a direct and thorough assessment of the minor.
In paediatrics, is important to pursue a model that combines a patient-centred approach, in this case, centred on the child or adolescent, promoting direct communication of providers with the paediatric patient, and a family-centred approach, in which decisions are made jointly by providers, parents and minors, emphasising their collaboration.6 In the latter approach, it is essential to give minors a voice, too, and not only to parents, and to establish channels for direct communication with the minor.
Finding the right balance in the involvement of children and adolescents in medical decision-making according to their level of maturity and actively promoting their participation is key. Having the means to assess the maturity of minors more objectively can help find this balance between the active autonomous involvement of minors and the need of parental support in decision-making. Thus, it is important to involve patients gradually and progressively in decision-making, encouraging their participation.
In a study conducted in the context of paediatric research that compared the patient-centred and family-centred approaches in the consent (parents) and assent (minors) process31 did not find differences in research participation decisions, but did find a significant difference in the knowledge of parents and older adolescents about the clinical trial when parents and adolescents were separated. The separate consent/assent process improved the knowledge of the trial and the associated risks and benefits in older adolescents and their parents, but not in younger children and their parents.
There are several barriers to an adequate assessment of decision-making competence or maturity in minors. One of them is the lack of time in medical visits, although in the primary care setting and in patients with chronic disease, the continued contact with the patient throughout time can allow monitoring of the development and maturity of the minor. The lack of knowledge about ethical and legal aspects has also been identified as another limitation. An interesting study32 evinced that the knowledge of primary care physicians of the Basic Law on the Autonomy of the Patient3 was quite poor: only 25% knew which was the medical age of majority, 34% knew that the person responsible for assessing maturity was the physician in charge of the patient and a very scant 8.5% had an in-depth understanding of the mature minor doctrine. Paradoxically, despite the deficient knowledge of ethical and regulatory foundations, 73% of surveyed physicians reported having no difficulty assessing the maturity of minors.32
Several studies have found that the participation of the minor in decision-making is associated with an increased level of satisfaction in both parents and minors with the received care, greater cooperation by the minor with treatment and a stronger sense of control, which makes the disease feel less stressful and facilitates positive adjustment.4,17,18 However, it does not seem as if this participation is sought routinely, and the biggest challenge is to ensure an adequate attitude toward this issue in health care professionals.33
CONCLUSION
The introduction of objective tests (such as the MadurTest) or standardised protocols can facilitate this task, but in any case it is essential to involve minors in decision-making, together with their parents and (whenever possible) individually, not only out of respect for the autonomy of the minor, but also to promote and foster its development.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
REFERENCES
- Beauchamp TL, Childress JF. Principles of Biomedical ethics. New York: Oxford University Press; 2013.
- Piaget J. IB. The psychology of the child. New York: Basic books; 1969.
- Ley Básica 41/2002, de 14 de noviembre, básica reguladora de la autonomía del paciente y de derechos y obligaciones en materia de información y documentación clínica [online] [accessed 16/01/2023]. Available at www.boe.es/buscar/act.php?id=BOE-A-2002-22188
- Olszewski AE, Goldkind SF.The default position: Optimizing pediatric participation in medical decision making. Am J Bioeth. 2018;18:4-9.
- Sabatello M, Janvier A, Verhagen E, Morrison W, Lantos J. Pediatric Participation in Medical Decision Making: Optimized or Personalized? Am J Bioeth. 2018;18:1-3.
- Scherer DG. Pediatric participation in medical decision making: The devil is in the details. Am J Bioeth. 2018;18:16-8.
- Fuertes Rodrigo C, Pérez Álvarez C, Babiano Castellano B, Galbe Sánchez Ventura J. Consentimiento informado: algo más que una firma. Rev Pediatr Aten Primaria. 2012;14:331-4.
- Esquerda M, Pifarre J, Gabaldón S. Evaluación de la competencia para tomar decisiones sobre su propia salud en pacientes menores de edad. FMC Form Medica Contin. 2009;16:547-53.
- Tejedor Torres JC, Crespo Hervas D, Niño Ráez E. Consentimiento y confidencialidad en medicina del niño y adolescente. Med Clin (Barc). 1998;111:105-11.
- Barrouillet P. Theories of cognitive development: From Piaget to today. Dev Rev. 2015;38:1-12.
