Vol. 24 - Num. 95
Original Papers
Determinants of preterm birth in Galicia
Andrea Vila Farinasa, Nerea Mourino Castrob, Leonor Varela Lemac, M.ª Isolina Santiago Pérezd, Alberto Malvar Pintosd, Julia Rey Brandarize, Cristina Candal Pedreirae, Mónica Pérez Ríosf
a Área de Medicina Preventiva y Salud Pública. Universidad de Santiago de Compostela. Santiago de Compostela. A Coruña. España.
bÁrea de Medicina preventiva y Salud Pública. Universidad de Santiago de Compostela. Santiago de Compostela. A Coruña. España.
cÁrea de Medicina Preventiva y Salud Pública. Universidad de Santiago de Compostela. Santiago de Compostela. A Coruña. España.
dServicio de Epidemiología. Dirección Xeral de Saúde Pública. Consellería de Sanidade. Xunta de Galicia. Santiago de Compostela. A Coruña. España.
eÁrea de Medicina preventiva y Salud Pública. Universidad de Santiago de Compostela. Santiago de Compostela. A Coruña. España.
fÁrea de Medicina preventiva y Salud Pública. Universidad de Santiago de Compostela. Ciber de Epidemiología y Salud Pública. CIBEResp. A Coruña. España.
Correspondence: L Varela. E-mail: leonor.varela@usc.es
Reference of this article: Vila Farinas A, Mourino Castro N, Varela Lema L, Santiago Pérez MI, Malvar Pintos A, Rey Brandariz J, et al. Determinants of preterm birth in Galicia . Rev Pediatr Aten Primaria. 2022;24:249-59.
Published in Internet: 04-10-2022 - Visits: 11780
Abstract
Introduction: premature infants are at higher risk of complications after birth, and prematurity is the leading cause of death in the neonatal period. The main objective of this study was to characterize preterm births in Galicia, Spain.
Material and methods: in 2016, we carried out a cross-sectional study in Galicia using the Risk Behavior Information System, or SICRI. The study universe consisted of all Galician women aged 18 to 49 years who gave birth between September-2015 and August-2016 (n=18 822) and their liveborn infants (n=19 204). Data were collected between November 2016 and January 2017 through computer-assisted telephone interviews with participants. We estimated the prevalence of preterm birth (before 37 weeks of gestation), overall and based on different variables. We fitted a logistic regression model to identify variables associated with preterm birth.
Results: we obtained information from 6436 women aged 18 to 49 years. The response rate was 76%. In 2016, 7.9% of births in Galicia were preterm. The prevalence increased with age. The highest prevalence was found in women with multiple pregnancies. Obstetric characteristics such as multiple pregnancy and primiparity and risk behaviours were identified as factors that increase the probability of preterm birth. Attendance to childbirth classes and a pregnancy weight gain greater than 12 kg were identified as protective factors.
Conclusions: in Galicia, 8 out of 100 births are preterm. Some of the identified factors that increase the risk of preterm birth are modifiable, and health providers should take them into account in prenatal care.
Keywords
● Health education ● Pregnancy ● Preterm birthINTRODUCTION
Every year approximately 15 million premature infants are born worldwide. This is the result of birth before the 37th week of gestation, or preterm birth.1 Among premature newborns we can distinguish extremely premature, born before the 28th week of gestation (WG), very premature (28-31 WG), moderately premature (32-33 WG) and late premature (34-36 WG).2 Owing to the immaturity of their organs and immune system, premature newborns are at increased risk of suffering complications, such as necrotizing enterocolitis, intraventricular haemorrhage or bronchopulmonary dysplasia.3 For this reason, prematurity is the main cause of death in newborns and the second cause, after pneumonia, in children under the age of 5 years.4 Moreover, it has been observed that prematurity could have a negative impact on school performance and development during childhood,3 and on cardiovascular health in adult life by increasing the risk of impaired cardiac function.5
According to the World Health Organization (WHO), the number of preterm births is increasing in almost every country for which data are available.4 In Spain, the prevalence of preterm birth increased from 6.9% in 20116 to 7.5% in 2016.7
These prevalences indicate that prematurity is a significant problem in Spain, highlighting the need to explore its determining factors.
