Vol. 24 - Num. 95
Original Papers
Knowledge and opinion on integrated care for children with cerebral palsy in Primary Care
Lidia Aguilera Nietoa, M.ª José Peláez Canterob, Daniel Hinojosa Nogueirac, Josep Vicent Balaguer Martínezd
aPediatra. CS Palma-Palmilla. Málaga. España.
bPediatra. Unidad de Crónicos Complejos y Cuidados Paliativos Pediátricos. Hospital Regional Universitario de Málaga. Málaga. España.
cDepartamento de Nutrición y Bromatología. Instituto de Nutrición y Tecnología de los Alimentos. Centro de Investigación Biomédica. Universidad de Granada. Granada. España.
dPediatra. CAP Sant Ildefons. Cornellà de Llobregat. Barcelona. España.
Correspondence: L Aguilera . E-mail: lidia.agnil@hotmail.com
Reference of this article: Aguilera Nieto L, Peláez Cantero MJ, Hinojosa Nogueira D, Balaguer Martínez JV. Knowledge and opinion on integrated care for children with cerebral palsy in Primary Care . Rev Pediatr Aten Primaria. 2022;24:261-71.
Published in Internet: 11-10-2022 - Visits: 10001
Abstract
Objective: patients with cerebral palsy (CP) require multiple treatments and services. The primary objective of the study was to describe the opinion, perception and knowledge of primary care (PC) paediatricians about the comprehensive approach to the care of children with CP and their current management of this condition.
Material and methods: cross-sectional, descriptive and nationwide study carried out through an online survey of paediatricians and family physicians dedicated to paediatric care and practicing in the PC level in January and February 2021.
Results: we received a total of 335 responses. Ninety-one percent of respondents thought they had insufficient training and limited knowledge, and 65% did not considered themselves adequately qualified to manage children with CP. In addition, 97.3% believed that training on CP is necessary and 99% that specific protocols need to be developed. Of all respondents, 57.2% would like to be the care coordinator working in collaboration with hospital paediatricians. Last of all, 75% believed that the caregivers were not satisfied with the care received, and that the provision of comprehensive care to children with CP from PC or the availability of specific units for their management would improve family satisfaction, a result that was statistically significant.
Conclusions: most paediatricians do not feel qualified for the management of children with CP from PC and consider that training and the development of specific guidelines are necessary. Professionals believe that an integrated, comprehensive approach to the care of these patients would improve the quality of life of families, and advocated for hybrid care coordination models.
Keywords
● Cerebral Palsy ● Primary health careINTRODUCTION
Cerebral palsy (CP) is the most common cause of disability in children. Its overall prevalence is estimated at 2.11 per 1000 live births,1 and it is higher in newborns with birth weight under 1500 g (59.2 per 1000 live births) and those born preterm before 28 weeks’ gestation (111.8 per 1000 live births).1,2 Among the causes of CP, there are many factors that can cause brain lesions (including consumption of toxins during pregnancy, congenital infection or hypoxia), although in 80% of cases the cause is unknown.3
This condition encompasses a group of permanent, but not unchanging, disorders of movement and posture, causing activity limitation, resulting from non-progressive lesions that occurred in the immature central nervous system of the foetus or infant.4 These impairments are often accompanied by other comorbidities, such as chronic musculoskeletal pain, sleep disorders, epilepsy and disturbances of sensation (visual, auditory) and behaviour, among others, that substantially impact the quality of life and prognosis of these children.5-7 This makes it a very heterogeneous condition requiring a multidisciplinary approach.
In recent decades, the role of parents as principal caregivers has increasingly been taken into account in the management of patients with CP. However, they are still dissatisfied with the care their children receive.8 These children, due to their fragility and multiple comorbidities, require multiple forms of care and treatment, consuming large amounts of resources and time; this impacts both the physical and the mental health of the caregiver, who is consequently exhausted.9,10 The caregiver’s distress arises especially from lack of coordination in the care these patients require11 and is associated primarily with organisational aspects of care delivery rather than with specific interventions.12 In this connection, a key step would be to create the figure of the “coordinating paediatrician” for paediatric CP patients, to manage their integrated care and facilitate coordination between primary care (PC) and hospital-based care, which would significantly improve the quality of life of the patient and the family.8,13 The PC paediatrician plays an essential role in the followup of children with CP, and given their greater accessibility and closeness to the family, they could be considered the ideal figure to organise the comprehensive management we are discussing. In order to do so, they must be familiar with the associated comorbidities so as to prevent them, and, if they are diagnosed, know when to refer the patients and what treatment options are available. However, there are practically no protocols on the followup of children with CP at the PC level.