- Kohlberg l. Psicología del desarrollo moral. Bilbao: Desclée de Brouwer; 1992.
- Kohlberg l. The philosophy of moral development: moral stages and the idea of justice. San Francisco: Harper & Row; 1981.
- Ogando Díaz B, García Pérez C. Consentimiento informado y capacidad para decidir del menor maduro. Pediatr Integral. 2007;10:877-83.
- Hein IM, De Vries MC, Troost PW, Meynen G, Van Goudoever JB, Lindauer RJL. Informed consent instead of assent is appropriate in children from the age of twelve: Policy implications of new findings on children’s competence to consent to clinical research. BMC Med Ethics. 2015;16(1):76.
- Ley 26/2015, de 28 de julio, de modificación del sistema de protección a la infancia y a la adolescencia [online] [accessed 16/01/2023]. Available at www.boe.es/buscar/act.php?id=BOE-A-2015-8470
- Grootens-Wiegers P, Hein I, van den Broek J, de Vries M. Medical decision-making in children and adolescents: developmental and neuroscientific aspects. BMC Pediatr. 2017;17:1-10.
- Esquerda M, Pifarre J, Viñas J. El menor maduro: madurez cognitiva, psicosocial y autonomía moral. In: Bioética y Pediatría. Sociedad de Pediatría de Madrid y Castilla-La Mancha, eds.; 2010. p. 367-73.
- Esquerda M, Pifarre J, Miquel E. La capacidad de decisión en el menor. Aspectos particulares de la información en el niño y en el joven. An Pediatr Contin. 2013;11:204-11.
- Hein I, Troost P, Broersma A, De Vries M, Daams J, Lindauer R. Why is it hard to make progress in assessing children’s decision-making competence? BMC Med Ethics. 2015;16:1-6.
- Espejo M, Miquel E, Esquerda M, Pifarré J. Valoración de la competencia del menor en relación con la toma de decisiones sanitarias: escala de la competencia de Lleida. Med Clin (Barc). 2011;136:26-30.
- Miquel E, Esquerda M, Real J, Espejo M, Pifarré J. Design and Validation of an Instrument To Measure a Minor’s Maturity When Faced with Health Decisions. J Bioeth Inq. 2019;16:431-441.
- Romo Martínez JM. Juicio moral en estudiantes. Un diagnóstico. Rev Iberoame Educa. 2004. ISSN: 1681-5653.
- Barba B. Razonamiento moral de principios en estudiantes de secundaria y bachillerato. Rev Mexi Investi Educ. 2001;6:501-23.
- Pérez Delgado E, García Ros R. La psicología del desarrollo moral. Madrid: Siglo XXI; 1991.
- Gilligan C. In a different voice: Psychological theory and women's development. Cambridge, MA: Harvard University Press; 1982.
- Cesur S, Topçu MS. A reliability and validity study of the Defining Issues Test: the relationship of age, education, gender and parental education with moral development. Educ Sci: Theory Pract. 2010;10:1681-96.
- Garmon LC, Basinger KS, Gregg VR, Gibbs JC. Gender differences in stage and expression of moral judgment. Merrill-Palmer Q. 1996;42:418-37.
- Gibbs JC, Arnold KD, Burkhart JE. Sex differences in the expression of moral judgment. Child Dev. 1984;55:1040-3.
- Weithorn LA, Campbell SB. The competency of children and adolescents to make informed treatment decisions. Child Dev. 1982;53:1589-98.
- Park N, Peterson C. Moral competence and character strengths among adolescents: The development and validation of the Values in Action Inventory of Strengths for Youth. J Adolesc. 2006;29:891-909.
- Annet R, Brody J, Scherer D, Turner CW, Dalen J, Raissy H. A randomized study of a method for optimizing adolescent assent to biomedical research. AJOB Empir. Bioeth. 2017;8:189-97.
- Sánchez Jacob M, Riaño Galán I, Martínez González C. Evaluación de los conocimientos legales y éticos de los profesionales sanitarios en relación con el adolescente. Rev Ped Aten Primaria. 2008;39:59-72.
- Coad JE, Shaw KL. Is children's choice in health care rhetoric or reality? A scoping review. J Adv Nurs. 2008;64:318-327.