Although progress has been made in recent years in identifying the obstetric risk factors associated with preterm birth,8 little is known of its relationship with environmental and social factors. The main objective of this study was to characterise preterm births in Galicia in 2016.
MATERIALS AND METHODS
Study setting
The study was carried out in Galicia, an autonomous community located in the north-west of Spain, which had 2.7 million inhabitants in 2016. The population of Galicia is concentrated in 7 cities, which in 2016 ranged between 68 308 and 292 817 inhabitants, and in the coastal strips of the north-west and south-west.
Study design
In 2016, we conducted a cross-sectional study within the framework of the Galician Risk Factor Information System (SICRI). The target population was 18 822 women aged 18 years and over, resident in Galicia, who gave birth between 1 September 2015 and 31 August 2016, and their 19 204 children born live during that period. The framework used to select the sample of women was the register of the Newborn Screening Programme for Early Detection of Endocrine and Metabolic Diseases. The sampling was random, stratified by age group (18-24, 25-29, 30-34, 35-39 and 40 or over), and in a second stage a child was selected for each mother in cases of multiple birth. We calculated the sample size of mothers independently for each age band, with an expected prevalence of 50% and a sampling error of less than 2%. The theoretical sample size was 6777 mothers and their children born live. The information was collected between November 2016 and January 2017 using the computer-assisted telephone interviewing (CATI) system.
Variables
The instrument we used to collect information was a questionnaire developed specifically for this study and subsequently validated on a sample of the target population. Questions were included on behaviour, attitudes and experiences, referring to the 6 months before pregnancy, pregnancy, delivery, and the time of the survey.
Various sociodemographic and health characteristics were assessed:
- Sociodemographic characteristics: maternal age, at the time when the information was collected, categorised in four age groups (18-24, 25-29, 30-34, 35-39 and 40 or over); country of birth (Spain or other); area of residence (urban, semi-urban or rural); educational attainment (basic: cannot read or write or no education but can read and/or write or incomplete primary education; intermediate: compulsory or post-compulsory secondary education or vocational training; higher: undergraduate or graduate university education); living situation (living with partner vs not living with partner) and employment situation (employed: in work or on leave; unemployed; inactive: student, homemaker or pensioner).
- Pregnancy history: primiparity and voluntary termination of pregnancy (previous voluntary termination of pregnancy [VTP]).
- Obstetric characteristics – planning and monitoring of pregnancy: planned pregnancy, pregnancy by artificial insemination, preconception consultation with a healthcare provider, high-risk pregnancy, multiple pregnancy, bed rest during pregnancy, attendance at childbirth classes. All these variables were treated as dichotomous (yes/no). Information was obtained on weight status before the pregnancy, classifying it according to body mass index (BMI) as underweight, normal weight, overweight or obese, and on weight gain of more than 12 kg during pregnancy (yes/no).
- Health status indicators: self-perceived health status before and during pregnancy (very good, good, normal, poor or very poor) and use of sleep aids, anxiolytics, antidepressants or diabetes medication before or during pregnancy.
- Maternal lifestyle: smoking and drinking (never, before pregnancy or during pregnancy), physical activity (before and during pregnancy) and adherence to dietary recommendations (before and during pregnancy). These last two variables were considered to be lifestyle indicators; we considered that women who reported exercising had actually done so and that they adhered to dietary recommendations if they reported having fruit or vegetables every day and fish every week.
To identify preterm births, we asked participants in which week they had given birth. We defined preterm birth as birth before 37 WG.
Statistical analysis
We performed a descriptive analysis and estimated the prevalence of preterm birth according to various characteristics of the mothers. We calculated 95% confidence intervals (CIs) for all obtained percentages.
To identify the determinants of preterm birth, we fitted a multivariate logistic regression model, in which preterm delivery was the dependent variable, and the sociodemographic characteristics, pregnancy-related variables, pregnancy history, obstetric characteristics, health status indicators and health-related behaviours found to be significantly associated with the dependent variable (p < 0.2) in a previous bivariate analysis were included as explanatory variables. The variables with a p < 0.05 were retained in the final model, and we calculated the adjusted odds ratios (ORs) of having a preterm delivery for each of them. We also calculated the corresponding 95% CIs.