In 2017, the NICE guidelines on the assessment and management of cerebral palsy in patients under 25 years were published,14 and the autonomous community of Castilla y León (Spain) produceda guideline, the “Guía para el seguimiento de la parálisis cerebral en Atención Primaria” (Guideline for the followup of cerebral palsy in primary care)15, to address many of the issues mentioned above, such as early screening and the detection of the most frequent comorbidities.
Recently, the study “Comprehensive approach to children with cerebral palsy”, a proposal for monitoring and referral to specialists of children with CP of mild to moderate severity, has been published.16 It would therefore be desirable to develop and disseminate generalised protocols encompassing all the interventions to be carried out and the criteria for referral to different specialists.
These questions lead us to consider whether PC paediatricians are really the ideal figures to coordinate the multidisciplinary management of children with CP, whether they are equipped and feel qualified to do so and how they perceive their current management of these patients. The purpose of this study is to assess all these issues.
MATERIALS AND METHODS
Study design
We conducted a nationwide, cross-sectional descriptive study from January to February 2021.
Study population
The study population was made up of paediatricians and family physicians dedicated to paediatric care working in PC in Spain. According to the Ministry of Health’s statistical website, there were 6502 posts in PC paediatrics in Spain in 2019.17 The inclusion criteria were specialists in paediatrics or family medicine working in PC in the field of paediatrics. We excluded internal medicine residents and paediatric specialists employed outside the PC setting.
Sample size
We estimated a minimum sample size of 364 responses was necessary to obtain a representative sample. The sample size was calculated for a margin of error of 0.05 and a level of confidence of 95%, assuming the largest possible variability (50%).18
Data-collection method
A questionnaire for data collection was developed and pilot-tested on paediatricians before the study. The questionnaire was completed on an anonymous and voluntary basis, with a single response accepted per respondent; it was distributed via the Google Drive platform through the mailing list of the Research Group of the Spanish Association of Primary Care Paediatrics (AEPap) and PEDIAP in a message that informed the professionals about the study and invited them to participate.
The questionnaire included items on socio-demographic characteristics, the clinical management of paediatric patients with CP and perceptions about the current ability to provide care for these patients, the figure of the coordinating doctor and the need for training (Table 1).
| Table 1. Questionnaire |
|---|
| Sociodemographic characteristics |
| 1. Job title |
| 2. Age |
| 3. Sex |
| 4. Experience in paediatrics (hospital vs out-of-hospital setting) |
| 5. Have you ever worked as a paediatrician in a unit specialising in patients with cerebral palsy? |
| 6. Province/city where you work |
| 7. Work setting (rural, semi-urban, urban) |
| 8. Do you have any patients with cerebral palsy in your paediatric quota? |
| 9. Is there a specialised unit for the integrated management of children with cerebral palsy in your catchment area?/td> |
| 10. Who is the coordinating paediatrician for children with cerebral palsy in your catchment area? |
| Managing patients with cerebral palsy from the primary care level |
| 11. Do you refer patients with cerebral palsy to early intervention? |
| 12. Do you refer patients with cerebral palsy to rehabilitation? |
| 13. Children with cerebral palsy have a significant risk of dysphagia. What do you do to detect it? |
| 14. Do you routinely perform a nutritional assessment with anthropometric measurements on children with cerebral palsy in your PC practice? |