The analysis was performed with the weighted sample using the Stata software, version 14.2.
Ethical considerations
Because this study was voluntary and confidentiality was guaranteed, it did not require approval by an ethics committee. The study was conducted by telephone, and therefore the agreement of the women to participate in the call implied consent.
RESULTS
We obtained information from 6436 women aged from 18 to 49 years. The response rate was 76%.
The mean age of participants at the time of delivery was 33.4 years; 9.9% were aged 40 or over. Primiparous mothers (57.0%) were on average 2 years younger than non-primiparous mothers (32.4 vs. 34.6 years). In all, 44.1% had higher education, 94.7% were married or lived with a partner, 11.9% smoked during pregnancy and 59.6% attended childbirth classes (Table 1).
| Table 1. Characteristics of women aged 18 to 49 years who gave birth in Galicia between September 2015 and August 2016. Percentages with 95% confidence intervals | |||
|---|---|---|---|
| Sociodemographic characteristics | % | 95% CI | |
| Age | 18-29 years | 21.3 | 21.1-21.5 |
| 30-34 years | 34.1 | 33.9-34.3 | |
| 35-39 years | 34.7 | 34.5-34.9 | |
| ≥40 years | 9.9 | 9.8-10.0 | |
| Country of birth | Spain | 89.1 | 88.3-89.9 |
| Other | 10.9 | 10.1-11.7 | |
| Area of residence | Urban | 71.0 | 69.9-72.1 |
| Semi-urban | 19.5 | 18.6-20.4 | |
| Rural | 9.6 | 8.8-10.3 | |
| Educational attainment | Basic | 18.8 | 17.8-19.7 |
| Intermediate | 37.1 | 35.9-38.3 | |
| Higher | 44.1 | 42.9-45.4 | |
| Living situation | Living with partner | 94.7 | 94.2-95.3 |
| Not living with partner | 5.3 | 4.7-5.9 | |
| Employment situation | Employed | 71.7 | 70.6-72.9 |
| Unemployed | 18.6 | 17.6-19.6 | |
| Inactive | 9.7 | 9.0-10.4 | |
| Pregnancy history | Primiparous | 57.0 | 55.8-58.3 |
| Previous voluntary termination of pregnancy (VTP) | 8.7 | 8.0-9.4 | |
| Obstetric characteristics - planning and monitoring of pregnancy | % | 95% CI | |
| Planned pregnancy | 80.1 | 79.1-81.1 | |
| Pregnancy by artificial insemination | 6.9 | 6.3-7.6 | |
| Preconception consultation | 39.8 | 38.6-41.1 | |
| High-risk pregnancy | 20.4 | 19.4-21.4 | |
| Multiple pregnancy | 3.6 | 3.2-4.1 | |
| Bed rest during pregnancy | 26.9 | 25.8-28.1 | |
| Childbirth classes | 59.6 | 58.4-60.9 | |
| Weight status before pregnancy | Underweight | 4.8 | 4.3-5.4 |
| Normal weight | 66.3 | 65.1-67.5 | |
| Overweight | 21.0 | 19.9-22.0 | |
| Obese | 7.9 | 7.3-8.6 | |
| Weight gain >12 kg | 39.8 | 38.5-41.0 | |
| Health status (HS) | % | 95% CI | |
| Self-perceived HS before pregnancy | Very good | 25.1 | 24.0-26.2 |
| Good | 47.6 | 46.3-48.9 | |
| Normal | 25.2 | 24.1-26.3 | |
| Poor or Very poor | 2.1 | 1.7-2.5 | |
| Self-perceived HS during pregnancy | Very good | 33.1 | 31.9-34.3 |
| Good | 37.4 | 36.1-38.6 | |
| Normal | 20.4 | 19.3-21.4 | |
| Poor or Very poor | 9.2 | 8.5-10.0 | |
| Medication before or during pregnancy | Sleep aids or anxiolytic drugs | 4.5 | 4.0-5.1 |
| Antidepressant drugs | 3.6 | 3.1-4.1 | |
| Medication for diabetes | 2.9 | 2.5-3.3 | |
| Lifestyle habits | % | 95% CI | |
| Smoking | Never | 72.1 | 71.0-73.3 |
| Before pregnancy | 16.0 | 15.0-16.9 | |
| During pregnancy | 11.9 | 11.1-12.8 | |
| Drinking | Never | 45.8 | 44.6-47.1 |
| Before pregnancy | 51.5 | 50.2-52.8 | |
| During pregnancy | 2.7 | 2.3-3.1 | |
| Before and during pregnancy | Physical activity | 18.0 | 16.9-19.0 |
| Adherence to dietary recommendations | 41.4 | 40.1-42.7 | |

A total of 7.9% (95% CI: 7.2-8.7) of the women had a preterm delivery. The highest prevalence was observed among women with multiple pregnancy and with poor or very poor self-perceived health status before the pregnancy: 31.0% (95% CI: 24.9-37.2) and 17.4% (95% CI: 10.9-24.0), respectively (Table 2; this table does not show prevalences for characteristics that were not associated with preterm birth).
| Table 2. Prevalence of preterm birth according to maternal characteristics with the corresponding 95% confidence intervals (95% CI) | ||||
|---|---|---|---|---|
| Sociodemographic characteristics | % | 95% CI | p-value | |
| Age | 18-29 years | 6.6 | 5.4-7.7 | 0.012 |
| 30-34 years | 6.9 | 5.7-8.1 | ||
| 35-39 years | 6.7 | 5.5-7.9 | ||
| ≥40 years | 10.2 | 8.4-12.1 | ||
| Educational attainment | Basic | 8.6 | 7.0-10.2 | 0.093 |
| Intermediate | 6.9 | 5.8-8.0 | ||
| Higher | 6.6 | 5.6-7.6 | ||
| Living situation | Living with partner | 6.9 | 6.3-7.6 | 0.044 |
| Not living with partner | 9.9 | 6.6-13.2 | ||
| Pregnancy history | % | 95% CI | p-value | |
| Primiparous | No | 6.4 | 5.4-7.4 | 0.077 |
| Yes | 7.6 | 6.7-8.5 | ||
| Previous voluntary termination of pregnancy (VTP) | No | 6.8 | 6.1-7.5 | 0.014 |
| Yes | 9.8 | 7.2-12.4 | ||
| Obstetric characteristics - planning and monitoring of pregnancy | % | 95% CI | p-value | |
| Pregnancy by artificial insemination | No | 6.4 | 5.8-7.1 | <0.001 |
| Yes | 16.1 | 12.7-19.5 | ||
| Preconception consultation | No | 6.0 | 5.2-6.8 | <0.001 |
| Yes | 8.7 | 7.6-9.9 | ||
| High-risk pregnancy | No | 4.8 | 4.1-5.4 | <0.001 |
| Yes | 16.2 | 14.1-18.2 | ||
| Multiple pregnancy | No | 6.2 | 5.6-6.8 | <0.001 |
| Yes | 31.0 | 24.9-37.2 | ||
| Bed rest during pregnancy | No | 5.1 | 4.4-5.7 | <0.001 |
| Yes | 12.6 | 11.0-14.2 | ||
| Childbirth classes | No | 9.3 | 8.1-10.5 | <0.001 |
| Yes | 5.6 | 4.8-6.3 | ||
| Weight gain >12 kg | No | 8.2 | 7.3-9.1 | <0.001 |
| Yes | 5.4 | 4.5-6.3 | ||
| Health status (HS) | % | 95% CI | p-value | |
| Self-perceived HS before pregnancy | Very good | 4.8 | 3.8-5.9 | <0.001 |
| Good | 7.0 | 6.1-8.0 | ||
| Normal | 8.6 | 7.1-10.0 | ||
| Poor or very poor | 17.4 | 10.9-24.0 | ||
| Self-perceived HS during pregnancy | Very good | 5.3 | 4.3-6.3 | <0.001 |
| Good | 6.4 | 5.4-7.5 | ||
| Normal | 8.1 | 6.6-9.6 | ||
| Poor or very poor | 13.9 | 11.0-16.8 | ||