| 15. Do you perform a blood test for nutritional assessment on children with cerebral palsy? |
| 16. Children with cerebral palsy have a higher risk of low bone mineral density and osteoporosis. What do you do to detect it? |
| 17. Do you refer patients with cerebral palsy to ophthalmology? |
| 18. Do you refer patients with cerebral palsy to dentistry? |
| Opinion on current management of cerebral palsy patients |
| 19. Do you consider that you have sufficient training to manage children with cerebral palsy? |
| 20. Do you think that your current knowledge on the management of cerebral palsy is limited? |
| 21. Have you received specific training courses on this condition? |
| 22. Do you think specific training on this condition is necessary? |
| 23. Is there a specific protocol on patients with cerebral palsy in your autonomous community? |
| 24. Do you consider a specific protocol on the followup and referral of children with cerebral palsy is needed in your catchment area? |
| 25. Would you like to be the coordinating paediatrician for CP, working jointly with the different hospital-based specialists? |
| 26. Who do you consider should be the coordinating physician for children with cerebral palsy in your catchment area? |
| 27. Do you consider yourself qualified to be the coordinating physician for your patients with cerebral palsy? |
| 28. Do you consider that the families of your patients with cerebral palsy are satisfied with the coordination of the care they receive? |
| 29. Do you consider that it would improve the quality of life of your patients with cerebral palsy and their families if you were the coordinating physician? |
| 30. Do you consider that multidisciplinary care units need to be established in the hospital setting to followup patients with cerebral palsy? |

Statistical analysis
We performed a descriptive analysis of the sample by calculating percentages and assessing the distribution of the responses obtained in the different autonomous communities of Spain.
We calculated the overall response rate for each item in the questionnaire. Then, we analysed the responses by age group, based on whether the paediatrician acted as the care coordinator for CP patients and whether the health care area where the paediatrician was employed had a specific paediatric CP unit. The differences between groups were assessed by means of the χ2 test. Differences were considered significant when the p value was less than 0.05. The calculations were performed with the SPSS software, version 23.0.
Ethical issues
Given that the study did not include patient data and the completion of the questionnaires was anonymous and voluntary, we considered the study exempt from the need of approval by an ethics committee.
RESULTS
Characteristics of the sample
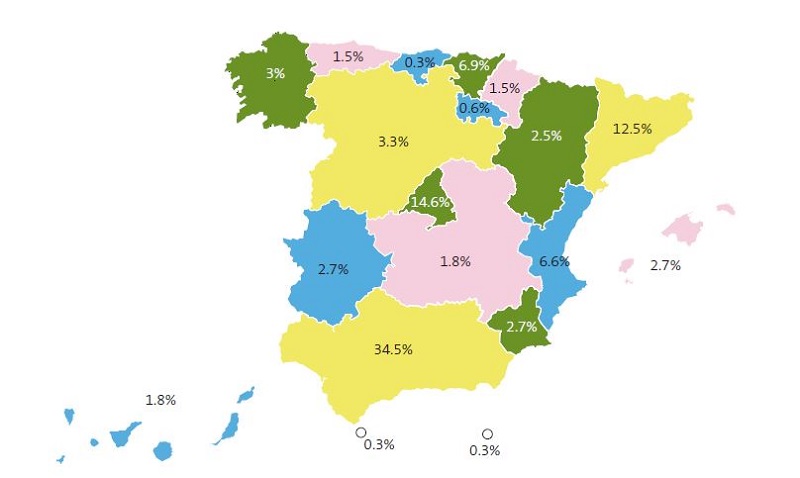
A total of 335 responses were received. Of these, 93.7% were from paediatricians and 6.3% from family physicians. The proportion of women was 84.5% and the majority age group was 50 to 59 years (41.50%). As for professional experience, most had more than 20 years (54.3%). In all, 76.4% worked in an urban area. Figure 1 presents the distribution of submitted responses by autonomous community.
As regards experience with patients suffering from CP, 96.7% of respondents had not previously worked in units specialising in patients with cerebral palsy. However, as many as 78.5% had one or more children with CP in their caseloads.
Concerning the organization of care for paediatric patients with CP, 58.2% reported that there was no specialised unit to deliver integrated care to children with CP in their health care area, 22.1% that these units did exist, and 19.7% did not know. As regards the figure of the coordinating paediatrician for these patients, 43.6% of respondents stated there was no established care coordinator, 31.9% that it was a hospital-based paediatrician and in 9% that it was a PC paediatrician. Finally, 15.5% did not know who acted as the coordinating physician.
General responses to the questionnaire
Eight items in the questionnaire asked about the management of paediatric patients with CP at the PC level (Table 2).
| Table 2. Percentage distribution of responses regarding the management of patients with childhood CP | |
|---|---|
| Referral to early intervention | |
| Yes, whenever suspected, even if the patient has not been assessed by paediatric neurology | 66.9% |
| Yes, but only at the suggestion of paediatric neurology | 1.8% |
| It depends on the patient (sometimes referred to early intervention and sometimes to paediatric neurology) | 25.1% |
| No, patients are referred by paediatric neurology | 6.2% |
| Referral to rehabilitation | |
| Yes, after diagnosis | 52.2% |
| Yes, if there are joint deformities | 4.8% |
| No, referrals are made by the hospital paediatrician | 43% |
| Referral to ophthalmology | |
| Yes, always | 21.3% |
| Yes, if there are signs of pathology (nystagmus, lack of visual attention, etc.) | 29.2% |
| No, referrals are made by the hospital paediatrician | 49.5% |
| Referral to dentistry | |
| Yes, always | 35.2% |
| Yes, if there are signs of pathology | 42.4% |
| No, referrals are made by the hospital paediatrician | 22.4% |
| Detection of dysphagia and referral to gastroenterology | |
| Always refers patients to gastroenterology | 5.8% |
| Periodically asks the family about the presence of signs of dysphagia and refers patients if they have symptoms | 50.4% |
| Does not usually ask the family. Only refers the patient to gastroenterology if the family reports symptoms | 30.7% |
| Does not ask or refer. Referrals are made by the hospital paediatrician | 13.1% |
| Routine nutritional assessment with anthropometric measurements | |
| Yes, periodically | 37% |
| No, it is performed by gastroenterology or a hospital paediatrician | 63% |
| Nutritional assessment with blood tests | |
| Yes, routinely, every 6 months | 1.5% |
| Yes, every year | 3.2% |
| Yes, when the there are signs of inadequate weight gain | 28.1% |
| No, they are performed by the hospital paediatrician | 67.2% |
| Detection of low bone mineral density and osteoporosis and referral to rheumatology | |
| Refers all children to rheumatology | 1.2% |
| Would request a densitometry test, if possible, in children with high fracture risk (previous fractures, reduced mobility) | 26.2% |
| Would request a densitometry test, if possible, for all children before referral to rheumatology | 8.1% |
| Only refers patients if bone fractures are suspected | 6% |
| Does not refer patients. Referrals are made by the hospital paediatrician | 58.5% |

Finally, respondents were asked about their opinions and perceptions regarding the current management of children with CP.
Most respondents considered that they did not have sufficient training to care for children with CP (91.1%) and that their knowledge is too limited for them to manage these patients (94.6%). Almost all were of the opinion that specific training on CP is needed (97.3%) and only 10.1% had received courses on it. Of the minority that had received some kind of training, 94% were paediatricians who had at least one patient with CP in their caseload, a result that was statistically significant.
We inquired about the need for a specific protocol for the followup and referral of children with CP from the PC level; practically all respondents confirmed that need (99.1%). We asked whether specific protocols for managing these patients existed in the corresponding autonomous community; 10.2% did know them, but most did not (62.8%) or stated that they did not exist (27%). Despite the fact that Castilla y León is the only community in which there is known to be a protocol, only 2 of the respondents (18%) from that community were aware of its existence.
With regard to the coordination of the care of patients with CP, the majority (78.2%) advocated a hybrid coordination model (hospital paediatrician and PC paediatrician), 14.9% considered that the PC paediatrician should fulfil this role and the other 6.9% that it should be fulfilled by the hospital paediatrician. More than half (57.2%) replied that they would like to be the coordinating paediatrician, working in collaboration with hospital specialists, and 60.9% considered that the quality of life of children with CP and their families would improve if this were so. However, 65.1% thought that they were not qualified to perform the role of coordinating physician and 75% considered that families were not satisfied with the care currently received.
The last question raised the issue of whether they considered it necessary to establish multidisciplinary care units in the hospital setting for the followup of paediatric patients with CP. Most respondents answered in the affirmative (97.3%).