| Sleep aids or anxiolytic drugs (before or during pregnancy) | No | 6.8 | 6.1-7.4 | <0.001 |
| Yes | 13.4 | 9.3-17.4 | ||
| Antidepressant drugs (before or during pregnancy) | No | 6.9 | 6.2-7.5 | <0.001 |
| Yes | 13.3 | 8.5-18.0 | ||
| Medication for diabetes (before or during pregnancy) | No | 7.0 | 6.3-7.6 | 0.029 |
| Yes | 11.3 | 6.6-16.0 | ||
| Lifestyle habits | % | 95% CI | p-value | |
| Smoking | Never | 6.6 | 5.9-7.4 | <0.001 |
| Before pregnancy | 6.6 | 5.0-8.2 | ||
| During pregnancy | 10.5 | 8.3-12.7 | ||
| Physical activity (before and during pregnancy) | No | 7.4 | 6.7-8.2 | 0.033 |
| Yes | 5.5 | 4.1-6.9 | ||

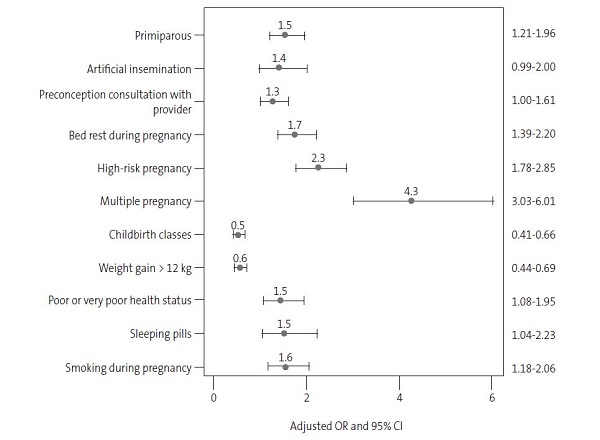
The probability of having a preterm delivery was higher among women with multiple pregnancy (OR: 4.3) or high-risk pregnancy (OR: 2.3). Other factors associated with a higher probability of preterm birth were bed rest during pregnancy (OR: 1.7), smoking during pregnancy (OR: 1.6), use of sleep aids or anxiolytics (before and during pregnancy) (OR: 1.5), primiparity (OR: 1.5), poor or very poor self-perceived health status during pregnancy (OR: 1.5), pregnancy by artificial insemination (OR: 1.4) and preconception consultation with a healthcare provider (OR: 1.3).
The probability of preterm birth was lower among women who attended childbirth classes (OR: 0.5) or whose weight increased more than 12 kg during pregnancy (OR: 0.6) (Figure 1).
| Figure 1. Characteristics associated with preterm pregnancy. Odds ratios (OR) with the corresponding 95% confidence intervals (95% CI) |
|---|
 |

DISCUSSION
In Galicia, 8 out of every 100 pregnant women had a preterm delivery in 2016. The factor that most increased the probability of preterm birth was multiple pregnancy. Some of the factors associated with preterm birth, such as smoking or weight gain during pregnancy, are modifiable. We identified two factors associated with a lower probability of preterm birth: attending childbirth classes and gaining more than 12 kg during pregnancy.