Responses by age group
The responses were analysed with respect to opinions and perceptions on the management of children with CP, classifying the sample by age into those aged under 50 (n = 144; 42.3%) and those over 50 (n = 191, 57%). We observed that younger paediatricians would like to be coordinating physicians for CP patients and also thought that this would improve the patients’ quality of life, a statistically significant result. The differences between the two age groups can be seen in Table 3.
| Table 3. Odds ratios of affirmative responses in younger versus older paediatricians | |
|---|---|
| OR (95% CI) younger/older paediatricians | |
| Do you consider that you have sufficient training to manage children with cerebral palsy? | 0.76 (0.33-1.72) |
| Do you think that your current knowledge of managing childhood cerebral palsy is limited? | 0.56 (0.22-1.54) |
| ¿Have you received specific training courses on this condition? | 1.05 (0.51-2.15) |
| Do you think specific training on this condition is necessary? | 6.25 (0.77-3.15) |
| Do you consider a specific protocol on the followup and referral of children with cerebral palsy is needed in your catchment area? | 0.37 (0.03-4.1) |
| Would you like to be the coordinating paediatrician for cerebral palsy, working jointly with the different hospital specialists? | 1.98 (1.27-3.01) |
| Do you consider yourself qualified to be the coordinating physician for your patients with cerebral palsy? | 1.03 (0.66-1.63) |
| Do you consider that the families of your patients with cerebral palsy are satisfied with the coordination of the care they receive? | 1.02 (0.61-1.68) |
| Do you consider that it would improve the quality of life of your patients with cerebral palsy and their families if you were the coordinating physician? | 2,1 (1.34-3.35) |
| Do you consider that multidisciplinary care units need to be established in the hospital setting to followup patients with cerebral palsy? | 2.71 (0.55-1.32) |

Responses of paediatricians who act as coordinating doctors for patients with childhood CP
We used the χ2 test to compare the opinions of paediatricians who coordinated the care of CP patients from the PC level and those who did not (Fig. 2). We found that 86.6% of paediatricians who acted as coordinating physicians liked doing so and that 46.6% considered that families were satisfied with their work, compared to 54.5% and 22.2% of non-coordinating paediatricians, respectively. These differences were statistically significant.
| Figure 2. Percentages of affirmative responses from paediatricians who act as coordinating physicians of childhood CP patients from PC versus paediatricians who do not |
|---|
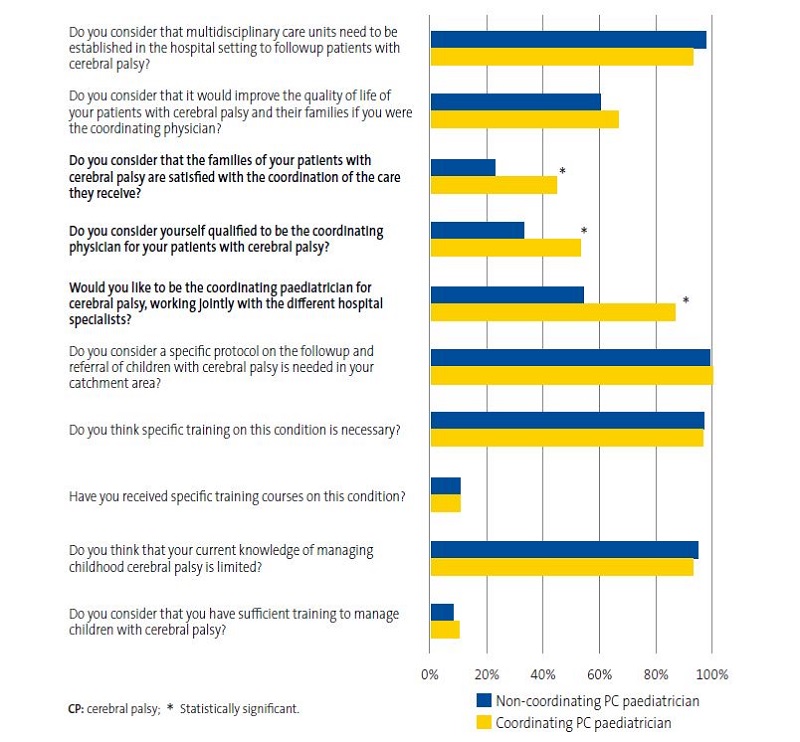 |

Responses of paediatricians who have specific childhood CP management units in their catchment area
We also applied the χ2 test to compare the opinions of professionals working in areas where there are specific clinics for the management of children with CP and those working in areas without such services (Fig. 3). Among the results, we found that 47.2% of PC professionals that reported the availability of specific services in their catchment area stated that they would like to perform the role of coordinating physician and 37.8% that they considered that families were satisfied, compared to 60.15% and 21.07% of paediatricians without these services in their area, differences that were statistically significant.
| Figure 3. Percentages of affirmative responses from paediatricians who have specific units for patients with childhood CP in their working area vs paediatricians without specific units |
|---|
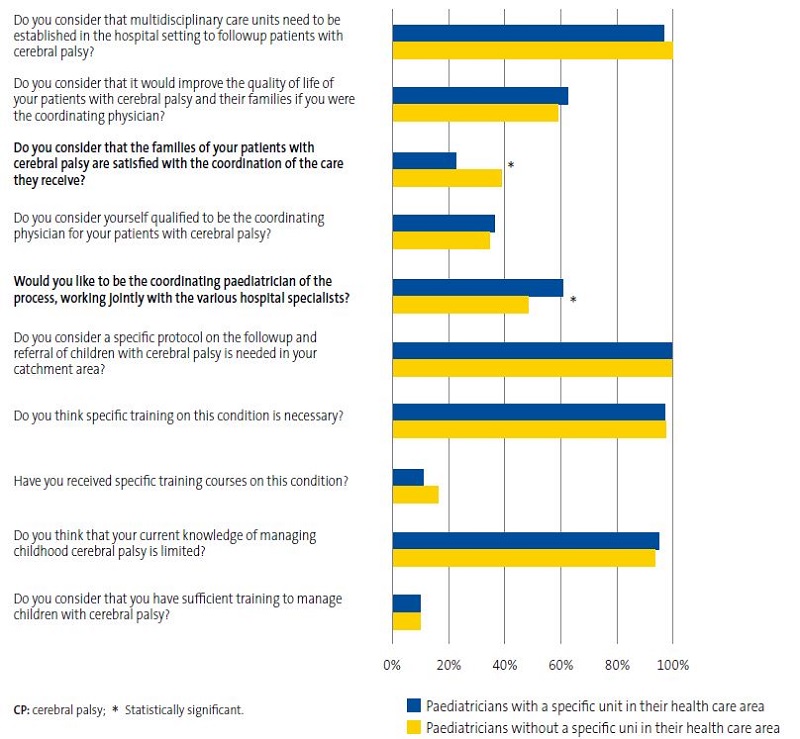 |

DISCUSSION
The great majority of respondents considered that their knowledge and training for managing patients with childhood CP were insufficient. Although more than half have at least one such patient in their caseloads, only one in ten has received training on the subject. Similarly, around 90% did not know whether there were specific protocols in their region for the followup of children with CP at the PC level. In the case of Castilla y León, the only autonomous community that has a guideline for the management of paediatric patients with CP in PC,15 only 18% of the paediatricians who responded to the questionnaire were aware of it. Bearing this in mind, practically the entire sample claimed that training and the development of protocols to guide management were essential.
The coordination of comprehensive care for paediatric patients is another point of concern. OF all respondents, 59.9% stated that there was no coordinating physician or they did not know who performed that function. Only 9% of respondents served as the care coordinator from PC. It is striking that despite these results, more than 50% of the paediatricians would like to oversee the comprehensive care of children with CP, advocating a hybrid coordination model. However, only a third felt qualified to do so. It is probably therefore a problem of aptitude rather than attitude. The satisfaction of families with the care their sick children receive is another issue worth highlighting. Only a quarter of the paediatricians considered that caregivers were satisfied, although this perception varied according to the resources that the healthcare system could offer. Accordingly, a higher proportion of professionals who provided comprehensive care to children with CP, or had access to specific units that could, considered that the families were satisfied compared to those who could not offer these services. This difference was statistically significant.