In Spain, according to data from the National Institute of Statistics (INE),7 7.5% of births in 2016 were preterm, a similar percentage to the one estimated in this study in Galicia. The information provided by the INE does not make it possible to ascertain the characteristics of women who have a preterm delivery in Spain, a key issue in designing preventive strategies. Various studies have identified biological determinants as the main risk factors for preterm birth.9 Among them, the most relevant risk factor is extreme maternal age (under 18, over 40).10-12 We were unable to assess the impact of extreme maternal age in detail in our study, as the sample did not include any women younger than 18 years. The bivariate analysis showed that the prevalence of preterm birth was higher among women aged 40 or over, although advanced maternal age did not remain in the model as an explanatory variable, probably because of its relationship with variables such as artificial insemination or multiple pregnancy. In line with previous studies, primiparity and multiple pregnancy were associated with an increased probability of preterm delivery.8,13 The risk of preterm birth among primiparous women was associated mainly with a greater risk of preeclampsia, with the resulting increase in iatrogenic preterm birth.13 In the case of multiple pregnancy, the characterisation of preterm birth must be addressed in a broader context, since it may be explained by factors associated with spontaneous preterm birth (such as uterine distension), by its association with fertility treatments or artificial insemination, as well as by the greater frequency of induced delivery associated with the complications of multiple gestation.14,15 Various causes of maternal infertility could predispose to preterm birth, although the underlying mechanism of this association is unknown.16,17 These causes include advanced maternal age in developed countries, with the consequent diminished ovarian reserve.18
In our study, various forms of care that women received before delivery were associated with preterm birth. These included preconception consultation and bed rest. Women who seek preconception consultations with healthcare providers could have had some medical condition and/or a poor obstetric history, such as high-risk pregnancies or previous miscarriages. We were unable to assess this with the data available to us, as we did not have access to a detailed obstetric history. Bed rest was identified in our study as a factor that increases the probability of preterm birth, although we do not know the reason why it was recommended and there could be a reverse causation bias if bed rest was prescribed due to the risk of preterm birth. Healthcare professionals recommend that pregnant women with severe preeclampsia or preterm premature rupture of membranes should maintain strict or modified bed rest from diagnosis to the end of gestation.19
An important issue that healthcare professionals should take into account is weight gain during pregnancy. As described in a previous study,20 we found that a gestational weight gain greater than 12 kg was associated with a lower probability of preterm birth. At present, the guidelines of the Institute of Medicine (IOM) guidelines are generally taken as reference in Spain, and the recommended weight gain varies between 5 kg and 25 kg depending on pre-pregnancy maternal BMI and whether or not the pregnancy is multiple. In the case of a singleton pregnancy in a mother with normal weight (BMI 18.5-24.9 kg/m2), a gestational weight gain of 11.5 to 16 kg is recommended. A weight gain greater or smaller than recommended by the IOM is associated with adverse perinatal outcomes, including low birth weight or prematurity when the weight gain is insufficient.21
Maternal depression, anxiety or stress can lead to hormonal changes in the hypothalamic-pituitary-adrenal axis, precipitating preterm birth.22 Furthermore, suffering a mental health disorder during pregnancy may result in women perceiving a poor state of health or even needing pharmacological treatment to control it. As in previous studies,8 the probability of having a preterm delivery was higher among women who were using sleep aids or anxiolytics, before or during pregnancy, or who had a poor or very poor self-perceived health.
Normally, women change their behaviour during pregnancy, establishing healthier lifestyle habits. This was observed among the Galician women, who during pregnancy gave up smoking, and especially drinking. Despite the decrease observed in the prevalence of tobacco use, 12% of pregnant women continued smoking, an alarming percentage. The effects of smoking on the child’s health are well established, and are associated with vasoconstriction and foetal hypoxia caused by various components of tobacco after passing through the placenta. These effects on foetal health notably include the risk of placental abruption, premature rupture of membranes or intrauterine growth restriction.23 Smoking ranks as the main modifiable factor on which healthcare professionals who provide care to Galician pregnant women should intervene. Even though the number of cigarettes consumed by women who continued smoking during pregnancy decreased (data not shown), this is not sufficient and there should be progress towards total cessation of smoking. To achieve this, healthcare professionals should deliver clear health messages stating the objective risk associated with tobacco consumption.
As far as we know, this is the first study to identify childbirth classes as a protective factor against preterm birth in Europe.24 In Galicia, these classes are provided as one of the services covered by the public health system of the region.25 They consist of at least 8 structured group sessions, taught by midwives, directed towards health education and promotion aimed at women and their partners from 28 WG onwards. They address various aspects of pregnancy, childbirth, the postpartum period, breastfeeding, newborn care, sexuality and contraception. A Cochrane review from 201626 showed that care provided by midwives based on respecting the physiology of pregnancy, childbirth and the postpartum period with the minimum possible intervention (the midwife-led continuity model) is associated with a decreased probability of preterm birth, contrary to the results of a previous review,7 which found no differences.