To date, there are few publications in Spain that address the management of children with CP, especially in the PC setting, apart from the above-mentioned guidelines in Castilla y León15 and the recently proposed Comprehensive approach to children with cerebral palsy.16 Nor has anything been published on paediatricians’ perception of and opinion on this subject. There is a national consensus document on the management of children with palliative care needs, who could include some children with CP. This document proposes a model of comprehensive care that takes the child’s physical, psychological, spiritual and social dimensions into consideration, based primarily in the home.19
At present, the organization of the care of children with CP in Spain is heterogeneous. Some, but not all, hospitals have specific units devoted to the care of chronic/complex patients, but not all children with CP have access to them.20 In this regard, it is essential to centralise care where the patient lives, as Dewan and Cohen suggest.21 According to the current evidence, more than half the families of complex patients are not satisfied with the healthcare resources available to them.11,22 They perceive that the family is ultimately made to assume full responsibility for coordinating the child’s care, which entails significant emotional strain and financial problems.12,23 If this comprehensive approach to paediatric patients with CP were undertaken from PC, perhaps these inequalities could be mitigated. In this way, not only would sick children be guaranteed easy access to coordinated care, but the family could be rid of its role as “coordinator” and devote itself exclusively to care at home, probably improving the quality of life of the child and the family.
This study has a series of limitations. On the one hand, it must be pointed out that although we did not reach the number of questionnaires we had hoped for (364), we did receive 335 responses, so precision was not affected since it was very close to the desired number. The final margin of error of the study with the sample obtained was 5.21%.24 On the other hand, the uneven representation of the different regions must be taken into account. However, given that all autonomous communities were represented in the sample of responses that PC operates similarly throughout Spain, it is unlikely that there are great differences between them.
Despite the limitations mentioned, it should be noted that the results, on aspects that have not been studied previously, are very uniform and all point in the same direction: the need to train PC paediatricians, organise clinics or care teams that allow coordinated care delivery for paediatric patients with CP, and the development of protocols that involve the participation of PC professionals in addition to their adequate dissemination, to ensure that all professionals are aware of their existence. This could be a starting point for creating new organisational models in which PC paediatricians, as doctors who are trusted and are more accessible to the families, would take charge of the comprehensive management of children with CP, having been trained, and with the collaboration of specialist paediatricians. It would be interesting to study the perception of families according to the care they currently receive and assess changes in that perception, as well as the changes in the opinions of paediatricians, if this were put into practice.
CONCLUSION
In conclusion, this study provides relevant information on the opinions and perceptions of paediatricians regarding the comprehensive approach to paediatric patients with CP. Most believe that a comprehensive approach is essential in the management of children with CP, and that PC paediatricians should be involved in it. They are aware that caregivers are overwhelmed and dissatisfied and that their complex care needs are not being met. However, practically all the paediatricians surveyed recognised that they were not qualified and did not have sufficient knowledge to coordinate the management of these patients. They also considered it necessary to create protocols and provide training courses for PC paediatricians, in addition to working jointly with hospitals to address all the needs of children with CP.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
CP: cerebral palsy · PC: primary care.
REFERENCES
- Oskoui M, Coutinho F, Dykeman J, Jetté N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55:509-19.
- Hafström M, Källén K, Serenius F, Maršál K, Rehn E, Drake H, et al. Cerebral Palsy in Extremely Preterm Infants. Pediatrics. 2018;141:e20171433.
- Marret S, Vanhulle C, Laquerriere A. Pathophysiology of cerebral palsy. Handbook Clin Neurol. 2013;111:169-76.
- Rosenbaum P, Paneth N, Leviton A, Goldstein M. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol. 2007;49:8-14.
- Smithers-Sheedy H, McIntyre S, Gibson C, Meehan E, Scott H, Goldsmith S, et al. A special supplement: findings from the Australian Cerebral Palsy Register, birth years 1993 to 2006. Dev Med Child Neurol. 2016;58:5-10.
- Palisano RJ, Hanna SE, Rosenbaum PL, Russell DJ, Walter SD, Wood EP, et al. Validation of a Model of Gross Motor Function for Children With Cerebral Palsy. Phys Ther. 2000;80:974-85.