Among the limitations of this study are those related to its cross-sectional design, and to the fact that the information was obtained from post-natal self-reporting by mothers. The latter may be a source of recall bias, since questions were asked relating to the 6 months before participants became aware of the pregnancy. A social desirability bias could also be present, leading them to conceal behaviours, especially when asked about smoking, drinking, or the use of sleep aids, anxiolytics or antidepressants. Because of the cross-sectional nature of the study, sometimes it is not possible to determine the direction of causality; this was the case when we analysed the association between bed rest and preterm birth. Two further limitations arise from the fact that we did not include underage pregnant women or pregnant women who had stillbirths.
One of the strengths of this study was the high participation rate and the sample size, as it included 1 in 3 of the total of nearly 19 000 mothers who gave birth in Galicia during the study period. Moreover, its design makes it possible to generalise the conclusions, since the women did not come from a specific health system and were a representative sample of pregnant women.
It should be emphasised that many of the studies published to date on preterm births adopt a pathogenic approach aimed at evaluating specific therapeutic interventions, losing sight of the population-based approach. This study was conducted from a public health perspective, paying particular attention to modifiable variables. The results underscore the importance of appropriate health education in pregnancy, providing lifestyle recommendations in preconception consultations (for example, ideal weight gain during pregnancy), and of encouraging attendance at childbirth classes. In Spain, during the SARS-CoV-2 pandemic, childbirth classes were considered dispensable in most public hospitals, and it was exceptional for women to be provided with a safe alternative, such as online access, to maintain them.
CONCLUSIONS
In Galicia, 8 out of every 100 births are preterm; some of the identified factors that increase the probability of a preterm birth are modifiable, and health professionals must therefore keep them in mind when providing recommendations to pregnant women during prenatal evaluations. The identification of childbirth classes as a factor that reduces the probability of preterm birth was an important finding, one that encourages the future performance of a study to specifically assess the impact of this intervention.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
BMI: body mass index · CI: confidence interval · INE: Instituto Nacional de Estadística (National Institute of Statistics) · IOM: Institute of Medicine · OR: odds ratio · SICRI: Sistema de Información sobre Conductas de Riesgo de Galicia (Galician Information System on Risk Behaviours) · VTP: voluntary termination of pregnancy · WG: week of gestation.
REFERENCES
- Liu l, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388:3027-35.
- Mendoza Tascón LA, Claros Benítez DI, Osorio Ruíz MÁ, Mendoza Tascón LI, Peñaranda Ospina CB, Carrillo Bejarano JH, et al. Epidemiología de la prematuridad y sus determinantes, en una población de mujeres adolescentes y adultas de Colombia. Rev Chil Obstet Ginecol. 2016;81:372-80.
- Shapiro-Mendoza CK, Barfield WD, Henderson Z, James A,.House JL, Iskander J, et al. CDC Grand Rounds: Public Health Strategies to Prevent Preterm Birth. MMWR Morb Mortal Wkly Rep. 2016;65:826-30.
- March of Dimes, PMNCH, Save the Children, WHO. Born Too Soon: The Global Action Report on Preterm Birth. Geneva. Eds CP Howson, MV Kinney, JE Lawn. World Health Organization; 2012 [online] [accessed 23/08/2022]. Available at www.marchofdimes.org/materials/born-too-soon-the-global-action-report-on-preterm-.pdf
- Telles F, McNamara N, Nanayakkara S, Doyle MP, Williams M, Yaeger l, et al. Changes in the Preterm Heart From Birth to Young Adulthood: A Meta-analysis. Pediatrics. 2020;146:e20200146.
- Nacimientos por tipo de parto, tiempo de gestación y grupo de edad de la madre 2011 [Todos los partos, Todos los Tiempos, Todas las edades]. In: Instituto Nacional de Estadística [online] [cited 8/05/2021]. Available at www.ine.es/jaxi/Tabla.htm?path=/t20/e301/nacim/a2011/l0/&file=01011.px&L=0
- Nacimientos por tipo de parto, tiempo de gestación y grupo de edad de la madre 2016 [Todos los partos, Todos los Tiempos, Todas las edades]. In: Instituto Nacional de Estadística [online] [cited 8/05/2021]. Available at www.ine.es/jaxi/Tabla.htm?path=/t20/e301/nacim/a2016/l0/&file=01011.px&L=0
- Cobo T, Kacerovsky M, Jacobsson B. Risk factors for spontaneous preterm delivery. Int J Gynaecol Obstet. 2020;150:17-23.
- Ceriani Cernadas JM. The main causes of prematurity and their very common associated disorders. Arch Argent Pediatr. 2019;117:210-1.
- Lawlor DA, Mortensen l, Andersen A-MN. Mechanisms underlying the associations of maternal age with adverse perinatal outcomes: a sibling study of 264 695 Danish women and their firstborn offspring. Int J Epidemiol. 2011;40:1205-14.
- Fuchs F, Monet B, Ducruet T, Chaillet N, Audibert F. Effect of maternal age on the risk of preterm birth: A large cohort study. PloS One. 2018;13:e0191002.
- Fraser AM, Brockert JE, Ward RH. Association of Young Maternal Age with Adverse Reproductive Outcomes. N Engl J Med. 1995;332:1113-8.
- Ferrero DM, Larson J, Jacobsson B, Di Renzo GC, Norman JE, Martin JN, et al. Cross-Country Individual Participant Analysis of 4.1 Million Singleton Births in 5 Countries with Very High Human Development Index Confirms Known Associations but Provides No Biologic Explanation for 2/3 of All Preterm Births. PloS One. 2016;11:e0162506.
- Refuerzo JS. Impact of multiple births on late and moderate prematurity. Semin Fetal Neonatal Med. 2012;17:143-5.
- Kulkarni AD, Jamieson DJ, Jones HW, Kissin DM, Gallo MF, Macaluso M, et al. Fertility Treatments and Multiple Births in the United States. N Engl J Med. 2013;369:2218-25.
- Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and Very Low Birth Weight in Infants Conceived with Use of Assisted Reproductive Technology. N Engl J Med. 2002;346:731-7.
- Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update. 2012;18:485-503.
- Fortuño C, Labarta E. Genetics of primary ovarian insufficiency: a review. J Assist Reprod Genet. 2014;31:1573-85.
- Artal R. Exercise during pregnancy and postpartum period. In: Uptodate [online] [cited 29/03/2021]. Available at www.uptodate.com/contents/exercise-during-pregnancy-and-the-postpartum-period#
- Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, et al. Association of Gestational Weight Gain With Maternal and Infant Outcomes: A Systematic Review and Meta-analysis. JAMA. 2017;317:2207-25.
- Rogozińska E, Zamora J, Marlin N, Betrán AP, Astrup A, Bogaerts A, et al. Gestational weight gain outside the Institute of Medicine recommendations and adverse pregnancy outcomes: analysis using individual participant data from randomised trials. BMC Pregnancy Childbirth. 2019;19:322.
- Lockwood CJ. Spontaneous preterm birth: pathogenesis. In: Uptodate [online] [cited 8/04/2021]. Available at www.uptodate.com/contents/spontaneous-preterm-birth-pathogenesis?search=preterm%20birth&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3
- Kyrklund-Blomberg NB, Cnattingius S. Preterm birth and maternal smoking: risks related to gestational age and onset of delivery. Am J Obstet Gynecol. 1998;179:1051-5.
- Cunningham SD, Lewis JB, Shebl FM, Boyd LM, Robinson MA, Grilo SA, et al. Group Prenatal Care Reduces Risk of Preterm Birth and Low Birth Weight: A Matched Cohort Study. J Womens Health (Larchmt).2019;28:17-22.
- Guías técnicas del Plan de Atención Integral a la Salud de la Mujer: Grupo de trabajo del plan de atención integral a la salud de la mujer. Guía técnica do proceso de educación prenatal e postnatal. Xunta de Galicia; 2008. Available at www.sergas.es/Asistencia-sanitaria/Documents/40/PMG05.pdf
- Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev. 2015:CD004667.