- Novak I, Hines M, Goldsmith S, Barclay R. Clinical Prognostic Messages From a Systematic Review on Cerebral Palsy. Pediatrics. 2012;130:e1285-312.
- Martínez de Zabarate JM, Ros I, Peña JL, García R, Rodríguez G. Carga del cuidador del paciente con parálisis cerebral moderada-grave: ¿influye el estado nutricional? An Pediatr (Barc). 2021;94:311-7.
- Byrne MB, Hurley DA, Daly l, Cunningham CG. Health status of caregivers of children with cerebral palsy: Caregiver health in CP. Child Care Health Dev. 2010;36:696-702.
- Tseng M-H, Chen K-l, Shieh J-Y, Lu l, Huang C-Y, Simeonsson RJ. Child characteristics, caregiver characteristics, and environmental factors affecting the quality of life of caregivers of children with cerebral palsy. Disability and Rehabilitation. 2016;38:2374-82.
- Liptak GS, Orlando M, Yingling JT, Theurer-Kaufman KL, Malay DP, Tompkins LA, et al. Satisfaction With Primary Health Care Received by Families of Children With Developmental Disabilities. J Pediatr Health Care. 2006;20:245-52.
- Hayles E, Jones A, Harvey D, Plummer D, Ruston S. Delivering healthcare services to children with cerebral palsy and their families: a narrative review. Health Soc Care Community. 2015;23:242-51.
- Schwabe AL. Comprehensive Care in Cerebral Palsy. Phys Med Rehabil Clin N Am. 2020;31:1-13.
- Shaunak M, Kelly VB. Cerebral palsy in under 25s: assessment and management, 2017. In: NICE Guideline [online] [accessed 13/09/2022]. Available at www.nice.org.uk/guidance/ng62
- Guía para el seguimiento de la parálisis cerebral en Atención Primaria. In: Portal de Salud de la Junta de Castilla y León, Consejería de Sanidad, 2017 [online] [accessed 13/09/2022]. Available at www.saludcastillayleon.es/institucion/es/biblioteca/materiales-consejeria-sanidad/buscador/guia-seguimiento-ninos-paralisis-cerebral-atencion-primaria
- Peláez Cantero MJ, Moreno Medinilla EE, Cordón Martínez A, Gallego Gutiérrez S. Abordaje integral del niño con parálisis cerebral. An Pediatr (Barc). 2021;95:276.e1-276.e11.
- Recursos, población asignada y actividad. Ministerio de Sanidad, Consumo y Bienestar Social. In: Portal Estadístico del SNS-Portal Estadístico del SNS, 2019 [online] [accessed 13/09/2022]. Available at www.mscbs.gob.es/estadEstudios/estadisticas/docs/siap/Resumen_grafico_2019.pdf
- Sample Size Calculator. QuestionPro [online] [accessed 13/09/2022]. Available at https://www.questionpro.com/es/calculadora-de-muestra.html
- Cuidados Paliativos Pediátricos en Sistema Nacional de Salud: Criterios de Atención. Ministerio de Sanidad, Servicios Sociales e Igualdad, 2014 [online] [accessed 13/09/2022]. Available at https://www.sanidad.gob.es/ca/organizacion/sns/planCalidadSNS/pdf/01-Cuidados_Paliativos_Pediatricos_SNS.pdf
- Gimeno Sánchez I, Muñoz Hiraldo ME, Martino Alba RJ, Moreno Villares JM. Atención específica para los niños con complejidad médica en España: buscando el mejor modelo. An Pediatr (Barc). 2016;85:56-7.
- Dewan T, Cohen E. Children with medical complexity in Canada. Paediatr Child Health. 2013;18:518-22.
- Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130:e1463-70.
- Brehaut JC, Garner RE, Miller AR, Lach LM, Klassen AF, Rosenbaum PL, et al. Changes over time in the health of caregivers of children with health problems: growth-curve findings from a 10-year Canadian population-based study. Am J Public Health. 2011;101:2308-16.
- Margin of Error Calculator. QuestionPro [online] [accessed 13/09/2022]. Available at https://www.questionpro.com/es/calculadora-de-margen-de-error.html